KOLEGIUM ORTHOPAEDI DAN TRAUMATOLOGI INDONESIA
PERHIMPUNAN DOKTER SPESIALIS ORTHOPAEDI DAN TRAUMATOLOGI INDONESIA
JAKARTA, JUNI 2012
KURIKULUM
PENDIDIKAN DOKTER SPESIALIS
ORTHOPAEDI DAN TRAUMATOLOGI
Penanggung Jawab : Prof. dr. Errol U Hutagalung, SpB, SpOT(K)
- (Ketua Kolegium Orthopaedi dan Traumatologi Indonesia )
Prof Dr. dr. Moh. Hidayat, SpB, SpOT(K) - (Wakil Ketua)
Ketua Komisi Kurikulum: Prof. Dr. dr. Putu Astawa, MKes. SpB, SpOT (K) Sekretaris Komisi : Dr. dr. Nucki N Hidajat, MKes, SpOT(K) Anggota : Prof. Dr. dr. Moh Hidajat, SpB, SpOT(K)
- Staf Pengajar PPDS Orthopaedi dan Traumatologi FKUB
dr. Ifran Saleh, SpOT(K)
- KPS PPDS Orthopaedi dan Traumatologi FKUI Dr. dr. Ismail, SPOT ( K )
- SPS PPDS Orthopaedi dan Traumatologi FKUI Dr. dr. Ferdiansyah, SpOT(K)
- Ka Dept. Orthopaedi & Traumatologi FK UNAIR /RSU Dr.Soetomo
Dr. dr. Dwikora Novembri Utomo, SpOT(K) - - KPS PPDS Orthopaed dan Traumatologi FUNAIR
dr. Mouli Edward, SpOT(K)
- - KPS PPDS Orthopaed dan Traumatologi FKUNAIR Dr. dr. Hermawan Nagar Rasyid, SpOT(K), MT(BME), PhD
- KPS PPDS Orthopaedi dan Traumatologi FK UNPAD dr. Yoyos Dias Ismiarto, SpOT(K)
- SPS PPDS Orthopaedi dan Traumatologi FK UNPAD Prof. Dr. dr. H.R. Agung Saifullah, SpB,SpOT(K) - KPS PPDS Orthopaedi dan Traumatolohi FK UNHAS dr. M. Ruksal Saleh, SpOT(K), PhD
- SPS PPDS Orthopaedi danTraumatologi FK UNHAS dr. Ismail Mariyanto, SpOT(K)
dr. Mujaddid Idulhaq, M.Kes, SpOT
- SPS PPDS Orthopaedi dan Traumatologi FK UNS Dr. dr. Rahadyan Magetsari, SpOT(K)
- KPS PPDS Orthopaedi dan Traumatologi FKUGM Dr. dr. Puntodewo, M.Kes, SpOT(K)
- SPS PPDS Orthopaedi dan Traumatologi FKUGM Prof. Dr. dr. I Ketut Siki Kawiyana, SpB, SpOT(K) - KPS PPDS Orthopaedi dan Traumatologi FK UNUD dr. I Ketut Suyasa, SpB, SpOT (K)
- SPS PPDS Orthopaedi dan Traumatologi FK UNUD Dr. dr. Edi Mustamsir, SpOT (K)
- KPS/Ka. SMF Orthopaedi dan Traumatologi FKUB dr. Istan Irmansyah, SpOT (K)
- SPS PPDS Orthopaedi dan Traumatologi FKUB
Editor : Prof. Dr. dr. Putu Astawa, MKes, SpOT(K)
- Staf Pengajar PPDS Orthopaedi dan Traumatologi FK UNUD
Dr. dr. Nucki N Hidajat, MKes, SpOT(K)
- Kepala Dept. Orthopaedi dan Traumatologi FK UNPAD /RS Dr. Hasan Sadikin
Syukur Alhamdulillah kita panjatkan ke hadirat Allah SWT, bahwa telah bisa diterbitkan buku kurikulum Progam Pendidikan Dokter Spesialis (PPDS) Orthopaedi dan Traumatologi oleh Kolegium Orthopadi dan Traumatologi edisi tahun 2012 ini, Buku ini merupakan revisi dan perubahan format serta penambahan di beberapa bagian dari edisi 2007, hal ini dilakukan atas dasar bahwa ilmu Orthopaedi dan Traumatologi merupakan cabang ilmu kesehatan yang terus bergerak secara dinamis sesuai dengan kebutuhan masyarakat maupun perkembangan ilmu teknologi kedokteran sendiri.
Penambahan yang paling signifikan adalah dalam aspek kompetensi afektif serta bidang sport injury, yang menjadi sumber rujukan adalah Kurikulum pendidikan dari British Orthopaedic Assossiation (BOA) yang disesuaikan dengan kondisi situasional local dan tingkatan kompetensi dari KKI (Konsil Kedokteran Indonesia).
Kami sangatlah menyadari buku kurikulum ini jauh dari kesempurnaan sehingga merupakan keniscayaan adanya asupan dan kritikan yang dapat membuat buku ini menjadi lebih baik.
Wassalam. Editor.
Ketua Kolegium Orthopaedi dan Traumatologi
Indonesia
Dokter Spesialis Orthopaedi dan Traumatologi adalah dokter yang telah mencapai kemampuan tertentu dan secara professional mengkhususkan diri dalam pelayanan bidang Orthopaedi dan trauma muskuloskeletal dan mempunyai kemampuan menyerap, mengembangkan serta mentransformasikan keilmuannya.
Penerbitan Buku Kurikulum Pendidikan Dokter Spesialis Orthopaedi dan Traumatologi edisi tahun 2012 merupakan hasil penyempurnaan cetakan sebelumnya, Pada edisi ini dimasukan berbagai informasi baru yang merupakan hasil pengembangan dan pendalaman serta penyelarasan dari berbagai sumber.
Buku kurikulum ini disusun oleh Kolegium dan menjadi paduan bagi seluruh pimpinan, pendidik, tenaga kependidikan, dan paserta didik program dokter spesialis Orthopaedi dan Traumatologi di Indonesia, untuk dapat dilaksanakan secara konsisten. Disamping itu, untuk melengkapi buku ini diterbitkan pula buku Standar Penyelenggaraan Pendidikan Profesi Dokter spesialis Orthopaedi dan Traumatologi.
Kami mengucapkan terima kasih dan penghargaan setinggi-tingginya kepada Editor, Tim komisi Kurikulum kolegium Orthopaedi dan Traumatologi, dan anggota Kolegium lainya yang telah bekerja keras untuk menuangkan informasi yang relevan dan terkini serta melakukan kajian-kajian secara berkesinambungan dalam penyusunan buku ini.
Saran dan kritik untuk penyempurnaan buku kurikulum ini dapat ditujukan kepada Tim kurikulum kolegium Orthopaedi dan Traumatologi Indonesia.
Semoga Allah Subhanahu Wata’ala memberikan bimbingan, petunuk, dan kekuatan kepada kita. Aamiin.
Jakarta, Juni 2012 Ketua Kolegium Orthopaedi & Traumatologi Indonesia (Periode Nopember 2010 – Nopember 2012)
SURAT KEPUTUSAN Nomor : 013/Koleg-IOT/XII/2012
Kolegium Orthopaedi dan Traumatologi Indonesia Tentang
PELAKSANAAN PEMAKAIAN BUKU KURIKULUM
PENDIDIKAN DOKTER SPESIALIS ORTHOPAEDI DAN TRAUMATOLOGI KOLEGIUM ORTHOPAEDI DAN TRAUMATOLOGI
Menimbang : 1. Bahwa untuk menjalankan kegiatan Pendidikan Dokter Spesialis Orthopaedi dan Traumatologi diperlukan Buku Kurikulum Pendidikan Dokter Spesialis Orthopaedi dan Traumatologi.
