EPIGASTRIC PAIN SYNDROME IS AN INDICATOR OF
ACTIVE GASTRITIS
Gontar Alamsyah Siregar, Sahat Halim, Galdy Wafie
Division of Gastroentero-Hepatology, Department of Internal Medicine, Faculty of Medicine, University of Sumatera Utara/ Adam Malik Hospital, Medan, Indonesia
Abstract
Objective. Dyspepsia become one of major health problems. It causes morbidity, social problems, and economic burden. This study is about to know correlation between dyspepsia and gastritis histopathologically.
Methods. A retrospective descriptive analysis in 2013 to patients with dyspepsia who were under treatment in 2009-2012, and fulfilledthe Rome III criteria
Results. Epigastric pain is the most common symptom in dyspepsia patients. There is a correlation between epigastric pain syndrome and neutrophil infiltration (p-value 0,042). There are significant positive correlations between degree of epigastric pain with chronic inflammation (r=0,396, p-value 0,008) and neutrophil infiltration (r=0,415, p-value 0,005). There are significant negative correlations between degree of nausea and vomit with degree of chronic inflammation (r= -0,371, p= 0,013) and degree of neutrophil infiltration (r= -0,359, p= 0,017), and also between degree of abdominal bloating with degree of chronic inflammation (r= -0,416, p= 0,005) and degree of neutrophil infiltration (r= -0,436, p= 0,003).
. Simple random sampling was done to get 44 patients with dyspepsia, 22 are H.pylori positive and 22 patients are H.pylori negative. The severity of chronic inflammation, neutrophil infiltration, glandular atrophy, intestinal metaplasia were assessed. Univariate and bivariate analysis (chi square, fisher's exact, and Spearman correlation test) were done using SPSS version 22.
Conclusion. Epigastric pain syndrome may be useful as an indicator of active gastritis, with marked neutrophil infiltration.
Keywords. Epigastric pain, active gastritis, neutrophil
Tujuan. Dispepsia menjadi salah satu masalah kesehatan utama, menimbulkan morbiditas, masalah sosial, dan beban ekonomi. Tujuan penelitian ini untuk mengetahui hubungan gejala dispepsia dengan histopatologi gastritis.
Metode. Penelitian deskriptif analitik secara retrospektif pada tahun 2013 terhadap pasien dispepsia yang berobat pada tahun 2009-2012, yang memenuhi kriteria Rome III. Dilakukan Simple Random Sampling untuk mendapatkan 44 pasien dispepsia yang terdiri dari 22 orang dengan H.pylori positif dan 22 orang dengan H.pylori negatif. Dinilai derajat inflamasi kronik, derajat infiltrasi neutrofil, derajat atrofi, dan derajat metaplasia intestinal. Dianalisis secara univariat dan bivariat (uji chi square, fisher exact, dan korelasi Spearman) dengan SPSS versi 22.
Hasil. Nyeri epigastrium merupakan gejala terbanyak yang dialami pasien dispepsia. Terdapat hubungan antara epigastric pain syndrome dengan infiltrasi neutrofil (p-value 0,042). Terdapat korelasi positif yang signifikan antara derajat nyeri epigastrium dengan derajat inflamasi kronik (r= 0,396, p= 0,008) dan derajat infiltrasi neutrofil (r= 0,415, p= 0,005). Terdapat korelasi negatif yang signifikan antara derajat mual muntah dengan derajat inflamasi kronik (r= -0,371, p= 0,013), dan derajat infiltrasi neutrofil (r= -0,359, p= 0,017), serta derajat perut kembung dengan derajat inflamasi kronik (r= -0,416, p= 0,005) dan derajat infiltrasi neutrofil (r= -0,436, p= 0,003).
Kesimpulan. Epigastric pain syndrome menjadi petunjuk gastritis aktif yang ditandai adanya infiltrasi neutrofil.
