190
Widjaja et al Med J IndonesSubcapsular hemorrhage
of
the
liver
after
laparoscopic
cholecystectomy,
a
case
report
Suwandhi
Widjaja*,
Sumanto
Simont, Aru Witjaksono
Sudoyol
Abstrak
Seorang wanita berusia44 tahun dengan diagnosis kolesistitis kronika denganbatu kandung empedutelnh dilakukan kolesitektomi laparoskopik. Setelah tindal<an, penderita mengeluh nyeri pada perut kanan atas disertai penurunan hemoglobin. Pada pemeril<sacn USG maupun CT-scan terlihat adanya perdarahan subkapsular hati pada lobus kanan dibawah diafragma. Pada laporan knsus
ini
dibahas mengenai etiologi komplikasi yang sangat jarang ini.
Àbstract
A woman of 44 years old with diagnosis of chronic cholecystitis with gall stones had undergone laparoscopic cholecystectomy. After the procedure, she complained of dull pain in the rtght upper abdomen with the declining of hemoglobin level. The USG and CT-scan examination showed hepatic subcapsular hentorrhage on the subphrenic right lobe. The causes of this very unsual complication was discussed
in
this report.Keywords
:
Iaparoscopic cholecystectomy, liver rupture, complicationLaparoscopic cholecystectomy
wasfirst
performed in
France
in
1987.''"
This
technique has
gained
remarkably rapid
widespread use
andacceptance
all
over
theworld, and
become the standardfor
thetreat-ment
of acute
as
well
as
chronic
cholecystitis.
Retrospective comparative studies between
laparo-scopic cholecystectomy and open
cholecystectomy
showed thatlaparoscopic cholecystectomy
resulted onshorter
hospital
stay, more
rapid recovery,
and mini-mal use o.fpostoperative
analgesiathan open cholecys-tectomy.-"
However,
the
laparoscopic cholecystectomy
were
comparable
with
opencholecystectomy
in
types
andnumber of complications.5 Complications of this
tech-nique
were problems related
to
distention
of the
peritoneal
cavity,
lack
of
depthperception afforded by
video image
andproblems related to new instruments
usedin
this
techn1qu".6Th"
most common
complica-tions
of
laparoscopic cholecystectomy were biliary
duct
injury
such
asstricture or bile
leakage,vascular
'
Research Laboratoryfor
Viral Hepatitis Atma Jaya School of Medicine, Jakarta, Indonesiaf Department of Internal Medicine, Faculty of'Medicine, University of Indonesia, Jakarta, Indonesia
injury
such as hemorrhage
or
arterio-biliary fistula,
infection/abscess, superficial wound infection,
andconversion
to opencholecystectomy.
Thesecomplica-tions
occurred
in
approximately
J.l%
to 7Vo
of
the
procedures dependàn
Ure""nt"ir.7'8'e
Although
there were several reports
of
unusual
com-plications
of
laparoscopic
cholecystectomy
reported
as
right
paranephric
s,r.rarterio-biliary
fis-enlc
rupture,
la
ih"r"
was no any
report
concernedabout
theliver
rupture
asthe complication
of
this
procedure.
In
this report
wepresent a
casewith
subcapsular hemorrhage
of
theliver
as
an
unusual
complication
of
laporoscopic
cholecystectomy.
CASE
RBPORT
Vol 8, No 3, July - September 1999
liver function
testsuch
as serumalbumin
was4.4 gldl,
globuline
was
2.3gldl,
direct and
indirect bilirubin
were 0.2
mg/dl
and0.1
mg/dl
respectively, the
trans-aminaseswere
l2Ull
for AST
andl6U/l
for ALT.
Theblood ureum
was 28mg/dl.
Laparoscopic cholecystectomy was performed on
thenext day,
in
accordance
to
the
standard
procedure,uneventful
courseof
theoperation
wasnotified.
After
the procedure, thepatient
wascomplained
ofdull
pain
in
the
right
upper
abdomen.
