2010 THE AUTHORS. JOURNAL COMPILATION 2010 BJU INTERNATIONAL Lower Urinary Tract
TURis-PVP VS STANDARD TURP FOR BPE GEAVLETE
et al.
Transurethral resection (TUR) in saline plasma
vaporization of the prostate vs standard TUR of
the prostate: ‘the better choice’ in benign
prostatic hyperplasia?
Bogdan Geavlete, Razvan Multescu, Mihai Dragutescu, Marian Jecu,
Dragos Georgescu and Petrisor Geavlete
Department of Urology, ‘Saint John’ Emergency Clinical Hospital, Bucharest, Romania
Accepted for publication 29 January 2010
randomized trial. All patients were evaluated preoperatively and at 1, 3 and 6 months after surgery by IPSS, health-related quality of life (HRQL) score, Qmax and postvoid residual
urine volume (PVR).
RESULTS
Patients from both series had similar preoperative characteristics. TURis-PVP and TURP were successfully performed in all cases (75 and 80, respectively). The operative duration, catheterization period and hospital stay were significantly shorter for TURis-PVP patients at 35.1 vs 50.4 min, 23.8 vs 71.2 and 47.6 vs 93.1 h, respectively (all P< 0.05). At the 1, 3 and 6 months follow-ups, improvements in the variables measured were better in the TURis-PVP group: the IPSS was 4.4 vs 8.3 and the Qmax was 22.7 vs
20.5 mL/s at 1 month; the IPSS was 4.8 vs 8.6
and the Qmax was 22.3 vs 20.0 mL/s at 3
months; and the IPSS was 5 vs 9.1 and the Qmax was 21.8 vs 19.3 mL/s at 6 months (All
P< 0.05).
CONCLUSIONS
TURis-PVP represents a valuable endoscopic treatment alternative for patients with BPE, with superior efficacy, short-term results and complication rates compared with monopolar TURP.
KEYWORDS
transurethral resection in saline plasma vaporization of the prostate, transurethral resection of the prostate, benign prostatic hyperplasia
Study Type – Therapy (RCT) Level of Evidence 1b
OBJECTIVE
To evaluate the efficiency, safety and short-term outcome of transurethral resection in saline plasma vaporization of the prostate (TURis-PVP), and to compare it to the standard TUR of the prostate (TURP).
PATIENTS AND METHODS
In all, 155 patients with benign prostatic enlargement (BPE) secondary to benign prostatic hyperplasia (BPH), with a maximum urinary flow rate (Qmax) of <10 mL/s, an
International Prostate Symptom Score (IPSS) of >19 and prostate volume of 30–80 mL were enrolled in this prospective,
INTRODUCTION
BPH represents an important health problem in contemporary society and is the most common disease in male urological pathology, with a prevalence of 60% for patients aged 61–70 years, 70% for those aged 71–80 years and 80% for those aged >80 years [1,2]. Although benign, this disease with progressive evolution has a negative impact on the health-related quality of life (HRQL) of the patients, marked by obstructive and irritative LUTS. Surgical treatment for benign prostatic enlargement (BPE) continues to represent the second most frequent major surgical procedure in older
men, with three out of 10 men undergoing such an intervention.
The BPE endoscopic approach has used various therapeutic methods. According to the European Association of Urology (EAU) Guidelines 2009, monopolar TURP is the treatment of choice for prostates sized 30–80 mL [3]. However, this ‘gold-standard’ is marred by a significant morbidity and mortality rate, at 18% and 0.2%, respectively [4].
Recently, several alternatives have been introduced, aiming to improve the performances of TURP and to reduce its associated complications, which mainly
consist of bleeding, sepsis and TUR syndrome from fluid absorption.
Bipolar electrosurgical technology made transurethral electro-vaporization increasingly popular, especially after the development of the Gyrus® PlasmaKinetic® Tissue Management System (Gyrus Medical Ltd, Bucks, UK). This technique had already proved to be as effective as TURP for BOO, as it provided good long-term results and implied fewer early complications [5].
A new development of this technique, the TURis®-PVP using the Olympus® UES-40 Surgmaster generator (Olympus, Tokyo, Japan) and the ‘mushroom’ vapo-resection
G E A V L E T E E T A L .
electrode was recently introduced in clinical practice.
In the present study, we aimed to evaluate the efficiency, safety and short-term results of this new procedure and to compare it to standard TURP.
