VoI9, No 3, July
-
September 2000 Resistance pattern of M.tuberculosis
153Resistance
pattern
of
Mycobacterium tuberculosis to
fÏrst-line
antituberculosis drugs
Tjahjani
Mirawati
Sudiro,
Amin
Soebandrio, Prawoto,Pratiwi
SudarmonoAbstrak
Dalam laporan
ini
kami menganalisispoln
resistensiM.
tuberculosis yang diisol.asidi
laboratorium Mikrobiologi Fakultas Kedokteran Universitas Indonesia selama tahun 1996-1998 dan membandingkannya dengan data tahun 1995 dari laboratorium kami yang telah dipublikasi. Selama tahun 1996, 1997,dan
1998 tetah diperiksa masing-masing 2360, 2468 dan 1849 spesimen. Dari-rp"ii^"n
teriebut, dengan menggunakan medium liwenstein-Jensen berturut-turut ditemukan 164 (6,9Vo),
I8I
(7,37o)' dan 214 (tt,OE") biakan positif-M. tubeiiutosis pada tahun 1996, 1997dan
1998. Dibandinglcan dengan laporan tahun sebelumnya dari laboratorium knmi oleh Wahid dkk., terlihat adanya fluktuasi tingkat resistensi terhadap satu atau lebih obat antituberkulosis utama (streptomisin, INH, etambutoL, dan rifampisin)dari
15,97o pada tahun 1995,1 7,97o pada tahun 1996, I2,7Vo pada tahun 1997 dan 8,4%padatahunlggS.Jugaterlihatpolnresistensiyangberbedaselama4tahunterakhirini. Padatahunl995-l99Tresistensiyang tertin'ggi adalah terhadap rifampisin, yaitu berturut-turut 14,0Vo, 7,9Vo, dan 9,4Vo pada tahun 1995, 1996 dan 1997, sedangkan padn tahun 1998 resistensi terhadap INH adalah yang lertinggi (4,7Vo). Resistensi terhadap etambutol tidak ditemukan pada tahun 1996 dan 1997, tetapi ditemuknn pada2
isolat pada tahun 1998. Selama tahun 1996 dan1997
tidak ditemukan isolat )'ang resistenterhadap tiga atau lebih obat antituberkulosis (OAT). Pada tahun 1998 ditemukan
I
isolat yang resisten terhadap streptomisin, etambuiolian
INH. Selama tahun 1996-1998 tidak ditemukan isolat M.tuberculosis yang resisten terhadap keempat OAT yang diuii.Abstract
In
this report we analyzed the resistance pattems of M. tuberculosis isolated in our laboratory from 1996to
1998 and compared themwith pubiished data of the year 1995 from our laboratory. In our laboratory, 2360, 2468 and 1849 specimens were examined in 1996'
1997 and 1998, respectively. From these specimens, using Lôwenstein-Jensenmedia, 164 (6.9Eù, 181 (7.3Eù
and2l4
(l1.6Vo)were found positivefor
M. tuberculosisin
1996, 1997, 1998 respectively. Compared with the earlier published reports from our laboratory, we found a fluctuationof
the resistance rate to oneor
morefirst
line antituberculosis drugs (streptomycin, INH, ethambutol, and rifampicin)from
15.9Voin 1995,t 7.9%
in
1996, I2.7Vo in 1997 anà 8.4%in
1998. We also found dffirent pattems of resistance in the Iast 4 years.During
1995 to 1997 the highest rate of resistance was to rifampicin, i.e. l4.0Vo, 7.9Vo, and 9.4Voin 1995,
1996 and in 1997 respectively; whilein
1998 the resistance to INH was the highest (4.7qd. Resistance to ethambutol was not found in 1996 and 1997, butit was
foundin 2
isolates in 1998. Resistance to threeor
more drugs was not foundin
1996 and 1997, Resistance to streptomycin, ethnmbutol and INH was found in one isolatein
1998. Resistance to four antitubercuLosis drugs was not found in 1996to
1998.Keyw o rds : S t rep t omy cin, I N H, e t hamtu b o L, rifamp ic in
drugs available
arelimited, routine monitoring of
theMDR-TB
is very important. Wahid et al have reportedthat
M.
