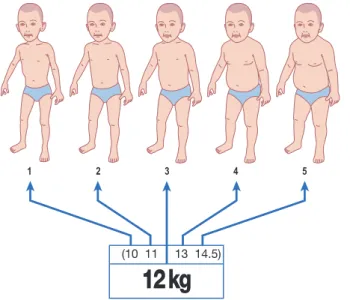
Specialist Emergency Physician and Registrar Program Director, Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand; Head of the Emergency Department. Review all information presented and familiarize yourself with the layout of the book. Go to the page of the book with the correct weight, or the nearest weight if that exact weight is not listed.
This is the generic name of the drug, with an indication of the route of administration if more than one appears. This is the suggested dilution of the drug to ensure a manageable volume to administer accurately: this should be a balance between too much volume (especially for infants less than 10 kg) and too much. This is the size of the syringe needed to prepare the diluted drug solution.
This is the milliliter volume of the diluted solution to be given via intravenous or intraosseous tube. The milligram dose of the drug to be infused with the amount of diluent to be added is shown.
Newborn / Small Infant
Include a pharmacist as part of the resuscitation team, if possible, to assist with the emergency medication administration process. The approach to resuscitation of the pediatric patient should be pre-planned and standardized, both in the general emergency medical care and the specific medication administration system. They should be available to all members of the resuscitation team and not just one person.
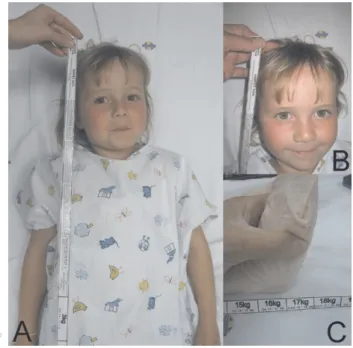
Part of the standardized approach to pediatric resuscitation should include references for a number of body weight estimation methods, including a height-based weight estimation method (e.g., the PAWPER tape or Broselow® tape). This is unprofessional and unnecessary, and rather reflects the team leader's lack of competence and confidence. To complete this task (which is of paramount importance), both the needs of the group and the individuals must be addressed.
ABWIBWUse TBW for the dose recommended in this book at the lower end of the range. These drugs are included because of the importance of early antibiotic therapy (as part of early targeted therapy for sepsis among others) starting in the ED.
Small Neonate
1 5 4mg/2mL undiluted (2mg/mL) 0.6
1 5 4mg/2mL undiluted (2mg/mL) 0.8
Cardioversion 1J/kg Joules - use the nearest higher setting for the indicated energy level if this exact setting is not available.
5 4mg/2mL undiluted (2mg/mL) 0.9
Adjust the dose according to the indication; warm up before use Joules - use the closest higher setting to that shown.
5 4mg/2mL undiluted (2mg/mL) 1.5
Infant
5 4mg/2mL undiluted (2mg/mL) 1.8
5 4mg/2mL undiluted (2mg/mL) 2
5 4mg/2mL undiluted (2mg/mL) 2.4
5 4mg/2mL undiluted (2mg/mL) 2.7
Toddler
5 4mg/2mL undiluted (2mg/mL) 3
Small Child
Metronidazole 7.5mg/kg/dose tds 500mg/100mL (5mg/mL) 18 21
5 4mg/2mL undiluted (2mg/mL) 3.5
5 4mg/2mL undiluted (2mg/mL) 4
Child
5 4mg/2mL undiluted (2mg/mL) 4.5
5 4mg/2mL undiluted (2mg/mL) 5
5 4mg/2mL undiluted (2mg/mL) 6
5 4mg/2mL undiluted (2mg/mL) 6.5
Large Child
5 4mg/2mL undiluted (2mg/mL) 7
5 4mg/2mL undiluted (2mg/mL) 8
Young Adolescent
Adolescent / Small Adult
Adolescent / Small Adult
5 4mg/2mL undiluted (2mg/mL) 8
10 20mg/2mL undiluted (20mg/mL) 2
In true emergencies, however, if a previous reaction to a drug was not severe and if there is no alternative drug to use, that drug or one in the same class can be used with due caution. Methylxanthines may antagonize the effects of adenosine - so it is less effective in patients taking theophylline or caffeine - the usual dose may need to be doubled. High dose adrenaline should not be used in cardiac arrest as it has been shown to worsen the outcome compared to standard dose adrenaline.
Amiodarone can be used for many arrhythmias in the ED but especially refractory VF/VT as well as stable wide- and narrow-complex tachycardias. Should ideally be diluted with D5W; in an emergency and if the drug must be administered immediately, many experts believe that any diluent can be used. Amiodarone diluted in D5W at concentrations less than 150 mg/250 ml (or <0.6 mg/ml) can be unstable and ideally should not be used for an infusion.
Emergency drug dosage antihistamines can also be used, but have a greater potential for side effects. Fresh blood (<5 days old) should be used as it results in a higher survival rate in children requiring resuscitation from major bleeding. This formula should not be used to calculate blood requirements in the acute phase of hemorrhagic shock.
Calcium chloride should only be used for acute or acute indications for IV calcium administration. Calcium gluconate should be used for less urgent conditions due to the greater safety of this solution. A synchronized shock should be used for perfusion of arrhythmias other than polymorphic ventricular tachycardias - here an unsynchronized shock will work better.
There is no evidence as to which energy levels should be used with biphasic waveform cardioversion and the recommendation is to use the same as for monophasic machines. Clonazepam can be used to abort status epilepticus; has an anticonvulsant effect of longer duration than diazepam and similar to lorazepam. Etomidate may also be used for procedural sedation (especially the cardio version), but propofol or ketamine are generally the preferred agents for most indications.
CONCENTRATE Overview
Doses should be adjusted in patients with hemodynamic compromise - in general, a half-strength dose is used in these patients. If used for PSA, doses should be carefully titrated to about 0.1 mg/kg.
CONCENTRATE Overview
In children with head injury, premedication with high-dose fentanyl before RSI has some effect in reducing the effects of the sympathetic stimulation induced by laryngoscopy and tracheal intubation. Conversion from fosphenytoin to phenytoin takes about 15 minutes, so make sure the patient has been given another form of anticonvulsant medication before starting fosphenytoin. In patients with pulmonary oedema, furosemide increases systemic venous capacitance, thereby reducing left ventricular filling pressure (preload).
Either intermittent bolus therapy or furosemide infusions can be used with equal safety and efficacy. Glucagon for hypoglycemia is not effective in patients with marked depletion of liver glycogen stores, such as in starvation, adrenal insufficiency, or chronic hypoglycemia. Can be used as an alternative to atropine for the management of organophosphate poisoning.
In patients who are not catecholamine depleted, ketamine releases catecholamines and stimulates the sympathetic nervous system, thereby increasing heart rate and blood pressure. This may increase ICP in patients with head injury, although cerebral perfusion pressure is maintained. Ketofol is a mixture of propofol and ketamine that can be used for procedural sedation or RSI.
Although useful, ketofol has yet to be studied under a wider range of uses and clinical conditions and should be used with care. Ketorolac is an anti-inflammatory drug that has been widely studied in children, primarily for the management of postoperative pain. It is therefore prudent to administer a judicious fluid bolus prior to the administration of labetalol.
Lidocaine is a second-line agent for the management of ventricular fibrillation and ventricular tachycardia. It can also be used before RSI in head-injured children to improve the autonomic response to intubation and. In emergency endotracheal intubation, lidocaine administration prior to intubation may mitigate the catecholamine effects of pharyngeal/laryngeal manipulation in patients where elevated ICP or elevated BP may be detrimental.