Mrs Funmi Awosusi Barts Health NHS Trust, Society of Pharmacy London/HIV Dr Alasdair Bamford Consultant in Pediatric Infectious Diseases, Great Ormond Street. Dr Laura Byrne Locum Consultant in HIV Medicine, St George's University Hospitals NHS Foundation Trust, London. Dr Emily Clarke Consultant in genitourinary medicine, Royal Liverpool and Broadgreen University Hospitals NHS Trust.
Dr Steven Welch Consultant in Pediatric Infectious Diseases, England Heart NHS Foundation Trust, Birmingham.
Scope and purpose
- Guideline development process
- Patient involvement
- Dissemination and implementation
- Summary of guideline update and date of next review
Psychosocial care: section 4 on Psychosocial care for women living with HIV during and after pregnancy has been expanded and its position moved within the guidelines to reflect its importance. Safety: New data are included for tenofovir DF, raltegravir, rilpivirine, dolutegravir, elvitegravir and cobicistat. Infant post-exposure prophylaxis (PEP): The length of infant PEP has been shortened where the risk of vertical transmission is VERY LOW.
Hepatitis: information has been added for tenofovir alafenamide for hepatitis B virus (HBV) infection and for direct-acting agents for hepatitis C virus (HCV) infection.
Recommendations and auditable outcomes
Recommendations
The psychosocial care of women living with HIV during and after pregnancy
Screening and monitoring of pregnant women living with HIV
Current issues on the use of ART in pregnancy and pregnancy outcomes
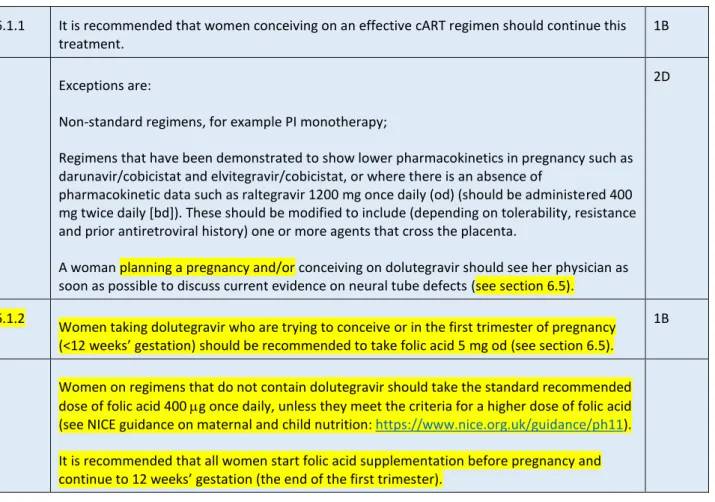
Current questions about the use of ART in pregnancy and pregnancy outcomes 6.1 Pregnancy with cART. As soon as they are able to do so in the second trimester, where the baseline viral load is. At the beginning of the second trimester or as soon as possible thereafter in women with a baseline viral load of HIV RNA copies/mL;.
Darunavir/r should be prescribed at a twice daily dose (600/100 mg twice daily) if resistance is known, and use of this higher dose should be considered when initiating darunavir.
HIV and hepatitis virus co-infections
7.1.10 cART active against both HBV and HIV should be continued postpartum in all women with HBV.
Obstetric management
For women with a viral load >1000 HIV RNA copies/ml plasma who present during labor or with SROM or who are admitted for PLCS. For untreated women in labor or with SROM whose current viral load is unknown; The use of an intravenous zidovudine infusion during labor may be considered in women on cART and with a plasma HIV viral load between 50 and 1000 HIV RNA copies/ml.
Neonatal management
Women who are advised not to breastfeed for the sake of their baby's health should have free formula to minimize vertical transmission of HIV. If the mother's antibody status is not documented, an HIV antibody test should be performed on the first sample received from the infant. Infants with a positive test for HIV should be started on cotrimoxazole prophylaxis from 4 weeks of age.
Infants with a positive HIV test should be urgently referred to a specialized center for the treatment of HIV according to the guidelines of the Children's HIV Association (CHIVA) and the Pediatric European Network for Treatment of AIDS (Penta).
Postpartum management of women
Auditable outcomes
6 Proportion of women with HBV/HIV co-infection in whom LFTs are performed 2 weeks after initiation of cART to detect evidence of antiretroviral hepatotoxicity or IRIS. 7 Proportion of women with HCV/HIV co-infection in whom LFTs are performed 2 weeks after initiation of cART to detect evidence of antiretroviral hepatotoxicity or IRIS. 8 Percentage of women who undergo invasive prenatal diagnosis before their HIV status is known.