tuberculosis isolated
in
our laboratory
in
1995 showedoverall
resistanceof
15.6Vo, and 5.l%o showed resistanceto the 4
first-line
drugs.l Here we report
anevaluation
of
routine susceptibility testing
of
M.
tuberculosis isolated
from clinical
specimens sent to
the laboratory
of
the Department
of
Microbiology,
Faculty
of
Medicine,
University
of
Indonesia in
Jakarta
from
1996 to 1998 and compared
its
resultswith
the
data published
in
1995
from the
samelaboratory.
Tuberculosis
(TB) is still
an
important public
healthproblem
in
Indonesia and
all
over the
world.
In
1996, 3.8million
casesof TB
have been reportedto WHO.2
Recently the problem
of
tuberéulosis have been
re-increasing due
to
the
increase
of
Human
Immuno-deficiency
Virus (HIV)
infections
and
multi-drug
resistant
TB
(MDR-TB). Since the
antituberculosisDepartment of Microbiology, Faculty of Medicine, University
154
Sudiro et alMETHODS
Samples
Retrospective analysis was done
on
the
data,dealing
with
thesusceptibility
of M.
tuberculosis
againstanti-TB,
obtained
fiom
various
clinical
specimens sent toour
laboratory
by
clinicians throughout
Jakarta.
All
specimens came
from
suspectedtuberculosis
patients,and
mainly
consisted
of
sputum,
but
there were
alsopleural effusion, bronchial
washing,
pus, urine,
andbody tluid/ascites.
The
sputum collected were
themorning
sputum takenin
three consecutive days.Isolation
of
M. tuberculosk
The
samples
were
first
decontaminated
andhomogenized
using
sodium hydroxide
at
a
final
concentration
of
2Vo.
Sampleswere inoculated
ontoLôwenstein-Jensen
medium, incubated
at
37oC
andobserved
twice
a
week
for
6
to
8
weeks for
mycobacterial growth.
Drug susceptibility
test
The proportional method
by
comparing the
isolateswith the
intemational standard strain
of
M.
tuberculosis
H37Rv waq
used
to
detect
drugresistance.
The
concentrations
of
the
drugs
testedwere respectively
as
followed: streptomycin
(1;
l0;
and
100
pglml),
isoniazid
(INH)
(0.1;
I
and
l0
pg/ml),
ethambutol
(1;
10
and
100
pg/ml),
andrifampicin (2.5:5
and20 ttg/nù).
RESULTS
We
examined
a
number
of
2360,
2468
and
1849specimens
collected
from
suspectedTB
patients
in
1996,
1997,
and
1998 respectively
(Table 1).
From
those
samplescollected
in
1996, 1997, and
1998 wefound
164 (6.9Vo),l8l
(7.3Vo), and 214(lI.6Vo)
were
culture-positive
for M.
tuberculosis
respectively. Thosepositive
clinical
specimenswere
obtainedfrom
Med J Indones
sputum,
pleural
fluid,
bronchial
washing,
pus,
body
fluid/ascites,
cerebrospinalfluid
and exudates.Table
1.
Specimens collected from suspected TB patients from 1996 to 1998Specimen 1996 1997
Sputum Pleural fluid Bronchial washing Pus
Others
1985 108
79
55 133
1985
137
102 70 174
1446
130
92 59 t22
Total 2360 I 849
In
1996,
13out
of
164isolates
(7.9Vo)were
found
tobe
resistant
to
rifampicin,
and
no
MDR-TB
wasdetected.
In
1997,
from
181 isolates
we
found
2(l.lVo)
resistantto
streptomycin,
4
(2.2Vo) resistant toINH,
13
(7.2Vo)resistant
to rifampicin,
I
resistant
tostreptomycin and
rifampicin, and 3
resistant
to
INH
and rifampicin.
