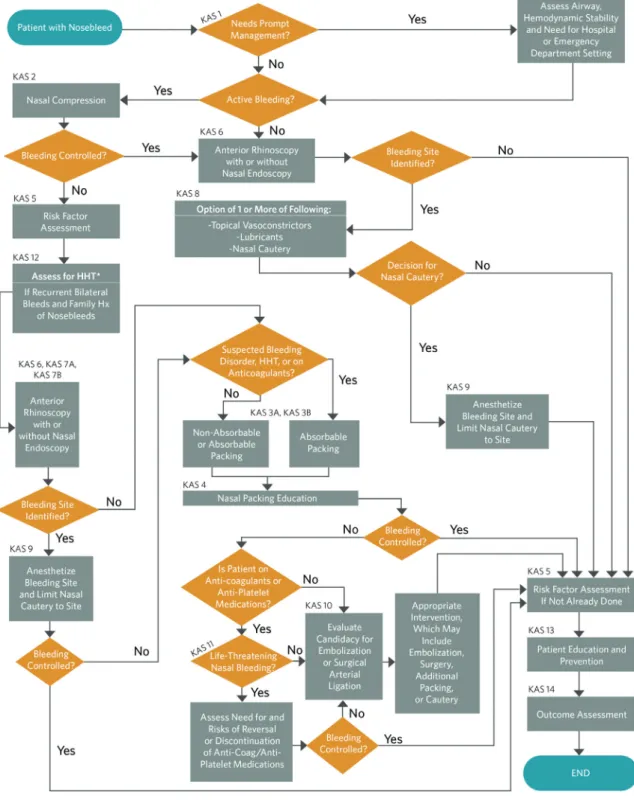
It is not intended to be a comprehensive, general guide to the management of patients with epistaxis. Physicians should use resorbable dressings for patients with suspected coagulation disorders or patients using anticoagulant or antiplatelet medications. In patients with ongoing active bleeding, nasal packing may slow or stop bleeding and facilitate intranasal examination to allow additional definitive control of bleeding.
The patient should understand that bleeding may recur during packing and/or Table 6. Nasal Packing: Frequently Asked Questions for Patients with Nosebleeds.

ANTERIOR RHINOSCOPY TO IDENTIFY LOCATION OF BLEEDING: The clinician
However, blood pressure should be monitored in patients with epistaxis, and decisions about blood pressure control should be based on the severity of the epistaxis and/or the inability to control it, individual patient comorbidities, and the potential risks of blood pressure lowering. INVESTIGATION USING NASAL ENDOSCOPY: The clinician should perform, or refer to a clinician who can perform, nasal endoscopy to identify the site of bleeding and guide further treatment in patients with recurrent epistaxis despite previous treatment with packing or cautery, or with recurrent unilateral nosebleeds. Recommendation based on observational studies and a preponderance of benefit over harm. Advantages: Improves localization of bleeding sites, improves identification of patients with posterior bleeding, improves identification of patients with nasal and nasopharyngeal pathology including tumors, reduces time needed to control bleeding, reduces unnecessary interventions, uses video or photo documentation to improve care and communication with patients/care team.
The clinician may perform, or may refer to a clinician who can perform, nasal endoscopy to examine the nasal cavity and nasopharynx in patients with epistaxis that is difficult to control or when there is concern for underlying pathology. unknown contributor to epistaxis. Option based on observational studies with a balance of benefits and harms. Benefits: Improved localization of bleeding sites, improved identification of patients with posterior bleeding, improved identification of patients with nasal and nasopharyngeal pathology including tumors, reduced time needed to control bleeding, reduced unnecessary intervention. The purpose of these statements is to make physicians aware of the benefit of evaluating the nasal cavity and nasopharynx with nasal endoscopy with a rigid or flexible scope in certain patients with epistaxis.
In a large case series, epistaxis was the prominent symptom in 7% of patients with a nasal foreign body. While the conditions listed here warrant evaluation with nasal endoscopy, they are not an exhaustive list of indications for endoscopy in the management of patients with epistaxis. The recent guidelines of the French Society of Otorhinolaryngology for adults with epistaxis recommend nasal endoscopy in the evaluation of all patients with epistaxis, even when ectasia of Kiesselbach's plexus is seen.50 The decision to proceed with nasal endoscopy in less severe epistaxis should be discussed with the patient or relatives, with the benefits of the procedure outweighed by the risks.