13 Proportion of infants born to women living with HIV who have HIV antibody testing for seroreversion performed at age 22–24 months.
Introduction
- UK prevalence and epidemiology of HIV in pregnancy, antenatal screening and risk of transmission
- HIV infection in children
- Reporting and long-term follow-up
- National Study of HIV in Pregnancy and Childhood (NSHPC)
- References
Between 2012 and 2016, the number of women diagnosed with HIV each year in the UK fell from around 1,700 to 1,200, and this was particularly marked among women from sub-Saharan Africa. Over the past decade, around two-thirds of children newly diagnosed in the UK were born abroad. However, despite the high uptake of antenatal screening and effective interventions, perinatal infections still occur in the UK.
Low rates of mother-to-child transmission of HIV after effective pregnancy interventions in the United Kingdom and Ireland, 2000-2006.
The psychosocial care of women living with HIV during and after pregnancy
- Psychosocial issues around HIV and pregnancy
- Social issues
- Psychosocial care
- The antenatal HIV MDT
- The psychosocial care of women newly diagnosed with HIV during pregnancy
- Perinatal mental health assessment
- References
Experiences of stigma and discrimination in social and health settings among trans people living with HIV in the UK. Intimate partner violence in HIV-infected women attending an urban clinic in the United Kingdom: prevalence and associated factors. Pregnant women living with HIV (WLH) supported in clinics by WLH peers: a cluster randomized controlled trial.
Correlates of suicidal ideation during pregnancy and postpartum among women living with HIV in rural South Africa.
Screening and monitoring of pregnant women living with HIV
- Sexual health screening
- Herpes simplex virus
- Chorioamnionitis and BV
- STI screening
- Cervical cytology
- Contraception
- Laboratory monitoring of pregnant women living with HIV
- Failure to suppress
- References
A Thai study of women living with HIV who were seropositive for HSV-2 found that treatment with zidovudine did not reduce vertical transmission of HIV [23]. Regarding cervical cytology, pregnant women living with HIV should be managed according to the 2016 NHS Cervical Screening Program guidelines [41] and the BASHH/BHIVA/FSRH guidelines on sexual and reproductive health in people living with HIV [42 ]. Female-to-male transmission of human immunodeficiency virus type 1: risk factors for male seroconversion.
The Ariel project: a prospective cohort study of mother-child transmission of human immunodeficiency virus type 1 in the era of maternal antiretroviral therapy.
Current issues in the use of ART in pregnancy and pregnancy outcomes
- Conceiving on cART
- Woman is not already on cART: when to start
- Elite controllers
- All women not on cART should commence cART
- Woman is not already on cART: what to start
- Late-presenting woman not on treatment
- Evidence on teratogenicity, neonatal outcomes and ART
- Preterm delivery (PTD)
- Pharmacokinetics of antiretrovirals in pregnancy
- NRTIs
- NNRTIs
- Integrase inhibitors
- PIs
- Other agents
- Stopping ART postpartum
- HIV-2
- References
HIV and hepatitis virus co-infections
- Hepatitis B virus (HBV)
- Hepatitis C virus (HCV)
- References
Risk factors for vertical transmission of hepatitis C virus: a single center experience with 710 HCV-infected mothers. Effects of mode of delivery and infant nutrition on the risk of mother-to-child transmission of hepatitis C virus.
Obstetric management
- Antenatal management
- Mode of delivery
- Management of SROM
- Use of intrapartum intravenous infusion of zidovudine
- Multiple pregnancies
- Place of birth
- Water birth
- References
Whenever possible, amniocentesis should be delayed until the viral load is <50 HIV RNA copies/mL. It is therefore the opinion of the writing group that ECV can be offered to women with breech presentation who have a plasma viral load <50 HIV RNA copies/ml. These studies support the practice of recommending planned vaginal delivery for women on cART with plasma viral load <50 HIV RNA copies/ml.
Vertical transmission of HIV was low at 0.4% in women giving birth with a viral load <50 HIV RNA copies/ml, but data on mode of delivery for this subgroup were not provided [25]. 1C 8.3.2 If the mother's HIV viral load is <50 HIV RNA copies/ml, immediate induction or augmentation. For all women with viral load <50 HIV RNA copies/mL, obstetric management should aim for delivery within 24 hours of SROM.
