GERD-Q and Other Diagnostic Tools for GERD Diagnosis
Gontar Alamsyah SiregarProfessor, Division of Gastroentero-Hepatology, Department of Internal Medicine, Faculty of Medicine, University of Sumatera Utara
Introduction
Reflux of gastric contents to the oesophagus is a physiological event: a healthy person typically has reflux episodes. Gastro-oesophageal reflux disease is defined as reflux that causes troublesome symptoms, mucosal injury in the oesophagus, or both of these. By this definition, oesophageal lesions (erosions, ulceration, intestinal metaplasia) are not needed for a diagnosis of the disease. 1 GERD can be further classified as the presence of symptoms without erosions on endoscopic examination (non-erosive disease or NERD) or GERD symptoms with erosions present (ERD). 2
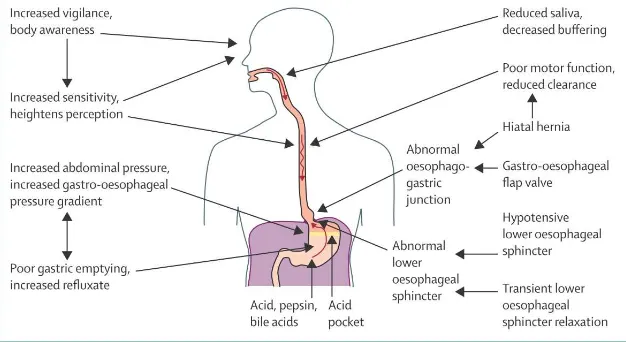
Pathophysiology GERD
Transient lower oesophageal sphincter relaxations (TLESRs)
Many GERD patients have a normal LES resting tone and do not have hiatal hernia, therefore the abnormal gastro-oesophageal reflux in these subjects is explained by an alternative theory. In fact, studies in healthy volunteers have identified reflux episodes during sleep and the postprandial period that are due to an increased number of inappropriate LES relaxations. TLESRs are brief episodes of LES relaxation unrelated to swallowing or peristalsis. Neurophysiology studies indicate that TLESRs are visceral reflexes with vagal afferent and efferent pathways that transmit information to and from the dorsal nucleus of the vagus. Gastric distension, by stimulation of proximal gastric tension and stretch receptors, has been recognized as a major factor inducing TLESRs. 4
In normal subjects, gastro-oesophageal reflux occurs only during TLESRs and swallow-induced LES relaxations, whereas in patients with GERD, TLESRs account for 48-73% of reflux episodes: thus TLESRs account for the majority of gastro-oesophageal reflux episodes. Patients with GERD have an equal frequency of TLESRs compared with normal individuals, although they have a higher percentage of TLESRs associated with reflux. Like LES resting pressure, the frequency of TLESRs is influenced by foods (fat, chocolate, etc.), alcohol and smoking. 4
Ineffective esophageal motility
propagated to the distal esophagus, or absent peristalsis. Hypocontractility is considered the most prevalent esophageal motor disorder in GERD and this concept has been further supported by different studies showing that esophageal peristaltic dysfunction was increasingly prevalent wit h more severe GERD presentation. Of note, in a group of patients with respiratory symptoms associated with reflux, IEM was found in 53% of asthmatics, 41% of chronic coughers and 31% of those with laryngitis. 5
Recently, studies carried out in patients with scleroderma, who are characterized by failed or absent peristalsis and low basal LES pressure, observed that these patients are frequently affected by GERD and its complications, thus substantiating the relevant role of esophageal clearance for the development of GERD. 5
Delayed gastric emptying
that gastrointestinal symptoms, including dyspepsia and regurgitation, occurred in many patients. These symptoms were not predictive of delayed gastric emptying. 6
Patients frequently complain of heartburn as well as postprandial dyspepsia or epigastric discomfort, and it is often difficult for patients to discriminate between these responses. It is currently believed that delayed gastric emptying contributes to the pathogenesis of GERD in a small proportion of patients, primarily by increasing available amounts of refluxate and causing gastric distension.The effects of gastric distension were investigated in a study by inflating an intragastric balloon in patients with GERD and controls. In both groups of patients, gastric distension significantly increased the rate of TLESRs, indicating that GERD-associated gastric distension may be a factor in postprandial GERD. 6
Increased intragastric pressure
Abnormal gastric emptying might contribute to GERD by increasing intra -gastric pressure. Patients with suspected abnormal gastric emptying should be tested with nuclear markers or ultrasound. If slow emptying is diagnosed, appropriate therapy should be considered. Medication such as metoclopramide and Nissen fundoplication improve gastric emptying. 7
