diabetes
mellitus:
an
In-Microalbuminuria
in
non-insulin
dependent
donesian
experience
I
Gde RakaWidiana*, Rully
Roesli**,
Ketut
SuwitraTAbstrak
Pada DMTI (diabetes melitus tergantung insulin) dan DMTTI (diabetes melitus tak tergantung insulin), mikroalbuminuria dapat meramalkan komplikasi
ginjal dan
mortalitas tinggi. Deteksi awal dan terapidini dari berbagai
faktor penyerta mungkin dapat menurunkan albuminuria dan mungkin dapat menghambat progresivitas penyakit m.enuju gagal ginjal kronik. Berbagai penelitian mengenai mikroalbuminuria pada penderita DMTTI serta faktor-faktor yang terkait telah dilakukan di Indonesia. Mikroalbuminuria dijumpai pada lebih dari sepertiga (397o) penderita DMTTI dan seperempat (24.7Vo) penderita GTG (gangguan toleransi glukasa) di masyaraknt dan antora 26 sampai 57% penderita DMTTI di rumah sakit, Umumnya, penderita DMTTI dengan mikroalbuminurta ûdak gemuk. Pada penderita DMTTI dengan mikroalbuminuria, tekanan darah dijumpai lebih tinggi dan retinopati dijumpai Lebih sering dibandingkan penderita tanpa milcroalbuminuria. Namun, beberapa fraksi lipid pada profil lipid dijumpai lebih buruk pada penderita DMTTI dengan mikroalbuminuria daripada penderita dengan normoalbuminuria. Beberapa enzim tubulus ginjal, yakni NAG (N- asetil--glukosaminidase) dan IAP ("intestinal alkaline phosphatase") konsentrasinya dijumpai lebih tinggi pada penderita DMTTI denganmikroalbuminuia daripada pendertta tunpa mikroalbuminuria. Enzim-enzim
ini mungkin
dapat dipakai sebagai petanda gangguan fungsi tubulus pada DMTTL Pada dua studi perlakuan, captopril dilaporlan bermanfaat menurunkan albuminuria dan meningkatkan HDL-kolesterol pada penderita nefropati d.iabetikayang sebagian besar mengalami mikroalbuminuria (stadium insipien).Abstract
In both
IDDM and NIDDM, microalbuminuria predicn diabetic kilney disease and increased mortality. Early detection and treatment of associated factors may reduce albuminurta and retard the progression toward chronic renalfailure.
With regard to microalbuminuria in NIDDM patients and its associatedfactors, studies have been done in Indonesia. Microalbuminurtawas found in more thanone third(39Vo) of NIDDM patients andin one quarter(24.7Vo) of IGT patients in the community, andin26 to 57Vo of NIDDMpatients in the hospinl setting. Generally, NIDDM patients with microalbuminuria were non-obese. There was a higher blood pressure andmore retinopathy inmicroalbuminurtc NIDDM patients thaninnormoalbuminuric ones. However, the lipidprofile was inconsistentLy worse in microalbuminuric than normoalbuminuric NIDDM patients. Tubular enzymes namely NAG (N-acetyl-p -glucosaminidase) and
IAP (intestinal alkaline phosphatase) were found higher
in
NIDDM patients with microalbuminuria than those without microal-buminuria. These enzymes were proposed as markers of early tubular changes in NIDDM. In tvvo interventional studies, captopril was beneficialin
reducing albuminuria and increasing HDL-cholesterolin
nephropathy patients who mostly werein
the incipient ( mic r o a Ib uminur ic ) s ta g e of d iab e tic n e p hr op at hy.Keywords : non-insulin dependent diabetes mellitus, microalbuminuia, Indonesia
Diabetic nephropathy
is a leading causeofrenal failure
in
developed
anddeveloping countries.
It
developsin
approximately one-third
of patients with type
1
(in-sulin-dependent) and
in
similar number
of
patientswith
type
2
(non-insulin dependent) diabetes
and*
Department of Medicine Wangaya General Hospital, Bali, Indonesia**
Subd"port^ent of Nephrology & Hypertension Department
,
of Medicine, Padjadjaran University, Bandung, Indonesiat
Subdepartment of Nephrology & Hypertension Departrnentof Medicine, Udayana University, Bali, Indonesia
progressing in the
majority
to end-stage diseaserequir-ing
dialysis or
transplantation.' Diabetic
nephropathy
characterized
by
increased
proteinuria, raised
blood
pressure, and glomerular changes, carries 20 to 40
fold
increasedrisk
of early mortality.'
In IDDM
(insulin-dependent diabetes
mellitus)
nephropathy
with
end-stage
renal
diseaseusually
takes about25-30
yearsto
develop.
However, in NIDDM (non-insulin-
depend-ent
diabetesmellitus)
the natural
history
of
renal
dis-eases isnot
well defined.'
ges (stage
I).
StageII,
usually
terized by
normal
hyperfunc-glomeruli, without clinical
or
laboratory
signs.
In
stageIII,
taking
place
during
thesecond decade,
a very
characteristic abnormality
develops,
namely
microalbuminuria.
The
third
decade (stageIV)
is
characterizedby well-known clinical
ap-parent diabetic nephropathy,
with
macroproteinuria,
increasingblood
pressure, andlinear
fall
in
GFR,lead-ing to
end-stagerenal failure, namely
stageV.4
Thecourse
of
diabetic nephropathy
in
NIDDM
is not
yet
well defined.
