The research into the Vision on Psychiatric/Mental Healthcare provides an evidence-based basis from which we can set clear goals. The vision for psychiatric/mental health services set out in this report complements the standards for mental health services in Ireland (Quality Framework for Mental Health Services in Ireland, MHC: 2007).
Recruitment and designing the format for the focus groups
Members of the steering group
List of Abbreviations
Glossary of Key Terms
Mental Health Promotion 'Action to maximize mental health and well-being among populations and individuals. Recovery involves the development of new meaning and purpose in one's life as one grows beyond the catastrophic effects of mental illness' (Anthony.
A note on terminology
Introduction
- Background
- Project Aims
- Project Objectives
- Terms of Reference
To review and establish the current role of the nurse working with people with mental health difficulties. To identify the factors that can hinder the role development of nurses working in psychiatry.
Action Plan
- Introduction
- The Consultation Process
- The Publication Format
- Summary of Key Findings
- Adopting a recovery approach
- Improving outcomes and service quality 3. Developing clinical capacity
- Enhancing organisational eff ectiveness
A review of the literature and findings from the consultation process, together with the Psychiatric/Mental Health Vision Action Plan, which sets out the recommendations and implementation plan. The overview of the literature and the sections on the project methodology are available in chapters 3 and 4 of the report 'Vision on psychiatric/mental health care'.
Adopting a recovery approach
Improving outcomes and service quality
Developing clinical capacity
Enhancing organisational eff ectiveness
Format of recommendations
An introduction to each topic is provided and describes the values and experiences articulated and the literature. These are not intended as a reference list, the full reference list is included at the end of the report.
Recommendations
Adopting a recovery approach Introduction
Real and Meaningful partnership/involvement
The main principle of a recovery approach is that the person is at the center of the mental health system” (WS 7). The following recommendations and accompanying actions support the adoption of a recovery approach at all levels and aim to improve experiences and outcomes for service users.
Supportive publications
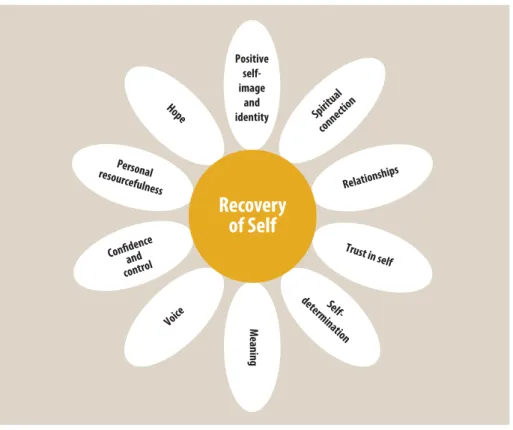
Recovery of Self
Adopting a recovery approach Recommendation 1
The principles and values of the recovery approach will inform psychiatric/ mental health nursing practice in all areas of care
Higgins (2008) presented a framework and audit tool for the development of a recovery approach within Irish mental health care. The audit tool, namely The Pillars of Recovery: Service Audit Tool (PoRSAT), has been developed to enable the provider, team and/or individual to monitor their progress in developing a recovery-oriented service.
National Practice Standards will be developed for all professionals working in Mental Health Services
6 Implementation of metrics to monitor organizational progress and professional performance in relation to recovery to be developed, utilized and evaluated nationally. RPNs report that they are guided and supported by the organizational systems, structures and processes to work in a recovery-oriented way.