2. AD / ART BAB 1. Pasal 13.2 Tentang Tugas Kolegium Orthopaedi dan Traumatologi Indonesia yaitu ayat 13.2.12 : Menyusun katalog pendidikan profesi dokter spesialis dan spesialis konsultan Orthopaedi dan Traumatologi Indonesia.
Mengingat : 1. SK Kolegium Orthopaedi dan Traumatologi Indonesia mengenai Koordinator Pelaksana Komisi Kurikulum Kolegium Orthopaedi dan Traumatologi Indonesia tanggal 23 Desember 2009 yaitu menugaskan Komisi Kurikulum untuk merevisi Kurikulum dan Standarisasi Seleksi Nasional Peserta Didik, yang diharapkan revisi Kurikulum sudah dapat digunakan pada Januari 2011.
2. Untuk menjalankan kegiatan Pendidikan Dokter Spesialis Orthopaedi dan Traumatologi diperlukan Buku Kurikulum Pendidikan Dokter Spesialis Orthopaedi dan Traumatologi.
Memutuskan : 1. Bahwa hasil revisi Buku Kurikulum Pendidikan Dokter Spesialis Orthopaedi dan Traumatologi dapat mulai digunakan sebagai buku pegangan Program Studi Orthopaedi dan Traumatologi Indonesia. 2. Surat keputusan ini berlaku sejak tanggal ditetapkan.
3. Bila kemudian hari ada kekeliruan, SK ini dapat diperbaiki sebagaimana mestinya.
CARA PENGGUNAAN BUKU
Buku ini terdiri atas 4 Bab.
Bab I
, Pendahuluan mengambarkan filosofi yang mendasari
disusunnya Kurikulum dan beberapa pengertian tentang istilah yang
dipergunakan didalamnya.
Pada Bab II
, Menjelaskan tentang isi atau kontain yang terbagi
dalam bidang Kognitif, Psikomotor, dan Afektif.
Bidang kognitif dikelompokkan berdasarkan kombinasi antara region
anatomis (Spine, Hip, Knee, Ankle Foot, Shoulder Elbow, Hand),
Diseases
(Oncology, Paediatrik, Sport Injuri, dan Trauma), dan
Ilmu-ilmu Dasar (
Basic science, General Orthopaedi
).
Bidang Psikomotor dikelompokkan dalam Trauma Hard Tissue dan
Soft Tissue (General, Upper limb, Pelvic girdle, Lower limb, spine),
dan Non trauma dengan pembagian sesuai dengan regionya.
Bidang Afektif di bagi kedalam 6 kelompok, yaitu Perilaku
Profesional, Komunikator yang baik, mengajar dan melatih,
Keeping
Up to date
, Menjadi manajer yang baik,
Promoting Good Health
,
Etika.
Bab III
, Menjelaskan secara sistematika tahapan pencapaian
Kompetensi, dan ruang lingkup yang harus di bahas maupun
dikerjakan. Tingkat Kompetensi yan dipakai dalam buku ini adalah
sesuai dengan standar dari KKI, yang matrikulasi semua ini
dijabarkan di dalam lampiran 1, 2 dan 3.
Bab IV
, Dalam bab ini dijelaskan secara sistematis cara
melaksanakan Kurikulum dari ketiga aspek Pendidikan, Prasyarat,
serta Ketentuan-ketentuan yang harus dipenuhi, serta bagaimana cara
memonitor dan evaluasinya.
Tim Penyusun dan Editor………. i
Kata Pengantar ... iii
Kata Sambutan Ketua Kolegium ……….. iv
Surat Keputusan Penggunaan Buku Kurikulum... Vi Cara penggunaan buku ... Vii Daftar isi ... viii
BAB I PENDAHULUAN... 1
1.1 Pengertian Kurikulum Ilmu Orthopaedi dan Traumatologi Indonesia ………... 2
1.2 Model Kurikulum………. 2
BAB II ISI KURIKULUM... 3
2.1 Bidang Kognitif (Applied Clinical Knowledge Syllabu).... 6
2.2 Bidang Psikomotor (Applied Clin Procedures Syllabus. 25 2.3 Bidang Afektif (Professional & Management and Good Clinical Practice)………. 34 BAB III TINGKAT KOMPETENSI DAN LINGKUP BAHASAN………... 41
3.1. Tingkat Kompetensi………. 41
3.2 Tahapan Pencapaian Kompetensi………...…….. 43
BAB IV PELAKSANAAN KURIKULUM... 47
4.1 Cara Pelaksanaan ………. 47
4.2 Modul tambahan Kursus ………. 47
4.3 Karya Ilmiah Wajib……….. 48
4.4 Pelaksanaan Stase………. 48
4.5 Monitor dan Evaluasi ………... 50
4.6 Buku Acuan Wajib ……….. 52
DAFTAR PUSTAKA... 53
LAMPIRAN... 54
Lampiran 1 Tingkat Kompetensi Kognitif Peserta didik berdasarkan Topik dan Thapan Pendidikan……… 54
75
84 91 Lampiran 2 Tingkat Kompetensi Psikomotor Peserta Didik
berdasarkan Topik dan Tahapan………... Lampiran 3 Tingkat Kompetensi Afektif Berdsarkan Topik dan
Tahapan Pendidikan ………
BAB I
PENDAHULUAN
Pencapaian kesehatan yang optimal sebagai hak asasi
manusia masyarakat perlu mendapat perhatian. Pelayanan yang baik
dan bermutu merupakan dambaan masyarakat Indonesia. Untuk
mendapatkan itu perlu dihasilkan pelayan kesehatan yang baik
termasuk perawat, dokter umum dan juga dokter sepesialis. Dokter
sebagai salah satu komponen utama pemberi pelayanan kesehatan
masyarakat mempunyai peran yang sangat penting sehingga
Pendidikan Kedokteran akan menjadi penting.
Untuk memberikan perlindungan kepada pasien dan
mempertahankan mutu pelayanan kesehatan pemerintah dengan
Undang-undang RI No. 20 tahun 2003 tentang Sistem Pendidikan
Nasional dan Undang-Undang RI No. 29 tahun 2004 tentang
Praktik Kedokteran menekankan Standar Pendidikan Kedokteran
dam memberi kepastian hukum kepada masyarakat dan Dokter.
Asosiasi Institusi Pendidikan Kedokteran berkoordinasi
dengan Organisasi Profesi, Kolegium, Asosiasi Rumah Sakit
Pendidikan, Departemen Pendidikan Nasional dan Departemen
Kesehatan Kolegium kedokteran dalam menyusun standar
Pendidikan Profesi Dokter berkoordinasi dengan Organisasi Profesi,
Asosiasi Institusi Pendidikan, Departemen Pendidikan Nasional dan
Departemen Kesehatan
1.1.
Pengertian Kurikulum Ilmu Orthopaedi dan Traumatologi
Indonesia
Kurikulum merupakan seperangkat rencana dan pengaturan
pendidikan yang meliputi tujuan pendidikan, isi, bahan pelajaran,
cara pencapaian dan penilaian, yang digunakan sebagai pedoman
penyelenggaraan Pendidikan Ilmu Orthopaedi dan Traumatologi
1.2. Model Kurikulum
Model Kurikulum berbasis Kompetensi dilakukan dengan
pendekatan terintegrasi baik horizontal maupun vertikal, serta
berorientasi pada masalah kesehatan individu, keluarga dan
masyarakat dalam konteks pelayanan kesehatan paripurna
.