The onserof
àiseàse inNIDDM
isuruuily
not
clearly
defined
and themetabolic
disarrangementmay not
be aspronounced
asit
is
in IDDM.
The
sameclassification may
be usedin
NIDDM
but thesituation
is
much more complicated and
somewhat different,
becausehyperfiltration
is
lesspronounced
and maybeabsent.'
In
IDDM,
microalbuminuria,
defined
asuri-excretion
20-200
pg
perd
as
stron
value
for
sub-disease.6-8
stage,microal-buminuria
is
aspecific
clinical
marker
that canpredict
clinical
nephropathy
in thefuture
courseofthe
disease. The stageof overt
clinical
diabetic nephropathy
which
characterized persistent
proteinuria
and reduced renalfunction
asthe main
symptoms,
is
considered
to
be ogressesto
end-stage acan also
predict
the patients.After
9 yearsreported
thatmicroal-buminuric
NIDDM
patients ha^ve
amortality
of
l48Vohigher than diabetic
controls.e
In NIDDM,
microal-buminuria
is
found
in
25Voof patients.
It
is
alsofound
quite common
at
diagnosis
of
NIDDM.IO
In
these patients, there may be a numberof factors
beside renaldisease
which
albumin excreti
sential renal
di
suspected.
NIDDM
patients have a significant increaseof
blood
pressure.
Abnormal
lipid
profiles are
alsofound
in
somebut not
all microalbuminuric
diabetes.5In
Indonesia, prevalence
of
diabetes rangesàetween
l-3Vo,
thenumber
can belarger
in big
cities
and thereis
a
trend
of
increase
in
its
prevalence.
All
types
of
diabetes can be
found, however,
asin
other countries,
the mostfrequent type found
isNIDDM.
The percent-ageof IDDM
is very small
andthere were
only few
reports
of
MRDM particularly from
Bandung,
Semarang,
Yogyakarta,
and Surabaya(Symposium
onThe
Paradigm
of
Diabetic
Nephropathy
and
Nephrocardiologic Complications
in
NIDDM,
Ban-dung 1996; The
IXth
KOPAPDI, Denpasar lgg3).
Reports in Indonesia showed that
diabetic nephropathy
was the second highest causeofend-stage
renal diseasewho
underwent maintenance
dialysis.
It
was reported
17.6Vo
in
Jakarta (Symposium
on
Management
Aspects
of
Kidney
Diseases,Jakarta 1990),
and22.5Voin
Yogyakarta (Darmaatmaja J, Unpublished Review
and Study Reports). The
Indonesian
Society of
Nephrology
in its
annual report, has reported
that
during 3
years
(1993
to
1995)
16-lgVo
of
end,-stagerenal failure
patients
with
maintenance hemodialysis
were
associatedwith
diabetes(Indonesian Society
of
Nephrology.
Annual report
1996,unpublished).
High
costof
replacement therapy
with
dialysis or
kid-ney
transplantation
are theonly
choice
tomaintain
life
in
these
patients. Therefore, possible preventive
measures
in
preventing
or
retarding
the
development
to
end-stagerenal
failure
is very important.
Early
detection may
bepossible by detecting
microal-buminuria
as aroutine
testfor
NIDDM
patients, at
aparticular situation.
Associated
factors that may
ag-gravate the development
to clinical
nephropathy
mayalso be detected
and treatedpromptly. This
paper
at-tempts
to
elucidate studies
in
Indonesia
regarding
microalbuminuria
and
associatedfactors
in
diabetesmellitus particularly in
NIDDM
patients that may
bebeneficial to
thepossible preventive
measures.EXPLORATIVE
STUDIES
Community-based
epidemiologic studies
to
explore
microalbuminuria
in
diabetes
is
rare
in
Indonesia.
Most of
the studies werehospital-based
with different
study
methods
and
subject selection.
In
Ujung
pan-dang,
Adam
&
Sampelingfound
rhat ourof
50NIDDM
patients examined,
44Vohad microalbum
inwia,
2g%ohad normoalbuminuria,
and 28Vo
with
macroal-buminuria (National
Congress
of
the
Indonesian
Society
of
Internal Medicine, yogyakarta 1990).
In
Surabaya,Soewanto
andTjokroprawiro
reported that
among
46 NIDDM
patients screened,
26.g%ohad
microalbuminuria
(National
Symposium
on
En-docrinology and Metabolism, Surabaya 1997). In
Yogyakarta,
Widiana
etal.
screened24-hours
urinary
samples
for
microalbuminuria
in
NIDDM
patients.Using qualitative
immunoturbidimetry
method,
among 104 patients examined,
57Vo
had
microal-bu mi n uri a, 33Vo normo albumin uri a, and I O Vo h ad
Soesilawati
et al.
in
Jakarta using semiquantitative
Micral
test@,found
3l.6To
of
NflpU
pàtients
hadmicroalbuminuria
(3rd
National
Congress
of
In-donesian
Society of Endocrinology,
Semarang 1993).A
community
based-study
was done
in
Singapama, west JavaProvince.
Thepopulation of this sub-district
of Tasikmalaya Regency was
113,401.The study
wascarried out
in
subjects aged
of
more than 20
years.Using the
selection
criteria,
28,571 patients
were screenedby Accutrend
test@for its blood
sugar. TheOGTT (oral glucose tolerance test)
was usedfor
con-firmation
of
the diagnosis
of DM
or IGT
(impaired
glucose
tolerance).