An inclusive consultation process is required to review the title of ‘Registered Psychiatric Nurse’ to refl ect the role related to the
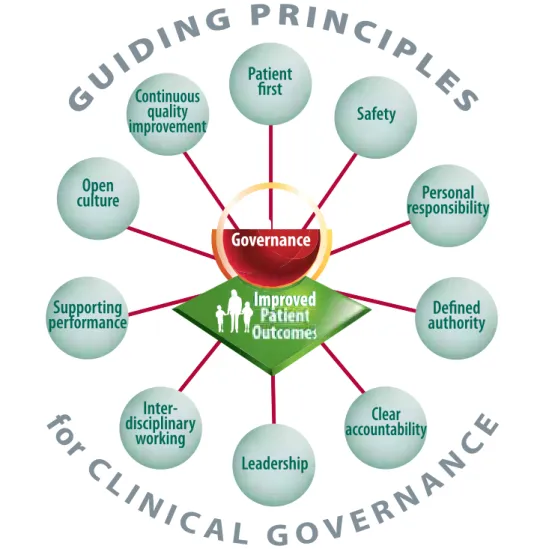
Improving outcomes and service quality Introduction
Personal responsibility
Defined authority
Clear accountability
Continuous quality
Patient first
Leadership
Nurses who recognize the absolute centrality of the perspective of service users (and carers) and recognize the ability of service users to be actively involved in all decisions. Nurses who practice from a core belief that healing is possible and consistently demonstrate this to service users and carers will improve outcomes for service users.
Key Performance
Modern mental health service providers must demonstrate service-level clinical effectiveness to key stakeholders (Sugarman et al. 2009). According to Sugarman et al. 2009) the use of KPIs based on routinely collected outcome data promotes a culture of transparency and openness to outcomes and allows providers to monitor performance while giving clinicians the freedom to develop therapeutic programs that can best provide true health improvement.
Indicators
Psychiatric nurses are the largest profession working in mental health services in Ireland, therefore they have a major role in the provision of mental health services and are in direct contact with service users and their carers/family members. The following recommendations and accompanying actions aim to improve experiences and outcomes for service users, as well as service quality at all levels of service delivery.
Enhanced clinical
They have good prerequisites for measuring results, and they must continue to strengthen their focus on measuring service users' results in practice. I was unhappy in the group home - in an independent home for 16 years and it's great - CPN is essential.
Supportive Publications
Key Performance indicators/ measures will be developed,
Clearly developed quality, safety and risk management systems and processes will be developed and utilised to enhance clinical
Clearly developed quality, safety and risk management systems and processes will be developed and used to improve clinical practice. Psychiatric nurses will continue to improve the integration of social inclusion values into their clinical practice as members.
Psychiatric nurses will continue to enhance the integration of social inclusion values into their clinical practice as members of
Public Health data will inform population focused nursing practice
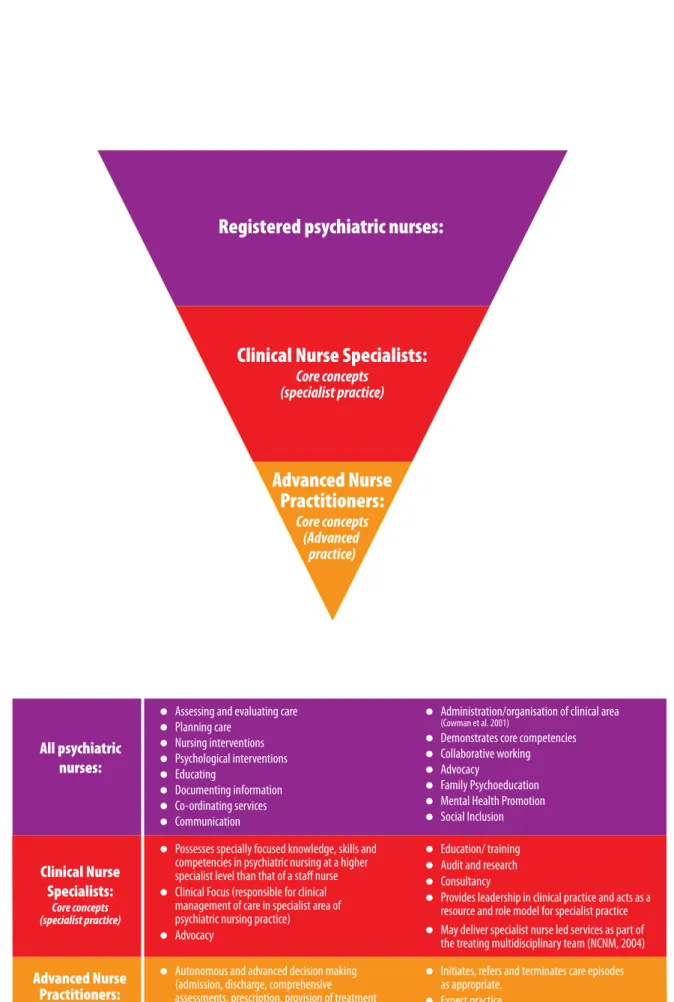
Developing Clinical Capacity Introduction
Nurse prescribing was a role that was identified during the consultation as being of particular benefit to service users in mental health services. Generally, no additional cost for CNS/CMS and ANP/AMP services (staff costs and activity levels for CNS/CMS and non-CNS/CMS services and ANP and non-ANP services have been aligned).