The physical
ex-amination
showed no
sign
of
acute abdomen or
hipovolemic shock, however, the hemoglobin level
progressively
declined,from
12.3 gVo to7 .8 g%o.Basedon
those
findings,
intra abdominal
hemorrhage
was suspected andUSG
wasperformed immediately.
TheUSG
showed multiple
hypoechoic structures
which
ran
rather
horizontally
among
the
fragmented
liver
tissue
within
subcapsular
liver
right lobe
space,just
beneath
the
diaphragrn. These
findings
were
com-patible
with
theliverrupture with
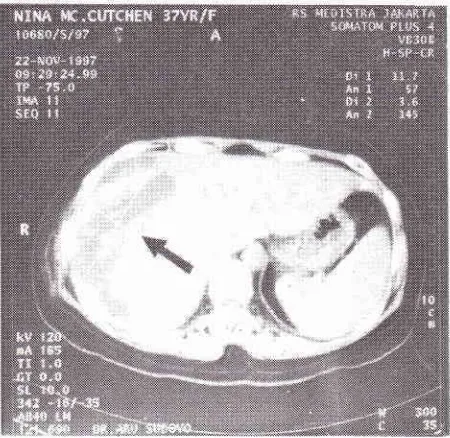
large hematoma. TheCT-scan
wasperformed
andconfirmed
thesefindings
Figurel [arrow].
Thesefindings
were
different
to thepre
operative
USG
,
in
which
the
liver
was entirely
normal without
any
lesion
at
all.
Since the patient's
general
condition
was
not
deteriorated and the
hemoglobin
level
wasnot
further declining,
thecon-servative treatment
with
blood transfusion was
ap-plied. The patients
showed
uneventful recovery
andwas
discharge
from the hospital on November
24th1997.
Figure 1. This CT-scan showed a large sub-capsular hematoma (arrow)
on
the subphrenic right lobe of the liver. The liver was torn horizontally rather vertically.Liver subcapsular
hemonhage l9l
DISCUSSION
The complications
of
laparoscopic cholecystectomy
are
divided
into
several catagories. Themost common
complications
are those
related
to
the lack
of
depthperception afforded
by video image
and
new
instru-ments
usedin this
technique.
In this group,
the most
complications
are
vascular
or biliary injury,
which
causes
the
such
bleeding, stricture
of biliary
duct or
biliary
leakage.
The other complications
are related
with
the introduction
of
laparoscopic instrument
through the abdominal
wall, which injures
the
major
blood
vesselsor
theintestines
.The
problerns
related
to
the distention
of
the peritoneal
cavity
arealso
animportant factor
to
convert
the
laparoscopic
ap-proached
to
open cholecystectomy.
This
complica-tions, such as
adhesions
due
to
prior
operation
or
previous
abdominal infection
may cause
the laparo-scopiccholecystectomy
becamemore delicate
andin-creased
the likelihood
of
convertion
to
open
cholecystectomy.
In
this
group
of
cornplications,
thecarbon
dioxide
pneumoperitoneum
used during
thelaparoscopic cholecystectomy
can cause adverselocal
and systemiceffects,
such as gasembolism,
hypercap-nia, acidosis,
andarrhyth*iur.r)'
ro' r7However,
subcapsular hemorrhage
of
the
liver
after
laparoscopic-cholecystectomy
so
far
was never
reported in
theliteratures,
thusthis
ismay
be
thefirst
report
in thejournal
.The
exact causeof liver
rupture
in
this
case
is
not clearly
defined
because
no
laparotomy
was
performed.
In
this
case,there
is
nohistory
of
abdominal operation, but
she hadobviously
chronic recurrent inflamation
of
the
gall
bladder,
which may induce the
adhesion
of
the
liver
to
thediaphragm
orthe abdominal
wall.
As
shown
on the
CT [figure
1], the
liver
was, torn
horizontally rather vertically.
This finding
supportsthe
suggestions
that the rupture may be due
to
thedisruption
of
the
liver
capsule
by
traction on liver
adhesion
to
diaphragm
by
pneumoperitoneum
or
oc-cured during
the
removal
of
the gall bladder.