It
wasfound
that crude prevalenceof
NIDDM
was233
(1.03Vo) andcrude prevalence of
IGT was 5009
(l8.lVo).
Persistent
microalbuminuria
was
diagnosed when
at leasttwo out three
semiquan-titative
Micral
test conducted
within 6 months,
werepositive. The
results
of
the study
showed that
prevalence rate
of
persistentmicroalbuminuria
amongNIDDM
patients was
39Voand among
IGT
patientswas
24.'lVo.tl
OBSERVATIONAL
STUDIES
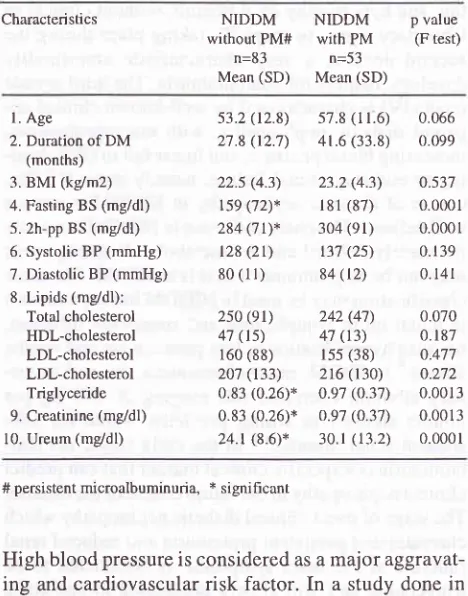
In
NIDDM,
subjects
with
microalbuminuria
were
older than
thosewithout microalbuminuria. This
may also berelated to
thelonger duration
of
the diseasein
NIDDM
with microalbuminuria
subjects compared tothose without. Other variables were also
analyzed.There was
no
significant difference found
in
BMI,
blood
sugarlevels, blood
pressure,lipid profile
in bothgroups
(seetable 1). Although statistically
it was
not
significantly
different,
subjectswith microalbuminuria
tend
to
have ahigher both systolic
anddiastolic blood
pressure. Nevertheless,
higher ureum
and creatinine
levels
werefound
in NIDDM
subjects.lI In this
study,urinary enzymes
were also examined, consisting of
NAG (N-
acetyl-B-D-glucosaminidase),
IAP
(intes-tinal
alkaline
phosphatase), and
TNAP
(tissue
non-specific
alkaline phosphatase). Elevation
of
theseenzymes
may reflect early tubular changes.
It
wasfound that concentration
of
theIAP
andNAG but not
the
TNAP
enzymes were increased inNIDDM
patientswith
persistent
microalbuminuria
compared
to
thosewithout
microalbuminuria. It was also shown
that
NIDDM
patients
with
microalbuminuria had higher
frequency
of high IAP (>
2Ulgr)
andhigh NAG (>
5U/gr) levels
than thosewithout
microalbuminuria,
thatis
44.4Vovs
33.8Vofor IAP level
and74.lVo vs
68.17ofor NAB level, consecutively.l
ITable
l.
Characteristics of NIDDM patients with and withoutpersistent microalbuminuria (adapted from Roesl i, I 996) I I
Characteristics
NIDDM NIDDM
p valuewithout
PM#
withPM
(F test)n=83
n=53Mean
(SD)
Mean (SD)l. Age
2. Duration of DM
(months) 3. BMI (kg/m2)
4. Fasting BS (mg/dl)
5. 2h-pp BS (mg/dl)
6. Systolic BP (mmHg)
7. Diastolic BP (mmHg)
8. Lipids (mg/dl): Total cholesterol
HDL-cholesterol LDL-cholesterol LDL-cholesterol Triglyceride
9. Creatinine (mg/dl)
10. Ureum (mg/dl)
s7.8 (r 1.6) 0.066
4r.6 (33.8) 0.099
23.2
(4.3)
0-s37 181(87)
0.0001 304(91)
0.0001t1't
(2s)
0.13984(t2)
0.141242
(47)
0.070 47(r3)
0.187 155(38)
0-477 216(130)
0.272 0.97(o.3'7)
0.0013 o.97(0.37)
0.0013 30.1(13.2)
0.0001 53.2 (t2.8)27.8 (12.7)
22.s (4.3) 159 (72)x 284 (7 t)*
t28 (2r)
80(ll)
250 (el) 47 (ts) 160 (88)
zj't
(133)0.83 (0.26)*
0.83 (0.26)*
24.1 (8.6)*
# persistent microalbuminuria, * significant
High blood
pressure is considered as amajor
aggravat-ing
andcardiovascular
risk factor.
In
astudy
donein
Yogyakarta,
Widiana
has
reported that NIDDM
patients
with
persistent
microalbuminuria
diagnosedas
incipient
diabetic nephropathy
had
significant
higher blood
pressure thanNIDDM
patients with
nor-moalbuminuria.
This study
recruited34
patients
with
incipient
diabetic nephropathy and
34
controls
(NIDDM
patients
with
normoalbuminuria),
matchedfor
age and sex. Patients
with
incipient
diabetic
nephropathy
tend to have
longer diabetes (mean
5.9 years vs4.2
years) and had morefrequent retinopathy
(50.0Vo
vs
I7.6Vo).
Most
of
the retinopathy
in
both
groups was
of
the background
type. However,
since ageof
both
groups
was similar means that
microal-buminuria may be related
to
the
longer onset
of
NIDDM
(see table
2).