Kata kunci. Nyeri epigastrium, gastritis aktif, neutrofil
Introduction
In the western countries, approximately 60% of total cases are dyspepsia cases.3 In Indonesia, there are approximately 30% cases found in general practice and 60% cases in specialized practice.4 According to Indonesian Health Profile Data 2007, dyspepsia is ranked the 10th of the diseases found in the inpatient clinic in 2006.5
Dyspepsia is considered more as a syndrome instead of a diagnosis, whereas gastritis is a diagnosis established based on the histology findings. Gastritis involves inflammation process in the mucosal and submucosal membrane of the stomach as a response to acute and chronic injury.
6
In this study, we aim at investigating the correlation between dyspepsia and histopathology of gastritis, which is considered as a diagnosis.
Patients and Methods
The present study was a retrospective descriptive analysis in 2013 to patients with dyspepsia who were under treatment in Permata Bunda Hospital, Medan, Indonesia, from 2009-2012. A simple random sampling was carried out, and 44 dyspeptic subjects were obtained, consisted of 22 H. pylori positive subjects and 22 H. pylori negative subjects. H. pylori was considered positive from positive results of campylobacter like organism (CLO) test.
Inclusion criteria included all adult dyspeptic patients older than 18 years old that fell into one of the Rome III criteria, i.e., postprandial fullness, early satiation, epigastric pain, and epigastric burning. The symptoms persisted at least for the last 3 months and the onset of the symptom was at least 6 months before the diagnosis. Exclusion criteria included those with gastric malignancy and history of gastric surgery with partial removal of gastric mucosa (partial gastrectomy).
Gastritis degree was evaluated from biopsy of the mucosa of gastric antrum and body. The samples were stained using Hematoxylin-Eosin and were evaluated by the pathologist of anatomic pathology of the medical faculty of Sumatra Utara University referring to visual analogue scale of the updated Sydney System. The higher degree was used if differences of degree were found between the body and antrum. All specimens were analyzed by the same pathologist. The degree of chronic inflammation, neutrophil infiltration activity, glandular atrophy, and intestinal metaplasia were scored 0 to 3, i.e., normal (0), mild (1), moderate (2), and severe (3).
SPSS version 22 (SPSS Inc., Chicago) was used for the analysis. The data were analyzed using univariate and bivariate analysis with 95% confidence interval. Bivariate analysis was carried out using fisher’s exact test, chi-square, and Spearman correlation with a significance level set at p< 0.05.
Results
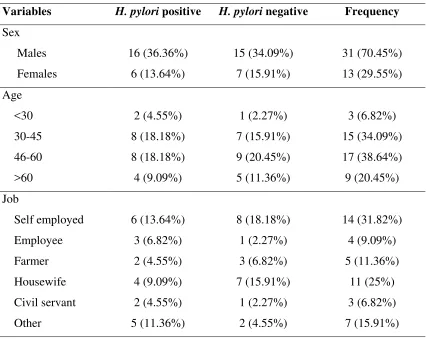
Table 1. Characteristics of the subjects
Variables H. pylori positive H. pylori negative Frequency
Nutrition status Normal
Underweight and Overweight
14 (31.82%) 8 (18.18%)
18 (40.91%) 4 (9.09%)
32 (72.73%) 12 (27.27%)
Total 22 (50%) 22 (50%) 44 (100%)
There were 44 subjects, consisted of 31 males (70.45%) and 13 females (29.55%). Mean age was 49 years, with 19 years being the youngest and 74 years being the oldest. The highest number of age group was from the age group of 46-60 and 30-45. Male to female ratio in the H. pylori positive group was 2.67:1, while that in the H. pylori negative group was 2.14:1. The majority of subject`s employment status was self-employed (31.82%) and housewife (25%). The majority of the subjects had a normal nutrition status (32 subjects, 72.73%).
