THE PALEOLITHIC CURRICULUM:
FIGURE IT OUT
( WITH THE HELP OF EX PERTS)
Martin Schreiber and Mitchell L. Halperin
Depa rtm ent of Medicine, Rena l Divisions, Mt. Sina i a nd St. Micha el’s Hospita ls, University of Toronto, Toronto, Onta rio, Ca na da M5B 1A6
T
he virtual explosion in the amount of biomedical information, the switch away from a lecture-based style of teaching, and the perception that more of the student’s time should be directed to patient-oriented activities have created an intense competition for time in the undergraduate medical curriculum. Our objectives are to impart an enthusiasm for learning together with an improved capacity to understand concepts and the ability to solve problems in clinical medicine. We rely heavily on the deductive capacities of the student. We shall emphasize horizontal (basic) and vertical (clinical) integration of disciplines that relate energy metabolism with fluid, electrolyte, and acid-base balances. The setting in which we begin to define a problem is in ‘‘Paleolithic times’’ because this is when metabolic control systems evolved and were most likely to be retained. Students are asked to deduce the best possible solutions for that problem, to ask for data to test their hypotheses, and to consider the ramifications of that solution in integrative terms. Subject matter is presented by informed leaders in either a small or large group format initially to set the stage. An interactive computer program was written as a supplement to demonstrate how we would utilize the information and concepts to design an element for teaching. The implications are that controls that were designed for primitive needs may lead to disorders in modern times because the current stimuli and needs are different. The power of the student’s growing ability to solve problems should be reinforced by demonstrating the degree to which the properties deduced by the student to solve a particular problem are actually consistent with data from the literature.AM. J. PHYSIOL. 275 (ADV. PHYSIOL. EDUC. 20): S185–S194, 1998.
BACKGROUND
We propose a novel way to teach clinically relevant physiology to medical students. Our approach was developed in the context of the explosion in the amount of biomedical information, which has led to an increasingly crowded curriculum for medical stu-dents, with keen competition for curricular time among basic and clinical science departments (9). In light of this, four major curricular changes were proposed to try to educate future physicians more
rationally: student-centered learning, an explicit at-tempt to make the curriculum relevant to students’ needs, problem-based learning (PBL) (2), and inte-grated learning (6, 7). Each of these is considered below, followed by our critique to set the stage for a description of our approach.
Student-Center ed Lear ning
Making Curriculum Relevant
A second related response is the notion of relevance (6). Even when students are not themselves selecting the material for study, a major goal of many modern curricula is to capture their interest by showing how material, at whatever level of learning, will ultimately be relevant to them in clinical practice.
Pr oblem-Based Lear ning
This strategy relies on small group teaching sessions led by a tutor (who is usually a ‘‘nonexpert facilita-tor’’). Students are given a clinical case as a starting point to generate their own learning agenda in a particular content area. They set objectives, disperse to do independent study, and then rejoin the group to share what they have discovered with their peers.
Integrated Lear ning
In this response, there are greater attempts to provide an integrated approach to the undergraduate curricu-lum (7, 8). The term ‘‘integration’’ is generally taken to mean that the relationships among individual disci-plines are made explicit and emphasized. This should then allow one to more clearly understand both normal biology and disease states.
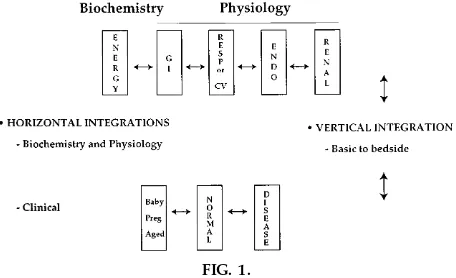
Integration can be both horizontal and vertical. Figure 1 provides a schematic view of how such integrations can be conceptualized in our subject area. Horizontal integration can occur at the level of the basic sciences; a specific example would be the description of the control of blood glucose levels in terms of both
molecular mechanisms or biochemistry (e.g., ‘‘How do glucose transporters work?’’) and physiology (‘‘What are the effects of insulin on blood glucose metabolism?’’). Horizontal integration can also occur at the level of clinical subjects; for example, ‘‘What is the impact of a chronically elevated blood glucose level (an endocrinologica lissue) on the function of peripheral nerves (a neurologica l consideration)?’’ Integration can also be ‘‘vertical,’’ meaning that the relationship of basic to clinical sciences is empha-sized. For instance, one might ask, ‘‘How does the presence of an elevated concentration of glucose in blood lead to the development of kidney disease in a patient with type II diabetes mellitus?’’