Blood
pressure
were found
higher both
in
systolic (143
+
I
mmHg
vs
127+
ll
mmHg, p < 0.05)
andin diastolic (89 + 9 vs 81
+
ll
mmHg,
p <
0.05)
in
patients
with
incipient diabetic
nephropathy
than thosewithout
diabetic nephropathy.
Diastolic blood
pressure
of
95 mmHg
or
more
wasfound
morefrequent
in incipient diabetic nephropathy
patients than those
without diabetic nephropathy
(32Vovs
l1Vo, p < 0.05). Poorcorrelation
wasfound
between [image:3.595.309.543.112.410.2]Table
2.
Clinical characteristics of NIDDM parients with and withoutIDN* (adapted from Widiana et al., 1993)12
patients
with microalbuminuria
waslower
than thatin
NIDDM
patientswithout microalbuminuria.
Besideof
high
totalcholesterol
and lowHDL-
cholesterol
levels,NIDDM
patients
with microalbuminuria
had also an
abnormal fraction
of
lipids
including
ratio
of
total
cholesterol/HDl-cholesterol which is more
than 4,5.Triglyceride
andLDl-cholesterol
levels were
similar
between
two
groups.It
was alsofound
thatretinopathy
was more frequent among
NIDDM
patients with
microalbuminuria
than thosewithout.
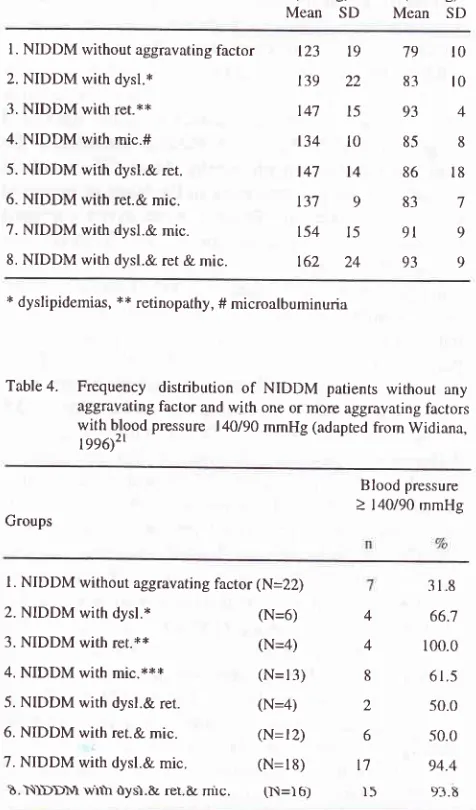
Table
3.
Blood pressurein
106 NIDDM patients without any aggravating factor and with one or more aggravating factors (adapted from Widiana, 1996)'''Groups
Blood pressure
Systolic
Diastolic (mmHg) (mmHg) MeanSD
Mean SD CharacteristicsNIDDM
NIDDMwith
IDN
withoutIDN
p valuen=34
n=34Mean
(SD)
Mean (SD)I. MÆ
2. Age (years)
3. Duration of DM (years) 4. RBW** (7o)
5. Retinopathy Background type Proliferative type
6. Neuropathy
l7/ t7 47.91 (13.03)
5.92 (4.64) 86.32 (17.06)
l7 (50.080) t4
3
t8
l'7 I t7 47.4t (t3.6'.1)
4. r6 (3.68) 86.76 (22.s9)
6 (t7.6Eo)
5
I
l3
0.438 0.062 o.464
0.010
0.330
x Incipient diabetic nephropathy, ** Relative body weight
To
determine
therelationship
betweenblood
pressureand some aggravating factors
namely
dyslipidemias,
diabetic
retinopathy,
and microalbuminuria inNIDDM
patients, Widiana,
in
Yogyakarta has
screened 106
NIDDM
for
blood
pressure,
lipid
profile,
and
the presenceof
retinopathy
andmicroalbuminuria.l3
Out
of
those patients;
44
(4l.5Vo) had dyslipidemia,
36 (34.2Eo) haddiabetic retinopathy,
and 59(55.6Vo)had
microalbuminuria. It
wasfound,
thatNIDDM
patientswith
one
or
more of the three
(dyslipidemia,
retinopathy,
and
microalbuminuria)
aggravating
fac-tors had
higher blood
pressure than thosewithout
anyaggravating
factor. Meanwhile,
patients
without
anyaggravating
factor had
mean
blood
pressure
around 120180mmHg
(see
table 3). Most
of
parienrs
wirh
aggravating factors had
a meanblood
pressureof
morethan
140/85
mmHg, levels
of
which
is
considered to
increase cardiovascular
morbidity
and
mortality in
diabetes
and should
betreated.
Fifty
percent
or
morepatients
with
oneor
more
abovementioned
aggravat-ing
factors had
ablood
pressureof
140190mmHg
or
more. Meanwhile, around
307oof
NIDDM
patientswithout
anyaggravating factor
had ablood
pressureof
140190or
more (see
table
4).In
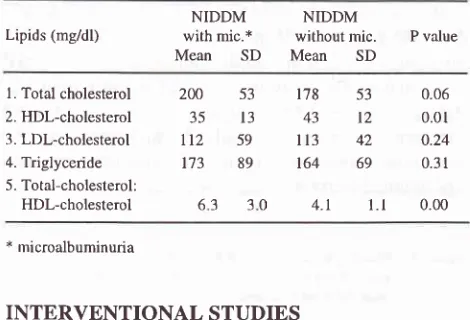
another study
involving
68NIDDM
patients, other
aspect
of
cardiovascular
risk
factor,
namely
dys-lipidemia
was evaluated.l4It *us
reported that thetotal
cholesterol level
in
NIDDM
patients
with
microal-butrrr.tr'.rtir.
srrs
KigKe,tt\l.ir. tK.l!