In
1998
from
214
isolates,
196(9l.6Vo) were
sensitive
to
the
four
firstline
drugs.From
l8
(8.4Vo) resistant isolateswe found 2
isolates were resistantto
streptomycin,8
isolates \ryere resistant toINH,
5 isolates were resistant torifampicin,
I
isolatewas reslstant
to
streptomycin and
INH,
and
1
isolatewas
resistant
to
streptomycin and ethambutol.
We
found
I
isolate
was
resistant
to 3
drugs,
i.e.streptomycin, ethambutol,
andINH.
Isolates resistant tofour
drugs were notfound (Table
2).Regarding
the
resistance
to
each drug,
in
1996
we
found drug
resistance
of M.
tuberculosis
only
torifampicin,
i.e.
13
(7.9Vo)isolates.
In
1997,3
(1.77o) isolateswere
fôund to
be resistant
to
streptomycin,
7(3.9Vo)
isolates were
resistant
to
isoniazid,
and 17
(9.4%o),isolateswere resistant
to rifampicin.
In
1998,l0
isolates
(4.77oof
total
isolates)
were
resistant
toisoniazid,
5
(2.3Vo)
isolates
were resistant
tostreptomycin,
5
(2.3Vo) isolates
were
resistant
torifampicin, and
2
(O.9Vo)isolates were
resistant
toVol 9, No
j,
July-
September2000
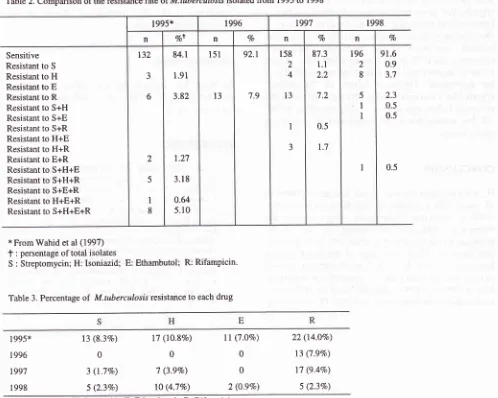
Resistance pattern of M. tuberculosisTable 2. Comparison of the resistance ftte of M.tuberculosis isolated from 1995 to 1998
155
1995* 1996 t99'l r998
n Vo+ n Vo n Vo n %
Sensitive
Resistant to S
Resistant to H
Resistant to E
Resistant to R
Resistant to S+H
Resistant to S+E
Resistant to S+R
Resistant to H+E
Resistant to H+R
Resistant to E+R
Resistant to S+H+E
Resistant to S+H+R
Resistant to S+E+R
Resistant to H+E+R
Resistant to S+H+E+R
132 J 6 1 5
I
8 84.1 1.91 3.82 1.27 3.18 0.64 5.10l5l
l3
92.1 7.9 158 2 4 13I
3 87.3 1.1 2.2 7.2 0.5 1.7 196 2 8 5I
I
I
91.6 0.9 3.7 2.3 0.5 0.5 0.5* From Wahid et al (1997)
f
: persentage oftotal isolatesS : Streptomycin; H: Isoniazid; E: Ethambutol; R: Rifampicin'
Table 3. Percentage
of
M.tuberculosis resistance to each drug1995*
1996
1997
I 998
13 (8.3Vo)
0 3 (1.7%)
5 (2.3Vo)
17
(lO.87o)
ll
(1.OVo)00
7
(3.9Vo)
0 t0(4.7Vo)
2 (0.9%\22 (l4.OVo)
13 (7.9Vo)
17 (9.47o)
5 (2.3Vo) S: Streptomycin; H: Isoniazid; E: Ethambutol; R: Rifampicin'
*From Wahid et al (1997)
DISCUSSION
Resistance
of
M.
tuberculosis
to
antituberculosisdrugs has been reported
worldwide.
