Presented by:
• WHO 2010 kasus negleted ,2016 masih tetap negleted
Ular berbisa tersebar sangat luas mulai dari laut, darat (dataran rendah sampai dataran tinggi). Luasnya daerah distribusinya membuta ular teradaptasi dengan sempurna pada habitatnya.
Variasi habitat, pakan dan persebaran geografi memperlihatkan perbedaan komposisi racun mereka.
Setiap ular berbisa memiliki karakter bisa yang khas, sehingga antibisa ular yang digunakanpun juga harus khusus.
Indonesia mempunyai kasus yang sangat banyak untuk gigitan ular berbisa.
Namun demikian data tersebut tersebar diseluarh rumah sakit dan puskesmas di seluruh Indonesia.
Data keseluruhan belum terkumpul didalam satu sitem data base.
Data yang terkumpul (Maret 2015 – Agustus 2016) di Kabupaten Bondowoso (Jawa Timur) saja adalah 148 kasus mulai kasus gigitan,
terdiri dari kasus gigitan Ular viper pohon Trimeresurus insularis (85 kasus),Ular weling
Bungarus candidus (5 kasus), Ular kobra Naja sputatrix (15 kasus). Ular tanah
Colleselasma rhodostoma (2 kasus), 5 kasus gigitan oleh ular tak berbisa (non venomous snake: ular kopi Coelognathus flavolineatus dan Ular air Xenochrophis trianguligera),
dan 36 kasus gigitan yang tidak dapat diidentifikasi jenis ularnya. Selain itu, terdapat juga 5 kejadian venom Ophthalmia (mata tersembur oleh bisa Ular kobra Naja
•
1.lingkungan:kebun,sawah,tambang,hutan gunung,rawa
•
Carana memakai APD(sandal,sepatu boot,sepattu
berlampu,lampu sener kepala,senter,tongkat,celana panjang
•
2.rumah:rumah kotor sarang tikus,katak,kandang
ayam,membersihkan tumpukan kayu,gundukan rayap,lubang di
dinding kayu,bambu ,menaa anaman bambu,perdu
•
3.pekerjaan:petani,nelayan,penari ular,snake handler,pawwang
ular,restoan menu ular,penyamak kulit ular
WHO review 2016
Kolaborasi dokter dan herpetologi sudah
dimulai RECSINDONESIA sejak tahun
2013 sampai sekarang dalam hal
identifikasi ular
Faktor penting:
1.First aids
2.Transportasi
3.Manajemen di pkm dan rs
4.Kesadaran masyarakat
5.Pemulihan fisik dan mental
Indonesia
Jumlah total ular 348 jenis
Yang berbisa:
•
Elapidae: 55 jenis
•
Viperidae: 21 jenis
Famili Viperidae
1.
Daboia siamensis
Subfamili Crotalinae (Pit Viper)
1.
Trimeresurus albolabris
2.
Trimeresurus puniceus
3.
Calloselasma rhodostoma
Famili Colubridae (Colubrinae)
1.
Boiga Cynodon
2.
Boiga multomaculata
3.
Boiga dendrophila
4.
Boiga irregularis
Famili Elapidae
1.
Naja sputatrix
2.
Naja sumatrana
3.
Opiophagus hannah
4.
Calliophis bivirgata
5.
Calliophis intestinalis
Rhabdophis chrysargos
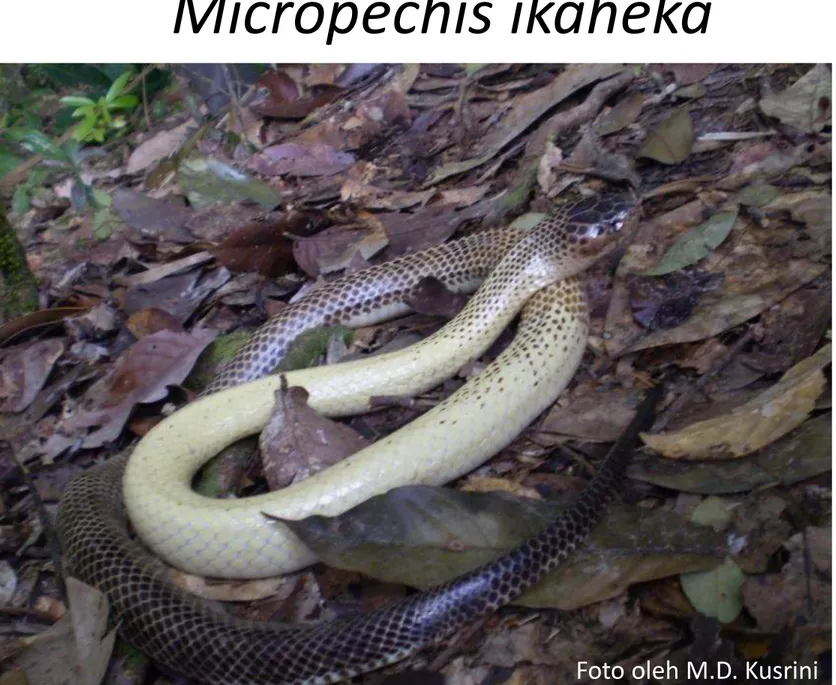
Micropechis ikaheka
Papuan taipan (Oxuyuranus
Papuan black snake (Pseudechis
Eastern brown snake
(Pseudechis textilis)
Ular laut
Blue
spotted sea snake
(Hydrophis cyanocinctus)
Thailand
SNAKE
NON-VENOMOUS VENOMOUS
Cardiotoxin Hemotoxin Neurotoxin
Nephrotoxin Necrotoxin
1.Bengkak dan memar disebabkan karena venom yg menyebabkan
peningkatan permeabilitas vascular dan ischemia disebabkan karena trombosis pada first aids yang salah berupa torniquet.