ISI KURIKULUM
Isi Kurikulum meliputi prinsip-prinsip metode ilmiah,
biomedik, ilmu kedokteran klinik dalam hal ini Ilmu Orthopaedi
dan Traumatologi, Ilmu humaniora yang disesuaikan dengan
Standar Kompetensi yang ditetapkan. Prinsip-prinsip metode
ilmiah meliputi metodologi penelitian, filsafat ilmu, berpikir kritis,
biostatistik dan
evidence-based medicine
.
Ilmu biomedik meliputi anatomi, biokimia, histologi,
biologi sel dan molekuler, fisiologi, mikrobiologi, imunologi,
parasitologi, patologi, dan farmakologi. Ilmu biomedik dijadikan
dasar ilmu kedokteran klinik dalam hal ini Ilmu Orthopaedi dan
Traumatologi sehingga anak didik mempunyai pengetahuan yang
cukup untuk memahami konsep dan praktik kedokteran klinik.
Ilmu-ilmu humaniora meliputi ilmu perilaku, psikologi
kedokteran, sosiologi kedokteran dan profesionalisme. Menurut Dr.
Victor Neufeldt, satu kunci konsep kurikulum baru adalah “…
that
it is not only the sum total of residents’ experience, planned or
unplanned. A broader view is needed, and the curriculum should be
seen as an
activity
where residents and faculty
learn
and
work
Kurikulum berdasarkan Kompetensi terdiri atas dua
komponen utama yaitu
Core
Kurikulum dan
Non Core
Kurikulum
(
miss program of special study, local content
.)
Core
Kurikulum
sangat penting yang harus dikuasai oleh semua residen dan terdiri
dari :
1. Bidang Kognitif (
Applied Clinical Knowledge Syllabus
)
2. Psikomotor (
Applied clinical Procedure Syllabus
)
3. Afektif (
Professional and Management and Good Clinical
Practice
)
Core Curriculum
dapat disederhanakan menjadi
General
Core Curriculum
kemudian komponen Kurikulum sehingga
memudahkan Peserta Didik untuk mengikuti proses belajar
mengajar.
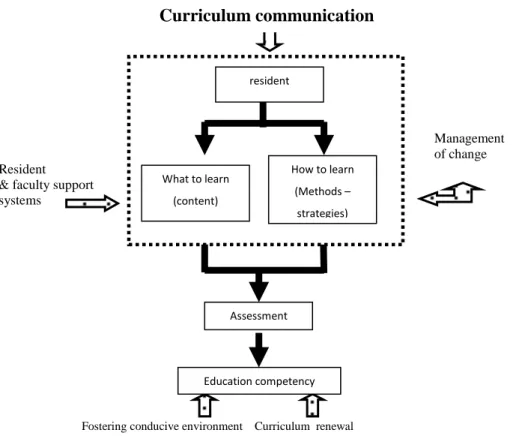
Fostering conducive environment Curriculum renewal
Gambar 1.1. Skema Tujuan Komprehensif Kurikulum
Management of change Resident
& faculty support systems
Curriculum communication
resident What to learn (content) How to learn (Methods – strategies) Assessment Education competency2.1. Bidang Kognitif
(Applied Clinical Knowledge Syllabus
)
1. BASIC SCIENCE
No. General Core
Curriculum
Komponen Curriculum
1A Anatomy: Clinical and functional anatomy with pathological and operative relevance
Anatomy (and embryology) of nervous and vascular systems
Surgical approaches to the limbs and axial skeleton
Anatomy (and embryology) of musculo-skeletal system
1B. Tissues: Bone - Structure & Function
Cartilage - articular, meniscal - Structure & Function
Muscle and tendon - Structure & Function
Synovium - Structure & Function
Ligament - Structure & Function
Nerve - Structure & Function
Intervertebral disc - Structure & Function 1C Physiology,
Biochemistry & Genetics:
Structure and function of connective tissues
Application/relevance of modern genetics to orthopaedic disease and treatment
Shock - types, physiology, recognition and treatment
Metabolism and hormonal regulation
Metabolic and immunological response to trauma
Blood loss in trauma/surgery, fluid balance and blood transfusion
Bone grafts, bone banking and tissue transplantation 1D. Biomechanics &
Bioengineering:
Biomechanics of musculoskeletal tissues
Biomechanics of fracture fixation
Tribology of natural and artificial joints
Design of implants and factors associated with implant failure(wear, loosening)
Kinematics and gait analysis
2. BONE, JOINT DISEASE & GENERAL ORTHOPAEDIC
2A General: Osteoarthritis
Osteoporosis
Metabolic bone disease
Rheumatoid arthritis and other arthropathies (inflammatory, crystal, etc)
Haemophilia
Curriculum
2A General: (Cont.) Neuromuscular disorders - inherited and acquired
Osteonecrosis
Osteochondritides
Heterotopic ossification 2B Investigations: Blood tests
Musculoskeletal imaging: x-ray, contrast studies ( myelography, arthrography), CT, MR, ultrasound, radioisotope studies
Effects of radiation
Bone densitometry
Electrophysiological investigations 2C Operative Topics: Tourniquets
Principles of Sterilization
Design of theatres & Skin preparation
Anaesthesia - principles and practice of local and regional anaesthesia and principles of general anaesthesia
Principle treatment of musculoskeletal tumor
Principle surgery of musculoskeletal tumor
Infection, Thromboembolism & Pain:
Infection of bone, joint, soft tissue, including tuberculosis , and their prophylaxis
2D Miscellanous: Thromboembolism and prophylaxis
Behavioural dysfunction and somatization
AIDS and surgery in high-risk patients
Management of Pain and pain relief
Complex regional pain syndromes e.g. Reflex Sympathetic
Dystrophy and Causalgia 2E Prosthetics &
Orthotics:
Principles of design
Prescription and fitting of standard prostheses
Principles of orthotic bracing for control of disease, deformity and instability
2E Research & Audit: Design and conduct of clinical trials
Data analysis and statistics - principles and applications
Principles of Epidemiology
Audit 2F Medical Ethics: Duties of care
Informed consent
Medical negligence
3. HAND & MICRORECONSRUCTION
3A. Anatomy of: The wrist/MCP/PIP/DIP joints and CMC joint of the thumb
The flexor and extensor mechanism of the fingers including interaction between extrinsic and intrinsic mechanism
The posture of the thumb in pinch, power and key grip
The nerve supply to the hand
The closed compartments of forearm and hand
3B. Pathology: An understanding of the special circum-stances associated with swelling and the effects of rising pressure in a closed compartment secondary to infection and injury
An understanding of the special circum-stances in which oedema causes fibrosis and permanent stiffness
Tendon injury and healing
Nerve injury and healing
An appreciation of the imbalances and deformities associated with inflammatory arthritis
A classification system for congenital hand disorders
Langers lines
Hand tumours (e.g. ganglion/enchondroma)
Dupuytren's disease 3C. Clinical
Assessment:
History of examination of hand and wrist in the assessment of tendons, distal radioulnar and radiocarpal joints
Ability to elicit median, ulnar and radial nerve function and disorders
Recognition of patterns of presentation of common compressive neuropathies and brachial neuralgia
Assessment of intrinsic and extrinsic motors in digits and recognition of common deformities and deficiencies
Awareness of presentation of work-related hand disorders
Ability to examine and assess common rheumatoid hand deformities, e.g.: inferior radioulnar subluxation and carpal translo-cation; MCP subluxation and ulnar drift; digital Boutonniere and swan neck; thumb Boutonniere deformity and CMC disease
Curriculum
3D. Investigations: Interpretation of plain and stress x-rays of wrist.