Supporting Publications
Service users expressed a demand for nurses to take an active role and expand and advance their practice in managing their care. Positive outcomes can be achieved through the development of specialist nursing roles and advanced practice in areas such as improved service delivery, increased satisfaction, a positive contribution to the provision of quality care and population health (OECD, 2004) together by providing advanced clinical skills and strengthening nursing leadership and research.
Professional Development for Psychiatric Nurses
Registered psychiatric nurses
Clinical Nurse Specialists
Advanced Nurse Practitioners
Developing clinical capacity Recommendation 8
Psychiatric nurses will continue to access, comprehend and utilise evidence based practice to inform their clinical practice
Psychiatric nurses will provide a more expanded scope of practice to increase clinical capacity and will continue to
4 Positive risk taking is promoted through guidelines, policies, processes and protocols and managed through local clinical governance structures. 5 Critical incidents and incident reports are routinely audited and a culture of learning is promoted as a result of these audits.
Psychiatric/ mental health nursing will improve care by developing new, expanded, specialist and advanced roles in
Psychiatric nurses at management and clinical grade levels must engage in professional and clinical leadership development.
Psychiatric nurses at management and clinical grades must engage in professional and clinical leadership development
The strengthening of all educational programmes is critical to preparing nurses with the appropriate knowledge, skills,
A national policy is required regarding the reintroduction of post-registration programs (conversion programs) that result in additional registration on ABA register giving priority to Psychiatric, Intellectual Disability and General Nursing to meet service needs. At the time of writing, a review of the undergraduate nursing and midwifery degree programs is underway by the Department of Health.
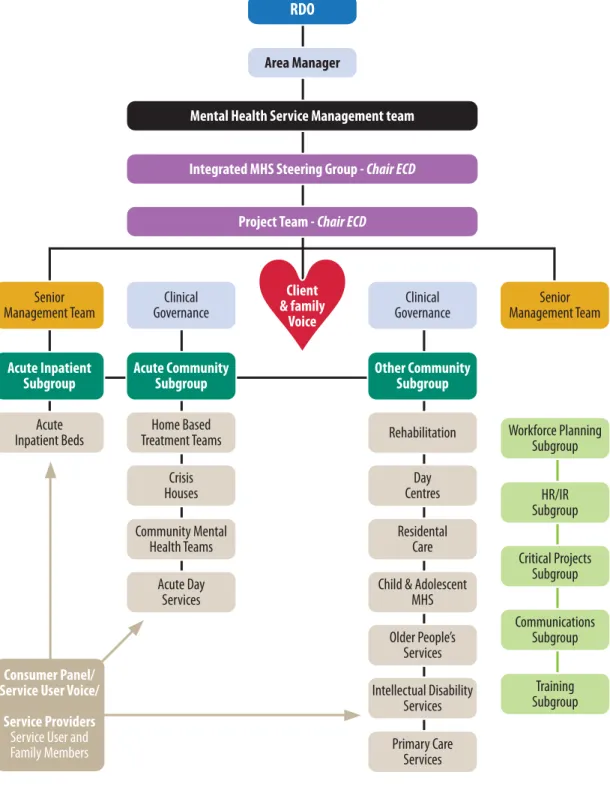
Enhancing organisational eff ectiveness Introduction
The following recommendations and associated actions aim to increase organizational effectiveness across all levels and aim to improve experiences and outcomes for users of services. 2010) Teamwork within Mental Health Services in Ireland. Department of Health and Children (2006) A vision for change: Report from the expert group on mental health policy.