2.Hipotensi dan shock disebabkan hipovolemia leakage plasma dan darah ,vasodilatasi dan kerusakan myocardial
3.Oligopeptida dan vasodilatasii autocoid menyebabkan transient hipotensii dini
4.Procoagulasi enzyym menyebabkan defibrinogenesis,DIC,coagulopathi 5.Phospolipase adalah anti coagulan
6.Platelet aktiasi atau inhibisi dan sequestrasi menebabkan trombositopeni 7.Perdarahan sistemik spontan disebabkan oleh enzym N metaloprotease
haemorrhagins
8.Complemen akivasi platelet koagulasi darah dan mediator humoral
Patofisiologi venom (WHO review 2016)
Di rumah sakit
Ada antibisa ular yang siap diberikan
Kapan PBI dipakai
Jarak jauh
Ular tidak diketahui jenisnya
LOCAL
•
Swelling > half bitten
limb/48 hours
•
Toes especially fingers
•
Rapid extension within a few
hours
•
Enlarged tender lymphnode
draining the affected area
SYSTEMIC
•
Haemostatic abnormality
•
Neurotoxic signs
•
Cardiovascular abnormalities
•
Acute kidney injury
•
Myoglobinuria/generalised
rhabdomyolysis/haemolysis
•
Supporting lab evidence of
systemic envenoming
•
HOME
• DO NOT PANIC
• DO NOT GIVE CONSTRICTING BAND (TORNIQUET), SUCKING, or OTHER TRADITIONAL TREATMENT
• IMMOBILIZE BITTEN AREA (will be discussed)
• SEND TO PRIMARY HEALTH CARE OR EMERGENCY DEPARTMENT
• BRING DEAD OR ALIVE SPECIMENT OR SNAKE PHOTO INTO
EMERGENCY TO BE IDENTIFIED TO GIVE A SUITABLE ANTIVENOM
•
PRIMARY HEALTH CARE
• DO GENERAL EXAMINATION, MAKE IT STABLE !
• EVALUATE THE IMMOBILIZATION
• GIVE IMMOBILIZATION IF NO IMMOBILIZATION BEFORE
• GIVE ANALGESIA WHEN NEEDED
• MARK THE EDEMA BY USING RPP TEST (will be discussed)
• DO NOT DO CROSS INCISION !!!!
•
20 minutes Whole Blood Clotting Test (20’WBCT)
•
Rate Proximal Progression (RPP) Test
•
Electrocardiography
•
Laboratory check
• Haemoglobin
• White blood cells
• Platelet count
• Liver function test
• Renal function test
• PT
• APTT
•
Aim : to make sure hemotoxin or not by knowing from the
coagulation.
•
How to do?
• Take a glass bottle, DO NOT USE PLASTIC BOTTLE
• Take 2 ml of blood
• Then take that blood into the glass bottle
• Wait for about 20 minutes
• Repeat that test 2 times minimal
• Result :
• After waiting about 20 minutes:
• Clotting (+) : no coagulation disorder (NonHemotoxin)
•
Aim : to evaluate the edema progression to make a
best next medical treatment.
•
How to do?
•
Take a tape as a mark to measure the edema
•
Make sure the proximal margin of the edema, then take the
distal margin of the tape into the proximal margin of the
edema.
•
Note the time when the tape was given (date and time)
•
Repeat the evaluation of the edema every 2 hours
•
Result : cm/hour
•
Example : 10/10/15 ; 09.00
–
11.00 = 4 cm. So we have
5 cm
5 cm / 2 hours, so RPP = 2.5 cm/hour
Keep the Airway Breathing and Circulation stable
•
Airway
• 02 Non Re-Breathing Mask 12 lpm
• Laryngeal Mask Airway and Endotracheal Tube (if needed)
• Suction if gargling (+), Head tilt and chin lift if snoring (+)
•
Breathing
• Evaluate the respiratory rate
•
Circulation
• Make iv access, give Normal Saline 0.9% (don’t forget to take some
blood for laboratory checking)
• Blood pressure
• Pulse
• Oxygen saturation by using pulse oxymetri
•
Immobilize bitten area by using Pressure Bandaging
Immobilization
•
Antivenom :
DRUG OF CHOICE
• If the snake that bite the patient include in 3 snakes which are covered by the SABU, we can give SABU quickly
• 2 vials SABU + 100 ml Normal Saline 0.9% dripped 60-80 drop per minute
• Repeated every 6-8 hours. BE AWARE TO RE-ENVENOMATION SIGN!!!
•
Symptomatic
• Analgesia : morphine (PS≥7) and paracetamol infusion or oral (PS<7)
•
Antibiotic
•
Anticholinesterase drugs
• Especially for neurotoxin envenoming
• Should give atropine before giving the drugs to prevent physostigmine intoxication.
• Physostigmine dose
• Adult (>12 yo) : 1.0-2.0 mg
• Children ≤ 12 yo : 0.02 mg/kg/dose (max single dose 0.5 mg)
Presinaptik : Phosolipase A2 merusak vesikel sinaptik release
Postsinaptik:polipeptide toxin yang mengeblock acetylcholin reseptor pada muscle end plate
Dendrotoxin:K+ channel oksin menstimulasi sehingga terjadi over release neurotransmitter
Asciculins:anicholinesterase mengeblok normal breakdown dan recycling neurorasmiier release
Neuromuscular junction snake toxin
•
SABU covers 3 venomous snakes
1.
Agkistrodon rhodostoma
2.
Naja sputatrix
Any questions after this meeting? Feel free to reach Dr. dr. Tri Maharani, M.Si, Sp. EM
by phone or whatsapp 085334030409 (Telkomsel) or 08973665684 (Tri)