Prevalensi tinggi dari Vitamin D Kekurangan Hamil
Wanita: Sebuah Nasional Cross-Sectional Survei
Stefanie Vandevijvere1*, Sihame Amsalkhir2, Herman Van Oyen1, Rodrigo Moreno-Reyes2
1 Department of Public Health and Surveillance, Scientific Institute of Public Health, Brussels,
Belgium, 2 Department of Nuclear Medicine, Hoˆpital Erasme, Universite´ Libre de Bruxelles,
Brussels, Belgium
High Prevalence of Vitamin D Deficiency in Pregnant
Women: A National Cross-Sectional Survey
Stefanie Vandevijvere1*, Sihame Amsalkhir2, Herman Van Oyen1, Rodrigo Moreno-Reyes2
1 Department of Public Health and Surveillance, Scientific Institute of Public Health, Brussels,
Belgium, 2 Department of Nuclear Medicine, Hoˆpital Erasme, Universite´ Libre de Bruxelles,
Brussels, Belgium
PROQUEST
Nama : Eliza Eka Nurani
Nim : G2B013013
SI ILMU GIZI
FAKULTAS ILMU KEPERAWATAN DAN KESEHATAN
Prevalensi tinggi dari Vitamin D Kekurangan Hamil
Wanita: Sebuah Nasional Cross-Sectional Survei
Stefanie Vandevijvere1*, Sihame Amsalkhir2, Herman Van Oyen1, Rodrigo Moreno-Reyes2
1 Department of Public Health and Surveillance, Scientific Institute of Public Health, Brussels,
Belgium, 2 Department of Nuclear Medicine, Hoˆpital Erasme, Universite´ Libre de Bruxelles,
Brussels, Belgium
Abstrak
Peningkatan jumlah studi menunjukkan bahwa kekurangan vitamin D selama kehamilan dikaitkan dengan beberapa hasil yang merugikan kesehatan pada ibu, neonatus dan anak-anak. Tidak ada data negara perwakilan tersedia di status vitamin D ibu hamil di Eropa. Tujuan dari penelitian ini adalah untuk memperkirakan prevalensi defisiensi vitamin D pada wanita hamil Belgia dan untuk menilai faktor-faktor penentu status vitamin D pada trimester pertama dan ketiga kehamilan. Para wanita dipilih melalui multi-tahap desain proporsional untuk ukuran sampling. Sampel darah dikumpulkan dan kuesioner selesai tatap muka. 55 klinik kebidanan dipilih secara acak dan 1.311 wanita hamil berpartisipasi dalam studi. Median serum 25-hydroxyvitamin D [25- (OH) D] konsentrasi secara signifikan lebih rendah pada trimester pertama (20,4 ng / ml) dibandingkan pada trimester ketiga (22,7 ng / ml). Dari semua wanita, 74,1% (95% CI = 71,8-76,5%) adalah vitamin D yang cukup (25- (OH) D, 30 ng / ml), 44,6% (95% CI = 41,9-47,3%) yang kekurangan vitamin D (25- (OH) D, 20 ng / ml), sementara 12,1% (95% CI = 10,3-13,8%) yang sangat kekurangan vitamin D (25- (OH) D, 10 ng / ml). Dari semua wanita termasuk, 62,0% dilaporkan mengambil multivitamin D-mengandung vitamin, yang hanya 24,2% mulai mengambil orang-orang sebelum kehamilan. Risiko kekurangan vitamin D (25- (OH) D, 20 ng / ml) secara signifikan lebih tinggi bagi perempuan kurang berpendidikan dan wanita yang melaporkan tidak akan pada hari libur untuk iklim cerah. Risiko kekurangan vitamin D yang parah (25-(OH) D, 10 ng / ml) menurun untuk wanita yang melaporkan konsumsi alkohol selama kehamilan, menurun dengan lebih sering menggunakan tabir surya lotion dan meningkat untuk perokok dan wanita yang melaporkan preferensi untuk bayangan. Kesimpulannya, kekurangan vitamin D sangat umum di kalangan wanita hamil di Belgia dan ini menimbulkan kekhawatiran tentang konsekuensi kesehatan untuk ibu dan anak tersebut. Sebuah strategi skrining ditargetkan untuk mendeteksi dan mengobati wanita yang berisiko tinggi kekurangan vitamin D yang parah diperlukan di Belgia dan di Eropa.
Pengantar
Manusia mendapatkan vitamin D (cholecalciferol) dari paparan sinar matahari, diet dan suplemen makanan. Seperti beberapa makanan mengandung atau yang diperkaya dengan vitamin D (seperti hati, ikan berlemak, telur, susu dan produk susu, susu kedelai, mentega, margarin), sintesis kulit vitamin D yang disebabkan oleh radiasi ultraviolet B (UVB) adalah penentu utama status vitamin D pada populasi [23]. Vitamin D sekali disintesis di kulit dimetabolisme menjadi 25- dihydroxyvitamin D [25- (OH) D] dalam hati. Karena lagi paruhnya, (OH) D dianggap yang terbaik bio-penanda status vitamin D. 25-(OH) D kemudian dimetabolisme di ginjal oleh 1- hidroksilase untuk aktif hormon steroid 1,25-dihydroxyvita- min D [1,25 (OH) 2D]. Beberapa modifikasi metabolisme vitamin D terjadi selama kehamilan.
Ekspresi 1-a hidroksilase meningkat pada ginjal dan plasenta dan konsentrasi serum 1,25 (OH) 2D meningkat pada kehamilan normal dari yang pertama trimester ketiga. Peran 1,25 (OH) 2D selama kehamilan untuk meningkatkan penyerapan kalsium usus sejak lama diakui [24].
Cut-off poin digunakan untuk menentukan insufisiensi vitamin D dan kekurangan yang tidak mapan dan tetap kontroversial. Namun demikian ada konsensus untuk mempertimbangkan serum 25- (OH) D di bawah 20 ng / ml sebagai tidak cukup rendah [25], dan beberapa bukti menunjukkan bahwa nilai-nilai yang lebih tinggi dari 30 ng / ml mungkin terkait dengan hasil kesehatan yang lebih baik pada populasi dewasa. [26,27]. Ketidakpastian mengenai serum optimal 25- (OH) D konsentrasi tion pada wanita hamil bahkan lebih tinggi. Selama nilai-nilai yang diusulkan tidak divalidasi dalam uji klinis kontroversi akan tetap [28].
Ada kekhawatiran tentang konsekuensi kesehatan tingginya prevalensi kekurangan vitamin D di seluruh dunia antara populasi umum, termasuk wanita hamil. Kecukupan arus vitamin D rekomendasi diet untuk mencapai status vitamin D yang optimal selama kehamilan telah dipertanyakan [24]. Meskipun survei kecil sebelumnya menunjukkan bahwa kekurangan vitamin D pada wanita hamil adalah umum di Eropa [29,30], tidak ada perkiraan negara-lebar terpercaya status vitamin D pada wanita hamil di negara-negara Eropa. Oleh karena itu tujuan dari penelitian ini adalah untuk melaksanakan nasional pertama perwakilan survei sampel acak pada status vitamin D pada wanita hamil di negara Eropa dan untuk menilai faktor-faktor penentu status vitamin D pada trimester pertama dan ketiga kehamilan.
Metode
Pernyataan Etika
Penelitian ini dilakukan sesuai dengan pedoman yang ditetapkan dalam Deklarasi Helsinki dan semua prosedur yang melibatkan subyek manusia telah disetujui oleh komite etika medis rumah sakit Erasme di Brussels. Subyek disediakan persetujuan tertulis untuk berpartisipasi dalam penelitian ini.
Sampling
Target populasi survei terdiri semua wanita hamil di Belgia selama pertama dan trimester ketiga kehamilan pada periode September 2010 hingga Juni 2011. Para wanita dipilih sesuai dengan multi-stage proporsional-to-desain ukuran sampel stratified sebagai direkomendasikan untuk studi menilai kekurangan yodium [31]. Negara ini dibagi menjadi dua wilayah. Di masing-masing daerah klinik kebidanan diperintahkan oleh provinsi dan ukuran berdasarkan jumlah pengiriman selama satu tahun terakhir dan 60 kelompok dari 4 klinik dipilih per wilayah menggunakan sampling sistematik untuk memiliki klinik pengganti yang cukup dalam kasus beberapa menolak untuk berpartisipasi. Dari ini 60 cluster, 30 cluster dipilih secara acak dan dalam setiap cluster klinik pertama diundang untuk berpartisipasi. Di setiap klinik semua dokter kandungan gynaecologist- diundang untuk berpartisipasi dalam rangka meratakan efek ginekolog mungkin. Tujuannya adalah untuk memasukkan 22 perempuan dalam setiap cluster yang 11 pada trimester pertama dan 11 pada trimester ketiga kehamilan.