{s.sr{
\rr
\\\\\\(
patients without microalbuminuria
(see
table
5).
In
contrast,
the HDl-cholesterol level
in
NIDDM
l. NIDDM without aggravating factor
2. NIDDM with dysl.* 3. NIDDM with ret.**
4. NIDDM with mic.# 5. NIDDM with dysl.& ret.
6. NIDDM with ret.& mic. 7. NIDDM with dysl.& mic. 8. NIDDM with dysl.& ret & mic.
123
139
147
134
147
t3'7
t54
162
t0 t0
4
19
'7922
8315
93l0
85t4
86983
8
t8
7
9
9
15
9l24
93 * dyslipidemias, ** retinopathy, # microalbuminuriaTable
4.
Frequency distribution of NIDDM patients without anyaggravating factor and with one or more aggravating factors with blood pressure | 40/90 mmHg (adapted from Widiana,
r/g('2l
Blood pressure > 140/90 mmHg Groups
l. NIDDM without aggravâting factor (N=22)
2. NIDDM with dysl.*
3. NIDDM with ret.**
4. NIDDM wirh mic.***
5. NIDDM with dysl.& ret.
6. NIDDM with ret.& mic. 7. NIDDM with dysl.& mic.
b.N)DDM v'rrh ùys'l.E rel.&
mrc.
(N=)b)318
(N=6)
(N=a) (N=13)
(N=4)
(N=t2)
(N=18)
4
66;74
100.08
61.52
50.O6
50.0l'7
94.4)5
9f .E [image:4.595.41.274.116.288.2] [image:4.595.299.537.307.712.2]Table
5.
Lipid profile of NIDDM patients with and withoutmicro-albuminuria (adapted from Widiana et al, 1994)22
p
0.05)
>
andtwo
months aftertreatment
(84 vs 83mmHg,
0.05) were found. More interestingly,
creatinine
levels
tend
to
decreasein
captopril group
(1.7
to
1.3mg/dl,
p> 0.05) but
tendto
increasein
pl_acebogroup
(1.7
to
1.9mg/dl,
p> 0.05)
(seetable
6)r)
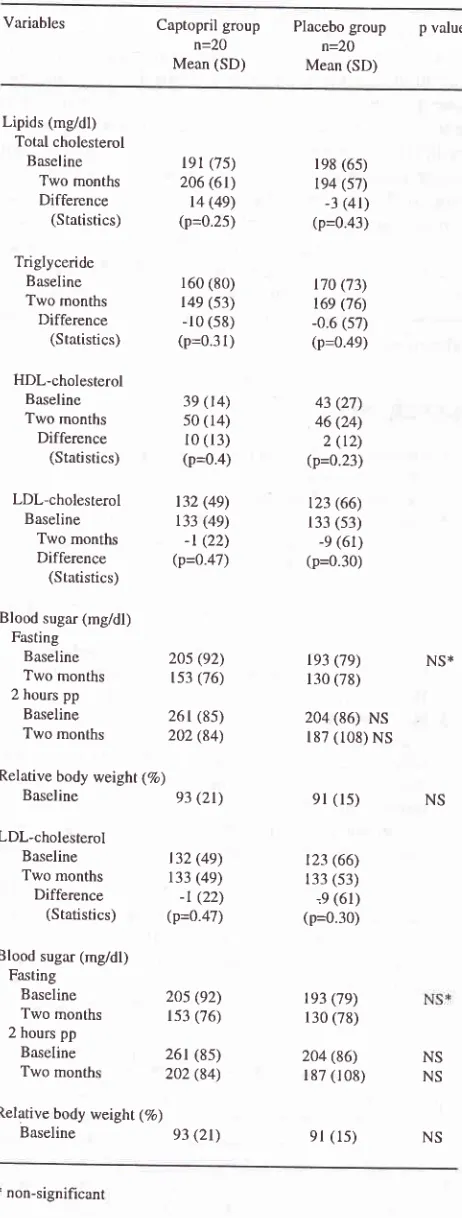
In
another studyin
Yogyakarta, Asdie
et al.found that
captopril improves
lipid profile
in
NIDDM
patients
with
albuminuria
by
increasing
HDl-cholesterol. In
randomized-placebo
controlled trial,
40patients
wereincluded
in
the study and divided
in
two
group
to
receive
captopril
12.5mg thrice
aday
or
placebo
for
two
months.
After two
months treatment, there was
asignificant
increased
of
HDl-cholesterol
(39
to
50mg/dl,
p< 0.05)
in captopril
group, but not
in
placebogroup
(43 to 46mg/dl,
p> 0.05).
Thereis
some degreeof
decreased
of
total-
cholesterolÆ{Dl-cholesterol
ratio
in bothcaptopril
and placebo group, 4.8 to 4.0 and4.6to
4.2, or decreasedby
l6Vo andSVo,consecutively.
This
changes may not related toblood
sugarcontrol or
body weight,
since there was nosignificant
changesof
blood
sugarlevels between baseline and
two
months after treatment in both groups andsimilar relative body
weight
atbaseline
in both
groups
were found.
