NATIONAL ORTHOPAEDIC REGISTRY
MALAYSIA (NORM)
ANNUAL REPORT OF
NATIONAL ORTHOPAEDIC REGISTRY MALAYSIA (NORM) HIP FRACTURE
2009
Editors:
Dr Mohammad Anwar Hau Abdullah Dr Ahmad Tajuddin Abdullah
Registry Committee
Dr Mohammad Anwar Hau Abdullah Dr Ahmad Tajuddin Abdullah
Dr Zulkiflee Osman Dr Saadon Ibrahim Dr Mohamad Yazid Din Dr Joehaimey Johari
Dr Se To Boon Chong Dr Tan Boon Cheong Dr Abdul Rauf Ahmad Dr Mohd Zamzuri Mohd Zain Dr Pan Chee Huan
December 2010
© National Orthopaedic Registry of Malaysia (NORM)
Publisher:
Jointly published by the National Orthopedic Registry of Malaysia (NORM) and the Clinical Research Centre (CRC), Ministry of Health Malaysia.
National Orthopaedic Registry of Malaysia 1st Floor MMA House,
124, Jalan Pahang, 53000 Kuala Lumpur, Malaysia.
Tel : (603) 4044 3060 / (603) 4044 3070 Fax : (603) 4044 3080
Email : norm@acrm.org.my
Website : http://www.acrm.org.my/norm
Suggested citation: Mohammad Anwar Hau Abdullah, Ahmad Tajuddin Abdullah (Eds). Annual Report of the NORM- Registry, 2009. Kuala Lumpur, Malaysia: National Orthopaedic Registry of Malaysia 2009.
Disclaimer:
Data reported in this report were collected for one year period (from January to December 2009), this report is copyrighted. Reproduction and dissemination of this report in part or in whole for research, educational or other non-commercial purposes are authorized without any prior written permission from the copyright holders provided the source is fully acknowledged.
Electronic version
The electronic version of this report may be downloaded at
http://www.acrm.org.my/norm or http://www.crc.gov.my/publication/report.
Funding
ACKNOWLEDGEMENTS
The National Orthopaedic Registry of Malaysia (NORM) would like to give its grateful appreciation to everyone who has helped make this report possible.
We would especially like to thank the following:
Clinical Research Centre Dr Goh Pik Pin Clinical Epidemiology Unit Dr Jamaiyah Haniff
Dr Dr Sharmini Selvarajah Dr Lim Chioa mei
Patient Registry Unit Dr Jaya Purany Stanley Ponniah Nurul Shuhada Binti Mohd Ali Scottish Hip Fracture Registry
NORM Governance Board
Chairman Dato’ Dr Azmi Shafei Director,
Division of Medical Development, Ministry of Health Malaysia.
Members Dr Jamaiyah Haniff
Head Of Clinical Epidemiology Unit,
Clinical Research Center, Hospital Kuala Lumpur.
Dr Jaya Purany Stanley Ponniah Head of Patient Registry Unit
Clinical Research Center, Hospital Kuala Lumpur. Dr Mohammad Anwar Hau Abdullah
Head of Department,
Department of Orthopaedic and Traumatology, Hospital Sultan Ismail, Johor Bharu.
Dr Se To Boon Chong
Department of Orthopaedic and Traumatology, Hospital Pulau Pinang,Pulau Pinang.
Dato’ Dr Suresh Chopra,
Head of Department,
Department of Orthopaedic and Traumatology, Hospital Sultanah Bahiyah, Alor Setar.
Dr Abdul Rauf Ahmad Head of Department,
Department of Orthopaedic and Traumatology, Hospital Tuanku Jaafar, Seremban.
Dato’ Dr Premchandran Menon
Head of Department,
Department of Orthopaedic and Traumatology, Hospital Tengku Ampuan Afzan (HTAA), Kuantan. Dr Pan Chee Huan
Head of Department,
Department of Orthopaedic and Traumatology, Hospital Tuanku Fauziah, Kangar.
Dr Thirumal a/l Manickam Head of Department,
Department of Orthopaedic and Traumatology, Hospital Tengku Ampuan Rahimah, Klang.
Dr Nahulan A/L Theva Rajah Head of Department,
Dato’ Dr Ramanathan A/L Ramiah
Head of Department,
Department of Orthopaedic and Traumatology, Hospital Raja Permaisuri Bainun, Ipoh. Mr.Sivapathasundaram A/L Nadarajah Head of Department,
Department of Orthopaedic and Traumatology Hospital Melaka, Melaka.
Dr K. Thevarajan Head of Department,
Department of Orthopaedic and Traumatology, Hospital Sultanah Aminah, Johor Bharu. Dr Faris Kamaruddin
Head of Department,
Department of Orthopaedic and Traumatology, Hospital Umum Sarawak, Sarawak.