APPROPRIATE INTERVENTIONS FOR IDENTIFIED BLEEDING SITE: The clinician should
Risk, harm, cost: procedural discomfort, cost of the procedure, lack of availability, risks of topical medications (anesthetics and decongestants), nasal bleeding risk of endoscopy. This procedure can assist in localizing the site of bleeding (either anterior or posterior) and direct treatment of active or recurrent bleeding.7,85 Statement 7a recommends that nasal endoscopy be performed for patients with persistent bleeding likely to be at high risk from either bleeding from a posterior source or bleeding secondary to underlying nasal pathology. Such recurrence of epistaxis is more commonly seen in those patients with bleeding from areas other than Kiesselbach's plexus and when the site of bleeding is not located at initial evaluation.9,75,77 With nasal endoscopy, the site of bleeding can be localized in 87% up to 93% of cases.7Posterior epistaxis can occur from sites on the septum (70%) or the lateral nasal wall (24%), making targeted therapy difficult without endoscopic identification of the source of bleeding.85.
Recurrent unilateral epistaxis, especially when associated with unilateral nasal obstruction, may be a sign of a nasal or nasopharyngeal mass or foreign body and should prompt evaluation with endoscopy of the nose and nasopharynx. The consensus statement of the British Rhinological Society strongly recommended, although based on low-quality evidence, that cauterization of an identified bleeding site be used as first-line treatment. Anesthesia of the nose is usually accomplished with local anesthesia, usually topical lidocaine or tetracaine.
The available evidence, although limited, suggests that cautery is better tolerated and more effective than packing, regardless of the cautery method.107 A randomized controlled trial of cautery for epistaxis showed that bipolar cautery was less painful with faster healing. faster than monopolar cautery.9. Evidence from a systematic review carried out as part of the UK epistaxis audit suggests that electrocautery is more effective than chemical cautery and any other method. Cauterization should be performed with a direct view of the target bleeding site to prevent excessive tissue damage and increase the chances of success.
LIGATION AND/OR EMBOLI- ZATION FOR PERSISTENT NOSEBLEEDS: The clini-
Electrocautery, especially bipolar cautery, may be preferable in terms of effectiveness, comfort, and cost compared to other early interventions.107,110 However, equipment availability and technical expertise limit the use of electrocautery, especially in the office setting. Traditionally, ligation of the anterior and posterior ethmoid arteries required an open approach and dissection along the medial course. Given the proximity of the posterior ethmoid artery to the optic canal in the posterior orbit, many surgeons have chosen to ligate the anterior ethmoid artery alone when performing open surgery for epistaxis to minimize the risk of vision loss.
Endovascular embolization of the anterior and/or posterior ethmoid arteries is contraindicated because they arise from the ophthalmic artery and carry inherent risks of blindness with such a procedure. Endovascular embolization is most appropriate for posterior epistaxis, and current practice of interventional radiologists and interventional neuroradiologists includes embolization of the bilateral sphenopalatine/distal internal maxillary arteries and, in selected cases, of the facial arteries that have an anastomotic connection(s) with the sphenopalatine artery via the infraorbital artery and alar and septal branches from the anterior nasal compartment. Brinjikji et al. demonstrated similar transient ischemic attacks in all groups, but increased stroke risk in the groups undergoing embolization alone (0.9%) or combined with surgical ligation (1.6%), compared with surgical ligation alone ligation (0.1%).37 .
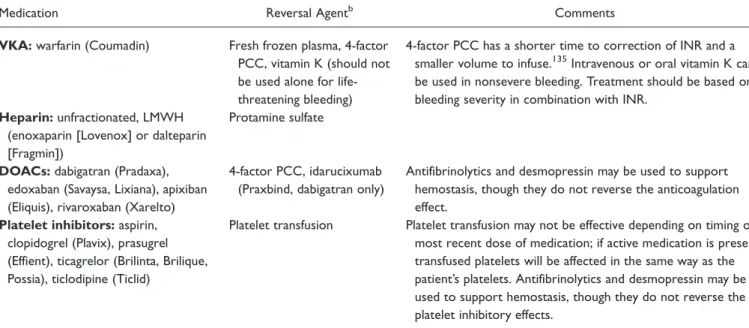
MANAGEMENT OF PATIENTS USING ANTICOAGULATION AND ANTI-ATROBOCATES: In the absence of life-threatening bleeding, the physician should institute first-line treatment prior to transfusion, reversal of anticoagulation, or withdrawal of anticoagulants/antiplatelets in patients using these drugs. Antifibrinolytics prevent thrombus breakdown by inhibiting plasmin and preventing dissolution of the fibrin clot.105 A small randomized controlled trial in patients taking antiplatelet drugs showed that topical TXA was superior to standard anterior nasal packing in stopping epistaxis. within 10 minutes of application (73% vs. 29%; P Patients receiving topical TXA were also less likely to experience rebleeding within the next 7 days. 105. In patients at high risk of thrombosis, who do not require urgent rever- regarding their anticoagulation, the physician managing the anticoagulation and comorbid conditions should be consulted regarding hemostatic management, especially regarding changes in the patient's treatment plan.