How-ever, there
was
no
significant
changes
of
total
cholesterol,
triglyceride,
andLDL-
cholesterol levels
in
both
grouprlsee
table
7).16Table
6.
Urinary albumin excretion rate (UAER), blood pressure, andcreatinine levels in NIDDM patients before and after treat-ment in captopril and placebo groups (adapted from Sja'bani
et al., 1994)r5
Variables Captopril
group
Placebogroup
p valuen=20
n=2OMean
(SD)
Mean (SD) Lipids (mg/dl) withNIDDM
mic.x
without NIDDMmic.
P valueMean SD Mean
SDl. Total cholesterol
2. HDl-cholesterol
3. LDl-cholesterol
4. Triglyceride
5. Total-cholesterol: HDL-cholesterol
2N
5335
13ll2
59173
89l'tç 53
0.0643 t2
0.01I
13 42
0.24164 69
0.314.t l.l
0.00* microalbuminuria
INTERVENTIONAL
STUDIES
There
were
some reports
of
interventional
studiesin
microalbuminuric diabetics
in
Indonesia.
In
Yogyakarta,
Sja'bani
et alreported
a studyto
evaluate theeffect
of captopril
onurinary
albumin excretion
in
NIDDM with
albuminuria.
The study showed thatafter
two
months,
captopril
12,5mg
thrice
aday
decreasesalbuminuria without significantly
reducing the blood
pressurein
NIDDM
patients.
Patientsincluded
in
thestudy had diabetic
nephropathy.
Most (36 out
of
40patients)
of
the patients were
in
the
stageof incipient
diabetic nephropathy.
Patients
were given captopril
12.5
thrice
a day or placebofor
two
monthsby random
allocation.
During
thestudy 42patients
wereincluded,
2
in
placebo group dropped-out in
thefirst
month. Out
of
40
patients analyzed (21 males; 19 females)
20patients received
captopril
(age
53.60
years) and
20patients received placebo (age 50.80 years).
Therewere
no significant
difference
of urinary
albumin
ex-cretion rate
(UAER) in both
groups at baseline(195.0
vs 346.1 mg per 24 hours,p=0.133),
and nosignificant
difference
of
sex,
age,
duration
of
diabetes, systolic
and
diastolic blood
pressure,
blood
sugar,
serumcreatinine levels,
and
the
presence
of
retinopathy
in
both groups.
After
onemonth treatment, therervas no
significant
decreased
of
UAER
between
the
two
groups
(21.6
vs
10.9mgl24 hr, p > 0.05). After two
months treatment,
there was asignificant
decreasedof
UAER in captopril group (195.0 to
78.3
mgl24hr,p
< 0.05) but notin
placebogroup
(346.1to290.l
mgl24
hr,
p> 0.05).
Although
there was aroundtwice
reduc-tion
(149
to
141 mmHg
vs
145
to
l4l mmHg) in
systolic
BP
and around
1.5times
reduction (90 to
84mmHg
vs 87
to
83 mmHg)
in
diastolic BP, no
sig-nificant
difference of systolic
BP before treatment ( 149vs
145mmHg, p > 0.05)
andtwo
months after
treat-ment (141vs
141mmHg,
p > 0.05) ofboth
groups, anddiastolic BP before
treatment
(90 vs 87 mmHg, p
>
* p of difference = 0.367, *x p of difference = 0,472,
*** p of difference = 0.012,
****
p of difference = 0.35530 63
UAER
Before treatment
One month difference Two months difference Blood pressure
Systolic
Before treatment Two months Diastolic
Before treatment Two months Creatinine levels
Before treatment Two months
difference
195.0 (209.3)
173.4
(l9l.s)
2t.6 (64.4)* 78.3 (79.7)
I 16.7 150.6;xxx
t4e (17)
l4l
(19)e0 (e)
84 (8) t.7 (t.7)
1.3 (0.9) -0.16 (1.4)
346.1
(561.2)
0.133 335.2 (4Ot.4)
0.21510.9 (154.3)**
290.1
(370.0)
0.032 55.9 (150.3)*x*xt4s (24)
t4t (26)
87 (e) 83 (e)
t.]
(1.4)l .e (1.7) 0.2 (0.9)
0.277 0.045
0.211 o.428
[image:5.595.49.284.112.272.2]Variables
Captopril group n=20 Mean (SD)Table
7.
Lipid profilein
NIDDM with persistent albuminuria incaptopril and placebo group before and after two months treatment (adapted from Asdie et al., 1994)16
DISCUSSION
Some studies
regarding
microalbuminuria in NIDDM
have been
carried
outin Indonesia.
Most of
the studies werehospital-
based. Prevalenceof microalbuminuria
in
hospital setting varies 26
to
5JVo.A
community-based study
found
a prevalence r ateof
39Voin
NIDDM
patients
and 24.7Voin
IGT
patients.
Interestingly,
it
was revealed
in
the study byRoesli
that theIGT group,
which is
alsoknown
as aprediabetic
stateof NIDDM,
has ahigh prevalence
of
persistent
microalbuminuria.
At
least oneimportant question
can be raised based onthis
result.
Is
microalbuminuria
a
feature
of
theprediabetic
statein
NIDDM?ll Ho*"u"r,
Viberti
ar-guedthat
in
prediabetic
state, somefactors related
tomicroalbuminuria should be taken
into
account.