Pengumpulan data
sosio-demografi dan sosial ekonomi, merokok dan konsumsi alkohol selama kehamilan dan selama 4 minggu sebelum wawancara, penyakit dan pengobatan dan penggunaan suplemen makanan selesai di tatap muka wawancara yang dilakukan oleh perawat studi. Perempuan dari Aljazair, Mesir, Libya, Maroko, Sudan, Tunisia, dan Sahara Barat dianggap keturunan Afrika Utara. Untuk semua wanita termasuk dalam studi ini, indeks massa tubuh (BMI) diperoleh dari berat dan tinggi badan dicatat oleh dokter kandungan selama konsultasi prenatal pertama di awal trimester pertama kehamilan. Trimester pertama BMI digunakan sebagai proxy untuk hamil BMI untuk perempuan trimester pertama dan ketiga kehamilan.
Analisis Sampel
Sekitar 5 ml darah utuh dikumpulkan oleh venipuncture dalam tabung non-heparinized. Aliquots serum kemudian disimpan pada - 80C untuk analisa lebih lanjut. Serum 25-hydroxyvitamin D (25- (OH) D) konsentrasi diukur dengan radioimmunoassay (DIASORIN, Stillwater, MN, USA).
Analisis Statistik
Analisis statistik dilakukan dengan menggunakan STATA 10.1 (StataCorp, Texas, USA). Sebagai serum 25- (OH) D tidak terdistribusi normal, metode non-parametrik digunakan. Median digunakan sebagai ukuran tendensi sentral.
Perbedaan antar daerah, dan kelompok usia trimester dieksplorasi menggunakan dua sampel Wilcoxon rank-sum test atau Kruskal- Wallis kesetaraan-of-populasi peringkat tes.
Kemungkinan memiliki serum 25- (OH) D konsentrasi lebih rendah dari 20 ng / ml (kekurangan vitamin D) versus status vitamin D non kekurangan diperkirakan melalui regresi logistik saat memasuki variabel-variabel berikut sebagai prediktor dalam model: musim, usia, trimester kehamilan, wilayah, BMI, perilaku merokok, konsumsi alkohol, penggunaan vitamin D yang mengandung suplemen makanan, konsumsi ikan, susu dan konsumsi produk susu, tingkat pendidikan, etnis, paritas, paparan sinar matahari selama hari kerja, paparan sinar matahari selama hari-hari akhir pekan, penggunaan tabir surya lotion, penggunaan solarium, bayangan atau preferensi matahari dan kadang-kadang terjadi pada hari libur untuk iklim cerah (ya / tidak pertanyaan). Selain kemungkinan memiliki serum 25- (OH) D konsentrasi yang lebih rendah dari 10 ng / ml (kekurangan vitamin D yang parah) versus status kekurangan vitamin D non parah diperkirakan melalui regresi logistik saat memasuki prediktor yang sama dalam model.
Hasil
Daerah
Brussels ** Flanders ** Wallonia Umur (tahun) trimester 1 trimester 3 trimester 1 trimester 3 trimester 1 3 trimester
Regions
Brussels** Flanders** Wallonia
Age(years ) 1st trimester 3rd trimester 1st trimester
rd st
3rd trimester
15–20 7 2 11 10
21–25 34 27 77 51
56 73
26–30 41 39 108 149
76 58
31–35 34 53 69 75
49 45
36–40 14 14 23 19
13 24
41–45 2 3 1 3
3 2
Total 132 138 289 307
218 219
Tabel 2. Karakteristik ibu hamil termasuk dalam studi (n = 1.311) (survei Belgia nasional status vitamin D pada wanita hamil, 2010-2011).
Dari semua wanita hamil termasuk, 640 berada di pertama, 666 berada di ketiga dan 2 berada pada trimester kedua kehamilan. Untuk informasi 3 wanita di trimester hilang. Untuk 41,7% dari perempuan ini adalah kehamilan pertama mereka (yang tidak diketahui untuk 0,4% dari wanita), sedangkan untuk 45,6% dari wanita ini akan menjadi anak pertama mereka (status tidak diketahui untuk 1,4% dari wanita). Kurang lebih 4% dari wanita dalam sampel telah mengalami keguguran sebelum setidaknya sekali. Untuk 77,6% dari wanita kehamilan mereka direncanakan (tidak diketahui untuk 3,3% dari wanita).
trimester ketiga kehamilan, tetapi prevalensi kekurangan vitamin D yang parah lebih tinggi pada trimester ketiga.
Untuk kedua wanita trimester pertama dan ketiga ada kecenderungan musiman yang jelas dalam mean serum 25- (OH) D konsentrasi dengan konsentrasi terendah di musim dingin dan tertinggi selama musim semi dan panas, sedangkan penurunan lagi di musim gugur. Perempuan asal etnis lain yang kekurangan vitamin D (25- (OH) D konsentrasi , 20 ng / ml) sepanjang tahun, kecuali selama musim panas untuk wanita trimester ketiga.
Dari semua wanita termasuk, 76,2% dilaporkan mengambil setidaknya 1 multivitamin selama kehamilan. Untuk 62,0% dari mereka yang Tamin multivi- terkandung vitamin D. Pada trimester pertama dan ketiga kehamilan persentase wanita yang menggunakan multivitamin yang mengandung vitamin D adalah masing-masing 52,6% dan 72,3%. Hanya 24,2% dari semua wanita hamil mulai mengambil multivitamin sebelum kehamilan, sementara 46,6% dari wanita-wanita mulai mengambil vitamin multi dalam trimester pertama kehamilan. Risiko kekurangan vitamin D (25- (OH) D, 20 ng / ml) meningkat secara signifikan dengan BMI dan secara signifikan lebih tinggi bagi perempuan yang dilaporkan tidak mengambil vitamin D yang mengandung vitamin multi (Tabel 4). Selain risiko kekurangan vitamin D adalah tiga kali lipat lebih tinggi pada wanita keturunan Asia, enam kali lipat lebih tinggi bagi perempuan Afrika Utara dan lima kali lipat lebih tinggi bagi perempuan keturunan Hispanik dibandingkan dengan bule. Risiko insufisiensi vitamin D secara signifikan lebih rendah bagi perempuan yang lebih berpendidikan dan bagi orang-orang yang melaporkan terjadi libur untuk iklim cerah. Selain risiko kekurangan vitamin D secara signifikan lebih rendah di musim panas, semi dan musim gugur dibandingkan dengan musim dingin. Risiko kekurangan vitamin D yang parah (25- (OH) D, 10 ng / ml) secara signifikan lebih rendah di antara ketiga dari trimester pertama ibu hamil (Tabel 5). Risiko penambahan kekurangan vitamin D yang parah meningkat untuk wanita yang melaporkan tidak mengambil vitamin D yang mengandung multivitamin, yang non asal Kaukasia dan yang melaporkan merokok selama kehamilan. Di sisi lain risiko kekurangan vitamin D yang parah menurun bagi perempuan yang melaporkan konsumsi alkohol selama kehamilan. Menariknya, risiko kekurangan vitamin D yang parah menurun dengan lebih sering menggunakan tabir surya lotion dan meningkat untuk wanita yang melaporkan preferensi untuk bayangan (Tabel 5). Paparan sinar matahari selama seminggu dan akhir pekan hari, dan konsumsi susu dan produk susu tidak terkait dengan baik kekurangan vitamin D yang parah atau normal.