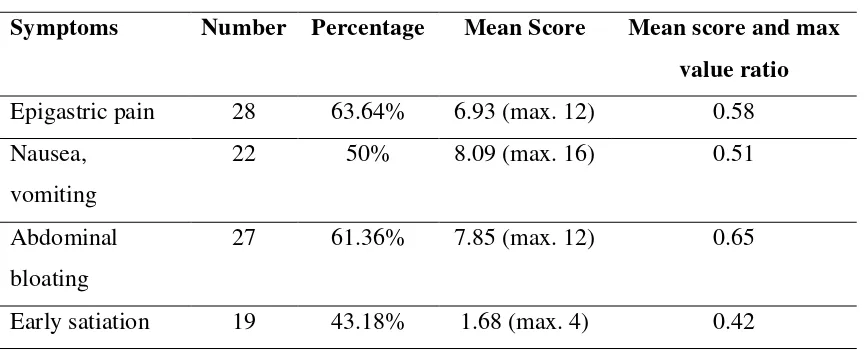
Table 2. Clinical manifestation of dyspepsia according to PADYQ
Symptoms Number Percentage Mean Score Mean score and max value ratio Epigastric pain 28 63.64% 6.93 (max. 12) 0.58 Nausea,
vomiting
22 50% 8.09 (max. 16) 0.51
Abdominal bloating
27 61.36% 7.85 (max. 12) 0.65
Early satiation 19 43.18% 1.68 (max. 4) 0.42
It is shown in Table 2 that the main symptoms of dyspeptic patients were epigastric pain and abdominal bloating, 63.64% and 61.36%, respectively. 50% of subjects experienced nausea and vomiting, while 43.18% had early satiation.
Table 3. Classification of dyspeptic symptoms
Symptoms Number Percentage
Postprandial distress syndrome (PDS) 15 34.09%
Combined type 12 27.27%
EPS was the majority of the symptoms (38.64%), followed by PDS (34.09%) and combined type (27.27%).
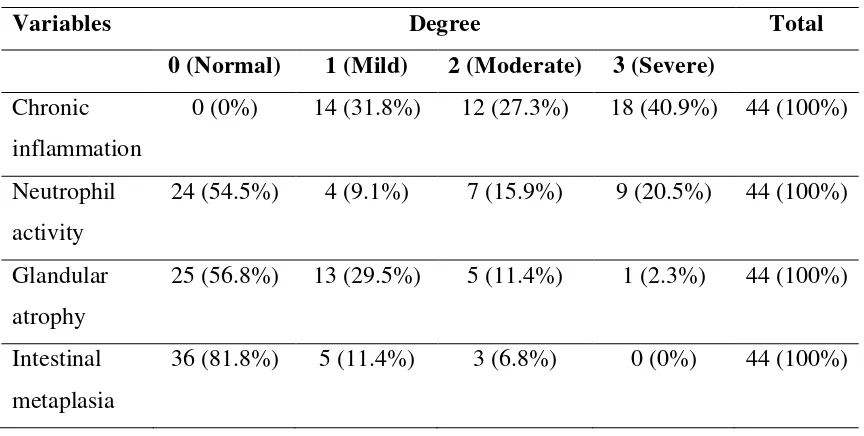
Table 4. Gastritis histopathology
Variables Degree Total
0 (Normal) 1 (Mild) 2 (Moderate) 3 (Severe) Chronic
inflammation
0 (0%) 14 (31.8%) 12 (27.3%) 18 (40.9%) 44 (100%)
Neutrophil activity
24 (54.5%) 4 (9.1%) 7 (15.9%) 9 (20.5%) 44 (100%)
Glandular atrophy
25 (56.8%) 13 (29.5%) 5 (11.4%) 1 (2.3%) 44 (100%)
Intestinal metaplasia
36 (81.8%) 5 (11.4%) 3 (6.8%) 0 (0%) 44 (100%)
Among 44 specimens with chronic inflammation, most of them had severe inflammation (40.9%), followed by mild inflammation (31.8%) and moderate inflammation (27.3%). Among 45.5% of specimens with neutrophil infiltration, those with severe, moderate and mild degree of neutrophil infiltration were 20.5%, 15.9%, and 9.1%, respectively. Among 43.2% of specimens with glandular atrophy, those with mild, moderate and severe degree were 29.5%, 11.4%, and 2.3%, respectively. Whereas among 18.2% of specimens with intestinal metaplasia, mild and moderate degree were found in 11.4% and 6.8%, respectively.