Studies have shown
that
essential hypertension,
obesity,
insulin
resistence, andcardiovascular
disease areprevalent
in
subjectsknown to
haveX-syndrome.
Some studies also
found
that essential hypertension,
obesity, hypertension, coronary heart
disease
werefound
with
increasedfrequency
in
patients
with
raisedalbumin excretion
(Viberti
1996,
oral
communica-tion).
In
the
study
by
Roesli,
it
was also
found
that
glycaemic control was significantly different
amongNIDDM
subjectswith
andwithout microalbuminuria,
IGT
subjectswith
andwithout microalbuminuria, with
p=0.001 both
for fasting
and2
hours post-load blood
sugar levels (data is not revealed;.1 I
ntàoA
sugarlevels
in
microalbuminuric were higher than
normoal-buminuric
subjectsboth
in
NIDDM
andIGT
subjects.It
should
be
elucidated whether
the
presence
of
microalbuminuria related
to
the difference
in
blood
sugar
control
or
the gradation
of
insulin
resistancerelated to the
stageof
the
disease.Since, many study
showed
the relationship between microalbuminuria
and
glycaemic levels, which
notonly found in diabetic
patients, but
alsofound
in
patient
with IGT.l7
NIDDM
patients
with microalbuminuria
areolder
andhaving
diabetes
longer than those without
microal-buminuria,
idiana
et alli."
Those
normal
meweight
and
ex,
and
alset al., reported that
retinopathy
wasalmost
three timesmore frequent
in
NIDDM
patients
with
microal-buminuria
than
those
without
microalbuminuria.l2
Blood
pressureis higher both systolic
anddiastolic in
NIDDM
patients
with
microalbuminuria than
thosePlacebo group
n=2O
Mean (SD)
p value
Lipids (mgidl) Total cholesterol
Baseline
Two months
Difference
(Statistics)
Triglyceride
Baseline
Two months
Difference (Statistics)
HDL-cholesterol
Baseline
Two months
Difference
(Statistics)
lel
(75) 206 (6t) t4 (49)(p=0.25)
160 (80)
149 (s3)
-10 (s8)
(p=0.31)
39 (14)
50 (14)
r0 (13)
(p=0.4)
198 (65)
t94 (s7) -3 (4t)
(p=0.43)
t70 (73)
169 (76)
-0.6 (s7) (p=o.ae)
43 (27)
46 (24)
2 (t2) (p=0.23)
t23 (66)
133 (s3)
-e (61) (p=0.30)
LDl-cholesterol
l3Z (49)Baseline
t33 (49) Twomonths
-l
(22)Difference
(p=O.47)(Statistics)
Blood sugar (mg/dl)
Fasting Baseline
Two months
2 hours pp Baseline
Two months
Relative body weight (Zo)
Baseline
93(Zl\
LDL-cholesterol
Baseline
l3Z(49)Two
months
133 (49)Difference
-l
(22)(Statistics)
(p=0.47)Blood sugar (mg/dl)
Fasting Baseline
Two months
2 hours pp Baseline
Two months
Relative body weight (%)
Baseline
93el)
20s (e2)153 (76)
261 (85)
2O2 (84)
2O5 (92)
153 (76)
261 (8s)
202 (84)
t93 ('7e)
130 (78)
204 (86) NS
187 (108) NS
9l
(15)t23 (66)
133 (53) -e (61) (p=0.30)
t93 (79)
130 (78)
204 (86)
l 87 (l 08)
el
(ls)
NS*
NS
NS
NS
t non-significanl
[image:6.595.41.272.127.736.2]without.
Patientswith microalbuminuriawho
haddias-tolic
blood
pressure 95mmHg
or more were more thantwice
asmany
than thosewithout microalbuminuria.l3
In
community-based study
by Roesli, blood
pressurewas
within normal
range andalthough
slightly
higher
in
NIDDM
patients
with
microalbuminuria
but nosig-nificant difference
wasfound.ll It
was
alsogeneraliy
found that, the more aggravating factors analyzed
(dys-lipidemia,
retinopathy, and microalbuminuria)
thehigher
blood
pressureboth systolic
anddiastolic,
andalso
the more frequent those
who
havehypertension.
Most
of
patients
with
aggravating
factors
had
meanblood
pressureof
140/85
mmHg
andmore
than 50Voof
them had
hieh
blood
pressure,
i.e.
)
i40l90
mmHg.l3
In
hospital-based study, there
wasno significant
dif-ferences
in lipid profile
betweenNIDDM
patientswith
microalbuminuria than those
without
microal-buminuria.
The mean values levels oftotal cholesterol,
LDl-cholesterol,
HDl-cholesterol, and triglyceride
were about the
samein
thosegroup. However,
it
wasfound that
NIDDM
patients
with
microalbuminuria
had
significant
lower
HDl-cholesterol
andsignificant
higher
in total-cholesterol/HDl-cholesterol ratio with
mean value
of
more than
4.5
than those without
microalbuminuria.l4
In
arandomized placebo-controlled
trial, captopril
isbeneficial
in
reducing
urinary
albu_minexcretion in
NIDDM
patientswith albuminuria.r)
Thereduction
of
albumin excretion
seemedto
be
causedby
captopril,
independent
of
its blood
pressurelowering
effect.
A1-though
blood
pressure wasslightly
reducedbefore
and after treatment,however,
nosignificant difference
wasfound. Captopril also
seem
beneficial
in
improving
lipid
profile
in
NIDDM
patients
with
microal-buminuria.