PATIENTS AND METHODS
A prospective, randomized study was performed to compare the short-term outcome of TURis-PVP and conventional TURP in patients with BPE with indications for surgery. The study was approved by the Local Ethics and Research Committee. In all, 155 patients with a mean (range) age of 66 (53– 81) years diagnosed with BPE and severe LUTS were enrolled (under approved written informed consent properly explaining the aims, methods, anticipated benefits, potential hazards and any other aspect of the study relevant to the patient’s decision to participate) and randomized by means of sealed envelopes containing consecutive numbers. In accordance with the informed consent, all patients were ‘blinded’ to treatment.
The inclusion criteria were represented by: a maximum urinary flow rate (Qmax) of <10 mL/
s, an International Prostate Symptom Score (IPSS) of >19 and a prostate volume (measured by TRUS) of 30–80 mL. The exclusion criteria consisted of: severe comorbidities, previous prostate surgery, history of prostate cancer, abnormal DRE and/ or increased PSA level.
A standard investigative protocol, which included general clinical examination with DRE, blood tests, PSA level measurement, urine culture, IPSS, HRQL, uroflowmetry
(evaluating Qmax) and abdominal
ultrasonography was applied in all cases. All patients received spinal anaesthesia and were operated on by the same surgeon after randomization.
Conventional TURP was performed in 80 cases using a 26 F Storz continuous flow monopolar resectoscope with a single wire loop and sterile water as irrigation fluid.
TURis-PVP, using the Olympus SurgMaster UES-40 bipolar generator, the special ‘mushroom’ type vapo-resection electrode and saline continuous flow irrigation was performed in 75 patients (Fig. 1). The spherical shape of the new type of electrode displaying a plasma corona on its surface was gradually moved into direct contact with the BPE tissue (the ‘hovering’ technique), thus producing a virtually blood-less vaporization at 280–320 W (Fig. 2). Several prostatic fragments were resected for pathological analysis. Coagulation of any haemorrhagic sources was practically concomitant, while larger vessels’ haemostasis was achieved by reducing the power of the generator to 120–140 W (Fig. 3). In all cases, a 20 F Foley catheter was placed at the end of the procedure.
During the follow-up, both the patients as well as the urologists performing the investigations were unaware of the treatment method applied in each case, to assure complete objectivity of the evaluation.
The 1, 3 and 6 months follow-ups assessed the IPSS, HRQL, Qmax and postvoid residual
urine volume (PVR) in all patients, and compared them between the series.
For statistical analysis of the data the Student’s t-test and the chi-squared tests were used, with P< 0.05 considered to indicate statistical significance.
RESULTS
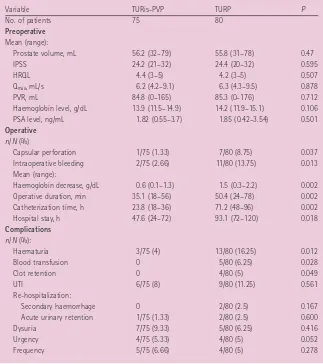
Table 1 shows the characteristics of the patients before surgery, which were similar between the groups.
TURis-PVP and TURP were successfully performed in all cases. Capsular perforation (P= 0.037) and significant intraoperative bleeding (P= 0.013) were more frequent during TURP (Table 1). The operative duration (P= 0.002), catheterization period (P= 0.002) and hospital stay (P= 0.012) were FIG. 1. Initial aspect at the beginning of the
TURis-PVP.
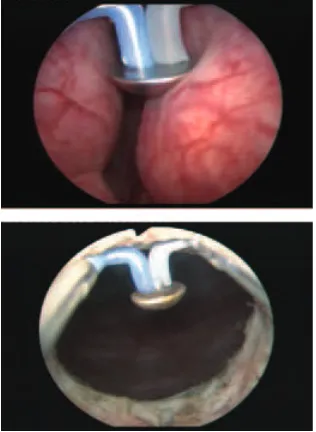
FIG. 2. Bladder neck (left) and median lobe (right) plasma vaporization.
T U R i s - P V P V S S T A N D A R D T U R P F O R B P E
significantly shorter for TURis-PVP than for standard TURP and monopolar TURP caused a higher decrease of the haemoglobin level (P= 0.002; Table 1).
The rate of complications represented by haematuria, UTIs and re-hospitalization for
acute urinary retention was higher for the TURP than for TURis-PVP (Table 1). Blood transfusion necessity, clot retention and re-hospitalization for secondary haemorrhage only occurred in the TURP group, with a rate of 6.25% (P= 0.028), 5% (P= 0.049) and 2.5% (P= 0.167), respectively (Table 1). The early
severe irritative complications were slightly more frequent in the TURis-PVP group (Table 1). The pathological analysis confirmed the BPH diagnosis in all cases, with no associated malignancy.