Table 5. Correlation of the type of dyspepsia with chronic inflammation and neutrophil infiltration
Symptoms Chronic Inflammation Neutrophil Infiltration
Yes No p Yes No p
Yes
A significant correlation was found between EPS and neutrophil infiltration (p= 0.042), however PDS and combined type did not show any significant correlation with neutrophil infiltration (p >0.05).
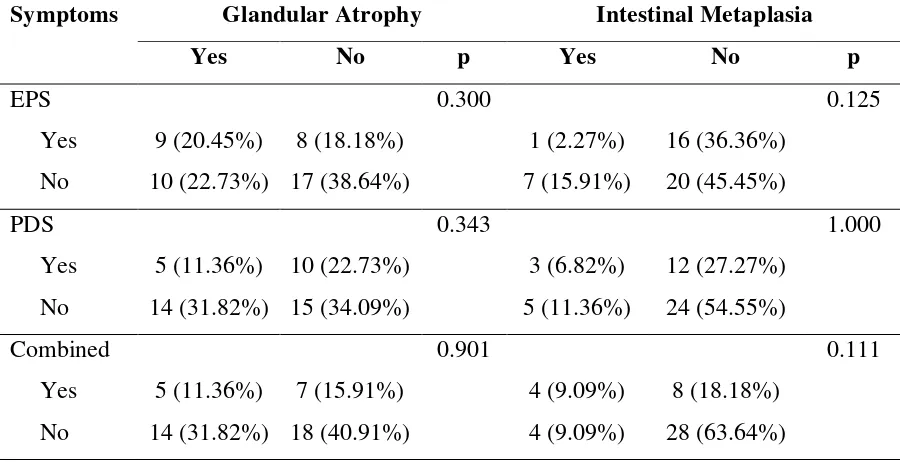
Table 6. Correlation of the type of dyspepsia with glandular atrophy and
intestinal metaplasia
Symptoms Glandular Atrophy Intestinal Metaplasia
Yes No p Yes No p
No significant correlations were found among EPS, PDS, and combined type with glandular atrophy and intestinal metaplasia (p> 0.05).
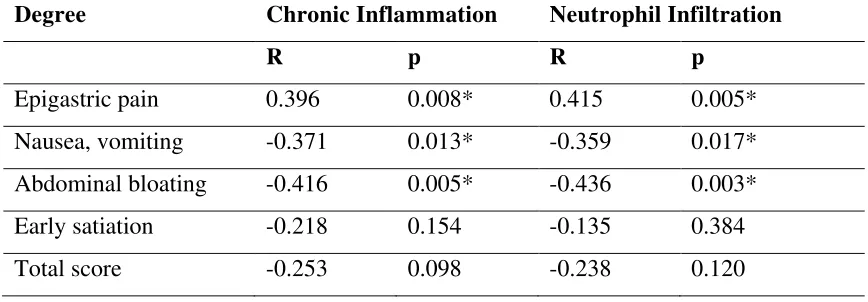
Table 7. Correlation of dyspepsia score with chronic inflammation degree and neutrophil infiltration
Degree Chronic Inflammation Neutrophil Infiltration
R p R p
Epigastric pain 0.396 0.008* 0.415 0.005* Nausea, vomiting -0.371 0.013* -0.359 0.017* Abdominal bloating -0.416 0.005* -0.436 0.003* Early satiation -0.218 0.154 -0.135 0.384
Total score -0.253 0.098 -0.238 0.120
*p-value < 0.05
The degree of epigastric pain was positively correlated with the degree of chronic inflammation (r= 0.396, p= 0.008) and the degree of neutrophil infiltration (r= 0.415, p= 0.005). The degree of nausea and vomiting was negatively correlated with the degree of chronic inflammation (r= -0.371, p= 0.013) and the degree of neutrophil infiltration (r= -0.359, p= 0.017). In addition, the degree of abdominal bloating was negatively correlated with the degree of chronic inflammation (r= -0.416, p= 0.005) and neutrophil infiltration (r= -0.436, p= 0.003).