Comparing our
report
herewith
the earlier published report
from
our
laboratory, we found a fluctuation
of
the
resistancerate
to
1 or
more drugs (streptomycin,
isoniazid,
rifampicin, and ethambutol),
which was
l5.9Vo
in
t995,t
7.9Eoin
1996,
12.77oin
1997
and 8.47o in
1998 respectively (Table
2). The
susceptibility
topyrazinamide
was not tested. We also founddifferent
pattems
of
resistance
in
the last
4
years. While in
1995, 1996, and
1997
the
highest
rate
of
resistancewas
to
rifampicin,
i.e.
l4.0Vo, 7.9Vo,
and
9.4Vorespectively;
in
1998,
resistance
to
INH
was
thehighest
(4.77o)
(Table 3).
Resistanceto
ethambutol,which
was notfound in
1996
aîd
1997, wasfound in
1998in
2
idôlates. Resistanceto
three
or
more
drugswas
not found
in 1996
and
1997,
but found
in
oneisolate
in 1998. In 1995,
the
presence of
8
isolatesresistant
to 4
drugs had been reported,
but we
could
notfind it in
1996to
1998.Compared
to
reports
from
other investigators,
theresistance
rate
of M.
tuberculosis reported here
is considered to berelatively low.
For example, Aditama
et
al
reported
a
resistance
rate
of
29.63Voin
casesobtained
from
Jakarta in
1994;3and a resistance rate
of
33Vo had been reportedin New York city in
1991.4 [image:3.595.76.574.88.486.2]156
Sudiro et alwith
positive
M.
tubercalosis
culture.
It
has
been reported that caseswith
secondarytuberculosis
have ahigher
rateof
resistance comparedto primary
cases.3'4Our
laboratory
doesnot
attachdirectly to
aparticular
hospital,
and most
of
the
specimens
came from
outpatient
cases.Thus,
the data onMDR-TB
coilectedin
our laboratory may not reflect
thereal
MDR-TB
inthe
population. Treatment
failure
of
TB
patientsreported
by clinicians is relatively high,
although
the reasonof failure
maynot
necessarily causedby
MDR-TB, but mainly
due
to the
compliance
of
patients
intaking
drugs.CONCLUSION
Here we reported our
data on the resistance patternof
M.
tuberculosis isolated
in
our
laboratory
in
1995-1998
to
isoniazid, ethambutol, streptomycin,
andrifampicin.
Although
the
resistance
rate
of
M.tuberculosis
in
our report is relatively low,
it
showsthat there
is
indeed,
a
change
of
resistance
patternfrom
year
to
year.
Resistanceto
ethambutol,
aswell
as resistanceto
more thantwo
drugs that wecould
notfind
in
1996and
1997,could
befound
in
1998. These results shows theimportance
of MDR-TB
monitoring,
Med J lndones
and also
suggests
that
multidrug
rherapy
is
still
considered
to
be the
method
of
choice
in
the managementof
tuberculosis.Acknowledgement
thank Ms. Anissah-for her technical
assistanceProf. Sardjito
fbr
his
critics and
suggestions
on manuscnpt.REFERENCES
l.
Wahid
MH,
HarunBH,
KiranasariA.
Pemeriksaanrnikrobiologik
dan
pola
resistensi
Mycobacterium tuberculosis di Bagian Mikrobiologi Fakultas Kedokteran Universitas Indonesia selamatahun
1995.
Majalah Kedokteran lndonesia 1997 :4'7 :624-'1 .Castro K. Global tuberculosis challenges. Emer-qing Intèc Dis 1998;4:408-9.
Aditama T, Wijanarko P. Resistensi primer dan sekunder
Mycobacteriurn tuberculosis di RSUP Persahabatan tahun 1994. J Respir lndones 1996:16:12-4.
Frieden
T,
SterlingT,
Pablos-MendezA,
Kilbum
J,Cauthen G, Dooley S. The emergence
of
drug-resistant tuberculosisin
NewYork city.
N
En-elJ
lr{ed
1993; 328:521-6.We
and this