HEREDITARY HEMORRHAGIC TELANGIECTASIA (HHT) IDENTIFICATION: The
Opportunity for quality improvement: To identify patients with HHT and refer them to the appropriate specialist for assessment and management of associated conditions (National Quality Strategy Domains: Patient Safety, Prevention and Treatment of Leading Causes of Morbidity and Mortality). Advantages: Allow earlier diagnosis of HHT, increase the use of resorbable packing for HHT patients, avoid inappropriate management of epistaxis Risk, harm, costs: Patient anxiety regarding possible The purpose of these statements is to improve the identification of patients with epistaxis who have HHT and to emphasize the importance of referral to a specialist with expertise.
Nosebleeds from telangiectasias are the main symptoms in 90% of patients with HHT.149,150 The frequency of epistaxis often increases with age, leading to anemia (low blood count), need for iron and blood transfusion, high medical costs, and a significant decrease in QOL in patients. with HHT. A review of current medications for the treatment of epistaxis in patients with HHT was recently published, summarizing the data supporting the long-term use of these adjuvants. 28,154 These reviews report that thalidomide can improve the severity and frequency of epistaxis, improve hemoglobin concentrations and reduce the need for blood transfusion. TXA has been shown to reduce the severity of epistaxis, as measured by the ESS,155 but did not improve hemoglobin levels, and selective estrogen modulators show promise in limited studies.28 Intravenous administration and local infiltration of bevacizumab has been shown to improve many clin. - cal factors in patients with HHT, such as frequency and duration of bleeding and ESS, but larger random Figure 5. (a).
Absorbable packing is preferred for HHT patients with active epistaxis, as removal of nonabsorbable packing may irritate the nasal cavity and increase the risk of rebleeding. While these absorbable materials are favored when a patient with HHT requires packing for epistaxis, specific studies of primary control of epistaxis and recurrence rates have not been published. Patients with HHT, diagnosed or undiagnosed, may initially present to an otolaryngologist or other clinician who treats epistaxis.
PATIENT EDUCATION AND PRE- VENTION: The clinician should educate patients with
Nnacheta, salaried employee of the American Academy of Otolaryngology – Head and Neck Surgery Foundation; Taskin M. Demographic, seasonal, and geographic differences in emergency department visits for epistaxis. Otolaryngol Head Neck Surg. British Rhinological Society multidisciplinary consensus recommendations on the hospital management of epistaxis.J Laryngol Otol.
Guidelines of the French Society of Otorhinolaryngology (SFORL): second-line treatment of epistaxis in adults. Economic evaluation of fseal compared to nasal packing for the treatment of anterior epistaxis. Laryngoscope. Trends in Epistaxis Embolization in the United States: A Survey of the Nationwide Inpatient Sample 2003-2010.J Vasc Interv Radiol.
Guidelines of the French Society of Otorhinolaryngology (SFORL): first-line treatment of epistaxis in adults. A prospective randomized controlled trial comparing Merocel and Rapid Rhino nasal tampons in the treatment of epistaxis. Eur Arch Otorhinolaryngol. Prospective study into the risk of not using prophylactic antibiotics for nasal congestion due to epistaxis.J Laryngol Otol.
Prospective clinical study of bleeding sites in idiopathic adult posterior epistaxis. J Otolaryngol Head Neck Surg. Cost-effectiveness analysis of endoscopic sphenopalatine artery ligation vs arterial embolization for intractable epistaxis. JAMA Otolaryngol Head Neck Surg.