NORM Steering Committee members:
Chairman Dr Ahmad Tajuddin Abdullah Head of Department,
Members Dr Mohammad Anwar Hau Abdullah Head of Department,
Department of Orthopaedic and Traumatology, Hospital Raja Perempuan Zainab II, Kota Bharu. Dr Saadon Ibrahim
Department of Orthopaedic and Traumatology, Hospital Sultan Ismail, Johor Bharu.
Dr Se To Boon Chong
Department of Orthopaedic and Traumatology, Hospital Pulau Pinang, Pulau Pinang.
Dr Tan Boon Cheong
Department of Orthopaedic and Traumatology, Hospital Pulau Pinang, Pulau Pinang.
Dr Abdul Rauf Ahmad
Department of Orthopaedic and Traumatology, Hospital Tuanku Jaafar, Seremban.
Dr Mohd Zamzuri Mohd Zain
Department of Orthopaedic and Traumatology, Hospital Tengku Ampuan Afzan (HTAA), Kuantan. Dr Pan Chee Huan
Department of Orthopaedic and Traumatology, Hospital Tuanku Fauziah, Kangar.
Dr Mohamad Yazid Din
Department of Orthopaedic and Traumatology, Hospital Sultanah Bahiyah, Alor Setar.
Dr Joehaimey Johari
NORM SOURCE DATA PROVIDERS 2008/2009
The current source data providers for NORM are:
No. Hospital Site investigators Second person-in-charge 1 Hospital Kuala
Lumpur
Mr Zulkiflee Osman Dr Mahazura Hj Mat Lawi Dr. Abdul Qahhar
2 Hospital Raja Perempuan Zainab II Kota Bharu
Mr Mohammad Anwar Hau Abdullah
Dr Joehaimey Johari
Sister Nik Noriah Nik Ibrahim
3 Hospital Sultanah Nur Zahirah Kuala Terengganu
Mr Ahmad Tajuddin Abdullah Dr Mustaqim Afifi @ Apipi Dr Hazulin Mohd Radzuan Dr Muhammad Hilmi Nasir Dr Mohd Ariff Razani Abd Razak
4 Hospital Tengku Ampuan Rahimah Klang
Dr Gurjit Singh Dr M. Thirumal
5 Hospital Sultanah Bahiyah Alor Setar
Dr Mohamad Yazid Din Dr Noor Mahazrinna Hayadin
Dr Lim Chiao Yee 6 Hospital Sultanah
Aminah Johor
Dr Mohd Adham Shah Dr Teo Pock Chin 7 Hospital Melaka Dr Rengsen Parthiban Dr Azhar Asari
9 Hospital Tuanku Fauziah Kangar
Dr Pan Chee Huan Mr Yeap Ewe Juan
Mr Zakaria Yusoff Dr Badrul Hashim Dr Zakaria Yusoff MA Shahizam Shafiee SN Norseha Baharom 10 Hospital Raja
Permaisuri Bainun Ipoh
Dr Manoharan Dr Selvynlloyd
Dr Iyngkaran Arasalingam
11 Hospital Tengku Ampuan Afzan Kuantan
Dato' Dr N Premchandran Dr. Mohd Zamzuri Mohd Zain
Dr Alaudin Haris Osman Dr Jeffrey Jaya Raj Dr Ahmad Hafiz bin Zulkifly 12 Hospital Ampang Dr Ng Yue Oon Dr Lynn Azura Md Sham
Dr Samyu Ali 13 Hospital Tuanku
Ja’afar Seremban
Dr Abdul Rauf Ahmad Dr Ng Tiong Soon Dr Johann Johari Sr Khamisah A. Ghani Sr Rohana Zakaria 14 Hospital Pulau
Pinang
Dr Se To Boon Chong Dr Tan Boon Cheong Dr Ooi Chee Lean Dr Chan Kok Yu 15 Hospital Serdang Dr Khoo Shaw Woei Dr Imma Isniza
Dr Harminder Singh Randhawa
16 Hospital Selayang Dr Ng Swee Soon Dr Ritzwan Ismayatim Dr Amir Fariz Zakaria 17 Hospital Queen
Elizabeth Kota Kinabalu
Dr Nahulan A/L Theva Rajah Dr CS Kumar
18 Hospital Umum Sarawak
PREFACE
The National Orthopaedic Registry Malaysia has been collecting data since mid 2008 and it is with great pleasure and pride that we see this report materialised.
I would like to thank all those who have collected, verified and analysed the data. The co-operation and energy demonstrated in units throughout the country indicates the
importance they place on improving patient management
The success of this report is due to continuous support and cooperation from various people and agencies. The effort of the entire group must be congratulated and it has been my sincere hope that this registry is able to sustain in coming years.
I also take this opportunity to thank the Clinical Research Centre Ministry of Health Malaysia, to have trust in us and to provide us with the funding for us embark in this project. This annual report is a testament of all your combined effort.