A knowledge of other views
Awareness of role of MRI/bone scan/ arthrography/arthroscopy
Place and interpretation of nerve conduction studies 3E.
Treatment:
Knowledge of a strategy of management for the osteoarthritic rheumatoid hand.
Understanding of the place of soft tissue
reconstruction, joint fusion, interposition and excision arthroplasty in the treatment of the arthritic hand and wrist.
Knowledge of the management of stenosing
tenovaginitis
Knowledge of the principles of treatment for common flexor and extensor tendon injuries and of the common surgical approaches to the digital flexor and extensor compartments
Fractures of metacarpals and phalanges
Familiarity with the surgical treatment of
Dupuytren’s disease
Awareness of the principles of tendon transfer for the reconstruction of mediun, ulnar and radial nerve palsy and familiarity with simple transfers, e.g. indicis to EPL
Knowledge of splinting techniques and
rehabilitation principles
Ability to plan management for finger tip injuries and undertake
closed management
Knowledge of surgical approach to digits with particular regard to the restoration of function and prevention of stiffness
Knowledge of the levels for digital amputation
Injuries of ulnar collateral ligament of thumb
Dislocations of carpus and carpal instability
Knowledge of closed and operative options of treatment for fractures of distal radius and common carpal injuries including scaphoid non union.
Familiarity with the surgical treatment of common compressive neuropathy
Curriculum 4. KNEE
4A. Anatomy: Knowledge of regional anatomy of the knee, including:
Surface anatomy
Neural and vascular structures and their relations with particular reference to standard anterior and posterior surgical approaches
Knowledge of regional anatomy of the knee, including:
Surface anatomy
Neural and vascular structures and their relations with particular reference to standard anterior and posterior surgical approaches
Bones and joints
Functional anatomy of ligaments and supporting muscles
Innervation of the knee including controlling musculature
The extent and function of the synovium and bursae of the knee
The structure and function of the menisci, and articular cartilage
4B. Biomechanics: The mechanics of the patello-femoral mechanism
The medial and lateral weight-bearing joints and their inter-relationship
The cruciate and collateral ligaments and other ligamentous and muscular supports
Menisci and articular cartilage
4C. Pathology: The mechanism of ligamentous, bony and combined trauma to the knee and healing potential
A complete knowledge of arthritides, including degenerate wear, ageing changes and traumatic damage
Pathology of inflammatory disease and infection affecting the knee
The response of synovium to debris
Benign and malignant conditions in the knee and surrounding structures including recognised classification where appropriate
4D. Clinical Assessment:
A sound knowledge and understanding of:
History and examination of the knee to include relevant surrounding structures
The standard clinical signs of the knee and relevant adjacent structures and competent skill in describing these
Curriculum 4D. Clinical
Assessment: (Cont.)
A critical understanding of rating and outcome measures in common use
4E. Investigations: Indications for and interpretations of:
Radiographs – standard and specialised
Blood investigation
Aspiration
Special investigations including CT, MRI and radioisotope scanning
Arthroscopy
Biomechanical testing
4F. Treatment: A sound knowledge of conservative and surgical
management, including the indications for referral to a specialist of:
Paediatric disorders, including deformity, dislocations, epiphyseal disorders, osteochondritis and discoid meniscus
Adolescent disorders including patello femoral and meniscal dysfunction, osteochondritis dissecans
Young adult disorders including patello femoral and meniscal injuries, instability and ligament deficiency, synovial disorders, benign and malignant tumours
Degenerative and inflammatory arthritis, including a balanced understanding of conservative and surgical options,including osteotomy, arthrodesis and arthroplasty
Traumatic disorders including skin and soft tissue injuries, fractures and dislocations of patella, tibia and femoral components, ligament ruptures and internal derangement of the knee. Conservative and surgical indications and detailed .Methods of treatment. Outcomes of conservative and operative management
Infections, particularly infections and inflammations of the bursae, intra-articular sepsis, prevention and management of sepsis in implant surgery
A sound working knowledge of the range of arthroplasties for primary and revision surgery for patello femoral, unicompartmental and total replacement of the knee with particular reference to secure bone anchorage, alignment, ligament stability and optimising range of movement; a good knowledge of post-operative complications, their Sprophylaxis and management
Curriculum 4F. Treatment
(cont):
A knowledge of the indications and techniques of revision surgery particularly for aseptic and septic loosening
A knowledge of simple arthroscopic surgery including meniscectomy, trimming and shaving
An appreciation of complex arthroscopic procedures
An appreciation of medical and surgical techniques available to repair and replace articular cartilage 5. ANKLE & FOOT
5A. Anatomy: Bones and articulations
Ligamentous structures – ankle/hindfoot/ midfoot
Plantar fascia and MTP anatomy
Surface markings of neural and vascular structures
Tendon anatomy
Muscle compartments of the foot
5B. Biomechanics: Function of the lower limb and foot in gait
Ankle and subtalar joint
Plantar fascia mechanisms
Tendon function
Orthoses and footwear 5C. Pathology: Arthritides
Degenerative joint disease
Rheumatoid foot disease
Neuropathy
Neuropathic joint and skin changes
Tumours
E.g. osteoid osteoma and plantar fibroma
Clinical Assessment:
History and clinical examination of the foot and ankle in order to assess pain, joint function, deformity, nerve, muscle and tendon function
5D. Ability to recognise and assess the following diseases of the ankle and foot: 1) Neurological
disorders:
Charcot joint
Morton's neuroma
Nerve entrapment
Neurological foot deformity
2) Trauma: Evaluation of skin and soft tissue injury
Compartment syndrome
Recognition of all fractures and dislocations
Curriculum
2) Trauma: (Cont.) Hindfoot pain
Ankle instability
Heel pain
Degenerative disease of the ankle
Rheumatoid arthritis
Osteochondritis dissecans of talus 3) Forefoot
disorders:
Hallux valgus
Hallux rigidus
Lesser toe deformities
Metatarsalgia
Inflammatory arthritis
4) Tumours: Ability to recognise and assess local foot swellings
Diabetic foot:
Complex foot deformity
Flatfoot deformity - mobile and rigid
Cavus deformity
Residual congenital foot deformity 5E. Investigations:
Radiograph: Standard foot and ankle views CT, MRI and
Scintigraphy:
Knowledge of role of these ancillary investiga-tions in certain specific condiinvestiga-tions e.g. infection, tumour, tibialis posterior rupture, osteonecrosis
EMG: Relevance to foot and ankle disorders
5F. Treatment Non-operative:
Knowledge of rational basis for the use of footwear modifications, orthoses and total contact casting
Operative: Detailed knowledge of closed and operative methods for management of fractures and dislocations of ankle, hindfoot and forefoot, including knowledge of common reconstructive surgical procedures for foot deformity including hallux valgus, lesser toe deformity, acquired flat-foot, to include arthrodesis, osteotomy and soft-tissue reconstruction
Knowledge of common amputations through foot
and ankle
Knowledge of common reconstructive surgical
procedures for degenerative and inflammatory disorders of ankle and foot including arthrodesis, arthroplasty, excision arthroplasty procedures to first ray both proximal and distally for management of hallux valgus and rigidus