Service users will have access to psychiatric nurses in primary care settings with specialist skills to engage in prevention,
Mental health nurses should be at the forefront of the delivery of mental health care in general practices, emergency departments, primary care and support services, taking an advisory role. Service users will have access to psychiatric mental health nursing skills in prevention, early detection and intervention.
Service users will have access to psychiatric mental health nursing skills in prevention, early detection and intervention
Service users will have equitable access to psychiatric/mental health nursing skills that are consistent and responsive to each
The current mental health service delivery structures and legislation need to be realigned to make the full possibility possible.
The current mental health service delivery structures and legislation need to be re-aligned to enable the full
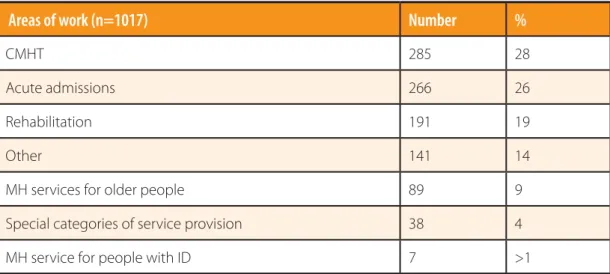
A national psychiatric/ mental health nursing workforce group will be established to determine the range of skills, knowledge
List of Recommendations
The principles and values of the recovery approach will inform psychiatric/mental health nursing practice in all areas of care and service delivery. Psychiatric nurses will continue to improve the integration of social inclusion values in their clinical practice as members of the treating clinical team.
Developing Clinical Capacity
Implementation and Review
The HSE, through the ONMSD, will establish national and regional implementation groups consistent with healthcare organizational structures. At the end of the five-year period, ONMSD will formally review progress on the recommendations and consider the need for further developments.
Literature review
Introduction
National Policy Context
Population mental health needs
Minority groups
Service users from other countries
Lesbian, Gay, Bisexual and Transgender (LGBT)
Children
Deliberate self-harm, which increased with age, accounted for 6.2% of primary presentations in the 15-17 age group; however, deliberate self-harm/suicidal ideation was recorded as a reason for referral in 22% of new cases seen. In 2009, the capacity of HSE children and adolescents hospital services increased from a total of 16 to 30.
Deliberate Self Harm (DSH) & Suicide
Although suicide prevention is a complex task, a review of the suicide prevention literature highlights a recurring finding that the key to suicide prevention is personal engagement with the service user and the psychological and social circumstances of their particular situation ( Hawton and van Heeringen, 2000). As acknowledged in the Reach Out document (HSE, 2005), improving access to quality mental health services is an essential part of any suicide prevention strategy.
Physical health care
Quality and Safety in Mental Health
It also aims to provide standards of continuous improvement in the quality and safety of mental health services. Staff skills, expertise and morale are key influencers in the delivery of a quality mental health service.
Psychiatric/ Mental Health Nursing and Professional Issues
Systematic evaluation and review of mental health services informed by best practice will enable providers to deliver quality service. The needs of service users and the evolving mental health services must inform the continued development of the psychiatric nurse as a practitioner.
Core Nursing Skills to Work in a Recovery Oriented Way
Change is a ubiquitous feature of modern health care policy and practice that occurs within a rapidly evolving knowledge and technological environment (Whittaker et al. 2000). Within such an environment the knowledge, skills and competencies required for competent mental health and psychiatric/mental health nursing practice are also changing.
Collaborative ethos
Communication
Refl exivity
Flexibility
Facilitating Support
Improved service user outcomes as a result of psychiatric nursing interventions
In a systematic literature review of the effectiveness of psychiatric nursing interventions, a set of ten core interventions were considered important to the psychiatric nurse's role in daily clinical practice (Gray et al. 2006). Similarly, in Ireland, a descriptive qualitative research study aimed to investigate the role and function of psychiatric nurses in clinical practice, identifying nine categories for the role of psychiatric nurses (Cowman et al. 2001).