There is also strong evidence of a possible link between obesity and G ERD. Specifically, it has been shown that there is a dose-response relationship between increasing body mass index (BMI) and prevalence of GERD and its complications. Some studies have reported that morbidly obese patients with GERD have a higher incidence of incompetent LES, transient LES relaxation and impaired esophageal motility than non-obese patients with GERD. However, a detailed mathematical analysis has shown that the severity of GERD (based on the DeMeester score) is associated with BMI, which suggests that obesity plays an independent role in the
The association of different pulmonary diseases and GERD has recently gained renewed interest. It has been shown that patients with end-stage lung disease have a high prevalence of GERD; up to 70%. Although in these patients pan-esophageal motor dysfunction is frequently found, a more negative thoracic pressure with an increase in the gradient between gastric and intra-thoracic pressure might also contribute. 7
Acid pocket
Most meals have a buffering effect that leads to reduced acidity of the stomach in the postprandial phase. However, acid reflux (as detected by pH monitoring) is generally most pronounced after meals. In the postprandial period, a layer of unbuffered acidic gastric juice sits on top of the meal, close to the cardia, ready to reflux. This occurrence has become known as the acid pocket and is facilitated by an absence of peristaltic contractions in the proximal stomach. In patients with gastro-oesophageal reflux disease, the acid pocket is located more proximally with respect to the squamocolumnar junction, and it could even extend above the manometrically defined lower oesophageal sphincter. Treatment with alginate-antacid preparations abolishes the pocket or increases the distance between the upper border of the acid pocket and the squamo columnar junction. 1
Oesophageal hypersensitivity
In a subgroup of patients with gastro-oesophageal reflux disease, reflux symptoms are noted while oesophageal acid exposure is within the normal range; thus, these individuals are hypersensitive to acid. Hypersensitivity to acid occurs both in people with erosive oesophagitis and in those with a macroscopically normal mucosa. Experiments in which acid is infused in the oesophagus indicate that the threshold to development of heartburn and pain is lower in patients with either erosive oesophagitis or non-erosive reflux disease than in controls. Factors contributing to the noted increased oesophageal sensitivity are impaired mucosal barrier function, upregulation of peripheral nociceptors, and central sensitisation. 1
Helicobacter pylori does not have an important role in the pathogenesis of gastro-oesophageal reflux disease. Eradication of the microorganism does not lead to an increased chance of development of the disorder. 1
Figure 1. Pathophysiology og gastro-oesophageal reflux disease 1
Diagnosis
Careful history taking is the main method to establish GERD diagnosis. Specific symptom of GERD is heartburn and/or regurgitation that occur after meal. However, it should be emphasized that most of diagnostic studies of heartburn and regurgitation symptoms are performed in Caucasian population. In Asia, the symptoms of heartburn and regurgitation are not the typical features for GERD. However, the experts have agreed that both symptoms are characteristics for GERD. 3
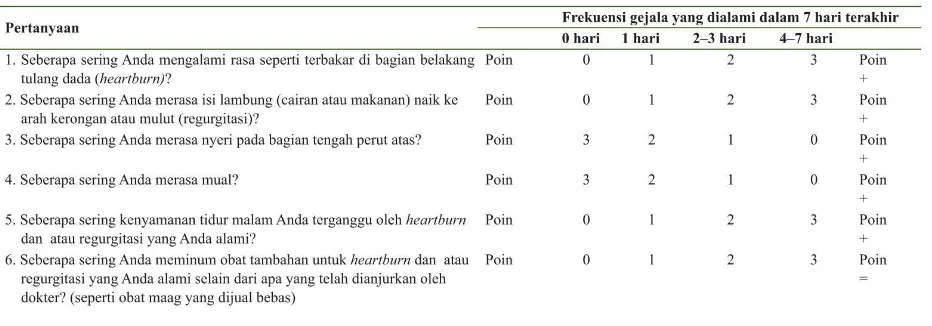
GERD-Q
will increase the sensitivity and specificity of diagnosis. An analysis on more than 300 patients at a primary health care service demonstrates that GERD-Q may provide sensitivity and specificity of 65% and 71%, which is similar to results obtained by gastroenterologists. Moreover, GERD-Q also shows the capacity to evaluate relative impacts of GERD on patients’ life and to provide assistance in selecting therapy. Table 1 is the GERD-Q that can be filled up by the patients themselves. For each question, respondent should fill up according to the frequency of symptoms that they have experienced in a week. Score 8 or more is the recommended cut -off point to detect individuals with high tendency to have GERD. GERD-Q has been validated in Indonesia. A symptom-based approach using GERD-Q reduced health care costs without loss in efficacy. GERD-Q score or PPI test alone cannot accurately diagnose. A definitive diagnosis of GERD still depends on endoscopy or 24-h pH monitoring. 3, 8, 9, 10