Thank you,
Dr Ahmad Tajuddin bin Abdullah Dr Mohammad Anwar Hau Abdullah
10
ABBREVIATIONS
ASA American Society of Anaesthesiologists
CRC Clinical Research Centre
CRF Case Report Form
csv Comma separated value
Dr Doctor
GA General Anaesthesia
HTAA Hospital Tengku Ampuan Afzan
ICT Information and Communication Technology
LMWH Low Molecular Weight Heparin
MJM Medical Journal of Malaysia
MOH Ministry of Health
NOHFR National Orthopaedic Hip Fracture Registry
NORM National Orthopaedic Registry of Malaysia
OT Operation Theatre
PTH Parathyroid Hormone
RTA Road Traffic Accident
SDP Source Data Provider
SERMS Selective Estrogen Receptor Modulators
SMS Short Messaging System
txt Text-delimited format
About National Orthopaedic Registry
The National Orthopaedic Registry of Malaysia (NORM) is a service supported by the Ministry of Health (MOH) to collect information about orthopaedic disease in Malaysia especially diabetes and hip fracture. This will enable us to know the incidence of the orthopaedic disease to evaluate its risk factors and treatment provided within the country. This information is useful in assisting the MOH, Non-Governmental Organizations, private healthcare providers and industry in planning and evaluation, leading to better orthopaedic disease prevention and control.
NORM is funded by Ministry of Health Malaysia (MOH) and was initiated by a group of health professionals from orthopaedic, public health specialists and epidemiologist in July 2007. Currently, 17 CRC’s hospitals and 1 Non-CRC hospital nationwide are contributing as Source Data Provider (SDP):
The source data providers are:
1. Hospital Ampang 2. Hospital Kuala Lumpur 3. Hospital Melaka 4. Hospital Pulau Pinang 5. Hospital Queen Elizabeth
6. Hospital Raja Perempuan Zainab II 7. Hospital Raja Permaisuri Bainon 8. Hospital Selayang
9. Hospital Serdang 10. Hospital Sultan Ismail 11. Hospital Sultanah Aminah 12. Hospital Sultanah Bahiyah 13. Hospital Sultanah Nur Zahirah 14. Hospital Tengku Ampuan Afzan 15. Hospital Tuanku Ampuan Rahimah 16. Hospital Tuanku Fauziah
17. Hospital Tuanku Jaafar 18. Hospital Umum Sarawak
12
NORM Organization
NORM Organization Chart
The organization of the NORM is shown below. The description of the duties and functions of each entity depicted follows.
Terms of References
Flow Chart of Registry Organisation
3B. CENTRE REGISTRY OFFICE
Centre for the collection of data, analysis of data, and feedback of information
This is staffed by the Clinical Registry Manager/Epidemiologist, CRA, Statistician, IT personnel and other supporting staffs To motivate, direct and communicate with its
staff on registry management & operations.
3A. STEERING / EXECUTIVE COMMITTEE
Ensure the register is run according to its stated aims, objectives and protocols
Ensure the rights of patients are respected Oversee the progress of the project Oversee the use of register data
Provide leadership and decision making on the registry
Establish a centre registry office to serve as administration and management centre
Facilitate access to data sources
1. EXPERT PANEL
Provide scientific & clinical advice to the project Guide future development of registry
Ensure good technical and scientific basis of the registry Decide initial data collection process and its contents Consists of specialists related to the field of registry Conduct literature review
Conduct quality control on the CRF & Data Interpreting results generated by the statistician Report writing
Facilitate access to data source by centre office
2. PRINCIPAL INVESTIGATOR (PI)
The PI is the chairperson of the expert panel & steering/executive committee
PI leads, manages & coordinates activities of the whole registry
5. SPONSORS
Responsible to the DG of Health for the effective, efficient and responsive operations of the database Provide the financial, human and information
resources required.
E.g. CRC, NIH, Specialist Department of MOH, Pharmaceutical Companies, Private Associations, U i ersities…etc.
4. RESEARCH ETHICS COMMITTEE APPROVAL
Seeking ethical approval for clinical research or waver of informed consent in registry project
8. SOURCE DATA PROVIDER (SDP)
Data collection
Includes all participated study sites May involve other data sources e.g.
Jabatan Pendaftaran Negara (JPN) for national all-cause mortality information Staffed by Site coordinators & RA
7. VENDOR FOR DATA STORAGE & SECURITY
9. USERS GROUP
Includes the public health practitioner, health care provider, health service planner & decision maker, researchers and on occasions, the public community.
Feedback on information gathered by the registry and contributes to future planning
6. GOVERNANCE BOARD
Membership should represent all stakeholders including source data providers, users groups and representative from the steering committee and the centre registry office
Chaired by a neutral party
Determines the policy and protocols for the operation of the registry
14
NORM Office
The collection, and analysis of data, and feedback of information are performed in a single centre referred to as the NORM Office. This unit is managed by staff nurse and other supporting personnel provided by CRC. The Clinical Research Centre (Kelantan) is currently the designated NORM Office.