Psychoeducation
Cognitive behavioural therapy (CBT)/ Counselling/psychotherapy (not CBT)
Management of violence, risk assessment and observation
Assessment
Medication management
Mental and physical health promotion
Developments in Specialist and Advanced nursing practice roles in Ireland and improved outcomes for service users/careers
The development of specialist and advanced practice roles in Ireland is part of the strategic development of the overall health service and takes place in the context of contemporary health and social policy, the requirements of population health and the service planning process. National policy documents such as the Report of the Commission on Nursing (Government of Ireland, 1998), the national health strategy Quality and Fairness: A Health System for You (DoHC 2001) and Begley et al. 2010) recommend the development of specialist and advanced nursing practice positions.
Conclusion
Project methodology
- Introduction
- Project design
- Anonymous survey
- Eligibility to participate and designing the survey
- Piloting the Survey
- Recruitment of the survey to maximise response rate
- Data collection for survey
- Focus groups and written submissions
- Recruitment and designing the format for the focus groups and written submissions
- Advertising for the focus groups and inviting written submissions
- Data analysis .1 Quantitative data
- Qualitative data
- Ethical considerations
- Limitations
- Summary
Before dissemination, the final draft of the survey was reviewed by the project team to ensure that it reflected the purpose. After each focus group, the data on the flip chart was compared with the project worker's notes.
Findings from the survey
Introduction
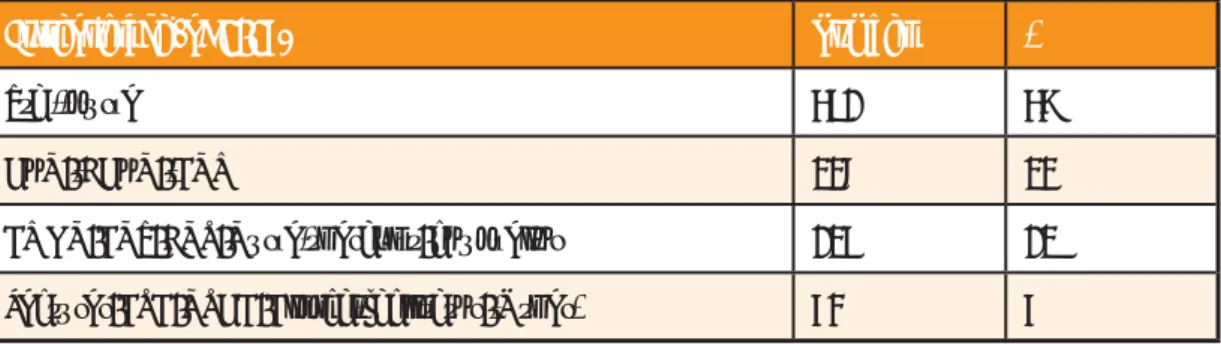
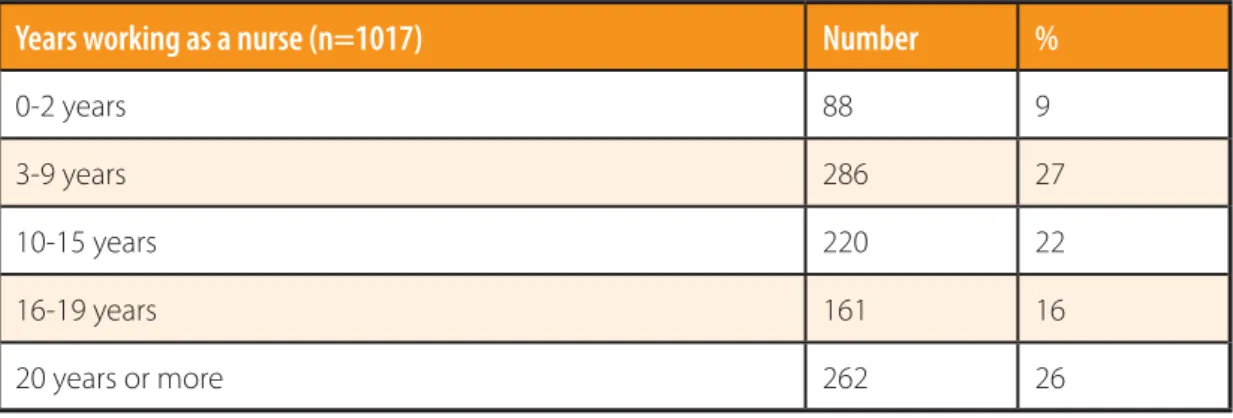
Response rate and profi le of survey participants
Current grade
Area of work
Professional registration
Highest educational qualifi cation
HSE area
Organising and planning care
Respondents were also asked to assess how often they engage with a variety of different organizations and individuals in their work with service users (see Table 6). It is clear from the examination of this section that there are many other people and organizations that psychiatric nurses interact with on a daily basis when working with service users.