Diskusi
status vitamin D di banyak negara Eropa. Hubungan status vitamin D dengan BMI telah dikaitkan untuk penyimpanan berlebihan vitamin D dalam jaringan lemak penurunan konsentrasi sehingga serum [47]. Etnisitas juga penentu utama status vitamin D dalam penelitian ini, seperti dilaporkan sebelumnya dalam populasi orang dewasa [32] dan pada wanita hamil [29,48,49]. Di Belgia, wanita hamil dari etnis yang berbeda memiliki konsentrasi vitamin D secara substansial lebih rendah dari wanita Kaukasia dan kekurangan vitamin D sepanjang tahun kecuali selama musim panas untuk wanita trimester ketiga. Selain tingkat pendidikan dikaitkan dengan status vitamin D pada populasi wanita hamil kami. Merokok meningkatkan risiko kedua kekurangan vitamin D dan kekurangan vitamin D yang parah; mekanisme ini tampaknya tidak jelas [50]. Menariknya risiko kekurangan vitamin D yang parah lebih rendah di antara perempuan yang melaporkan konsumsi alkohol selama kehamilan. Yang terakhir telah ditemukan juga di antara pria Korea [51]. Variabel yang mempengaruhi pembentukan previtamin D3 di kulit termasuk pigmentasi kulit dan intensitas cahaya UV matahari [52- 55]. Di musim panas, orang-orang berkulit terang yang menghabiskan setidaknya 15 menit di luar siang hari dengan tangan dan wajah terkena akan memiliki kadar vitamin D yang memadai mereka. Lotion tabir surya mencegah radiasi UV dari mencapai kulit dan karena itu mungkin mengurangi produksi vitamin D kulit [56]. Namun, penelitian lain menemukan efek ini menjadi hanya kecil [57]. Di Belgia, wanita hamil yang dilaporkan terjadi pada hari libur untuk iklim cerah memiliki risiko yang lebih rendah dari kekurangan vitamin D dan wanita yang dilaporkan menggunakan tabir surya lotion memiliki risiko yang lebih rendah dari kekurangan vitamin D yang parah. Yang terakhir ini mungkin karena fakta bahwa wanita yang menggunakan tabir surya lotion lebih sering terkena sinar matahari. Wanita yang melaporkan preferensi untuk bayangan memiliki risiko lebih tinggi kekurangan vitamin D yang parah dalam penelitian kami.
Asupan vitamin D selama kehamilan dan menyusui tidak diketahui, meskipun tampaknya lebih besar dari rekomendasi diet saat 400 IU / d atau 10 mg / d [58]. Beberapa studi menunjukkan bahwa kebutuhan makanan selama kehamilan dan menyusui mungkin setinggi 6000 IU / d [59] dan mengakui bahwa setidaknya 1500-2000 IU / d vitamin D mungkin diperlukan untuk mempertahankan tingkat darah dari 25 (OH) D di atas 30 ng / ml [24]. Seperti yang penulis mengakui bahwa bukti untuk mengusulkan intake tersebut langka dan selama manfaat kesehatan dari memiliki kadar serum 25 (OH) D lebih tinggi dari 30 ng / ml tidak jelas didirikan terutama pada wanita hamil, Belgia dewan unggul Kesehatan masih merekomendasikan suplemen vitamin D dari 20 mg / hari atau 800 IU selama kehamilan [58]. Namun, isi D vitamin multivitamin untuk wanita hamil di Belgia hanya 400 IU menunjukkan bahkan rekomendasi ini tidak diikuti perempuan sebagai hamil hanya mengambil satu pil multivitamin sehari. Dengan tidak adanya data survei dari negara-negara Eropa lainnya,
hamil yang berisiko tinggi kekurangan vitamin D yang parah. Selain kandungan vitamin D saat vitamin multi untuk kehamilan, 400 IU, bahkan tidak sesuai dengan rekomendasi Belgia saat ini 800 IU per hari, oleh karena itu langkah bijaksana setidaknya harus untuk meningkatkan kandungan vitamin D dalam multivitamin bagi ibu hamil untuk 800 IU.
Kesimpulannya, meskipun bahwa lebih dari 60% dari wanita hamil dilaporkan mengambil multivitamin yang mengandung vitamin D, kekurangan vitamin D sangat umum di kalangan wanita hamil di Belgia dan hingga 12% dari wanita hamil yang sangat kekurangan vitamin D. Sebuah strategi skrining ditargetkan untuk mendeteksi dan mengobati wanita yang berisiko tinggi kekurangan vitamin D yang parah jelas dibutuhkan di Belgia dan di negara-negara Eropa lainnya. Sementara beberapa studi observasional menunjukkan korelasi antara insufisiensi vitamin D dan kesehatan ibu dan neonatal sakit, bukti eksperimental dari suplemen uji klinis diperlukan untuk menginformasikan kebijakan kesehatan.
Ucapan Terima Kasih
Para penulis mengakui rumah sakit dan dokter ahli kandungan yang setuju untuk berpartisipasi dan semua wanita hamil yang berpartisipasi. Kami juga ingin berterima kasih B. Hauquier dan D. Martin untuk vitamin D analisis laboratorium.
Penulis Kontribusi
Disusun dan dirancang percobaan: SV RM-R. Melakukan percobaan: SA. Menganalisis data: SV. Kontribusi reagen / bahan / alat analisis: SV RM-R SA. Menulis kertas: SV RM-R HV.
Referensi
1. Valimaki VV, Alfthan H, Lehmuskallio E, Loyttyniemi E, Sahi T, et al. (2004) Vitamin D status
as a determinant of peak bone mass in young Finnish men. J Clin Endocrinol Metab 89: 76–80.
2. Ooms ME, Roos JC, Bezemer PD, van der Vijgh WJ, Bouter LM, et al. (1995) Prevention of bone loss by vitamin D supplementation in elderly women: a randomized double-blind trial. J Clin
Endocrinol Metab 80: 1052–1058.
3. Lips P, van Schoor NM (2011) The effect of vitamin D on bone and osteoporosis. Best
Pract Res Clin Endocrinol Metab 25: 585–591.
4. Jackson C, Gaugris S, Sen SS, Hosking D (2007) The effect of cholecalciferol (vitamin D3) on the risk of fall and fracture: a meta-analysis. QJM 100: 185–192. 5. Pettifor JM, Prentice A (2011) The role of vitamin D in paediatric bone health.
Best Pract Res Clin Endocrinol Metab 25: 573–584.
6. Bhan A, Rao AD, Rao DS (2010) Osteomalacia as a result of vitamin D
deficiency. Endocrinol Metab Clin North Am 39: 321–31.
7. Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, et al. (2007) Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. Am J Prev Med 32: 210–216. 8. Garland CF, Gorham ED, Mohr SB, Grant WB, Giovannucci EL, et al. (2007) Vitamin D and
prevention of breast cancer: pooled analysis. J Steroid Biochem Mol Biol 103: 708–711.
9. Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP (2007) Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr 85: 1586–1591.
10. Grant WB, Garland CF (2002) Evidence supporting the role of vitamin D in reducing the risk of cancer. J Intern Med 252: 178–179.
11. Grant WB, Garland CE (2003) Vitamin D as a risk reduction factor for colorectal cancer. Am Fam Physician 67: 465.
association of low serum 25-hydroxyvitamin d and 1,25- dihydroxyvitamin d levels with all-cause
and cardiovascular mortality. Arch Intern Med 168: 1340–1349.
13. Zittermann A (2003) Vitamin D in preventive medicine: are we ignoring the evidence? Br J Nutr 89: 552–572.
14. Holick MF (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80:
1678S–1688S.
15. Martini LA, Wood RJ (2006) Vitamin D status and the metabolic syndrome. Nutr Rev 64: 479–486.
16. Dror DK (2011) Vitamin D status during pregnancy: maternal, fetal, and postnatal outcomes.
Curr Opin Obstet Gynecol 23: 422–426.
17. Dror DK, Allen LH (2010) Vitamin D inadequacy in pregnancy: biology, outcomes, and interventions. Nutr Rev 68: 465–477.
18. Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, et al. (2007) High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates. J Nutr 137: 447–452.
19. Bodnar LM, Krohn MA, Simhan HN (2009) Maternal vitamin D deficiency is associated with bacterial vaginosis in the first trimester of pregnancy. J Nutr 139:
1157–1161.
20. Lucas RM, Ponsonby AL, Pasco JA, Morley R (2008) Future health implications of prenatal and early-life vitamin D status. Nutr Rev 66: 710–720.
21. Barrett H, Mcelduff A (2010) Vitamin D and pregnancy: An old problem revisited. Best Pract
Res Clin Endocrinol Metab 24: 527–539.
22. Hensel KJ, Randis TM, Gelber SE, Ratner AJ (2011) Pregnancy-specific association of vitamin D deficiency and bacterial vaginosis. Am J Obstet Gynecol
204: 41–49.
23. Holick MF (2007) Vitamin D deficiency. New Engl J Med 357: 266–281.
24. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, et al. (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:
1911–1930.
25. Grant WB, Holick MF (2005) Benefits and requirements of vitamin D for optimal health: a
review. Altern Med Rev 10: 94–111.
26. Grant WB, Boucher BJ (2011) Requirements for Vitamin D across the life span. Biol Res Nurs 13: 120–133.
27. Holick MF (2010) Vitamin D: extraskeletal health. Endocrinol Metab Clin
North Am 39: 381–400.
28. Grant WB, Holick MF (2005) Benefits and requirements of vitamin D for optimal health: a
review. Altern Med Rev 10: 94–111.
29. van der Meer IM, Karamali NS, Boeke AJ, Lips P, Middelkoop BJ, et al. (2006) High prevalence of vitamin D deficiency in pregnant non-Western women in The Hague, Netherlands. Am J Clin Nutr 84: 350–353.