Objectives of the NORM – Hip Fracture are to:
1. Determine the number and type of hip fractures among patients ages 50 years and above admitted into orthopaedic wards in MOH hospitals
2. Determine the cost/burden of treating hip fracture in terms of a) Average length of stay.
b) Percentage of patients that underwent surgery. c) The average waiting time for surgery.
3. Determine the demographic of the hip fracture patients admitted into MOH hospitals in terms of:
a) Gender proportion b) Age distribution c) Ethnic proportion d) Socio-economic status e) Pre-fracture residence f) Mechanism of Injury g) Pre-fracture morbidity.
4. Determine immediate treatment outcomes and complications, and functional outcome at six months post treatment.
5. Determine the current practice among orthopaedic surgeons in MOH hospitals a) Timing of surgery
b) Type of surgery (Implant used) c) Antibiotic prophylaxis
d) Thrombo-embolitic prophylaxis.
6. Facilitate service improvements.
8. Users
These are the individuals or institutions to which the regular database reports are addressed. They include
Orthopaedic professional
Health care provider
Public health practitioner
Industry
Decision maker
Researcher
16
EXECUTIVE SUMMARY
The National Orthopaedic Registry of Malaysia (NORM) on Hip Fracture for patients age 50 and above established in 2008. Its main objectives was to establish a national database of patients treated for hip fract (especially for ages 50 and above) in 18 orthopaedics departments within MOH hospitals and to revie patients’ demography, social background, hip fracture patterns, clinical practices and outcome. The follow the descriptive annual report on the data collected from 1st January to 31st December 2009:
1. The total number of cases analysed was 510.
2. Two-third (345 out of 510 cases) of the patients were female and 75.1% of them were from the post-menopausal women (mean age attained menopause was 50.4 year).
3. The mean age of the patients at the time of presentation (admission) was 74.5 years with the peak ag group was 70 to 79 year-old.
4. The ethnic distributions among the patients were not in line with the country’s population racial ratio. There were 44.5% Chinese, Malays 40.0% Malays and 13.9% Indian from this database.
5. Ninety-seven percent of patients lived in their home either independently or with carer(s), and majori (70.8%) of them were able to function and walk without any aids prior to the hip fracture.
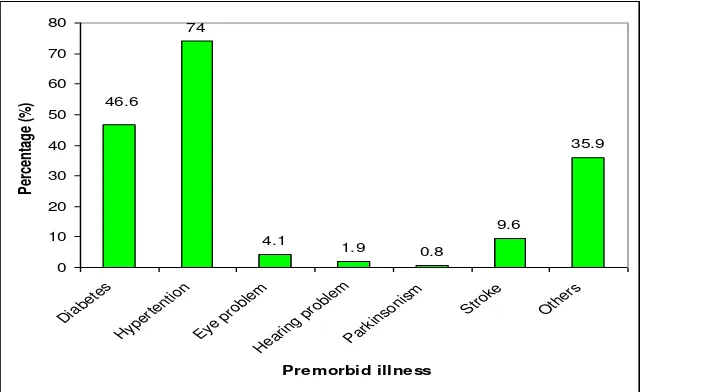
6. However, seventy percent (n=365) of the patients from the database were having some form of co-mo illness at the time of admission; the most common pre-morbid illness were hypertension (74.0%) diabetes mellitus (46.6%).
7. 12.2% of the patients were on some form of anti-osteoporotic medication; and among those on an osteoporotic medications, 77.4% and 46.8% of them were taking calcium and vitamin D supplement respectively.
8. There were only 5.3% of the patients have had previous hip fracture prior to the current admission.
9. For the current admission, 84.5% of the patients attributed “fall” as the cause of the hip fracture. 10. There were 82.5% of the patients underwent surgical treatment. And 17.5% (n=89) of the patients were trea
non-surgically. The most common reasons for conservative treatment were patient refusal (34.5%) and patient were medically unfit (32.2%).
11. Among those who were treated surgically, the surgeries were considered as delayed in 81.3% (340 ou 418 patients); the main reasons for the delay were lack of OT 49% and patients’ medical condition neede further optimisation (24%). However, there were 8% cases were due to financial problems.The m preferred method of fracture treatment was using DHS/DCS (54.1%), and there were 7.0% of the patien underwent total joint replacement.
13. About two third (63.1%) of the surgeries were performed by consultants or specialists and 61.7% surgi assistant were medical officers.
14. There were 88.7% of the patients did not received any form of thromboprophylactic.
15. Among the patients on chemical thromboprophylaxis; low molecular weight heparin (LMWH) was the m popular form of thromboprophylaxis (151 patients).
16. Surprisingly, 16.5 %(n=78) of patients who underwent surgery did not receive any form of antibio prophylaxis. The most common prophylactic antibiotic used was Cefuroxime (71.2%).
