The 19th century witnessed so many discoveries and advances in the field of medicine and public health. Public health in the 21st century must address these health inequalities to reduce the incidence of disease and improve health and well-being. The WHO was established as a specialized agency of the United Nations to serve as a coordinating authority on international public health issues.
The rising prevalence of obesity in the United States and around the world is growing faster than that of any other public health condition. Her chapter explores why a human rights framework is essential to public health work. It is the purpose of this multi-volume reference text to identify and analyze the diversity of work being done in the contemporary public health landscape.
Descriptive epidemiology of common mental disorders in the United States. Annu Rev Public Health.
GLOBAL POPULATION HEALTH
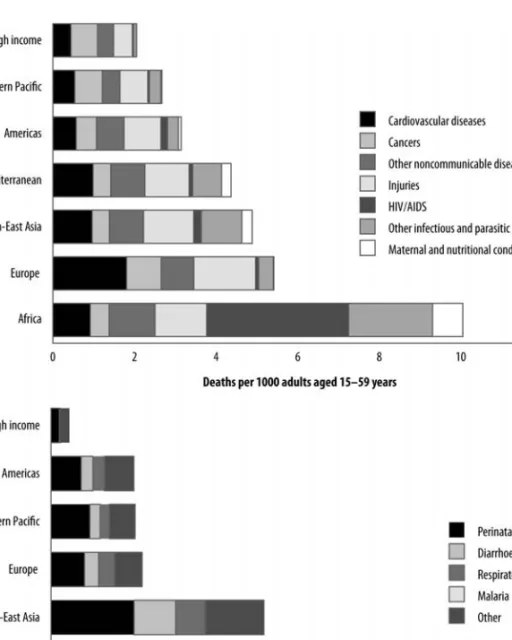
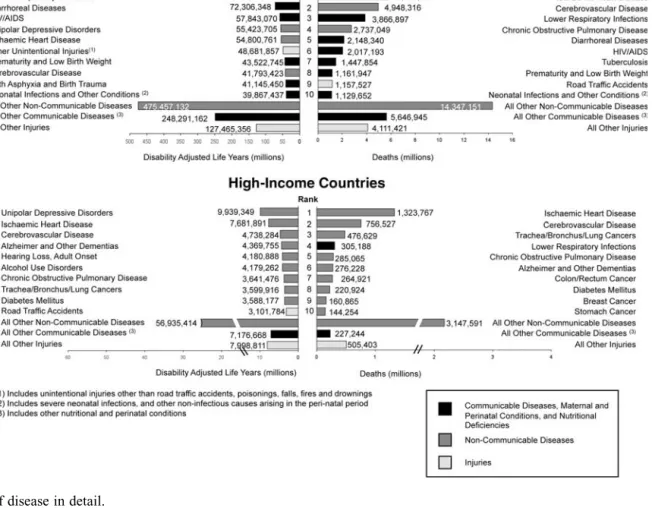
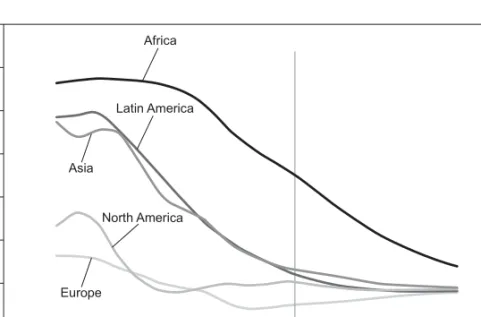
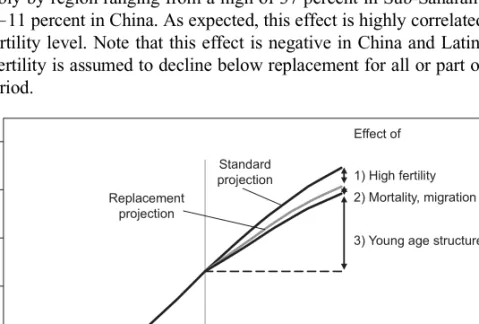
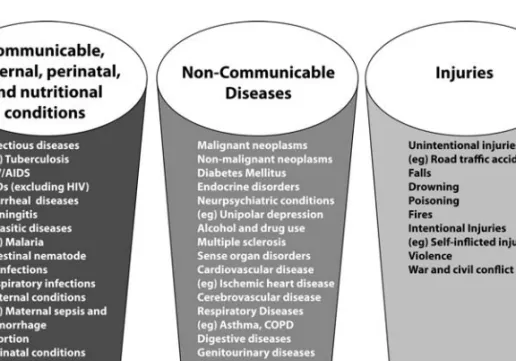
Because the prevailing public health literature is limited to the parameters of the WHO definition, the burden of disease in this chapter is defined in the above sense. As we have discussed, developing countries bear a disproportionate burden of the global share of diseases. Comprehensive family planning and reproductive health services were provided in the treatment area of the experiment.