Always / majority of time
Of the participants who indicated that the use of a nursing care plan was applicable to their role (n=935), more than nine in ten (92%; n=864) reported using a care plan. A further 18% (n=182) of participants indicated that they liaise with 'other' services or people, including legal services, social welfare services, general hospital staff, community welfare officers, probation officers, domestic staff, maternity services, Travelers support groups, Alzheimer's Association and other specific community and voluntary organisations.
Occasionally/
Similarly, about eight in ten (80%; n=753) of those who responded that using an interdisciplinary care plan fit their role (n=938) reported using this type of care plan. Percentages were calculated based on appropriate responses and do not include those who answered "not applicable".
Participants also reported how often they included different areas in service user assessments. Participants reported that they least often included the needs of their carers (51%; n=469) and their children (48%; n=424) in service user assessments.
With all / most service users
About one in ten participants (10%; n=104) indicated that they used "other" tools than those listed. However, as not all service users have children or relationships with their children or family members, caution must be exercised when interpreting this data.
With few / no service users
In addition, participants were asked how often they considered different aspects when planning care for service users. More than 80% of participants concerned medication management (90%), support systems (86%), coping mechanisms (85%), hopes and wishes for the future (84%), fears/anxieties (83%), material resources ( 83%). %) and caregiver/family strengths (81%) in planning care for all or most service users.
With all / with most service users
With few / with no service users
Service user and carer/ family involvement
Participants were asked to rate the level of service user and family involvement in six areas, namely care planning, decision making, goal setting, review of care received with the nurse, review of care received with the team and assessment of the care journey . They were least involved in reviewing care received with the multidisciplinary team and assessing the care pathway, with approximately three in ten participants indicating that service users had little or no involvement in this aspect of their care.
Extremely / very involved
Moderately involved
Little / no involvement
Recovery oriented approach
Has your service adopted a recovery approach?” (n=1017) Number %
Two lists were provided to participants regarding factors that may facilitate or inhibit the adoption of a recovery approach in their current area of practice. The most common factors facilitating the adoption of a recovery approach in their practice areas according to respondents were supportive family relationships (92%; n=847), community/peer support services (88%; n=773) and the environment in which care is provided, including specifically the local environment (84%; n=721) and the service user's home (84%; n=721) (see Table 13).
Facilitates adoption of recovery approach
Inhibits adoption of recovery approach
Systems and processes
Extremely / very important
Neutral Number (%)
Not at all / not important
Service user and carer/ family education
Participants were also asked to identify areas of family education in which they were involved. Examples of “other” areas of family education that respondents referred to include caregiver care programs, educating families about cognitive impairment and dementia, and facilitating evidence-based family skills programs.
Professional development
The most common areas identified were education about medication (56% n=573), education about early warning signs (43%; n=440) and education about available support for carers (35%; n=356).
Development of role
Facilitates development Number (%)
Inhibits development Number (%)
Qualitative aspect of survey
- Understanding of recovery
Individual empowerment
Recovery is a belief/ an attitude
Therapeutic relationship
Factors that facilitate adoption of a recovery approach
Supportive environment
Participants noted the importance of supportive management structures and organizational systems, including recovery-oriented policies, protocols and guidelines, and consistent staffing to facilitate the adoption of a recovery approach. Specifically, one participant noted how "clinical supervision would facilitate adoption of a recovery approach." Others referred to nurses as strong advocates for helping to facilitate a recovery approach.