17. It is notable that, 97.4% of patients were successfully treated and discharged.
18
CONTRIBUTING EDITORS
Technical support personnel
Database Administrator Ms Lim Jie Ying Clinical Data Manager Ms Teo Jau Shya
Table of Contents
SECTION 1: PATIENT DETAILS AND DEMOGRAPHIC 21
SECTION 2: PRE-FRACTURE STATUS (IMMEDIATELY PRIOR TO FRACTURE) 22
Table 2.1: Pre-Fracture status (immediately prior to fracture), Hip Fracture,, National Orthopadic Registry
National Orthopedic Registry Malaysia (NORM) 2009. 22
SECTION 3: FRACTURE TYPE 25
Table 3.1: Distribution of pathological fracture and fracture types at Pre-Operative Phase, Hip Fracture,
National Orthopadic Registry Malaysia (NORM) 2009 25
SECTION 4: PRE-OPERATION PHASE 26
SECTION 4: TREATMENT 27
Table 4.1: Type of treatment, Hip Fracture, National Orthopadic Registry Malaysia (NORM) 2009. 27 Table 4.2: Conservative reasons, Hip Fracture, National Orthopadic Registry Malaysia (NORM) 2009. 27 Table 4.3: Operation Status after 72 hrs to theatre and operation type list, Hip Fracture, National
Orthopaedic Registry Malaysia (NORM) 2009. (Surgery, N = 418) 28
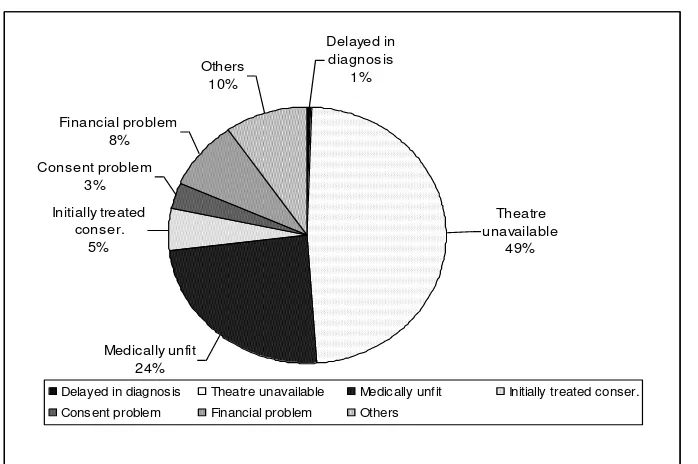
Figure 4.2: Delayed reasons after 72 hours to theatre and operation type list, Hip Fracture, National
Orthopadic Registry Malaysia (NORM) 2009. (Surgery, n= 340) 29
Table 4.4: Treatment detail (side and operation type) Hip Fracture, National Orthopadic Registry Malaysia
(NORM) 2009. 29
Table 4.5: Treatment detail (ASA grade) Hip Fracture, National Orthopadic Registry Malaysia (NORM)
2009. 30
Table 4.6: Treatment detail (anaesthetic type), Hip Fracture, National Orthopadic Registry Malaysia
(NORM) 2009. 31
Spinal (66.3%) and General Anaesthesia (28.9%) were the preferred mode of anaesthesia. 31 Table 4.7: Treatment detail (grade of staff), Hip Fracture, National Orthopadic Registry Malaysia (NORM)
2009. 31
Table 4.8: Treatment detail (type of chemical thrombop. and antibiotic prophylaxis), Hip Fracture,
National Orthopadic Registry Malaysia (NORM) 2009. 33
SECTION 5: POST OPERATIVE 34
20
Section 1: Patient Details and Demographic
In 2009, a total number of 510 patients recoded in the National Orthopaedic Registry of Malaysia-Hip Fracture. Two-third (345 out of 510 cases) of the patients were female whereas 32.4%
50-59 60-69 70-79 80-89 ≥90
Age Group (Ye ar)
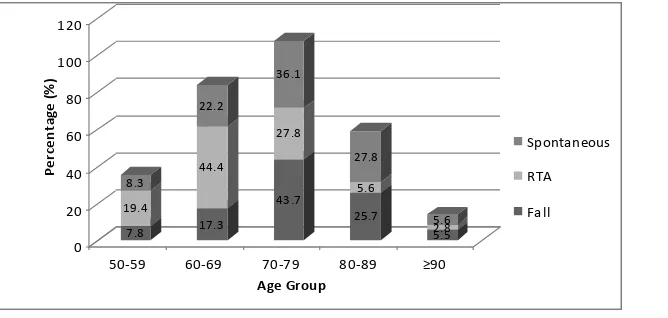
Figure 1.1: Distributions of Hip Fractures patient by age group, National Orthopaedic Registry of Malaysia (NORM, 2009)
The mean age of the patients at the time of presentation (admission) was relatively old at 74.5 years with standard deviation of 9.9. It was clearly known that, 8.6% were aged between 50-59 years old; 20.0 % were aged between 60-69 years old; 41.4. % were aged between 70-79 years old; 23.9 % were aged between 80-89 years old and the remaining 6.1 % were aged over 90 years old. The peak age-group was recorded at 70 to 79 year-old.