It
increases
HDl-cholesterol
levels,
without significantly
changesblood
sugarlevels
andmay therefore blood
sugarindependent.l6
Interestingly,
acommunity-based study reported
thattubular
enzymes levels, namely
NAG
(N-acetyl-p-D-glucosaminidase)
and
IAP
(intestinal alkaline
phos-phatase)
were
higher
in
NIDDM
patients with
microalbuminuria than those
without
microal-buminuria.
The
author proposed speculations
to
ex-plain
thesefindings.
First,
microalbuminuria
wasnot
only
due
to
the
increase
in
glomerular
passageof
albumin but also due
to
the
decreasein
the
protein
resorbtion capacity
of
the
tubules.
The early
tubular
changes
in
these
patients were identified by the
in-creased
urinary
IAP
and
NAG
levels.
Second,
thepresence
of
microalbuminuria
and
high level
of
IAP
and
NAG
arecoincidental. They
wereboth
detectedin
:iH:ï::Ë:ii"Ë1ff
earrv gromerurar
andtuburar
In
summary,
twenty six
to
fifty
seven percent
of
NIDDM
patients
in
hospital settings have
microal-buminuria.
More
than
athird of
NIDDM
patients
andone
quarter
of IGT
subjects havemicroalbuminuria in
community-based study. Generally,
NIDDM
patients
with
microalbuminuria
havehigher blood
pressure andmore retinopathy, inconsistent worse
lipid
profile,
higher
NAG-
and
lAP-level,
and are
non-obese.
Cohort-studies
andmorphological
studies
are neededto
confirm whether
NAG
and
IAP
can
be used
asmarkers of early
tubular
changes inNIDDM. A
longer-term
randomized
clinical trials with more
subjects
is needed toconfirm
thebeneficial effect
of captopril
onalbuminuria
andlipid profile in
NIDDM
patients.REFERENCES
l.
Krolewski AS, Wanam JH, Chrislieb AR, Busick EJ, Kahn CR. Changing natural historyof
nephropathyin
type
I diabetes. Am J Med 1985;18:785-94.2. Borch-Johnsen K, Andersen PK, Deckert T. The effect
of
proteinuria on relative mortality in type 1 (insulin-dependent diabetes mellitus). Diabetologia 1985;28:590-6.
3. Schmitz A. Nephropathy in non-insulin dependent diabetes mellitus and perspective for intervention. Diab Nutr Metab 1995;7:135-48.
4. Mogensen CE. Prediction of clinical diabetic nephropathy in IDDM patients. Alternatives to mi croalbumi nuria? Di abetes
1990;39:761-'7'7.
5. Mogensen CE. Natural history and potential prevention
of
diabetic nephropathy in insulin-dependent and non-insulin dependent diabetic patients. In : E1 Nahas AM, Mallick NP, Anderson S, editors. Prevention ofprogressive renal failure. Oxford: Oxford University Press; 1993; p 259-302. 6. Mogensen
CE,
ChristiensenCK.
Predicting
diabeticnephropathy in insulin-dependent diabetes mellitus patients. N Engl J Med 1984;31 l:89-93.
7. Mathiesen
ER,
OxenbollB,
JohansenK,
Svendsen PA, Deckere T. Incipient nephropathy in type 1 insulin-depend-ent diabetes. Diabetologia 1984;24:204-10.8. Viberti GC, Jarret RJ, Mahmud U,
Hill
RD, ArgyropoulosA,
KeenH.
Microalbuminuria as a predictorof
clinical nephropathy in insulin-dependent diabetes mellitus. Lancet 1982:1430-2.9. Mogensen CE. Microalbuminuria as a predictor of clinical diabetic nephropathy. Kidney Int 1987;31 :673-89. 10.
Gall MA.
Prevalenceof
micro
and macroalbuminuria,arterial hypertension, retinopathy and large vessel disease in european type 2 (non-insulin dependent) diabetes patients. Diabetologi a 199 1 ;34:65 5 -61.
diabetes and impaired glucose tolerance in the rural area of West Java. Highlighting the specific markers on the early
renal involvement [dissertation]. Antwerpen (Belgium):
Univ. of Antwerpen; 1996.
12. Widiana IGR, Sja'bani
M,
AsdieAH.
Blood pressure in non-insulin dependent diabetes mellitus patientswith
in-cipent diabetic nephropathy.
Acta Medica
Indonesiana1993 ;21 :52-9 (in Indonesian).
13. Widiana IGR. Blood pressure in
NIDDM
(non-insulinde-pendent diabetes mellitus)
with
some aggravating factors. Medika 1996;l l:855-9 (in Indonesian).14. Widiana
IGR,
Sja'baniM,
AsdieAH. Lipid
prohle inNIDDM
(non- insulin dependent diabetes mellitus) withmicroalbuminuria. Joumal
of Medical
Sciences 1994;26:21-7 (inlndonesian).
15. Sja'bani M, Widiana IGR, Asdie AH. Effecr of captopril on
albuminuria
in
diabetics.Medika
1994;20:41-8(in
In-donesian).
16. Asdie AH, Widiana IGR, Wiyono p. Effect of captopril on
lipid profile in non-insulin dependent diabetes mellitus with
albuminuria.
IndonesianClin Epidemio
Biostatistics199 4;1 :17 -22 (in Indonesian).