Community
Service user involvement
Interdisciplinary education
Factors that inhibit adoption of a recovery approach
Another question asked participants to expand on, or provide information on, factors they believe hinder the adoption of a recovery approach in their practice area. Finally, participants described how the stigma associated with mental health difficulties can hinder the adoption of a recovery approach.
Resources
The first major theme dealt with the practical issue of lack of resources, particularly lack of staff and time. An over-reliance on the medical model has also inhibited a holistic approach to recovery, according to many.
Medical model
Thirdly, a lack of interdisciplinary communication was seen as an inhibiting factor, as was a lack of support from management staff.
Interdisciplinary co-operation and support
Stigma
Skills and competencies
The survey asked another open-ended question about whether respondents have developed special skills and/or competencies that they do not use in their current nursing field. Some responses to this question included psychotherapy and counseling skills, management and leadership skills, clinical skills, venipuncture and research skills.
Development of RPN role
Facilitating the development of the RPN Role: The need for a supportive organisational culture
Management and leadership structures
Support opportunities for development
Inhibiting the development of the RPN Role
Dominance of medical model
Management support, leadership structures and resources
Summary
Findings from the focus group and written submissions
Introduction
Respondents understanding of working in a recovery-oriented way
Most respondents indicated that working in a recovery-oriented way involves understanding that recovery is a journey that is individual to each person and involves looking beyond individuals' mental health difficulties. Some responses indicated that it is imperative that the carer empowers the individual with mental health difficulties to create a meaningful life plan for them and recognize the service user as the expert in the relationship.
Individual care planning and collaboration
Some respondents understood that exploring how a person defines recovery for them was essential to working in a recovery-oriented way, as was the availability of meaningful therapeutic activity. Individualized care will contribute to empowering service users to take control of their situation and view mental health professionals as resources rather than experts.
Community-based approach
Under this theme, respondents described a recovery-orientation approach as a process that respects service users as unique individuals, recognizing their individual expertise, as well as their unique beliefs and strengths. This return of strength to the service user will enhance their recovery as it promotes a sense of mastery and confidence in them.
Recovery as being ‘symptom free’
A holistic approach: Moving away from the domination of the medical to incorporating a range of therapeutic skills and interventions
Inspiring hope
Facilitating RPNs to work in a recovery-oriented way
The first addressed the need to increase opportunities for recovery education and training. The second major theme addressed the need for a culture and organizational structures that would support a recovery-oriented approach.
Increase opportunities for education and training
The next question explored respondents' views on how nurses can be supported to work in a recovery-oriented way. They described the need for student curricula to be reviewed, as well as the need for recovery-oriented training and reflection opportunities for those already working in services to be increased.
Review curricula and Continuing Professional Development activities
Opportunities to refl ect
Supportive organisational culture, systems and structures
Recovery-oriented leadership and management structures
Introduce supportive recovery-oriented initiatives
Supportive culture
Values and principles that should underpin psychiatric nursing
Respondents were asked to comment on what values and principles they believed should underpin psychiatric/mental health care. The answers to this question covered a wide range of values and principles, and most of the respondents did not distinguish between the concepts of values and principles in their answers.
A recovery-oriented approach
The underlying theme covered in most of the responses was the need for psychiatric nursing to be based on the values and principles of respect for individual human rights, equality, confidentiality, hope, empathy, advocacy, reducing stigma, safety, honesty, dignity for the service user, informed consent and the values and principles that underpin a recovery approach.
Respect and dignity for the service user
Providing service-user centred care
A focus on ongoing development
Skills and competencies that require development to improve the experiences and outcomes as identifi ed in A Vision for Change (DoHC, 2006)
A number of focus group respondents cautioned that in developing their skills and competencies, it is important not to lose sight of the caring aspect of psychiatric nursing practice. They emphasized the importance of maintaining and building on the current skills and competencies that nurses have demonstrated in developing services and improving service user outcomes.