22
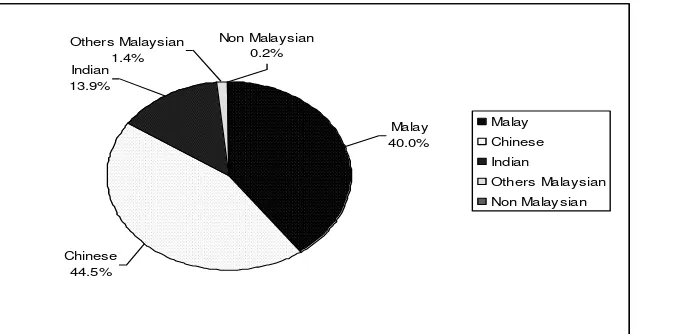
In terms of ethnicity, the majority of cases were Chinese (44.5%) followed by Malay (40.0 %,) and Indian (13.9 %). However, these figures may not represent the ethnic distribution of our country’s population racial ratio where Malays are made up an estimated 50.4% of the total population of 26.64 million, Chinese 23.7%, Indian 7.1%, and non-Malay Bumiputra 11%)1.
Section 2: Pre-Fracture status (immediately prior to fracture)
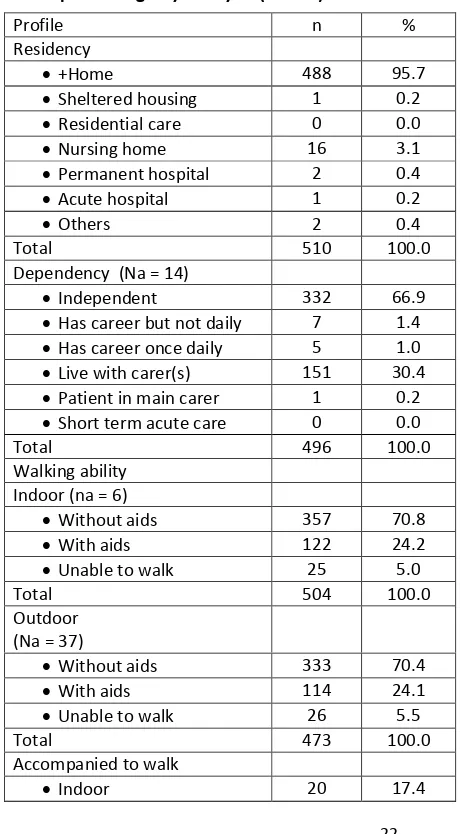
In regards to the dependency and walking ability of the patients, it is notable that majority of them lived in their home either independently or with carer(s) with the rate of 97 % whereby 70.4% of them were able to function and walk without any aids prior to the hip fracture.
Table 2.1: Pre-Fracture status (immediately prior to fracture), Hip Fracture,, National Orthopaedic Registry Malaysia (NORM) 2009.
Profile n %
Accompanied to walk
Outdoor 29 25.2
Both indoor and outdoor 66 57.4
Total 115 100.0
Footnote Na-not available *Denominator is 510
Comorbidity of the patients was also taken into account at the time of admission which illustrates the effect of all other diseases an individual patient might have other than the primary disease of interest.
Figure 2.1: Pre-Fracture status (pre-morbidity illness), Hip Fracture,, National Orthopaedic Registry Malaysia (NORM) 2009.
24
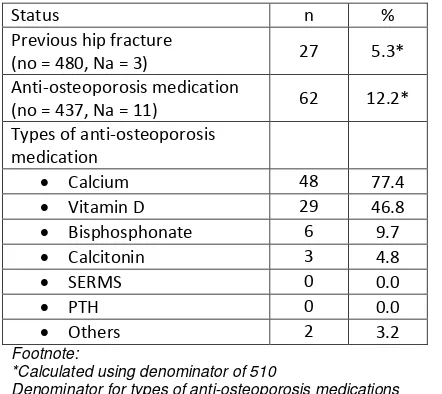
A total of 27 (5.3%) patients were reported having previous hip-fracture prior to the current admission out of which only 12.2% of the patients were on some form of anti-osteoporotic medication; and among those on anti-osteoporotic medications, 77.4% and 46.8% of them were taking calcium and vitamin D supplement respectively.