Curriculum 6. HIP JOINT 6A. Anatomy: 6B. Basic knowledge of the regional anatomy of the hip including:
Development of the hip joint
Relationship of bony elements
Blood supply of the femoral head
Anatomical course of all major regional vessels and nerves
The capsule, labrum and related ligaments
An understanding of the action, anatomy and innervation of the regional musculature
Detailed knowledge of the applied anatomy of common surgical approaches to the hip (medial, anterior, lateral and posterior)
6C. Biomechanics: An understanding of the lever arms, muscles and body weight forces that produce the joint reaction force in both normal and abnormal hips
An understanding of the application of these principles to the rationale of both pelvic and femoral osteotomies, and replacement arthroplasty
Knowledge of the tribological properties of materials used for articulating surfaces
Knowledge of the biocompatibility and mechanical properties of materials in common use in total hip arthroplasty
6D. Pathology: Basic knowledge of the pathology of pyogenic and non-pyogenic arthritis, slipped upper femoral epiphysis [SUFE], Perthes' disease and hip dysplasia
Mechanism and pattern of common fractures and fracture dislocations around the hip (intracapsular, extracapsular, acetabular and periacetabular, femoral head, etc)
Knowledge of the pathology of osteoarthritis, rheumatoid arthritis and the seronegative arthritides at the hip and of osteonecrosis of the femoral head
Familiarity with current theories of the aetiopathogenesis of osteoarthritis
An understanding of the microbiological rationale for the prevention of sepsis in total hip arthroplasty 6E. Clinical
Assessment:
A sound knowledge of clinical assessment of the hip, lumbosacral spine and knee. Particular reference should be paid to the gait, the Trendelenberg sign, limb length, loss of movement and deformity at the joint
Curriculum
6E. The trainee needs to be well informed of current opinion regarding aetiopathogenesis, clinical presentation and appropriate investigation of:
Proximal femoral fractures (intracapsular, extracapsular) and simple fracture dislocations of the hip
Osteoarthritis and the inflammatory arthropathies
Perthes' disease
Slipped upper femoral epiphysis
Septic arthritis
Osteonecrosis
Soft tissue conditions around the hip (snapping hip, gluteus medius tendonitis, etc)
A working knowledge of the clinical presentations and investigations of:
The sequelae of CDH and hip dysplasia
The sequelae of SUFE
Juvenile chronic arthritis
Non pyogenic arthritis
The painful total hip replacement
6F. Investigation: A working knowledge of the interpretation of plain radiographs, dynamic arthrography, CT, bone scintigraphy and MRI of the hip region
A working classification of proximal femoral and periacetabular fractures. Also, mechanisms and classification of failure of joint replacement and of periprosthetic fractures
6G. Treatment: Non-operative
An understanding of the principles of traction, bracing and spica immobilisation
An understanding of the non operative aspects of the management of hip pathology
Operative
A thorough knowledge of soft tissue surgery, osteotomy, arthrodesis and arthroplasty (excision and replacement). A sound knowledge of anterior, anterolateral, lateral and posterior approaches to the hip and of the complications associated with each
A sound knowledge of: internal fixation of proximal femoral fractures, hemiarthroplasty for intracapsular fractures, primary total hip replacement for OA and inflammatory arthropathies in the elderly, simple proximal femoral osteotomies. Familiarity with potential complications (i.e. thromboembolism, sepsis, dislocation, etc) and be aware of current opinion on the prevention and management of these complications
A knowledge of the indications for, and principles of, complex proximal femoral osteotomies, hip arthroscopy, reconstruction of the hip in young adults (JCA and hip dysplasia, etc), complex hip revision surgery
Curriculum
6G. Treatment (Cont.) An appreciation of complex acetabular and pelvic fractures, complex periacetabular osteotomies
An understanding of the place of modern technologies such as, joint resurfacing procedures minimally invasive hip replacements and computer assisted implantation in the management of hip pathology and the attendant risks and complications
7. THE SPINE
7A. Anatomy: Development of the spine, spinal cord and nerve roots
Surgical anatomy of the cervical, dorsal and lumbosacral spine
Anterior and posterior surgical approaches to the spine at each level
7B. Biomechanics: Basic knowledge of the biomechanics of the cervical and lumbosacral spines
An understanding of the biomechanics of spinal instability as applied to trauma, tumour, infection and spondylolysis/listhesis
Biomechanics of spinal deformity
A knowledge of the basic mechanics of spinal instrumentation
7C. Pathology: Pathophysiology of the ageing spine and degenerative disc disease
Acute and chronic infections of the spine
Pathology of spinal deformity
Pathology of the acutely prolapsed cervical and lumbar disc
Recognition of patterns of spinal injury and associated cord and nerve root damage
Tumours of the spine 7D. Clinical
Assessment:
A thorough knowledge of general and orthopaedic history-taking and examination
A knowledge of the assessment of spinal deformity
An understanding of the assessment of thoracic pain
A sound knowledge of clinical assessment of the spine for low back pain, sciatica, spinal claudication, neck pain, radiating arm pain, spinal injury and incipient myelopathy
A knowledge of the assessment of spinal tumour
A basic knowledge of the assessment of a patient after failed spinal surgery
Curriculum
7E. Investigation: A thorough knowledge of the basic investigations required in spinal surgery, specifically: blood tests, plain radiographs, bone scintigraphy, discography, electrophysiological studies [including cord monitoring], CT scanning, MRI scanning
A thorough knowledge of how each of these investigations contributes to the diagnosis and management of each of the major areas of spinal disease
7F. Treatment:
Non-operative A knowledge of the non-surgical methods available for the treatment of low back pain, sciatica, claudication, neck pain, spinal deformity, instability, tumour, infection and fracture to include:
Analgesics and NSAIDs, physiotherapeutic regimes, pain clinic techniques, bracing, use of radiotherapy and chemotherapy, non-operative management of spinal injuries
Operative A sound knowledge of the indications for and operative surgical management of the acute prolapsed lumbar intervertebral disc, spinal stenosis, lumbar spinal instability due to spondylolysis/listheses
A knowledge of the indications for, and operative surgical management of the acutely
prolapsed cervical disc, cervical stenosis, spinal injury and the surgery of spinal infection
A basic knowledge of the surgery of spinal deformity and tumours of the spine
8. TRAUMA
8A. Anatomy: Applied to diagnosis and surgical treatment of common bone, joint and soft tissue injuries
Knowledge of those anatomical structures particularly at risk from common injuries or in surgical approaches
Physeal anatomy and its application to injury
8B. Biomechanics: Application to open reduction and internal fixation of fractures and external skeletal fixation
Applied to fracture formation and fracture treatment both operative and non-operative
Biomechanics of implants and fracture fixation systems, including their material properties
Epidemiology and Research Methods:
Research and audit methods including the design of clinical trials
Curriculum 8C. Pathophysiology
& Pathology:
Applied to fracture and soft tissue healing, including skin, muscle, tendon and neurological structures
Classification systems for fractures and dislocations
Pathology of non-union of fractures
Response of the body, and local musculoskeletal tissues to infection
Systemic response of body to major injury