30. Milman N, Hvas AM, Bergholt T (2011) Vitamin D status during normal pregnancy and
postpartum. A longitudinal study in 141 Danish women. J Perinat Med 40: 57–61.
31. Sullivan KM, Mei S, Maberley G (2000) penilaian kemih Yodium: Sebuah panduan tentang Survey dan metode laboratorium. UNICEF / PAMM.
32. Moreno-Reyes R, Carpentier YA, Boelaert M, El Moumni K, Dufourny G, et al. Defisiensi D (2009) Vitamin dan hiperparatiroidisme dalam kaitannya dengan etnis:
survei cross-sectional pada orang dewasa yang sehat. Eur J Nutr 48: 31-37.
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868
Belgia wanita osteoporosis postmenopause. BMC Public Health 7: 64.
34. Bouillon RA, Auwerx JH, Lissens WD, Pelemans WK (1987) Status Vitamin D pada orang tua: musiman kekurangan substrat menyebabkan defisiensi 1,25-dihidroksikolekalsiferol. Am J Clin Nutr 45: 755-763.
35. HUYBRECHTS saya, Lin Y, De KW, Sioen saya, Mouratidou T, et al. (2011) sumber diet dan faktor sosiodemografi dan ekonomi yang mempengaruhi vitamin D dan asupan kalsium pada balita Flemish. Eur J Clin Nutr 65: 1039-1047.
36. Hypponen E, Power C (2007) hypovitaminosis D pada orang dewasa Inggris pada usia 45 y: penelitian kohort nasional prediktor diet dan gaya hidup. Am J Clin Nutr 85:
860-868.
37. Hirani V, Primatesta P (2005) konsentrasi vitamin D di antara orang berusia 65 tahun ke atas yang hidup di rumah tangga dan lembaga swasta di Inggris: survei penduduk. Umur Penuaan 34: 485-491. 38. Hintzpeter B, Nishikawa GB, Thierfelder W, Muller MJ, Scheidt-Nave C Status D (2008) Vitamin
dan kesehatan berkorelasi antara orang dewasa Jerman. Eur J Clin Nutr 62: 1079-1089.
39. Hintzpeter B, Scheidt-Nave C, Muller MJ, Schenk L, Nishikawa GB (2008) prevalensi tinggi kekurangan vitamin D dikaitkan dengan latar belakang imigran di kalangan anak-anak dan remaja di Jerman. J Nutr 138:
1482-1490.
40. van der Sluis IM, Hop WC, van Leeuwen JP, Pols HA, De Muinck Keizer- Schrama SM (2002) Sebuah studi cross-sectional pada parameter biokimia pergantian tulang dan vitamin d metabolit pada anak-anak Belanda yang sehat dan dewasa muda. Horm Res 57: 170-179.
41. Bukit TR, Flynn A, Kiely M, Cashman KD (2006) Prevalensi status vitamin D suboptimal di muda, dewasa dan mata pelajaran Irlandia tua. Ir Med J 99: 48-49.
42. Bukit TR, Cotter AA, Mitchell S, Boreham CA, Dubitzky W, et al. Status D (2008) Vitamin dan penentu dalam remaja dari Irlandia Utara Muda Hati 2000 kohort. Br J Nutr 99: 1061-1067.
43. Andersen R, MolGaard C, Skovgaard LT, Brot C, Cashman KD, dkk. (2005) Gadis remaja dan wanita lanjut usia yang tinggal di Eropa Utara berstatus musim dingin rendah vitamin D. Eur J Clin Nutr 59: 533-541.
44. McKenna MJ (1992) Perbedaan status vitamin D antara negara pada dewasa muda dan orang tua. Am J Med 93: 69-77.
45. Perlu AG, Morris HA, Horowitz M, Nordin C (1993) Pengaruh ketebalan kulit, usia, lemak tubuh, dan sinar matahari pada serum 25-hydroxyvitamin D. Am J Clin Nutr 58:
882-885.
46. Jacques PF, Felson DT, Tucker KL, Mahnken B, Wilson PW, dkk. (1997) Plasma 25-hydroxyvitamin D dan penentu dalam sampel populasi lansia. Am J Clin Nutr 66: 929-936.
47. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Penurunan bioavailabilitas vitamin D dalam obesitas. Am J Clin Nutr 72: 690-693.
48. Dijkstra SH, van Beek A, Janssen JW, de Vleeschouwer LH, Huysman WA, dkk. (2007) prevalensi tinggi kekurangan vitamin D pada bayi baru lahir dari ibu berisiko tinggi. Arch Dis Child 92: 750-753.
49. van der Meer IM, Middelkoop BJ, Boeke AJ, Bibir P (2011) Prevalensi defisiensi vitamin D antara Turki, Maroko, populasi Afrika India dan sub-Sahara di Eropa dan negara-negara asal mereka: ikhtisar. Osteoporos Int
22: 1009-1021.
50. Brot C, Jorgensen NR, Sorensen OH (1999) Pengaruh merokok pada status vitamin D dan metabolisme kalsium. Eur J Clin Nutr 53: 920-926.
Hubungan
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868
Survey 2009. Nutr Res Pract 6: 86-90.
52. Clemens TL, Adams JS, Nolan JM, Holick MF (1982) Pengukuran beredar vitamin D pada manusia. Clin Chim Acta 121: 301-308.
53. Holick MF, MacLaughlin JA, Doppelt SH (1981) Peraturan previtamin kulit D3 fotosintesis pada pria: pigmen kulit bukan merupakan regulator penting.
Ilmu 211: 590-593.
54. Holick MF (1981) The fotosintesis kulit dari previtamin D3: sistem photoendocrine unik. J Invest Dermatol 77: 51-58.
55. Goswami R, N Gupta, Goswami D, Marwaha RK, Tandon N, et al. (2000) Prevalensi dan pentingnya konsentrasi D 25-hydroxyvitamin rendah pada subyek sehat di Delhi. Am J Clin Nutr 72: 472-475.
56. Webb AR, Engelsen O (2006) Menghitung tingkat paparan ultraviolet untuk status vitamin D yang sehat. Photochem Photobiol 82: 1697-1703.
57. Farrerons J, Barnadas M, Rodriguez J, Renau A, B Yoldi, dkk. (1998) Secara klinis ditentukan tabir surya (sun perlindungan faktor 15) tidak menurun vitamin serum
D concentration sufficiently either to induce changes in parathyroid function or in metabolic
markers. Br J Dermatol 139: 422–427.
58. Hoge Gezondheidsraad (2009) Voedingsaanbevelingen voor Belgie¨. Herziening 2009. Brussel: Hoge Gezondheidsraad.
59. Hollis BW (2007) Vitamin D requirement during pregnancy and lactation.
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868
High Prevalence of Vitamin D Deficiency in Pregnant
Women: A National Cross-Sectional Survey
Stefanie Vandevijvere1*, Sihame Amsalkhir2, Herman Van Oyen1, Rodrigo Moreno-Reyes2
1 Department of Public Health and Surveillance, Scientific Institute of Public Health, Brussels, Belgium, 2 Department of Nuclear Medicine, Hoˆpital Erasme, Universite´ Libre de Bruxelles, Brussels, Belgium
Abstract
An increasing number of studies suggest that vitamin D deficiency during pregnancy is associated with multiple adverse health outcomes in mothers, neonates and children. There are no representative country data available on vitamin D status of pregnant women in Europe. The aim of this study was to estimate the prevalence of vitamin D deficiency among Belgian pregnant women and to assess the determinants of vitamin D status in the first and third trimester of pregnancy. The women were selected via a multi-stage proportionate-to-size sampling design. Blood samples were collected and a questionnaire was completed face-to-face. 55 obstetric clinics were randomly selected and 1311 pregnant women participated in the study. The median serum 25-hydroxyvitamin D [25-(OH)D] concentration was significantly lower in the
first trimester (20.4 ng/ml) than in third trimester (22.7 ng/ml). Of all women, 74.1% (95%CI = 71.8–76.5%) were vitamin D
insufficient (25-(OH)D ,30 ng/ml), 44.6% (95%CI = 41.9–47.3%) were vitamin D deficient (25-(OH)D ,20 ng/ml), while
12.1% (95%CI = 10.3–13.8%) were severely vitamin D deficient (25-(OH)D ,10 ng/ml). Of all women included, 62.0%
reported taking vitamin D-containing multivitamins, of which only 24.2% started taking those before pregnancy. The risk of vitamin D deficiency (25-(OH)D ,20 ng/ml) was significantly higher for less educated women and women who reported not going on holidays to sunny climates. The risk of severe vitamin D deficiency (25-(OH)D ,10 ng/ml) decreased for women who reported alcohol consumption during pregnancy, decreased with more frequent use of sunscreen lotion and increased for smokers and women who reported preference for shadow. In conclusion, vitamin D deficiency is highly prevalent among pregnant women in Belgium and this raises concerns about the health consequences for the mother and the offspring. A targeted screening strategy to detect and treat women at high risk of severe vitamin D deficiency is needed in Belgium and in Europe.