At the 1 month follow-up improvements in all the measured variables were better in the TURis-PVP group than the TURP group (Table 2). The differences remained stable and significant in all regards at the 3- and 6-month follow-ups At the 6-6-month evaluation of prostate volume by TRUS there were similar improvements for patients from both series, consisting of a decrease in prostate volume of 70.1% for TURis-PVP and 66.8% for TURP (Table 2). The PSA level measured at 1, 3 and 6 months also displayed a similar response in the two groups (Table 2).
DISCUSSION
Despite conventional monopolar TURP remaining the first-line treatment option for prostates of 30–80 mL, plasma energy in a saline environment is mentioned in the EAU Guidelines 2009 as a viable alternative [3].
The basis of TURis-PVP is represented by the ability of the UES-40 bipolar electrosurgical generator to produce a plasma corona on the surface of the spherical shape ‘mushroom’ type electrode. Plasma vaporization occurs by direct gentle contact with the tissue surface and performs concomitant haemostasis (Fig. 4).
Subjectively, this type of vaporization does not alter the visual characteristics of the tissues, enabling the surgeon to differentiate the adenomatous tissue, the muscular fibres of the prostatic capsula and the anatomical boundaries of the operating area with increased accuracy. Due to the lack of bleeding, visibility remains excellent throughout the procedure. The vaporization area emphasizes a remarkably smooth surface and sharp margins, with no irregularities or debris and no supplementary thermal lesions of the subjacent tissue (Fig. 5). The postoperative aspects of the prostatic fossa revealed a large passage, without obstruction, in every case (Fig. 6).
Some of the stages of conventional TURP were significantly reduced (concomitant vaporization and haemostasis, quick evacuation of the few resected tissue fragments), with the actual vaporization TABLE 1 The preoperative and operative characteristics and complication rates
Variable TURis-PVP TURP P
No. of patients 75 80
Preoperative
Mean (range):
Prostate volume, mL 56.2 (32–79) 55.8 (31–78) 0.47
IPSS 24.2 (21–32) 24.4 (20–32) 0.595
HRQL 4.4 (3–5) 4.2 (3–5) 0.507
Qmax, mL/s 6.2 (4.2–9.1) 6.3 (4.3–9.5) 0.878
PVR, mL 84.8 (0–165) 85.3 (0–176) 0.712
Haemoglobin level, g/dL 13.9 (11.5–14.9) 14.2 (11.9–15.1) 0.106
PSA level, ng/mL 1.82 (0.55–3.7) 1.85 (0.42–3.54) 0.501
Operative
n/N (%)
Capsular perforation 1/75 (1.33) 7/80 (8.75) 0.037
Intraoperative bleeding 2/75 (2.66) 11/80 (13.75) 0.013
Mean (range):
Haemoglobin decrease, g/dL 0.6 (0.1–1.3) 1.5 (0.3–2.2) 0.002
Operative duration, min 35.1 (18–56) 50.4 (24–78) 0.002
Catheterization time, h 23.8 (18–36) 71.2 (48–96) 0.002
Hospital stay, h 47.6 (24–72) 93.1 (72–120) 0.018
Complications
n/N (%):
Haematuria 3/75 (4) 13/80 (16.25) 0.012
Blood transfusion 0 5/80 (6.25) 0.028
Clot retention 0 4/80 (5) 0.049
UTI 6/75 (8) 9/80 (11.25) 0.561
Re-hospitalization:
Secondary haemorrhage 0 2/80 (2.5) 0.167
Acute urinary retention 1/75 (1.33) 2/80 (2.5) 0.600
Dysuria 7/75 (9.33) 5/80 (6.25) 0.416
Urgency 4/75 (5.33) 4/80 (5) 0.052
Frequency 5/75 (6.66) 4/80 (5) 0.278
G E A V L E T E E T A L .
occupying most of the operating time and increased the efficiency of TURis-PVP.
The power of the generator was adapted to tissue characteristics and consistency, providing the surgeon with additional technical flexibility: 320 W for fibrous tissue, 280–290 W for the average BPE tissue, 240 W for remaining BPE small fragments close to the capsula or apex and 120–140 W for coagulation.
Several studies involving plasma vaporization using the PlasmaKinetic Tissue Management System have been performed in recent years, aiming to compare the method with standard TURP in a prospective, randomized fashion. Patients included in the following trials presented similar baseline characteristics with those of the present series.