Mechanisms underlying Acute Respiratory Distress Syndrome and similar life threatening conditions
Science of fluid replacement therapy in the acutely injured including application to the treatment of burns
Science of treatment of compartment syndrome
Response of infants, children and the elderly to injury 8D. Clinical
Assessment:
Initial clinical assessment of the patient with severe injury, including spinal cord injury, soft tissue injury, burns and head injury
Assessment of all types of fracture and dislocation, their complications, early and late
Identification of life threatening/ limb threatening injuries. Understanding priorities of treatment 8E. Investigations: Knowledge of the principles, application and side effects
of commonly used investigations, including radiographs, CT and MRI scans, radio-isotope imaging, ultrasound scans and electrophysiological investigations
8F. Management: Knowledge of different treatment options for musculoskeletal injury, both non-operative and operative. Ability to analyse the pros and cons for each method
Ability to manage the overall care of the severely injured
Ability to undertake the complete treatment of all types of common fracture and dislocation including the bone and soft tissue treatment of open fractures and the treatment of pathological fractures
Where common injuries are normally treated by a sub specialist (e.g. spinal injury, arterial injury or intra cranial haemorrhage) there should be ability to manage the initial treatment of the patient and know the principles of the specialist treatment
Principles of reconstructive surgery for the injured, including treatment of non-union and malunion of fractures, bone defects, chronic post-traumatic osteomyelitis and delayed treatment of nerve injury; principles of soft tissue reconstruction
The principles of amputation in the injured and the rehabilitation of such patients
Curriculum
9. PAEDIATRIC ORTHOPAEDIC
9A Basic Science: Detailed knowledge of the growth of bones, physeal anatomy and its application to fracture types and pathological processes and infection in particular
Knowledge of the anatomy of bones and joints in the growing child and its application to growth and deformity
Knowledge of the neurological processes involved in the production of deformity e.g. spina bifida, cerebral palsy and muscular dystrophy
9B Clinical Assessment:
Core knowledge should be at least that of a general orthopaedic textbook
'Expert' knowledge, i.e. the level of the speciality journal is required for those wishing to pursue a career in children's orthopaedics
The trainee must be able to clinically examine a child competently and to relate effectively with the family
The trainee must be able to make proper management decisions in paediatric practice and to refer appropriately for treatment
9C Investigations: Knowledge of the indications for plain x-ray, arthrogram, CT, MRI and the ability to interpret the images
Knowledge of the indications for the use of ultrasound and nuclear imaging
Awareness of the limitations of certain investigations in paediatric practice
9D Treatment: A sound knowledge of normal variants, e.g. knock knees, bow legs and flat feet
A detailed knowledge of the treatment for:
o Fractures (including non-accidental injury) and growth plate injuries and recognise the sequelae
o Bone and joint infection
o Common childhood orthopaedic conditions, e.g. irritable hip, anterior knee pain
A working knowledge of the treatment for:
o Slipped epiphysis
o Perthes' disease
o Developmental dysplasia of the hip
o Talipes
o Scoliosis
o Simple foot deformities (e.g. hallux valgus, metatarsus varus)
Curriculum
9D Treatment (Cont.): oSimple congenital hand abnormalities (e.g. trigger thumb)
oOsteogenesis imperfecta
oSkeletal dysplasias
oTarsal coalitions
oTorticollis
oLeg length discrepancy
9E A knowledge of: Screening services for congenital abnormalities
Assessment of physical disability 10. SHOULDER & ELBOW
10A. Anatomy:
Basic knowledge of the regional anatomy of the shoulder including:
Detailed anatomy of the sternoclavicular, acromioclavicular, glenohumeral and elbow joints to include the connecting bones, muscles and tendons acting across them, neurovascular supply, bursae and relationships to local structures
Surgical approaches: deltopectoral and posterior approaches to glenohumeral joint; superior (McKenzie) approach to rotator cuff; and surgical approaches to the acromioclavicular and sternoclavicular joints
Structure and function of the above joints; a clear understanding of the static and dynamic stabilisers of the glenohumeral and elbow joints
10B. Biomechanics: Biomechanics of the shoulder and elbow to the level of the currently published specialist journals
Knowledge of the various types of shoulder and elbow prostheses including the factors influencing design, wear and loosening to the level of the currently published specialist journals
10C. Pathology: Sound knowledge of all commonly encountered benign and malignant conditions affecting the shoulder girdle, elbow and surrounding soft tissues
A basic understanding of the pathology of:
Impingement and rotator cuff disorders
Instability of the shoulder and the elbow
Inflammatory and degenerative conditions affecting the articular cartilage and synovium
Infection
Adhesive capsulitis of the shoulder
The pathology of the stiff elbow
Disorders such as ulnar neuritis and tennis or golfer’s elbow
Curriculum 10D. Clinical
Assessment:
Detailed history and examination of the painful, stiff or unstable shoulder or elbow
Knowledge of clinical tests used specifically to assess instability of the shoulder and elbow, rotator cuff disorders, the stiff shoulder or elbow and the use of local anaesthetic in assessment. Examples are the apprehension tests for shoulder instability, impingement signs and tests, Gerber’s lift off test, Napoleon's sign, elbow instability tests, ulnar nerve assessment
Knowledge of conditions causing referred symptoms to the shoulder and elbow (e.g. cervical spine diseases, entrapment neuropathies and thoracic outlet disorders)
Knowledge to the level of a basic specialist shoulder textbook of common conditions affecting the shoulder including instability, impingement, rotator cuff tears, adhesive capsulitis, osteoarthritis, rheumatoid disease, avascular necrosis, biceps tendon disorders, fractures of the proximal humerus and clavicle, and disorders of the acromioclavicular and sternoclavicular joints and scapula
Knowledge to the level of a basic specialist elbow textbook of common conditions affecting the elbow including instability, osteoarthritis, rheumatoid arthritis, causes of stiffness, soft tissue problems such as medial and lateral epicondylitis, neuropathies and fractures around the elbow
10E. Investigation: Knowledge of plain radiographs as used to assess shoulder and elbow disorders. This should include a knowledge of those special views (e.g. Modified axial, Stryker notch, Supraspinatus Neer outlet and cubital tunnel views) required to assess adequately the conditions which commonly affect the shoulder and elbow. The ability to recognise correctly normal and abnormal abnormalities on plain radiographs
Knowledge of the value of ultrasound, arthrography, CT and MRI as used to assess the shoulder and elbow. An ability to identify straightforward abnormalities on CT and MRI (e.g. full thickness and partial thickness rotator cuff tears on MRI and the pathological anatomy of fractures around the shoulder and elbow using CT)
Knowledge of the use and abuse of arthroscopy of the shoulder and elbow including a knowledge of normal and abnormal arthroscopic findings
Curriculum 10F. Treatment:
1) Non-operative An ability to supervise the non-operative management of fractures, dislocations and soft tissue injuries around the shoulder and elbow