Citation: Vandevijvere S, Amsalkhir S, Van Oyen H, Moreno-Reyes R (2012) High Prevalence of Vitamin D Deficiency in Pregnant Women: A National Cross-Sectional Survey. PLoS ONE 7(8): e43868. doi:10.1371/journal.pone.0043868
Editor: Claudia Kappen, Pennington Biomedical Research Center/LSU, United States of America Received April 23, 2012; Accepted July 26, 2012; Published August 24, 2012
Copyright: 2012 Vandevijvere et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The survey was funded by the Federal Public Service of Health, Food Chain Safety and Environment. Rodrigo Moreno-Reyes received support of the Belgian Fonds de la Recherche Scientifique Me´dicale (Convention no. 3.4578.09). The funder had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing Interests: The authors have declared that no competing interests exist. * E-mail: stefanie.vandevijvere@wiv-isp.be
Introduction
Vitamin D status is a well-known determinant of bone health [1,2]. Vitamin D deficiency increases the risk of osteoporosis [3] and fractures [4], while in its most severe form it causes rickets in children [5] and osteomalacia in adults [6]. The ubiquitous presence of vitamin D receptors in most tissues, including the placenta, suggests that vitamin D may have other roles as well. Adequate vitamin D intake is associated with a lower risk of cancer [7,8,9,10,11], cardiovascular diseases [12], autoimmune diseases [13], neurological disorders [14] and diabetes [15]. In addition, an increasing number of studies suggest that vitamin D deficiency during pregnancy is associated with multiple adverse health outcomes in mothers (gestational diabetes and pre-eclampsia), in neonates (wheezing) and children (low bone mineral density,
type-1 diabetes, eczema) [type-16–22]. However there is so far no conclusive
evidence about the causality of these relationships, as no randomised controlled trials of vitamin D supplementation with an appropriate assessment of a variety of health outcomes have been carried out to date [21].
Humans get vitamin D (cholecalciferol) from exposure to sunlight, diet and dietary supplements. As few food items contain or are fortified with vitamin D (such as liver, fatty fish, eggs, milk and dairy products, soy milk, butter, margarines), the skin synthesis of vitamin D induced by ultraviolet B radiation (UVB) is the main determinant of vitamin D status in the population [23]. Vitamin D once synthesized in the skin is metabolized into 25-dihydroxyvitamin D [25-(OH)D] in the liver. Due to its longer half-life, 25-(OH)D is considered the best bio-marker of vitamin D status. 25-(OH)D is then metabolized in the kidney by the 1-a hydroxyl1-ase to the 1-active steroid hormone 1,25-dihydroxyvit1-a-
1,25-dihydroxyvita-min D [1,25-(OH)2D]. Several modifications of vitamin D
metabolism occur during pregnancy.
The expression of 1-a hydroxylase is increased in the kidney
and placenta and the concentration of serum 1,25-(OH)2D
increases in normal pregnancy from the first to the third trimester.
The role of 1,25-(OH)2D during pregnancy to increase intestinal
calcium absorption is since long acknowledged [24].
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
below 20 ng/ml as inadequately low [25], and some evidence suggests that values higher than 30 ng/ml may be associated with better health outcomes in the adult population. [26,27]. The uncertainty concerning the optimal serum 25-(OH)D concentra-tion in pregnant women is even higher. As long as the proposed values are not validated in clinical trials the controversy will remain [28].
There is a growing concern about the health consequences of the high prevalence of vitamin D deficiency worldwide among the general population, including pregnant women. The adequacy of the current vitamin D dietary recommendations to reach an optimal vitamin D status during pregnancy has been questioned [24]. Although previous small surveys suggest that vitamin D deficiency among pregnant women is common in Europe [29,30], there are no reliable country-wide estimates of vitamin D status of pregnant women in European countries. Therefore the aim of this study was to carry out the first national representative random sample survey on vitamin D status in pregnant women in a European country and to assess the determinants of vitamin D status in the first and third trimester of pregnancy.
Methods Ethics Statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the medical ethical committee of the Erasme hospital in Brussels. The subjects provided written consent for participation in the study.
Sampling
The target population of the survey comprised all pregnant women in Belgium during the first and the third trimester of pregnancy in the period from September 2010 to June 2011. The women were selected according to a multi-stage proportionate-to-size stratified sampling design as recommended for studies assessing iodine deficiency [31]. The country was divided into two regions. In each region the obstetric clinics were ordered by province and size based on the number of deliveries during the past year and 60 clusters of 4 clinics were selected per region using systematic sampling in order to have enough replacement clinics in case some refused to participate. Out of these 60 clusters, 30 clusters were randomly selected and within each cluster the first clinic was invited to participate. In each clinic all gynaecologist-obstetricians were invited to participate in order to level out a possible gynaecologist effect. The aim was to include 22 women in each cluster of which 11 in the first trimester and 11 in the third trimester of pregnancy.
Data Collection
Blood samples were collected from the antecubital vein and a general questionnaire about demographic and socio-economic characteristics, smoking and alcohol consumption during pregnancy and during the 4 weeks prior to the interview,
diseases and medication and use of food supplements was
completed in a face-to-face interview conducted by the study nurse. Women from Algeria, Egypt, Libya, Morocco, Sudan, Tunisia, and Western Sahara were considered of North African descent. For all women included in the study, body mass index (BMI) was obtained from weight and height recorded by the
gynaecologist during the first prenatal consultation in the
beginning of the first trimester of pregnancy. First trimester BMI was used as a proxy for prepregnancy BMI for both first and third trimester pregnant women.
Analysis of Samples
Approximately 5 ml whole blood was collected by venipuncture
in a non-heparinized tube. Serum aliquots were then stored at–
80C for further analysis. Serum 25-hydroxyvitamin D (25-(OH)D) concentrations were measured by radioimmunoassay (Diasorin, Stillwater, MN, USA).
Statistical Analyses
The statistical analyses were carried out using STATA 10.1 (StataCorp, Texas, USA). As serum 25-(OH)D is not normally distributed, non-parametric methods were used. The median was used as the measure of central tendency.
Differences between regions, trimesters and age groups were explored using two-sample Wilcoxon rank-sum test or Kruskal-Wallis equality-of-populations rank test.
The odds of having a serum 25-(OH)D concentration lower than 20 ng/ml (vitamin D deficiency) versus a non deficient vitamin D status were estimated through multiple logistic regressions while entering the following variables as predictors in the model: season, age, trimester of pregnancy, region, BMI, smoking behaviour, alcohol consumption, use of vitamin D-containing food supplements, fish consumption, milk and dairy product consumption, education level, ethnicity, parity, exposure to sunlight during weekdays, exposure to sunlight during weekend days, use of sunscreen lotion, use of solarium, shadow or sun preference and sometimes going on holidays to sunny climates (yes/no question). In addition the odds of having a serum 25-(OH)D concentration lower than 10 ng/ml (severe vitamin D deficiency) versus a non severe deficient vitamin D status were estimated through multiple logistic regressions while entering the same predictors in the model.
Results
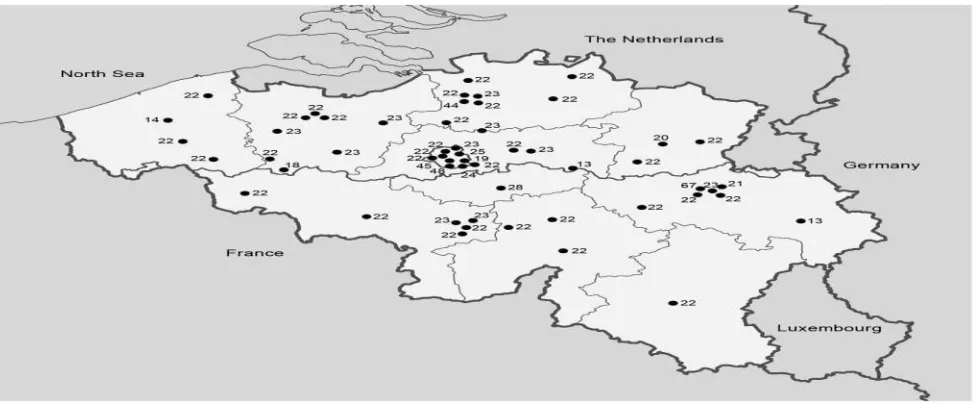
Among the 1311 pregnant women participating in the survey, there were 271 from Brussels, 597 from Flanders and 437 from Wallonia (Figure 1; Table 1). For 6 women information on the age was missing. The mean age of women was similar in all three regions. For 1307 women a general questionnaire was available. For 1 hospital (n = 23 women) certain questions (mainly nation-ality, ethnicity, education level) needed to be omitted from the questionnaire upon decision of the ethical committee of this particular hospital.