The study by Karaman et al. [6] on 75 patients determined better outcomes for the PlasmaKinetic vaporization of prostate (PKVP) during a 1-year follow-up. However, the present TURis-PVP cases, with a larger mean prostate volume (56.2 vs 50 mL), had a shorter operative duration (35.1 vs 40.3 min), a reduced catheterization period (23.8 vs 35 h); and improved IPSS (4.8 vs 5 and 5 vs 6,
respectively) and Qmax (22.3 vs 17 mL/s and
21.8 vs 17 mL/s, respectively) at the 3- and 6-month follow-ups.
A study by Patankar et al. [7] on 105 patients randomized for PKVP and TURP described an increased complication rate and inferior results at 21 days in the PKVP group compared with the present TURis-PVP data at 1 month (haematuria in 5.77% vs 4% of the cases and UTIs in 11.54% vs 8%, operative time 49.99 vs 35.1 min, IPSS 6.11 vs 4.4 and Qmax 19.16 vs 22.7 mL/s).
In a study published by Dincel et al. [8] on 21 PKVP patients with lower mean preoperative PVR (54 vs 84.8 mL), the postoperative improvement was better at the 3-month follow-up for the TURis-PVP patients (19.5 vs 18.0 mL).
TURis-PVP is a development of the previously described electro-vaporization of the prostate technique, with the benefits of bipolar technology, remarkably effective plasma-producing ‘mushroom’ electrode and high-power vaporization. Consequently, the mean reduction in prostate volume was substantially improved in the present series compared with published data (70.1% vs
42.5%, respectively) [9]. Differences remained consistent when comparing with the PKVP technique (70.1% vs 52.38%, respectively) [8]. At the same time, it is only fair to say that, despite the very promising initial short-term results, long-term studies assessing follow-up variables are mandatory to confirm the advantages of this recently introduced method.
Bipolar TURP using the same TURis system as the one in the present study was used in a trial on 45 patients with BPE with similar preoperative characteristics, published by Ho
et al. [10]. Results included longer operative
duration (42 vs 35.1 min) and higher haemoglobin decrease (1.4 vs 0.6 g/dL), as well as inferior Qmax (13.6 vs 22.7 mL/s at 1
month, 19.6 vs 22.3 mL/s at 3 month and 18.7 TABLE 2 Results at the 1-, 3- and 6-months follow-ups
Results, mean (range) TURis-PVP TURP P
IPSS
1 month 4.4 (1–8) 8.3 (2–14) <0.001
3 months 4.8 (1–9) 8.6 (3–16) <0.001
6 months 5 (1–9) 9.1 (3–17) 0.020
HRQL
1 month 1.2 (1–2) 1.4 (1–3) 0.046
3 months 1.4 (1–2) 1.6 (1–4) 0.015
6 months 1.4 (1–3) 1.7 (1–4) 0.042
Qmax, mL/s
1 month 22.7 (13.7–34.2) 20.5 (12.3–31.5) 0.023
3 months 22.3 (12.9–34.9) 20.0 (12.6–30.9) 0.021
6 months 21.8 (13.4–33.7) 19.3 (11.2–31.1) 0.018
PVR, mL
1 month 19.0 (0–36) 30.5 (0–45) 0.294
3 months 18.0 (0–33) 28.5 (0–52) 0.311
6 months 16.0 (0–41) 26.0 (0–64) 0.281
Prostate volume, mL
6 months 16.8 (12–23) 18.5 (14–22) 0.181
PSA level, ng/mL
1 month 1.10 (0.31–1.64) 1.18 (0.28–1.72) 0.483
3 months 0.93 (0.27–1.57) 0.97 (0.30–1.65) 0.445
6 months 0.74 (0.21–1.53) 0.80 (0.19–1.63) 0.499
FIG. 5. Smooth surface of the prostatic capsula after plasma vaporization.
T U R i s - P V P V S S T A N D A R D T U R P F O R B P E
vs 21.8 mL/s at 6 months) and IPSS (13.6 vs 4.4 at 1 month, 9.0 vs 4.8 at 3 months and 7.2 vs 5 at 6 months) improvements for the bipolar TURP series.
The comparison with standard TURP remains imperative and published data confirm the significant differences in efficiency, complication rates and results.
A prospective multicentre evaluation of 10 654 patients with initially similar obstructive profile emphasized important advantages for the TURis-PVP patients regarding the operating time and hospital stay (52.4 vs 35.1 min and 192 vs 47.6 h) [11]. The average catheterization time was described in the published data as
significantly longer compared with TURis-PVP (23.8 vs 115.2 h) [12]. The mean reported IPSS decrease for TURP (18.8–7.2) was inferior to that of the TURis-PVP series (24.2–5) [13].