An in-depth knowledge of the management of straightforward fractures and dislocations of the shoulder girdle and elbow. Knowledge of the treatment options for more complex fractures with an understanding that these might more appropriately be referred to someone with a special interest; examples of these might include four part fractures of the proximal humerus and complex intraarticular fractures of the distal humerus. An ability to recognise upper limb injuries involving injuries to the brachial plexus and refer on as appropriate
A knowledge of injection techniques for both the shoulder and the elbow
Knowledge of both the non-operative and operative treatment of common disorders such as recurrent anterior traumatic instability of the shoulder, rotator cuff impingement and small rotator cuff tears, adhesive capsulitis, acromioclavicular joint pain
2) Operative A knowledge of the management of soft tissue elbow disorders such as lateral and medial epicondylitis and ulnar neuropathy
Knowledge of the indications, options and complications for prosthetic replacement of the shoulder and elbow. A detailed knowledge of the surgical techniques is not required
2) Operative (cont.) Knowledge of the indications and benefits of arthroscopy of the shoulder and elbow. An ability to perform an arthroscopic assessment of the shoulder is expected but a knowledge of the techniques of arthroscopic surgery procedures is not required
Understanding the principles of management of tumours around the shoulder and elbow
11. ORTHOPEDIC ONCOLOGY
11A Basic Knowledge of the presentation, radiological features, pathological features, treatment and outcome for common benign and malignant bone tumours
Knowledge of the presenting features, management and outcome of soft tissue swellings, including sarcomas benign and malignant
Understanding of the principles of management of patients with metastatic bone disease in terms of investigation, prophylactic and definitive fixation of pathological fractures and oncological management
Curriculum 11B Classification benign/malignant Tissue of origin 11C Staging Investigations Enneking Classification Biopsy techniques
Basic Histopathologal Interpreatation 11D Treatment Principles surgical treatment
Incisional Excision Marginal Excision Wide Excision Radical Excision Radiotherapy Chemotherapy-principles of action
Treatment of pathological fracturres
Palliative treatment 11E Specific Tumours
Bone Primary
Osteoid Osteoma
Osteoblastoma
Osteosarcoma
Ewing sarcoma
Giant cell sarcoma
Chondrosarcoma
MFH
Fibrosarcoma
Multiple myeloma Metastases General Features Soft Tissues Tumor General features
12. SPORT INJURY
12A Arthroscopy Principles of Arthroscopy
Common indication of arthroscopy
Standard and additional portals for knee, shoulder arthroscopy
Complication of arthroscopy
12B Pathoanatomy of ACL/PCL injuries and their management
Pathoanatomy of MCL/LCL injueris and their management
Pathoanatomy of meniscal injuries and management
Patella-femoral disorder and various causes of anterior knee pain
Curriculum
12B Cont.: Types and synovials plicae and treatment
Management of knee dislocation and multiple ligaments injury
12C Shoulder Pathoanatomy of recurrent shoulder dislocation
and management
Types of shoulder impingement syndrome and ita
management
Rotator cuff arthropathy
Types of AC joint dislocation
12D Ankle Acute and chronic ankle ligaments injury
Impingement syndrome and meniscoid lesion
NO. TOPIC PROCEDURE 1. TRAUMA
1A Trauma General
Free flap
Full thickness skin graft
Muscle flap
Nerve repair
Pedicle flap
Removal external fixator or frame
Removal foreign body from skin / subcutaneous tissue
Removal K wires or skeletal traction
Split skin graft
Transpositional flap
Wound closure, delayed primary or secondary
Wound Debridement
Internal Fixation of Long Bone
Internal fixation of complex fracture
External fixation
Periarticuler fracture
Tendon repair
Vascular repair
Casting and splinting
1B Axial Sceleton
1) Cervical Spine Anterior fixation fracture / dislocation cervical spine
Application halo / tong traction cervical spine
MUA fracture / dislocation cervical spine
Posterior fixation fracture / dislocation cervical spine 2) Thoraco-lumbal
Spine
Posterior decompression / fixation thoracic spine
Lumbar Spine
Anterior decompression / fixation lumbar spine
Posterior decompression / fixation lumbar spine 3) Pelvis Simple acetabular fracture ORIF
Complex acetabular fracture ORIF
Pelvic fracture:
Pelvic fracture external fixator application
Simple pelvic fracture ORIF
1C Upper Limb
1) Brachial Plexus Exploration / repair / grafting brachial plexus 2) Clavicle ORIF clavicle fracture
ORIF non-union clavicle fracture 3) Shoulder Joint Anterior dislocation shoulder
Anterior dislocation shoulder closed reduction
Anterior dislocation shoulder open reduction +/- fixation
Acromioclavicular joint dislocation acute ORIF
Fracture proximal humerus ORIF
Glenoid fracture ORIF
Posterior dislocation shoulder closed reduction 4) Humerus Fracture diaphysis humerus non-op:
Non-union ORIF +/- bone grafting
Fracture diaphysis humerus IM nailing
Fracture diaphysis humerus MUA +/- POP
Fracture diaphysis humerus ORIF plating 5) Elbow Joint Dislocated elbow +/- fracture:
Dislocated elbow +/- fracture closed reduction
Dislocated elbow +/- fracture open reduction +/- fixation
Intraarticular distal humerus fracture ORIF
Lateral condyle fracture ORIF
Medial condyle / epicondyle fracture MUA / K wire / ORIF
Olecranon fracture ORIF
Dislocated elbow +/- fracture:
Radial head / neck fracture MUA +/- K wire
Radial head / neck fracture ORIF
Radial head replacement for fracture
Supracondylar fracture:
Supracondylar fracture MUA +/- K wires
Supracondylar fracture ORIF
6) Forearm Fasciotomy for compartment syndrome
Fracture distal radius:
Fracture distal radius – closed non-op
Fracture distal radius external fixation
Fracture distal radius MUA & percutaneous wires
Fracture distal radius MUA & POP
Fracture distal radius ORIF
Fracture shaft radius / ulna:
Fracture shaft radius / ulna IM nailing
Fracture shaft radius / ulna MUA & percutaneous wires
Fracture shaft radius / ulna MUA & POP
7) Wrist Carpal fracture / dislocation:
Carpal fracture / dislocation MUA & percutaneous wires
Carpal fracture / dislocation MUA & POP
Carpal fracture / dislocation ORIF
Scaphoid fracture non-op
Scaphoid fracture ORIF
Scaphoid fracture MUA & percutaneous wires
Scaphoid fracture non-union ORIF +/- graft
8) Hand:
Carpal fracture / dislocation:
5th metacarpal fracture / dislocation non-op
5th metacarpal fracture / dislocation MUA & percutaneous wires
5th metacarpal fracture / dislocation MUA & POP
5th metacarpal fracture / dislocation ORIF
Finger tip reconstruction
Infection:
Infection hand drainage (not tendon sheath)
Infection tendon sheath drainage
IPJ fracture / dislocation:
IPJ fracture / dislocation MUA & percutaneous wires
IPJ fracture / dislocation MUA +/- POP
IPJ fracture / dislocation ORIF
Ligament repair hand
Metacarpal fracture (not 1st or 5th) non-op
Metacarpal fracture (not 1st or 5th) MUA & Percutaneous wires
Metacarpal fracture (not 1st or 5th) MUA +/- POP
Metacarpal fracture (not 1st or 5th) ORIF
Phalangeal fracture non-op
Phalangeal fracture MUA & percutaneous wires
Phalangeal fracture MUA +/- POP
Phalangeal fracture ORIF
9) Tendon repair: Tendon repair extensor
Tendon repair flexor
MCPJ fracture / dislocation:
MCPJ fracture / dislocation MUA & Percutaneous wires
MCPJ fracture / dislocation MUA +/- POP
1D Lower Limb 1) Hip joint
1a) Dislocated hip: Dislocated hip closed reduction
Acute dislocated hip open reduction +/- fixation
Neglected dislocated hip open reduction +/- fixation
1b) Extracapsular
fracture:
Extracapsular fracture CHS / DHS
Extracapsular fracture intramedullary fixation
Extracapsular fracture other fixation
Intracapsular fracture:
Intracapsular fracture hemiarthroplasty
Intracapsular fracture internal fixation
Intracapsular fracture intracapsular fracture THR 2) Femur
2a) Diaphyseal
fracture closed:
Diaphyseal fracture traction or spica in child
Diaphyseal fracture intramedullary nailing