The characteristics of the pregnant women included in the study are shown in Table 2. More than 50% of the women included had a lower education level, which means only completion of secondary school or even lower education. More than 20% of the women in the sample were from non-Caucasian origin. Of all women included, 15% smoked during pregnancy and 12% reported having drunk alcohol during pregnancy (Table 2).
Of all pregnant women included, 640 were in the first, 666 were in the third and 2 were in the second trimester of pregnancy. For 3 women information on the trimester was missing. For 41.7% of the women this was their first pregnancy (unknown for 0.4% of the women), while for 45.6% of the women this would be their first child (status not known for 1.4% of the women). More or less 4% of the women within the sample had had a miscarriage before at least once. For 77.6% of the women their pregnancy was planned (unknown for 3.3% of the women).
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
Figure 1. Geographical distribution of the 55 hospitals visited in Belgium and the number of pregnant women (n = 1311) investigated by site (national survey on vitamin D status of pregnant women Belgium 2010–2011).
doi:10.1371/journal.pone.0043868.g001
Table 1. Number of pregnant women by region, trimester and age (national survey on vitamin D status among pregnant women
Belgium, 2010–2011).
Regions
Brussels** Flanders** Wallonia
Age(years ) 1sttrimester 3rdtrimester 1sttrimester 3rdtrimester 1sttrimester 3rdtrimester
15–20 7 2 11 10 21 17
21–25 34 27 77 51 56 73
26–30 41 39 108 149 76 58
31–35 34 53 69 75 49 45
36–40 14 14 23 19 13 24
41–45 2 3 1 3 3 2
Total 132 138 289 307 218 219
6 missing data for age.
**1 pregnant woman from 2ndtrimester.
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
Table 2. Characteristics of the pregnant women included in the study (n = 1311) (Belgian national survey on vitamin D
status in pregnant women, 2010–2011).
Characteristic N
% Secondary education or lower 54.54 715 % Higher education 27.23 357
% Of which during past 4 wks 15.41 202
% No 82.91 1087
% Not known 0.31 4
Drinking alcohol
% Yes 20.37 267
% Of which during past 4 wks 11.51 151
% No 78.49 1029
% Not known 1.14 15
*First trimester BMI used as a proxy for prepregnancy BMI. doi:10.1371/journal.pone.0043868.t002
significant. Of all women, 74.1% (95%CI = 71.8–76.5%) were
vitamin D insufficient (25-(OH)D concentration ,30 ng/ml) and
44.6% (95%CI = 41.9–47.3%) of the pregnant women were
vitamin D deficient (25-(OH)D concentration ,20 ng/ml), while
12.1% (95%CI = 10.3–13.8%) of the women were severely
vitamin D deficient (25-(OH)D concentration ,10 ng/ml). The percentage of women with vitamin D insufficiency and deficiency was higher in the first than in the third trimester of pregnancy but the prevalence of severe vitamin D deficiency was higher in the third trimester (Table 3).
For both first and third trimester women there was a clear seasonal trend in the mean serum 25-(OH)D concentrations with lowest concentrations in winter and highest during spring and summer, while decreasing again in autumn. Women of other ethnic origins were vitamin D deficient (25-(OH)D concentration ,20 ng/ml) all year round, except during summer for third trimester women (Figure 2).
Of all women included, 76.2% reported taking at least 1 multivitamin during pregnancy. For 62.0% of them the multivi-tamin contained vimultivi-tamin D. In the first and third trimester of pregnancy the percentage of women taking a multivitamin containing vitamin D was 52.6% and 72.3% respectively. Only 24.2% of all pregnant women started taking multivitamins before pregnancy, while 46.6% of these women started taking multi-vitamins within the first trimester of pregnancy.
The risk of vitamin D deficiency (25-(OH)D ,20 ng/ml) increased significantly with BMI and was significantly higher for women who reported not taking vitamin D-containing multi-vitamins (Table 4). In addition the risk of vitamin D deficiency was threefold higher among women of Asiatic descent, six fold higher for North African women and five fold higher for women of Hispanic descent compared to Caucasians. The risk of vitamin D insufficiency was significantly lower for more educated women and for persons reporting going on holidays to sunny climates. In addition the risk of vitamin D deficiency was significantly lower in summer, spring and autumn compared to winter (Table 4).
The risk of severe vitamin D deficiency (25-(OH)D ,10 ng/ml) was significantly lower among third than first trimester pregnant women (Table 5). In addition risk of severe vitamin D deficiency increased for women who reported not taking vitamin D containing multivitamins, who were of non Caucasian origin and who reported smoking during pregnancy. On the other hand risk of severe vitamin D deficiency decreased for women who reported alcohol consumption during pregnancy. Interestingly, risk of severe vitamin D deficiency decreased with more frequent use of sunscreen lotion and increased for women who reported preference for shadow (Table 5). Exposure to the sun during week and weekend days, and consumption of milk and dairy products were not associated with either severe or normal vitamin D deficiency.
Discussion
Despite the fact that more than 60% of the pregnant women reported taking multivitamins containing vitamin D during pregnancy, nearly 45% of the women were vitamin D deficient (25-(OH)D ,20 ng/ml). The prevalence of severe vitamin D deficiency was 12% during the first trimester and was slightly higher, 13%, during the third trimester of pregnancy. A previous small study in Brussels suggested that the prevalence of vitamin D
deficiency was high among the adult population and that
immigrants were at greater risk of vitamin D deficiency [32]. Other small-scale studies in Belgium showed a high prevalence of vitamin D deficiency among Belgian postmenopausal osteoporotic women [33] and elderly [34]. However, the present study is the first national survey on vitamin D status among pregnant women in Belgium. The high prevalence of vitamin D deficiency in Belgium stems from the fact that the contribution of dietary sources to the vitamin D status is negligible as was shown by the Flemish food consumption survey among preschoolers which estimated the mean vitamin D intake at only 2 mg/day [35].
The prevalence of vitamin deficiency (25-(OH)D ,20 ng/ml) is
high in many European countries [36–43] and some studies
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
Table 3. Serum 25-(OH)D concentration in pregnant women (n = 1311) (Belgian national survey on vitamin D status in pregnant
women, 2010–2011).
All women Wallonia Flanders 1sttrimester 3rdtrimester
N 1300 453 633 633 665
Age 28.565.1 27.965.5 28.864.7 28.365.1 28.865.1
Gestational weeks 22.2612.5 22.1612.8 22.4612.3 9.962.8 34.163.6 25-(OH)D(ng/ml)
Median 21.2 20.9 22.3 20.4 22.7*
IQR 13.8–30.0 13.5–29.1 14.6–30.6 13.6–26.7 14.3–34.1
95% CI 20.5–22.2 19.8–22.3 21.2–23.2 19.3–21.1 21.6–24.4
% ,10 ng/ml 12.1 12.3 10.9 11.6 12.6
% ,20 ng/ml 44.6 45.7 42.3 47.0 42.3
% ,30 ng/ml 74.1 76.3 72.5 82.2 66.7
*Different from first trimester pregnant women, p,0.001. doi:10.1371/journal.pone.0043868.t003
to an excessive storage of vitamin D in fat tissue decreasing thereby serum concentrations [47]. Ethnicity was also a major determinant of vitamin D status in the present study, as previously reported in the adult population [32] and in pregnant women [29,48,49]. In Belgium, pregnant women of different ethnic origins had sub-stantially lower vitamin D concentrations than Caucasian women and were vitamin D deficient all year long except during summer for third trimester women. In addition education level was associated with vitamin D status in our pregnant women population. Smoking increased the risk of both vitamin D deficiency and severe vitamin D deficiency; the mechanism for this appears to be unclear [50]. Interestingly the risk for severe vitamin D deficiency was lower among women who reported alcohol consumption during pregnancy. The latter has been found also among Korean men [51].
Variables influencing the formation of previtamin D3 in the skin
include skin pigmentation and intensity of the solar UV light [52–
55]. In summer, light-skinned people who spend at least
15 minutes outside during the day with their hands and face exposed will have adequate vitamin D levels. Sunscreen lotions prevent UV radiation from reaching the skin and might therefore
reduce the skin’s vitamin D production [56]. However, another
study found this effect to be only minor [57].