Special groups may be at greatest risk of being affected by heat in urban areas. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change.
Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Analyzes of the effects of global change on human health and welfare and human systems. Contribution of Working Group II to the Third Assessment Report of the Intergovernmental Panel on Climate Change.
Climate change and the potential for range expansion of Lyme disease vectorIxodes scapularisin Canada.Int J Parasitol. Currently, 80 percent of the poor do not live in Africa or in the poorest countries. The double burden of the costs of chronic diseases and diseases associated with poverty coexist.
Ejeta was given this honor for his great contribution to the production of sorghum, one of the five main grains in the world. Unedited draft report of the 17th expert committee on the selection and use of essential drugs.
PUBLIC HEALTH PREVENTION AND SAFETY
Many of these workers now show evidence of preventable lung disease, caused at least in part by OSHA's decision not to enforce its rules requiring the use of respirators.[28, 29] The aftermath of the attack revealed other problems. stubborn: public servants. not covered by the OSHA act, overlapping and unclear government jurisdictions, thousands of migrant and temporary workers without clearly defined employer-employee relationships, and a lack of rules for basic safety and health management programs, medical surveillance, or exposure assessment. Second, aside from anecdotal evidence, little evidence suggests that OSHA's consulting and other voluntary programs, which account for 28 percent of its 2003 budget, have had a measurable impact on hazards, injuries, or illnesses.[6] US National Institute for Occupational Safety and Health. The changing organization of work and the safety and health of working people: Knowledge gaps and research directions.
It is estimated that foodborne illness causes 76 million illnesses, 325,000 hospitalizations, and 5,000 deaths each year in the United States.[2] Resulting medical costs and productivity losses range from $6.6 billion to $37.1 billion.[3] This cost estimate is conservative and does not cover the full spectrum of foodborne illness, but only seven major foodborne infections in the US as of 1996. In the United States, salmonella are among the most common causes of bacterial foodborne illness, with more than an estimated million cases per year.[2] The U.S. Centers for Disease Control and Prevention (CDC) Foodborne Diseases Active Surveillance Network (FoodNet), which annually tracks the prevalence of salmonellosis in the United States, found a less than 10 percent reduction in human cases between 1996 and 1998 and 2007. reported. .[8] The American 2010
Tennessee infections in 47 states from August 2006 to May 2007 raised concerns about the microbiological safety of peanut butter.[19, 20] The outbreak strain was isolated from several jars of peanut butter, and contributing factors to the outbreak included water from a leaky roof and a sprinkler system in the roasting area of the oven. These individuals have increased susceptibility to infection, greater likelihood of more severe illness, including death, and increased potential for illness with an opportunistic pathogen.[43] Conditions in the immunocompromised that predispose them to foodborne infectious agents include inflammatory bowel disease, malignancy, immunosuppressive medications, chronic medical conditions, and HIV/AIDS.[44] The global immunocompromised population continues to increase due to the HIV/AIDS epidemic, life-prolonging treatment of immunodeficiency diseases, and the use of chemotherapy and immunosuppressive drugs in cancer and transplant patients. Recognizing the current data gaps, the World Health Organization (WHO) convened a group of international scientists for the ``WHO Consultation to Develop a Strategy for Estimating the Global Burden of Foodborne Disease'' in September 2006.[45] The consultation formed the strategic framework for assessing the burden of foodborne diseases, including a roadmap for collating existing information on the burden of disease and a time frame outlining the individual strategic activities.