In those with viral load <1000 HIV RNA copies/mL there were no cases of perinatal transmission (493 cases with SROM up to 25 hours). Therefore, for women on cART with SROM at term with a viral load <50 HIV RNA copies/mL and who do not have obstetrics. Therefore, women with SROM at term with a viral load <50 HIV RNA copies/mL should have prompt induction with a low threshold for treatment of intrapartum pyrexia.
It is the recommendation of the writing group that CS should be considered for women with a viral load of 50-399 HIV RNA copies/ml at term. The use of an intravenous zidovudine infusion during labor may be considered in women on cART and with a plasma HIV viral load of <1000 HIV RNA copies/ml.
Neonatal management
- Infant PEP
- VERY LOW RISK
- LOW RISK
- HIGH RISK
- Choice of triple combination PEP for neonates
- Intravenous ART in the neonate
- Timing of neonatal PEP
- Maternal genotypic resistance
- HIV-2
- PEP beyond 4 weeks
- Pneumocystis pneumonia (PCP) prophylaxis
- Immunisation
- Infant feeding
- Breastfeeding advice for women with HIV living in the UK
- Supporting women living with HIV to formula feed
- Suppression of lactation
- Choosing to breastfeed in the UK
- Communication with health professionals
- Diagnosis of infant HIV status
- Assays for the diagnosis of HIV infection status in infants .............................. Error! Bookmark not defined
- Neonatal management in maternal hepatitis co-infection
- HIV exposed but uninfected (HEU)
- References
Postpartum management of women
- Antiretroviral therapy
- Support services
- Postnatal follow-up of women
- Mental health assessment and support
- Contraception
- Cervical cytology
- Testing of partner and/or older children
- References
As discussed in Section 4, mental health problems are common in the context of HIV and pregnancy. If there are concerns about postnatal depression, women should be linked to Trust Community hub perinatal mental health services or referred to HIV liaison/community psychiatry for further assessment. Women should be informed that it is possible to become pregnant before the first postnatal period and therefore, if necessary, to use a condom until the postnatal examination [11].
There are several ART agents available that do not interact with systemic estrogens and/or progestogens, such as all NRTIs, raltegravir, dolutegravir, rilpivirine, and maraviroc. Postpartum follow-up may be an appropriate time to revisit testing of partners and/or older children. A woman newly diagnosed during pregnancy should be counseled and supported about testing her other children and partner if appropriate and there are no other concerns (such as risk of intimate partner violence, see section 4).
She should be informed that use of cART will not only significantly reduce her risk of vertical transmission of HIV [14] but will also reduce her risk of sexual transmission. If her viral load is undetectable for six months or more, she will not transmit HIV sexually; however, she should be advised to use condoms with her untested or HIV-negative partner until then [15]. The risk of viral rebound in the year after childbirth in women continuing to use antiretroviral therapy.
Beyond 'Option B+': understanding antiretroviral therapy (ART) adherence, retention in care and engagement in ART services among pregnant and postpartum women initiating therapy in sub-Saharan Africa. Sexual activity without condoms and risk of HIV transmission in serodiscordant couples when the HIV-positive partner uses suppressive antiretroviral therapy.
List of abbreviations
TD Tenofovir disoproxil salt TDF Tenofovir disoproxil fumarate TDM Therapeutic drug monitoring TTN Tachypnea of the newborn.
PICO questions
Induction of labor, instrumental delivery, episiotomy in HIV-positive pregnant women What fetal monitoring tests should be performed during labor? What should be the antiretroviral treatment for a woman who requires amniocentesis or chorionic villus sampling and who is not already receiving antiretroviral therapy? If mother is breastfeeding, how often should mother and baby be monitored and what tests should be used?
Consistent evidence from well-conducted randomized controlled trials or overwhelming evidence of another form. Evidence from randomized controlled trials with important limitations (contradictory results, method errors, indirect or imprecise), or very strong evidence from another research design. Benefits closely balanced with risks and burdens, some uncertain in estimates of benefits, risks and burdens.
Evidence from randomized controlled trials with important limitations (contradictory results, method errors, indirect or imprecise). Evidence from observational studies, unsystematic clinical experience, or from randomized controlled trials with serious defects. Uncertainty in the estimates of benefits, risks and liabilities; benefits can now be balanced with risks and liabilities.
2 mg/kg twice daily - round the dose to the nearest 0.5 mg to aid in administration. much less often than with ZDV). Intravenous: Usually as part of combination therapy 2 mg/kg IV twice daily (as a 30-minute infusion).