In Belgium, pregnant women who reported going on holidays to sunny climates had a lower risk of vitamin D deficiency and women who reported using sunscreen lotion had a lower risk of severe vitamin D deficiency. The latter is possibly due to the fact that women using sunscreen lotion are more often exposed to the sun. Women who reported a preference for shadow had a higher risk of severe vitamin D deficiency in our study.
The adequate intake of vitamin D during pregnancy and lactation is unknown, although it appears to be greater than the current dietary recommendations of 400 IU/d or 10 mg/d [58].
Some studies suggest that the dietary requirement during
pregnancy and lactation may be as high as 6000 IU/d [59] and
recognize that at least 1500–2000 IU/d of vitamin D may be
Figure 2. Serum 25-(OH)D concentrations over the different seasons, by trimester of pregnancy and ethnicity (national survey on vitamin D status among pregnant women in Belgium, 2010–2011).
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
Table 4. Risk of vitamin D deficiency during pregnancy in Belgium (25-(OH)D ,20 ng/ml) (n = 1100), results of multiple logistic regressions.
N of subjects N of deficient cases OR [95% Conf Interval] p
Season
Winter 470 278 1.000
Spring 384 127 0.234 0.165 0.332 ,0.001
Summer 93 12 0.100 0.049 0.203 ,0.001
Autumn 351 166 0.550 0.391 0.775 0.001
BMI* 1.051 1.022 1.080 ,0.001
Smoking
yes 219 118 1.000
no 1078 465 0.701 0.480 1.025 0.067
Use of multivitamins containing vitamin D
no 489 317 1.000
yes 809 266 0.224 0.168 0.300 ,0.001
Ethnicity
Caucasian, white 955 369 1.000
Asiatic 33 19 2.823 1.235 6.454 0.014
African (black) 64 34 1.309 0.694 2.468 0.406
North African 174 130 6.048 3.813 9.595 ,0.001
Hispanic 12 7 5.305 1.549 18.167 0.008
Education level
Secondary education or less 719 413 1.000
High school 353 108 0.488 0.349 0.681 ,0.001
University 195 52 0.509 0.331 0.783 0.002
Frequency of fish consumption (non-fatty fish)
Never 226 117 1.000
Less than once a month 225 90 0.564 0.354 0.897 0.016
1–3 days a month 505 216 0.839 0.564 1.248 0.386
1 day per week 270 124 0.794 0.506 1.248 0.318
2–4 days a week or more frequent 69 35 0.562 0.289 1.095 0.090
Sometimes going on holidays to sunny climates
Yes 882 366 1.000
No 408 215 1.703 1.248 2.324 0.001
*First trimester BMI used as a proxy for prepregnancy BMI. OR Odds ratio.
BMI Body mass index.
doi:10.1371/journal.pone.0043868.t004
needed in order to maintain a blood level of 25(OH)D above 30 ng/ml [24]. As those authors recognize that the evidence to propose such intakes is scarce and as long as the health benefits of having serum 25(OH)D levels higher than 30 ng/ml are not clearly established particularly in pregnant women, the Belgian Superior Health council still recommends a vitamin D supplement of 20 mg/day or 800 IU during pregnancy [58]. However, the vitamin D content of multivitamins for pregnant women in Belgium is only 400 IU indicating even this recommendation is not followed as pregnant women only take one multivitamin pill a day. In the absence of survey data from other European countries, we suspect that the prevalence of vitamin D deficiency in Belgium likely reflects the situation in other Western European countries. This assumption is based on the fact that the main risk factors associated with vitamin D deficiency (sun exposure and/or ethnicity) are common to many European countries. In addition
to the uncertainty concerning the optimal vitamin D intakes preventing vitamin D deficiency, there exists also a lack of recommendations to treat vitamin D deficient pregnant women.
Even in the last published guidelines the treatment of vitamin D deficient women is not specifically discussed [24]. The uncovering of the magnitude of vitamin D deficiency in pregnant women in Belgium (and Western Europe) should be translated into new research in order to fill the huge knowledge gap concerning the adequate amount of vitamin D to prevent and treat vitamin D deficient pregnant women. In addition, an increasing number of studies suggest that gestational vitamin D deficiency is associated with multiple adverse health outcomes in mothers and children
[16–22]. Therefore, there is an urgent need of randomised
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
Table 5. Risk of severe vitamin D deficiency during pregnancy in Belgium (25-(OH)D ,10 ng/ml) (n = 1121), results of multiple logistic regressions.
N of subjects N of severe deficient cases OR [95% Conf Interval] p
Trimester of pregnancy
first trimester 633 74 1.000
third trimester 665 84 1.751 1.128 2.719 0.013
Season
Winter 470 89 1.000
Spring 384 35 0.283 0.168 0.477 ,0.001
Summer 93 0
Autumn 351 34 0.324 0.191 0.551 ,0.001
Smoking
Yes 219 33 1.000
No 1078 125 0.463 0.268 0.801 0.006
Alcohol consumption
Yes 264 13 1.000
No 1022 143 2.370 1.162 4.834 0.018
Use of multivitamins containing vitamin D
No 489 115 1.000
Yes 809 43 0.121 0.075 0.193 ,0.001
Ethnicity
Caucasian, white 955 69 1.000
Asiatic 33 9 6.656 2.413 18.359 ,0.001
African, black 64 13 2.605 1.151 5.896 0.022
African, north 174 63 8.174 4.712 14.177 ,0.001
Frequency fatty fish consumption
Never 192 18 1.000
Less than once a month 188 24 2.205 1.010 4.816 0.047
1–3 days a month 498 59 1.481 0.755 2.904 0.254
1 day per week 291 35 1.391 0.671 2.885 0.375
2–4 days a week or more frequent 128 22 1.513 0.659 3.472 0.328
Use of sunscreen lotion
Yes, much of the time 644 36 1.000
Yes, sometimes 281 34 2.087 1.171 3.722 0.013
No 368 88 3.263 1.935 5.504 ,0.001
Preference sun/shadow
Sun 476 53 1.000
Shadow 497 70 1.983 1.225 3.210 0.005
Does not matter 321 35 1.206 0.691 2.104 0.510
OR Odds ratio.
doi:10.1371/journal.pone.0043868.t005
Given the high prevalence of vitamin D deficiency in pregnant women in Belgium and probably in many European countries, a vitamin D nutrition policy is needed at the country and European level. The current vitamin D recommendations for pregnant women are clearly insufficient to prevent and even more to treat vitamin D deficient pregnant women. Until the adequate treatment of vitamin D deficient pregnant women is established, a safe approach may be to correct vitamin D deficiency by targeting pregnant women at high risk of severe vitamin D deficiency. In addition the current vitamin D content of multi-vitamins for pregnancy, 400 IU, do not even comply with the current Belgian recommendations of 800 IU per day, therefore
a prudent step should at least be to increase the vitamin D content in multivitamins for pregnant women to 800 IU.
PLOS ONE | www.plosone.org 1 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women
Acknowledgments
The authors acknowledge the hospitals and gynaecologists who agreed to participate and all participating pregnant women. We also would like to acknowledge B. Hauquier and D. Martin for vitamin D laboratory analyses.
Author Contributions
Conceived and designed the experiments: SV RM-R. Performed the experiments: SA. Analyzed the data: SV. Contributed reagents/materials/ analysis tools: SV RM-R SA. Wrote the paper: SV RM-R HV.
References
1. Valimaki VV, Alfthan H, Lehmuskallio E, Loyttyniemi E, Sahi T, et al. (2004) Vitamin D status as a determinant of peak bone mass in young Finnish men. J Clin Endocrinol Metab 89: 76–80.
2. Ooms ME, Roos JC, Bezemer PD, van der Vijgh WJ, Bouter LM, et al. (1995) Prevention of bone loss by vitamin D supplementation in elderly women: a randomized double-blind trial. J Clin Endocrinol Metab 80: 1052–1058.
3. Lips P, van Schoor NM (2011) The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab 25: 585–591.
4. Jackson C, Gaugris S, Sen SS, Hosking D (2007) The effect of cholecalciferol (vitamin D3) on the risk of fall and fracture: a meta-analysis. QJM 100: 185–192.
5. Pettifor JM, Prentice A (2011) The role of vitamin D in paediatric bone health. Best Pract Res Clin Endocrinol Metab 25: 573–584.
6. Bhan A, Rao AD, Rao DS (2010) Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am 39: 321–31.
7. Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, et al. (2007) Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. Am J Prev Med 32: 210–216.
8. Garland CF, Gorham ED, Mohr SB, Grant WB, Giovannucci EL, et al. (2007) Vitamin D and prevention of breast cancer: pooled analysis. J Steroid Biochem Mol Biol 103: 708–711.
9. Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP (2007) Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr 85: 1586–1591.
10. Grant WB, Garland CF (2002) Evidence supporting the role of vitamin D in reducing the risk of cancer. J Intern Med 252: 178–179.
11. Grant WB, Garland CE (2003) Vitamin D as a risk reduction factor for colorectal cancer. Am Fam Physician 67: 465.
12. Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, et al. (2008) Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med 168: 1340–1349.
13. Zittermann A (2003) Vitamin D in preventive medicine: are we ignoring the evidence? Br J Nutr 89: 552–572.
14. Holick MF (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80: 1678S–1688S.
15. Martini LA, Wood RJ (2006) Vitamin D status and the metabolic syndrome. Nutr Rev 64: 479–486.
16. Dror DK (2011) Vitamin D status during pregnancy: maternal, fetal, and postnatal outcomes. Curr Opin Obstet Gynecol 23: 422–426.
17. Dror DK, Allen LH (2010) Vitamin D inadequacy in pregnancy: biology, outcomes, and interventions. Nutr Rev 68: 465–477.
18. Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, et al. (2007) High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates. J Nutr 137: 447–452. 19. Bodnar LM, Krohn MA, Simhan HN (2009) Maternal vitamin D deficiency is
associated with bacterial vaginosis in the first trimester of pregnancy. J Nutr 139: 1157–1161.
20. Lucas RM, Ponsonby AL, Pasco JA, Morley R (2008) Future health implications of prenatal and early-life vitamin D status. Nutr Rev 66: 710–720.
21. Barrett H, Mcelduff A (2010) Vitamin D and pregnancy: An old problem revisited. Best Pract Res Clin Endocrinol Metab 24: 527–539.
22. Hensel KJ, Randis TM, Gelber SE, Ratner AJ (2011) Pregnancy-specific association of vitamin D deficiency and bacterial vaginosis. Am J Obstet Gynecol 204: 41–49.
23. Holick MF (2007) Vitamin D deficiency. New Engl J Med 357: 266–281. 24. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, et al.
(2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96: 1911–1930.
25. Grant WB, Holick MF (2005) Benefits and requirements of vitamin D for optimal health: a review. Altern Med Rev 10: 94–111.
26. Grant WB, Boucher BJ (2011) Requirements for Vitamin D across the life span. Biol Res Nurs 13: 120–133.
27. Holick MF (2010) Vitamin D: extraskeletal health. Endocrinol Metab Clin North Am 39: 381–400.
28. Grant WB, Holick MF (2005) Benefits and requirements of vitamin D for optimal health: a review. Altern Med Rev 10: 94–111.
29. van der Meer IM, Karamali NS, Boeke AJ, Lips P, Middelkoop BJ, et al. (2006) High prevalence of vitamin D deficiency in pregnant non-Western women in The Hague, Netherlands. Am J Clin Nutr 84: 350–353.
30. Milman N, Hvas AM, Bergholt T (2011) Vitamin D status during normal pregnancy and postpartum. A longitudinal study in 141 Danish women. J Perinat Med 40: 57–61.
31. Sullivan KM, May S, Maberley G (2000) Urinary Iodine assessment: A manual on Survey and Laboratory methods. UNICEF/PAMM.
32. Moreno-Reyes R, Carpentier YA, Boelaert M, El Moumni K, Dufourny G, et al. (2009) Vitamin D deficiency and hyperparathyroidism in relation to ethnicity: a cross-sectional survey in healthy adults. Eur J Nutr 48: 31–37.
33. Neuprez A, Bruyere O, Collette J, Reginster JY (2007) Vitamin D inadequacy in Belgian postmenopausal osteoporotic women. BMC Public Health 7: 64. 34. Bouillon RA, Auwerx JH, Lissens WD, Pelemans WK (1987) Vitamin D status
in the elderly: seasonal substrate deficiency causes 1,25-dihydroxycholecalciferol deficiency. Am J Clin Nutr 45: 755–763.
35. Huybrechts I, Lin Y, De KW, Sioen I, Mouratidou T, et al. (2011) Dietary sources and sociodemographic and economic factors affecting vitamin D and calcium intakes in Flemish preschoolers. Eur J Clin Nutr 65: 1039–1047.
36. Hypponen E, Power C (2007) Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr 85: 860–868.
37. Hirani V, Primatesta P (2005) Vitamin D concentrations among people aged 65 years and over living in private households and institutions in England: population survey. Age Ageing 34: 485–491.
38. Hintzpeter B, Mensink GB, Thierfelder W, Muller MJ, Scheidt-Nave C (2008) Vitamin D status and health correlates among German adults. Eur J Clin Nutr 62: 1079–1089.
39. Hintzpeter B, Scheidt-Nave C, Muller MJ, Schenk L, Mensink GB (2008) Higher prevalence of vitamin D deficiency is associated with immigrant background among children and adolescents in Germany. J Nutr 138: 1482–
1490.
40. van der Sluis IM, Hop WC, van Leeuwen JP, Pols HA, De Muinck Keizer-Schrama SM (2002) A cross-sectional study on biochemical parameters of bone turnover and vitamin d metabolites in healthy dutch children and young adults. Horm Res 57: 170–179.
41. Hill TR, Flynn A, Kiely M, Cashman KD (2006) Prevalence of suboptimal vitamin D status in young, adult and elderly Irish subjects. Ir Med J 99: 48–49. 42. Hill TR, Cotter AA, Mitchell S, Boreham CA, Dubitzky W, et al. (2008)
Vitamin D status and its determinants in adolescents from the Northern Ireland Young Hearts 2000 cohort. Br J Nutr 99: 1061–1067.
43. Andersen R, Molgaard C, Skovgaard LT, Brot C, Cashman KD, et al. (2005) Teenage girls and elderly women living in northern Europe have low winter vitamin D status. Eur J Clin Nutr 59: 533–541.
44. McKenna MJ (1992) Differences in vitamin D status between countries in young adults and the elderly. Am J Med 93: 69–77.
45. Need AG, Morris HA, Horowitz M, Nordin C (1993) Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxyvitamin D. Am J Clin Nutr 58: 882–885.
46. Jacques PF, Felson DT, Tucker KL, Mahnken B, Wilson PW, et al. (1997) Plasma 25-hydroxyvitamin D and its determinants in an elderly population sample. Am J Clin Nutr 66: 929–936.
47. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 72: 690–693.
48. Dijkstra SH, van Beek A, Janssen JW, de Vleeschouwer LH, Huysman WA, et al. (2007) High prevalence of vitamin D deficiency in newborn infants of high-risk mothers. Arch Dis Child 92: 750–753.
49. van der Meer IM, Middelkoop BJ, Boeke AJ, Lips P (2011) Prevalence of vitamin D deficiency among Turkish, Moroccan, Indian and sub-Sahara African populations in Europe and their countries of origin: an overview. Osteoporos Int 22: 1009–1021.
50. Brot C, Jorgensen NR, Sorensen OH (1999) The influence of smoking on vitamin D status and calcium metabolism. Eur J Clin Nutr 53: 920–926. 51. Lee K (2012) Sex-specific relationships between alcohol consumption and
vitamin D levels: The Korea National Health and Nutrition Examination Survey 2009. Nutr Res Pract 6: 86–90.
52. Clemens TL, Adams JS, Nolan JM, Holick MF (1982) Measurement of circulating vitamin D in man. Clin Chim Acta 121: 301–308.
53. Holick MF, MacLaughlin JA, Doppelt SH (1981) Regulation of cutaneous previtamin D3 photosynthesis in man: skin pigment is not an essential regulator. Science 211: 590–593.
54. Holick MF (1981) The cutaneous photosynthesis of previtamin D3: a unique photoendocrine system. J Invest Dermatol 77: 51–58.
55. Goswami R, Gupta N, Goswami D, Marwaha RK, Tandon N, et al. (2000) Prevalence and significance of low 25-hydroxyvitamin D concentrations in healthy subjects in Delhi. Am J Clin Nutr 72: 472–475.
56. Webb AR, Engelsen O (2006) Calculated ultraviolet exposure levels for a healthy vitamin D status. Photochem Photobiol 82: 1697–1703.
PLOS ONE | www.plosone.org 2 August 2012 | Volume 7 | Issue 8 | e43868 Vitamin D Deficiency among Pregnant Women D concentration sufficiently either to induce changes in parathyroid function or
in metabolic markers. Br J Dermatol 139: 422–427.
58. Hoge Gezondheidsraad (2009) Voedingsaanbevelingen voor Belgie¨. Herziening 2009. Brussel: Hoge Gezondheidsraad.