Table 1. The GERD-Q in Indonesian Language 11
PPI Test
of 80% and specificity of 74% for establishing diagnosis of GERD patients with non-cardiac chest pain. It indicates that PPI test can be considered as a useful strategy and probably has economic value in management of patients with non-cardiac chest pain without alarm signs of suspected esophageal abnormalities. 3
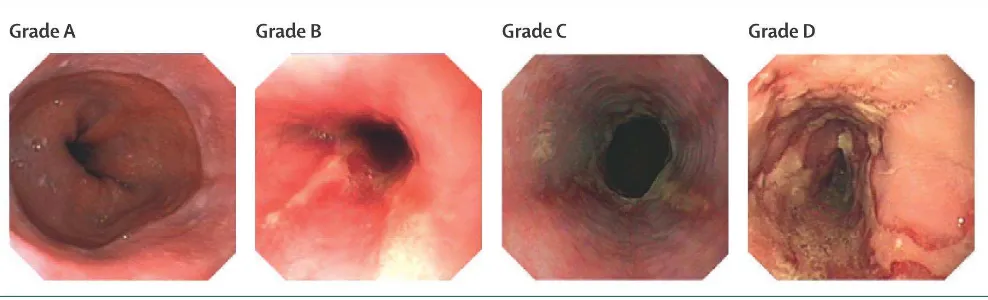
Upper Gastrointestinal Endoscopy
Upper gastrointestinal endoscopy (UGIE) is considered the gold standard for establishing the diagnosis GERD with erosive esophagitis. Using the UGIE, we can find the mucosal break of esophagus. 3 People who present with alarm symptoms (dysphagia, haematemesis, weight loss) warrant endoscopy, because they might have clinically significant complications of gastro -oesophageal reflux disease or other pathological features. For example, the test serves to rule out alternative diagnoses, such as eosinophilic oesophagitis, infection, and pill injury; furthermore, an observation of typical reflux oesophagitis confirms the diagnosis of gastro-oesophageal reflux disease. The severity of endoscopically observed reflux oesophagitis is graded with the Los Angeles classification. 1
Figure 2. Los Angles classification of reflux oesopahgitis 1
In grade A oesophagitis, endoscopic abnormalities are restricted to one or more mucosal lesions with a maximum
length of 5 mm. In grade B, one or more mucosal breaks are present, with a maximum length of more than 5 mm but
non-continuous across mucosal folds. In grade C oesophagitis, mucosal breaks are continuous between at least two
mucosal folds, but less than 75% of oesophageal circumference is involved. In grade D, mucosal breaks encompass
more than 75% of oesophageal circumference. 1
Conventionally, pH monitoring is done with a transnasally inserted catheter with pH sensor, capsules are roughly double the cost of a standard pH catheter. 1
Manometry
Oesophageal manometry is not indicated for diagnosis of gastro-oesophageal reflux disease because motor dysfunction associated with abnormal reflux is non-specific. The main indications for manometry are to ascertain the correct position for pH electrode placement and to exclude severe oesophageal motility disorders such as achalasia and absent peristalsis before antireflux surgery. Exclusion of other oesophageal disorders is important, because patients with achalasia can present with heartburn and regurgitation, which could lead to an erroneous diagnosis of gastro-oesophageal reflux disease. However, whether milder forms of peristaltic dysfunction predict postoperative dysphagia is uncertain. Manometry might be helpful in patients with predominant regurgitation because it can help to distinguish the rumination syndrome from gastro-oesophageal reflux disease. This diagnosis is best accomplished with concurrent pH and impedance monitoring. 1
References
1. Bredenoord AJ, Pandolfino JE, Smout AJPM. Gasto-oesophageal reflux disease. The Lancet. March 2013.
2. Katzs PO, Gerson LB, Vela F. Guidelines for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2013;108:308-328.
4. Giorgi F, Palmiero M, Esposito I, al e. Pathophysiology of gastro-oesophageal reflux disease. Acta Otorhinolaryngol ital. 2006;26(5):241-246.
5. Martinucci I, Bortoli N, Giacchino M, al e. Esophageal motility abnormalities in gastroesophageal reflux disease. World J Gastrointest Pharmacol Ther. 2014;5(2):86-96.
6. Castell D, Murray J, Tutuian R, al e. Review article: the pathophysiology of gastro-oesophageal reflux
disease − oesophageal a ifestatio s. Alimentary Pharmacology & Therapeutics. 2004;20:14-25.
7. Herbella F, Patti M. Gastroesophageal reflux disease: From pathophysiology to treatment. World J Gastroenterol. 2010;16(30):3745-49.
8. Bai Y, Du Y, )ou D, et al. Gastroesophageal Reflu Disease Questio aire GerdQ i real-world
practice: A national multicenter surve 8065 patients. Journal of Gastroenterology and Hepatology. 2013:626-631.
9. Jonasson C, Moum B, Bang C, Andersen KR, Hatlebakk JG. Randomised clinical trial: a comparison between a GerdQ-based algorithm and an endoscopy-based approach for the diagnosis and initial treatment of GERD. Aliment Pharmacol Ther. 2012;35:1290-1300.
10. )HOU LY, WANG Y, LU JJ, LIN L. A ura of diag osi g gastroesophageal reflu disease GerdQ,
esophageal impedance monitoring and histology. Journal of Digestive Diseases. 2014(15):230-238.