Table 2.4 Pre-Fracture status (immediately prior to fracture), Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Status n %
Previous hip fracture
(no = 480, Na = 3) 27 5.3*
Anti-osteoporosis medication
(no = 437, Na = 11) 62 12.2* Types of anti-osteoporosis
medication
Calcium 48 77.4
Vitamin D 29 46.8
Bisphosphonate 6 9.7
Calcitonin 3 4.8
SERMS 0 0.0
PTH 0 0.0
Others 2 3.2
Footnote:
*Calculated using denominator of 510
Denominator for types of anti-osteoporosis medications Na-not available
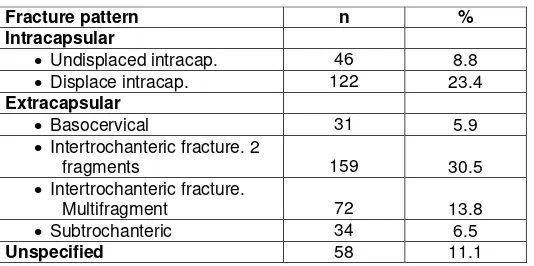
Section 3: Fracture Type
Table 3.1: Distribution of pathological fracture and fracture types at Pre-Operative Phase, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Footnote:
*Could not get exact 100.0% due to rounding error.
In general, the predominant mechanism of hip fracture that was reported is fall (85%). This is followed by spontaneous (8.1%) and RTA (6.9%).
7.8
50-59 60-69 70-79 80-89 ≥9
Age Group
Spontaneous
RTA
Fall
*Calculated using denominator of 498
Denominator for types of anti-osteoporosis medications is 62
Figure 3.2: Distribution of mechanism of injury, Hip Fracture, National Orthopaedic Registry
Fracture types n %
Undisplaced intracap. 44 10.1
26 Section 4: Pre-operation phase
In present-day surgical practice, fracture patterns are highly taken into consideration in which this question will guide the postoperative management.
Table 3.1: Pre-Operative Phase, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
The fracture patrons were categorised under three different categories. Extracapsular was the highest fracture pattern been reported with 63.3 %( n=296). Among all the fractures,
intertrochanteric fracture being the most common fractured type (44.3%). Intertrochanteric fracture was recorded at 3.8 % followed by subtrochanteric fracture and basocervical fracture (6.5% and 5.9 % respectively).
Meanwhile, 32.2 % (n=168) were diagnosed to be having Intracapsular fracture pattern with 8.8 % (n=46) fall under undisplaced intracap type and 23.4 % (n=122) fall under displace intracap type. It is also notable that 11.1% (n=58) patients were admitted with unspecified fracture pattern.
Fracture pattern n %
Intracapsular
Undisplaced intracap. 46 8.8 Displace intracap. 122 23.4 Extracapsular
Basocervical 31 5.9
Intertrochanteric fracture. 2
fragments 159 30.5
Intertrochanteric fracture.
Multifragment 72 13.8
Subtrochanteric 34 6.5
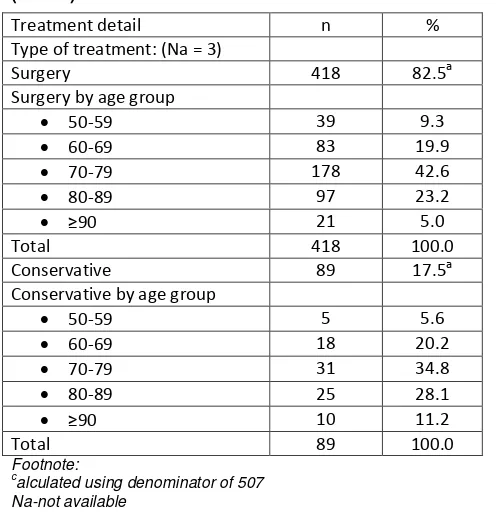
Section 4: Treatment
Table 4.1: Type of treatment, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Treatment detail n %
Type of treatment: (Na = 3)
Surgery 418 82.5a
Surgery by age group
50-59 39 9.3
Conservative 89 17.5a
Conservative by age group
50-59 5 5.6
alculated using denominator of 507 Na-not available
In general, the greatest percentage of patients with hip fracture clustered at the age group 70-79. In total, there were 82.5% (n=418) of the patients underwent surgical treatment for the hip fracture, and 17.5% (n=89) of the patients treated non-surgically. Among patients treated conservatively, 39.3% were > 80 years old, compared with 28.2% of those treated surgically.
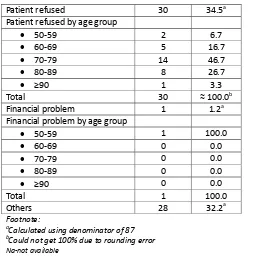
Table 4.2: Conservative reasons, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Treatment detail n %
Reason for conservative: (n = 89, Na = 2)
Patient medically unfit 28 32.2a Medically unfit by age group
50-59 0 0.0
28
Patient refused 30 34.5a
Patient refused by age group
50-59 2 6.7
Financial problem by age group
50-59 1 100.0
Calculated using denominator of 87
b
Could not get 100% due to rounding error
Na-not available
The most common reasons for conservative treatment were patient refusal (34.5%) and patients were medically unfit (32.2%).