Assessment skills
The next area in which respondents were asked to comment was what nursing skills and competencies need to be developed to improve experiences and outcomes for service users, for family members and for nurses, as identified in A Vision for Change (DoHC, 2006) . The second important competency that respondents felt needed to be developed was interpersonal and recovery-oriented communication skills.
Risk assessment skills
The first main category respondents emphasized was recovery-focused assessment skills, particularly risk assessment and skill development in relation to psychosocial interventions. These were described at all levels, from individual recovery-oriented communication to teamwork to leadership roles.
Psychosocial interventions
Some respondents indicated that training on specific interventions to respond to individuals who engage in DSH and suicide prevention training should be available to all RPNs. Specific Training in Brief and Focused Psychosocial/Psycho-Educational Interventions for People with Recurrent Suicide Attempts Aiming at Harm Reduction and Suicide Prevention.
Interpersonal and communication skills
Teamwork skills
What needs to be put in place to ensure that RPNs incorporate an evidence- based approach into practice?
Training, skills development and knowledge sharing
Supportive leadership and management
Critical refl ection
Practice-based research and outcome measurement
Development of the RPN role to improve services
Respondents were asked how the role of the RPN should be developed to improve the range and quality of services available to service users and carers. Finally, respondents saw effective support and leadership as critical in developing the RPN role to improve the range and quality of services available.
Identify service user needs and impact of interventions through research
Specific areas that respondents felt could be developed were the role of RPN in prevention and early intervention, provision of specialist services, psychosocial interventions and health promotion. Respondents also discussed the need for RPN role development in relation to social inclusion and working with carers and family members.
Prevention and early intervention
Some respondents actually indicated that contact with the mental health service could be avoided entirely if an RPN with specialist skills was accessible through the primary care setting. From my experience working as a Community Mental Health Nurse, many of the individuals who were treated on the Psychiatric Service could have been treated in primary care if earlier.
Promoting a consistent, responsive and timely service
Family/ carer education
Specialist and advanced practice roles
Health promotion and social inclusion
Support
How can RPNs best promote social inclusion
Provide training and education
Reduce stigma and mental health promotion
Psychiatric nurses as mental health activists
Challenging negative beliefs
Adopt a holistic and collaborative approach
Promoting active engagement within services in the community
Developing and supporting eff ective leadership for psychiatric nurses
The final question asked at this stage of the consultation asked respondents to comment on how effective psychiatric nursing leadership could be developed and supported. Third, respondents suggested how a national leader could be useful in promoting, developing and supporting psychiatric nursing.
Supportive initiatives
The first indicated a need for supportive initiatives to help nurses develop their leadership skills. Finally, a number of respondents described how some leadership qualities are innate in certain individuals and that while they can be developed in some, completing an education or training program does not guarantee an effective leader.
Specialist posts
Introduction of national leader for psychiatric nursing
Leadership qualities
Summary
This chapter provides an overview of the most important findings from this phase of the consultation process. Their views on the values and principles that should underpin psychiatric nursing, as well as their views regarding the development of the role of the RPN to improve the reach and quality of services available to service users and families improvements were also investigated.
National Service Users Executive (2011) Engaging service users in mental health services - Changing the balance of power. National Suicide Research Foundation (2004) Young people's mental health: A report of the findings of the lifestyle and coping survey.
Guiding Principles Descriptor (HSE, 2011)
Clinical Governance Development… an assurance check for health service providers
Information letter & Survey
Organisations websites which promoted this project information
Flyer to advertise study
Vision for Mental Health Nursing: Inform your Future
Focus group information letter*
Consent form - Focus groups
Schedule for Focus Groups*
Schedule for Focus Groups* (continued)
Focus Group Questions
Invitation to make a written submission
Invitation to make a written submission (continued)
Completed focus groups*
Received Written Submissions
Ethics
ISBN 978-1-906218-47-8 March 2012
Dr Steevens’ Hospital Dublin 8
Ireland