The greatest weakness of standard TURP remains the significant complication rate, which did not occur in the present TURis-PVP group (2.9% transfusion rate, 1.4% TUR syndrome rate, 5.8% failure rate and 0.1% mortality rate [11]).
Longer follow-up studies will be needed to clarify the place of TURis-PVP in the armamentarium of BPE endoscopic treatment. However, the long-term follow-up of patients treated by its predecessor, the PKVP, have already shown good and stable results with IPSS improvements from 21 to 7.1 and 7.6, and Qmax increase from 6 to 12.5
and 14.4 mL/s at 2 and 3 years, respectively [14].
In conclusion, TURis-PVP represents a promising endoscopic treatment alternative for patients with BPE, with good efficacy, reduced morbidity, fast recovery and satisfactory follow-up. Longer follow-up periods and more extensive trials will be required to establish the long-term advantages and general viability of the method. However, TURis-PVP seems to provide significant progresses in terms of short-term outcome compared to its predecessor, the PKVP, as well to bipolar TURP
and even conventional TURP. The short period of catheterization and hospital stay, reduced rate of complications and significantly improved follow-up features (IPSS, HRQL and Qmax) are reliable arguments in favour of this
new procedure.
CONFLICT OF INTEREST
None declared.
REFERENCES
1 Berry SJ, Coffey DS, Walsh PC, Ewing
LL. The development of human benign prostatic hyperplasia with age. J Urol 1984; 132: 474–9
2 Carter HB, Coffey DS. The prostate: an
increasing medical problem. Prostate 1990; 16: 39–48
3 Oelke M, Alivizatos G, Emberton M
et al. Guidelines on benign prostatic hyperplasia. In Parsons KF, Irani J, Chapple
CR et al. eds. European Association of
Urology Pocket Guidelines, Arnhem:
European Association of Urology, 2009: 90–7
4 Mebust WK, Holtgrewe HL, Cockett AT,
Peters PC. Transurethral prostatectomy:
immediate and postoperative
complications. A comparative study of 13 participating institutions evaluating 3885 patients. J Urol 1989; 141: 243–7
5 Hon NH, Brathwaite D, Hussain Z
et al. A prospective, randomized trial
comparing conventional transurethral prostate resection with PlasmaKinetic vaporization of the prostate: physiological changes, early
complications and long-term follow-up.
J Urol 2006; 176: 205–9
6 Karaman MI, Kaya C, Ozturk M, Gurdal
M, Kirecci S, Pirincci N. Comparison
of transurethral vaporization using PlasmaKinetic energy and transurethral resection of prostate: 1-year follow-up.
J Endourol 2005; 19: 734–7
7 Patankar S, Jamkar A, Dobhada S,
Gorde V. PlasmaKinetic Superpulse
transurethral resection versus conventional transurethral resection of prostate. J Endourol 2006; 20: 215–9
8 Dincel C, Samli MM, Guler C, Demirbas
M, Karalar M. Plasma kinetic
vaporization of the prostate: clinical evaluation of a new technique. J Endourol 2004; 18: 293–8
9 Kupeli S, Soygur T, Yilmaz E,
Aytaç S. Effect of transurethral
electrovaporization of the prostate on serum prostate specific antigen concentration. BJU Int 1999; 83: 783– 5
10 Ho H, Yip SK, Cheng CW, Foo KT.
Bipolar transurethral resection of prostate in saline: preliminary report on clinical efficacy and safety at 1 year. J Endourol 2006; 20: 244–7
11 Reich O, Gratzke C, Bachman A et al.
Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 2008; 180: 246– 9
12 Shishido T, Enomoto K, Fujita N et al.
[Comparison of clinical results between TUR-P and holmium laser enucleation of the prostate (HoLEP) based on the initial experience]. Nippon Hinyokika Gakkai Zasshi 2008; 99: 543–50
13 Marszalek M, Ponholzer A, Pusman M,
Berger I, Madersbacher S. Transurethral resection of the prostate. Eur Urol Suppl 2009; 8: 504–12
14 Kaya C, Ilktac A, Gokmen E, Ozturk M,
Karaman IM. The long-term results of transurethral vaporization of the prostate using plasmakinetic energy. BJU Int 2007; 99: 845–8
Correspondence: Bogdan Geavlete, Department of Urology, Saint John Emergency Clinical Hospital, Vitan-Barzesti 13, Sector 4, 042122, Bucharest, Romania.
e-mail: [email protected]
Abbreviations: TURis-PVP, trasurethral resection in saline plasma vaporization of the prostate; BPE, benign prostatic enlargement; EAU, European Association of Urology; IPSS, International Prostate Symptom Score; HRQL, health-related quality of life score; Qmax,