Diaphyseal fracture plate/screw fixation
Fasciotomy for compartment syndrome
2b) Subtrochanteric
fracture:
Subtrochanteric fracture intramedullary fixation
Subtrochanteric fracture plate/screw fixation
2c) Supracondylar
fracture (not intraarticular):
Supracondylar fracture (not intraarticular) DCS / blade plate etc
Supracondylar fracture (not intraarticular)
intramedullary fixation 3) Knee Joint
Acute haemarthrosis arthroscopy
Acute ligament repair
Intraarticular fracture distal femur ORIF
Patella dislocation closed reduction +/- open repair
Patella fracture ORIF
Patella tendon repair
Quadriceps tendon repair
Simple tibial plateau fracture
Complex tibial plateau fracture
Tibial plateau fracture arthroscopically assisted fixation
Tibial plateau fracture ORIF with plates & screws
4) Tibia & Fibula
Diaphyseal tibial fracture external fixation
(including frame)
Diaphyseal tibial fracture intramedullary nailing
Diaphyseal tibial fracture MUA & POP
Tibial shaft plating
Fasciotomy for compartment syndrome
Tibial
non-union:
Tibial non-union circular frame management
Tibial non-union intramedullary nailing +/- bone grafting
5)
Ankle
Ankle fracture / dislocation:
Ankle fracture / dislocation MUA & POP
Ankle fracture / dislocation ORIF Pilon fracture: Simple pilon fracture ORIF
Complex pilon fracture ORIF
Pilon fracture with circular frame
Tendoachilles repair
6) Foot
Amputation toe / ray for trauma
Simple calcaneal fracture ORIF
Complex calcaneal fracture ORIF
Metatarsal fracture ORIF
Phalangeal fracture MUA +/- K wire +/- ORIF
Talar, subtalar or midtarsal fracture / disloc:
Talar, subtalar or midtarsal fracture / dislocation MUA +/-POP +/- K wires
Talar, subtalar or midtarsal fracture / dislocation ORIF
Achilles Tendon Repair 2. ELECTIVE (NON TRAUMA)
2A Non Specific Site
Aspiration / injection joint
Benign tumour excision (not exostoses)
Biopsy bone - needle
Biopsy bone - open
Bursa excision
Cyst bone curettage +/- bone graft
Epiphysiodesis
2B Axial Sceleton
1) Cervical Spine Anterior decompression +/- fixation / fusion (C2-C7)
Atlantoaxial fixation +/- fusion
Biopsy cervical spine
1) Cervical Spine
(cont)
Excision cervical / 1st rib
Nerve root / facet joint injection cervical spine
Occipito-cervical fusion +/- fixation
Posterior decompression +/- fixation / fusion (C20C7)
2) Thoracic Spine Anterior decompression +/- fixation / fusion
Biopsy thoracic spine
Posterior decompression +/- fixation / fusion
Scoliosis correction - anterior release +/- instrumentation
Scoliosis correction - posterior fusion +/- instrumentation
3) Lumbar Spine Caudal epidural injection
Decompression lumbar spine with fusion +/- fixation
Decompression lumbar spine without fusion (not disectomy alone)
Discectomy open / micro
Nerve root / facet joint injection lumbar spine
4) Pelvis Salter Innominate Osteotomy
Reconstruction Acetabulum
Excision Sacrum
5) Brachial Plexus Exploration / repair / grafting brachial plexus
Neurolysis 2C Upper Limb
1) Shoulder Acromioclavicular joint excison - arthroscopic / open
/ lateral clavicle
Acromioclavicular joint reconstruction (e.g. Weaver Dunn)
Acromioplasty open
Anterior repair for instability arthroscopic
Anterior repair for instability open including capsular shift
Arthroscopic subacromial decompression
Arthroscopy diagnostic
Rotator cuff repair (open or arthroscopic) +/- acromioplasty
2) Elbow Arthrolysis elbow (open/arthroscopic)
Arthroscopy elbow diagnostic
Arthoscopy elbow therapeutic
Arthrotomy elbow
Excision radial head +/- synovectomy
Radial head replacement
Tennis / golfer elbow release
Total elbow replacement
Ulnar nerve decompression / transposition
3) Wrist Arthrodesis wrist (includes partial arthrodesis)
Arthroscopy wrist
Carpal tunnel decompression
De Quervain's decompression
Excision distal ulna
Ganglion excision at wrist
Ulna shortening
Ulnar nerve decompression at wrist
4) Hand Dupuytrens contracture operation
Excision synovial cyst
Fusion of MCPJ or IPJ
MCPJ replacement
Soft tissue reconstruction hand
Tendon transfer hand
Trapezium excision or replacement
Trigger finger release
Trigger thumb release
2D Lower Limb
1) Hip Joint Arthrodesis hip
Arthrogram hip
Arthroscopy hip – diagnostic
Arthroscopy hip – therapeutic
Arthrotomy hip
Excision arthroplasty hip (e.g. Girdlestone)
Open reduction for DDH
Osteotomy hip – pelvic for DDH
Osteotomy hip – proximal femoral for DDH
Osteotomy pelvis – not for DDH Slipped upper
femoral epiphysis:
Slipped upper femoral epiphysis open reduction
Total Hip Replacement: THR cemented THR hybrid THR surface replacement THR uncemented
Revision THR acetabular component
Revision Total Hip Replacement
Revision THR both components
Revision THR femoral component
2) Femur Amputation above knee
Femoral lengthening
Osteotomy corrective (not for DDH)
3) Knee Joint Open ACL reconstruction
Injection & aspiration Joint
Arthroscopy ACL reconstruction
Arthroscopic lateral release
Arthroscopic partial meniscectomy
Arthroscopic removal loose bodies knee
Arthroscopic synovectomy
Arthroscopic knee diagnostic
Osteotomy distal femoral
Osteotomy proximal tibial
Patella realignment
Patella resurfacing alone
Revision TKR
TKR
Unicompartmental knee replacement
4) Tibia & Fibula Amputation below knee
Tibial lengthening
Harvesting Fibular Graft
5) Ankle Joint: Arthrodesis ankle
Arthroplasty ankle
Arthroscopy ankle diagnostic
Arthroscopy ankle therapeutic
Arthrotomy ankle
Decompression tendons at ankle
6) Foot Amputation toe / ray
Calcaneal osteotomy
CTEV correction
Fifth toe soft tissue correction
First metatarsal osteotomy
First MTPJ arthrodesis
First MTPJ excision arthroplasty
First MTPJ soft tissue correction
Hindfoot arthrodesis
Ingrowing toenail operation
Lesser metatarsal osteotomy
Lesser toe arthrodesis
Lesser toe excision part/all phalanx
Lesser toe tenotomy
Tendon decompression or repair
Tendon transfer foot
2.3.
Bidang Afektif (
Professional & Management and Good
Clinical Practice)
1. Professional Behaviour The Objective
1 To achieve an excellent level of care for the individual patient a. to elicit a relevant focused history
b. to perform focused, relevant and accurate clinical examination
c. to formulate a diagnostic and therapeutic plan for a patient based upon the clinic findings
d. to prioritise the diagnostic and therapeutic plan
e. to communicate a diagnostic and therapeutic plan appropriately
2 To produce timely, complete and legible clinical records to include case-note records, handover notes, and operation notes.
3 To prescribe, review and monitor appropriate therapeutic interventions relevant to clinical practice including non – medication based therapeutic and preventative indications.
4 To prioritise and organise clinical and clerical duties in order to optimise patient care.
5 To make appropriate clinical and clerical decisions in order to optimise the effectiveness of the clinical team resource.
6 To prioritise the patient’s agenda ncompassing their beliefs, concerns expectations and needs
7 To prioritise and maximise patient safety. 8 To understand that patient safety depends on;
a. The effective and efficient organization of care b. Health care staff working well together
c. Safe systems, individual competency and safe practice
9 To understand the risks of treatments and to discuss these honestly and openly with patients
10 To systematic ways of assessing and minimizing risk
11 To ensure that all staff are aware of risks and work together to minimise risk 12 To manage and control infection in patients, Including;
a. Controlling the risk of cross-infection
b. Appropriately managing infection in individual patients
c. Working appropriately within the wider community to manage the risk posed by communicable diseases
Examples and Descriptors Patient assessment
a. Introducing self clearly to patients and indicates own place in team b. Checks that patients comfortable and willing to be seen
c. Informs patients about elements of examination and any procedures that the patient will undergo