This
suggestion may be comparablewith
the splenicrupture
after
laparoscopic
cholecystectomy
and
during
theexplorative abdominal
operation in which the
spleniccapsule
was torn on
its
adhesion
to
surroundings.la
One otherpossibility
is
thehepatic rupture
happeneddue to
injury
by theintroduction
of laparoscopicinstru-ment
during
the procedure.REFERENCES
[image:2.595.77.302.480.699.2]192
Widjajaetal
2. Dubois F, Icard P, Berthelot G, et al. Coelioscopic cholecys-tectomy: preliminary report of 36 case. Ann Surg 1990 ; 211
: 60.
3. Stoker ME, Vose J, O'Mara P, et al. Laparoscopic cholecys-tectomy: a clinical and financial analysis of280 operations. Arch Surg 1992;127 :589.
4. Glinatsis
MT,
Grifhth JP, McMahon MJ. Open vs laparo-scopic cholecystectomy: a retrospective comparative study.J Laparoendosc Surg 1992; 2 : 81.
5. Herrera MF, Chan C, Gonzalez-Ojeda A, Torres G, Mercado
MA,
dela
GanaL,
et al. Comparisonof
outcomes and complications for open and laparoscopic cholecystectomy in Mexico. J Laparoendosc Surg 1995 Oct; 5(5): 289-93.
6. Deyo GA. Complications of laparoscopic cholecystectomy. Surg Laparosc Endosc 1992Mac2(l):41, - 8.
7. The Southern Surgeons Club. A prospective analysis of I 5 I 8
laparoscopic cholecystectomies. New Eng J
Medl99l:324
:
l0?3.8. Graber JN, Schultz LS, PietrafittaJJ, Hickok DF. Complica-tions of laparoscopic cholecystectomy: a prospective review of an
initial
100 consecutive cases. Lasers Surg Med 1992;l2(l't:92
- 7.9. Wolfe BM, Gardiner BN, Leary BF, Frey CF. Endoscopic cholecystectomy. An analysis of complications. Arch Surg
l99l
oct;
126(10):ll92
- 6.10. Nishiyama
T,
TerunumaM,
SasakiK,
Hanyu S. Right paranepbric abscess as a rare late complication of laparo-scopic cholecystectomy. Int J Urol 1998 Mar; 5(2): 174 - 5.Med J Indones
ll.
CubillanaPL, EgeaLJA, Montiel MR, Gonzalez AP, Pastor GS, Campos RR, et al. Renal vein thrombosis caused by laparoscopic cholecystectomy. Scand J Urol Nephrol 1998 Feb; 32(l): 56 - 7.12. Kassasseya A, Z-iyani F, Rouffet F. Hemobilia after laparo-scopic cystectomy. Apropos of a case. Review of the litera-ture. Ann Chirurg 1997;51(2): 159 - 62.
13. Balsara KP, Dubash C, Shah CR. Pseudoaneurysm of the hepatc artery along with common bile duct injury following
laparoscopic cholecystectomy.
A
report ot two cases. Surg Endosc 1998 Mar; l2(3):276 - 7.14. Maw A, Puntis MCA. Delayed splenic rupture complicating laparoscopic cholecystectomy-case report and review.
Min-imally InvasiveTherapy 19971,6:87 - 91.
15. Liu SY, Leighton T, Davis I, Klein S, Lippmann M, Bongard
F.
Prospective analysisof
cardiopulmonary responses to laparoscopic cholecystectomy. J Laparoendosc Surgl99l;
I
:241 - 6.16. Wittgen CM, Andrus CH, Fitzgerald SD, Baudendistel
LI,
Dahms TE, Kaminski DL. Analysis of the hemodynamic and ventilatory effects
of
laparoscopic cholecystectomy. Arch Surgl99l
:126:997 -
1001.lT.Fitzgerald SD, Andrus CH, Baudendjstel LJ, Dahms TE,
Kaminski
DL.
Hypercarbia
during
carbon dioxide