Discussion
Mean age of dyspeptic subjects in this study was 49 years, which is considered a productive age group. In addition, the age groups with the most group experiencing dyspepsia were those in the age group of 46-60 and 30-45. This result is in accordance with the results from the previous studies such as that by Garg B, et al., which reported the mean age of dyspeptic patients was 47 years and the study by Mustapha SK, et al., which reported a mean age of 47.2 years.
Majority of the subjects in this study was male (70.45%), with a male to female ratio of 2.3:1. This result is in accordance with the previous studies which also suggested more male subjects than females. Shrivastava UK, et al., reported a male to female ratio of 1.8:1.
8, 9
10
This study demonstrated that epigastric pain was the most symptom experienced by dyspeptic subjects, followed by abdominal bloating. This result is in agreement with the study of dyspeptic patients in Jamaica conducted by Lee M, et el., which suggested that epigastric pain was the most symptom experienced by 76% of subjects, while abdominal bloating, nausea, vomiting and early satiation were found less.
EPS was found the highest in 38,6% of subjects, followed by PDS (34.1%) and combined type (27.3%). On the other hand, Saruc M, et al., reported that EPS was the highest (35.6%), followed by combined type (33.1%) and PDS (31.2%).
12
All subjects experienced chronic inflammation, while neutrophil infiltration, glandular atrophy and intestinal metaplasia were found in 45.5%, 43.2%, and 18.2%, respectively. Results were varied among studies. Garg B, et al., reported chronic inflammation 100%, neutrophil infiltration in 33.33%, glandular atrophy in 12.33%, and intestinal metaplasia in 7%,
13
8
while Darya, et al., reported chronic inflammation in 100%, neutrophil infiltration in 22.8%, glandular atrophy in 37.5%, and intestinal metaplasia in 6.2%.11 Zhang C, et al., reported chronic inflammation in 90.3%, neutrophil infiltration in 56.2%, glandular atrophy in 36.8%, and intestinal metaplasia in 37%.14 In addition, Hashemi MR, et al., investigated gastric histopathology and found active chronic gastritis in 47.1%, atrophic changes in 25%, and intestinal metaplasia in 8.9%.
A positive correlation was found between epigastric pain and the degree of chronic inflammation (r= 0.396, p= 0.008). This result is in accordance with the study of Saruc M, et al., suggesting that chronic inflammation was more severe in dyspeptic subjects with pain-dominant symptom (p< 0.05).
15
In addition, a positive correlation was found between the degree of epigastric pain and the degree of neutrophil infiltration (r= 0.415, p= 0.005). A significant association was also found between the type of epigastric pain syndrome and neutrophil infiltration (p= 0.042). This is in agreement with the result of Saruc M, et al., which suggested that neutrophil infiltration was significantly higher in EPS type dyspepsia than PDS (p< 0.05).
13
Neutrophil infiltration to gastric mucosa suggests an active gastritis. H. pylori
has been suggested as the primary etiology of chronic gastritis. It has also been reported in several studies that H. pylori is correlated with EPS. Perri F et al., reported that EPS type dyspeptic patients significantly had more H. pylori infection compared to PDS type (p= 0.026).16 A similar result has also been suggested by Saruc M, et al., in which H. pylori infection was found more often in EPS than PDS (p= 0.01).