Table 4.3: Operation Status after 72 hrs to theatre and operation type list, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009. (Surgery, N = 418)
Status: n %
No delay 78 18.7
Delay 340 81.3
Total 418 100.0
Operation type list (na = 38, missing = 92)
Could not get 100% due to rounding error
na-not available
Initially treated
Delayed in diagnosis Theatre unavailable Medically unfit Initially treated conser.
Consent problem Financial problem Others
Figure 4.2: Delayed reasons after 72 hours to theatre and operation type list, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009. (Surgery, n= 340)
Themain reasons for the delay were lack of OT time (53.8%) and patients’ medical condition needed further optimisation (27.1%). There were 9.4% (32 cases) due to financial problems.
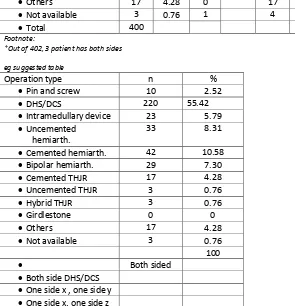
Table 4.4: Treatment detail (side and operation type) Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
n row % n row % n row %
Comment [c1]: Recommend analysis of % is done by the column. At least for single.
Comment [c2]:
30
*Out of 402, 3 patient has both sides
eg suggested table
Operation type n %
Pin and screw 10 2.52
DHS/DCS 220 55.42
Intramedullary device 23 5.79
Uncemented
Table 4.5: Treatment detail (ASA grade) Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Suggest the table to be designed this way:
All
1 of the patients in ASA 2 had surgery at both side
Majority of the patient; 81.9% were in ASA 1 or 2 at the time of surgery.
Table 4.6: Treatment detail (anaesthetic type), Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Anaesthetic type n %
GA 121 28.9
Spinal 277 66.3
Epidural 74 17.7
Intrathecal opiate 0 0.0
Sedation 2 0.5
Regional block 5 1.2
Wound infiltration 0 0.0
Total 479
Footnote:
aCalculated using denominator of 418 (number of treatment Surgery)
Spinal (66.3%) and General Anaesthesia (28.9%) were the preferred mode of anaesthesia.
Table 4.7: Treatment detail (grade of staff), Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Grade of staff n %
Surgeon (na = 3)
Consultant 67 16.1
Specialist 195 47.0
Clinical specialist 5 1.2
Medical officer 148 35.7
Others 0 0.0
Assistant (na = 5)
Consultant 11 2.7
32 Anaesthetist (na = 18)
Consultant 15 3.8
Specialist 103 25.8
Clinical specialist 2 0.5
Medical officer 272 68.0
House officer 8 2.0
Others 0 0.0
A aesthetist’s assist. a = 9
Consultant 0 0.0
Specialist 6 2.0
Clinical specialist 1 0.3
Medical officer 169 56.5
House officer 14 4.7
Others 109 26.5
Table 4.89: Treatment detail (type of chemical thrombop. and antibiotic prophylaxis), Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009.
Treatment detail Descriptive summary
n %
Type Chemical thromboprop. (n = 179, na = 12)
Heparin 16 9.6
LMW heparin 151 90.4
No. Of doses: Chemical thromb. (n = 179)
Mean (SD); Min, max 7.8 (5.7); 1, 30 Median IQR (1stQ, 3rdQ) 6.0 IQR (4, 10) Antibiotic prophylaxis (na = 36)
Yes 393 82.9
No 78 16.5
Contraindicated 3 0.6
Antibiotic prophylaxis: (n = 393)
Ampicillin 20 5.1
Amoxicillin 8 2.0
Cloxacilin 24 6.1
Cephalexin 1 0.3
Cefuroxime 280 71.2
Cefoperazone 21 5.3
Ceftriaxone 27 6.9
Ceftazidime 1 0.3
Gentamicin 2 0.5
Sulbactem 6 1.5
Others 15 3.8
34
Section 5: Post Operative
Table 5.1: Post Operative, Hip Fracture, National Orthopaedic Registry Malaysia (NORM) 2009
Post operative phase Descriptive summary
n %
Discharge status (na = 5, missing = 1)
Alive 491 97.4
Death 13 2.6
Discharge destination (missing = 1)
Home 454 89.2
Sheltered housing 2 0.4
Residential care 14 2.8
Nursing home 1 0.2
Permanent hospital 3 0.6
Acute hospital 12 2.4
Mortuary 13 2.6
Others 10 2.0
The overall length of hospital stay in patients with hip fracture was 13.6 days. It was notable that 97.4% of the patients were discharged alive from orthopaedic; 2.4% were transferred to another acute hospital; 89.2% of them were able to be discharged home. However, there were 2.6% of the patients (13 patients) died of various causes during the hospitalisation.
Figure 4.3: Duration of hospital stay, Hip Fracture, National Orthopadic Registry Malaysia (NORM) 2009.
Most patients stayed 7-13 days; 58.6% stayed 13 days or less.