For example, ICH's purposes are to promote agreement on standards for preclinical research, assessment of clinical trials for efficacy and safety, and management of drug quality and purity.[14] ICH's technical working groups are composed of representatives of pharmaceutical industry organizations as well as drug regulatory authorities from the EU, Japan and the USA. However, when epidemiological evidence suggested a small increase in the risk of cerebral hemorrhage in young, first-time users of cold medications containing phenylpropanolamine, the FDA quickly urged manufacturers to voluntarily remove this ingredient. .[16] The increase in relative risk was modest (less than 1.5 for users of over-the-counter cold remedies), and the absolute excess risk was estimated at 1 per 300,000 people to 1 per 3 million persons. Side effects,'' the lay term for side effects, are despised by pharmacovigilance professionals, probably because of its clarity.
An IOM report issued in September 2006 presented an unsatisfactory picture of FDA's post-approval safety systems.[25] The report cites a crisis of confidence that is undermining the credibility of both the FDA and the pharmaceutical industry. The FDAAA authorizes the agency to determine the content and ensure that important new safety information is promptly and clearly presented to prescribers.[31] The FDAAA also gives the FDA extensive authority to set conditions for the marketing and distribution of drugs.
PUBLIC HEALTH CONCERNS OF SPECIAL NEEDS POPULATIONS
The Institute of Medicine (IOM) [1] refers to disability as ``the nation's greatest public health problem,'' affecting not only the health of people with disabilities, but also their immediate families and the population as a whole. The evolving definition of disability presents an important obstacle to understanding what is needed for people with disabilities to maintain good health and functioning. The medical model of disability used in public health defines disability as a condition resulting from an underlying pathology.
This model posits only individual-level etiological factors (for example, injuries, accidents and congenital abnormalities) and equates disability with a state of ``unhealthy''. As a result, much of the focus in public health has remained in the area of ''disability. This model emphasizes the idea that people with disabilities can lead healthy and productive lives with the necessary support. However, healthcare policies based in the medical model still present barriers to access to healthcare, prevention and rehabilitation-related services for people with disabilities.
While advances in assistive technologies have generally improved access for people with disabilities to most public services and transportation, they have not greatly increased their access to health care facilities (for example, many health care facilities and clinics remain physical). inaccessible and many lack appropriate medical equipment to adequately meet the health care needs of people with disabilities). A contribution to this may also be the wariness of people with disabilities to be helped by a system that is so medically model-driven. This chapter highlights the role of public health in improving the health, well-being and overall quality of life of people with disabilities by considering epidemiological trends in the prevalence of disability, including issues related to health disparities, legal and regulatory environment that influence access to preventive and curative health services, methods for measuring and monitoring the population of people with disabilities, and specific public health priorities.
Future directions are also discussed, outlining ongoing efforts (in the United States and globally) in public health policy, program development, and research to improve the health and well-being of people with disabilities. The multifaceted nature of disability makes it difficult to adequately define, which limits the ability of public health agencies to systematically respond to the health care needs of people with disabilities. In addition to addressing research inconsistencies, another priority is to establish a framework for the development of a global common nomenclature. [17, 18] The International Classification of Functioning, Disability and Health (ICF) provides a consistent language for describing the components of health. and health-related conditions for people with disabilities across disciplines and across countries.[19] The ICF includes not only functional assessment, but also takes into account environmental and contextual factors that influence human functioning.[13]2.