The degree of nausea and vomiting was negatively correlated with the degree of chronic inflammation (r = -0.371, p= 0.013) and the degree of neutrophil infiltration (r= -0.359, p= 0.017), while the degree of abdominal bloating was negatively correlated with the degree of chronic inflammation (r= -0.416, p= 0.005) and the degree of neutrophil infiltration (r= -0.436, p= 0.003). H. pylori increases the release of IL-8 which induces chemotaxis of neutrophil and lymphocyte. More severe degree of chronic inflammation, particularly that in association with neutrophil infiltration, is correlated with H. pylori. This is in accordance with the previous study by Siregar GA, in which patients with nausea, vomiting, and abdominal bloating were negatively correlated with H. pylori infection.
13
Conclusion
Epigastric pain syndrome was correlated with neutrophil infiltration (p= 0.042), and the degree of epigastric pain was positively correlated with the degree of chronic inflammation and neutrophil infiltration. Epigastric pain syndrome may be useful as an indicator of active gastritis.
Acknowledgements
We would like to express our gratitude to Lidya Imelda Laksmi who has conducted the histopathological analysis in this study, as well as to Khaerani and Sulasmi who have assisted the endoscopy procedure in all patients.
References
2. Arruda SMB, Forones NM, Juca NT, et al. Could gastric histology be a useful marker for making decision on Helicobacter pylori eradication therapy in patients with dyspepsia? Arq Gastroenterol. 2009;46:209-13.
3. Nwokediuko S, Okafor O. Gastric mucosa in nonulcer dyspepsia: a histopathological study of Nigerian patients
4. Djojoningrat D. Dispepsia fungsional. In: Sudoyo AW, ed. Buku ajar Ilmu Penyakit Dalam. Jilid I edisi IV. Jakarta: BP FKUI; 2006. p. 354-6.
. Internet J Gastroenterol. 2006;5(2). http://www.ispub.com (accessed 10 May 2013)
5. Depkes RI. Profil Kesehatan Indonesia. Jakarta: Departemen Kesehatan Republik Indonesia; 2008. p. 28.
6. El-Zimaity HM. Recent advances in the histopathology of gastritis. Current Diag Pathol. 2007;13:340-8.
7. Ang D, Talley NJ, Simren M, et al. Endpoints used in functional dyspepsia.
Aliment Pharmacol Ther. 2011;33:1-61.
8. Garg B, Sandhu V, Sood N, et al. Histopathological analysis of chronic gastritis and correlation of pathological features with each other and with endoscopic findings. Pol J Pathol. 2012;3:172-8.
9. Mustapha SK, Bolori MT, Ajayi N, et al. Endoscopic findings and the frequency of Helicobacter pylori among dyspeptic patients in North-Eastern Nigeria. Internet J Gastroenterol. 2006; 6(1). http://www.ispub.com (accessed 10 May 2013)
10.Shrivastava UK, Gupta A, Gupta A, et al. Role of Helicobacter pylori in functional dyspepsia. Indian J Surg. 2004; 66:341-6.
11.Darya IW, Wibawa IDN. Korelasi antara derajat gastritis dan rasio pepsinogen I/II pada penderita gastritis kronis. J Peny Dalam. 2009;10:85-98.
12.Lee M, Emery H, Whittle D, et al. Helicobacter pylori infection in patients with functional dyspepsia in Jamaica. Internet J Trop Med. 2008;5(2). http:// www.ispub.com (accessed 10 May 2013)
14.Zhang C, Yamada N, Wu Y, et al. Helicobacter pylori infection, glandular atrophy and intestinal metaplasia in superficial gastritis, gastric erosion, erosive gastritis, gastric ulcer and early gastric cancer. World J Gastroenterol. 2005;11:791-6.
15.Hashemi MR, Rahnavardi M, Bikdeli B, et al. H. pylori infection among 1000 Southern Iranian dyspeptic patients. World J Gastroenterol. 2006;12:5479-82. 16.Perri F, Clemente R, Festa V, et al. Patterns of symptoms in functional
dyspepsia: role of Helicobacter pylori infection and delayed gastric emptying.