CRITIQUE
In general, we feel that these are well-intentioned innovations; however, certain changes in emphasis and execution may be required to better ensure that students are mastering clinically relevant basic science material in ways that will allow them to use this knowledge later at the bedside.
Student-Center ed Lear ning
This is a fine concept, but it must be managed carefully, with clear boundaries established. Students should pa rticipa te in defining what they will learn; this serves as an outstanding motivational tool. Not-withstanding, the teaching staff must not abdicate one of their key roles, which is to guide students toward the material that the teachers, by virtue of their experience, believe to be truly important.
Making Curriculum Relevant
Considerably more effort is needed in the area of making our curricula relevant to the students’ present and future interests and needs. In the course of curricular planning, the following questions must continually be asked: ‘‘How can I capture my stu-dents’ interest? Why do the students need to know this? How can I illustrate why understanding this concept will improve the ability of the student to make more accurate diagnoses and/or plan better options for treatment?’’
Pr oblem-Based Lear ning
There are notable strengths to PBL. A small group environment can foster student involvement in learn-FIG. 1.
ing, with a small student-to-tutor ratio. There may be greater student investment in learning than during a large group lecture, and there are opportunities for students to learn and practice skills of self-directed learning. We too, however, have a major concern about the use of nonexpert tutors (1). With nonex-perts, there is no good mechanism for ‘‘quality con-trol’’ with regard to what is being presented to the students by their peers during these sessions. The possibility that incorrect conceptualizations of criti-cally important areas may be perpetuated is of consid-erable concern. Furthermore, we believeexpertswith the ‘‘correct vision’’ are able to guide students toward far more efficient acquisition of concepts while still allowing the students a reasonable degree of indepen-dence and autonomy in the course of their learning.
Integrated Curriculum
We wholeheartedly endorse the notion of an inte-grated curriculum in both horizontal and vertical terms. Our major problem with the integrated curricu-lum is that, more often than not, it is not being realized. This may not be surprising; it is natural for a basic scientist or clinician with particular expertise in one discipline to wish to teach within that discipline and not cross into the ‘‘uncharted’’ territory of the broad field of integrative physiology and medicine. Nevertheless, this reticence must be overcome if our students are to become physiologically informed, competent clinical problem solvers. It may be that better strategies for achieving both horizontal and vertical integration are needed.
OUR APPROACH
We believe that the strategies for learning should change yet again. It is our feeling that the students of our ‘‘new’’ curriculum are performing less well than they might in applying the principles of physiology at the bedside. This is not the fault of the students, who are bright and highly motivated to learn when they arrive in medical school. It is our view that the faculty and/or the teaching methods do not provide enough motiva-tion and direcmotiva-tion to the learning process. For these reasons, we submit the following discussion.
Goals
In the paragraphs that follow, we describe one ex-ample of our approach. The problem at the outset is, ‘‘Where and how should we begin? Should we
pro-vide factual material as we did in the ’good old days’, or should we let the students decide what they think they ’need to know’?’’ We think the answer is emphati-callynoto both questions. Our fundamental goal is to facilitate our students’ learning of a set of physiologi-cal principles that will form the basis of an approach to solving problems in the areas of both physiology and clinical medicine.
Attract Inter est of Students
We try to capture the imagination and interest of the students by presenting the problem in such a way that it is1) intrinsically interesting to individual students, 2) clinically relevant, and/or 3) a good problem to solve. Once their interest is ‘‘captured,’’ students are guided toward the best solution. There are no limits set to the subject material, so the instructor(s) must be prepared to consider a wide breadth of subject material at an integrative physiology level (Fig. 1). Furthermore, instructors must be prepared to deal with the interest of a student in the clinical relevance of a problem, so the discussion may move to the clinical realm; however, the group leader must always remember the overall target and guide the discussion back to the original theme.
Technique
Our approach, in essence, is to have the students reach a consensus on what is the most important question—the more it is directed at survival needs, the better (this point will be considered in more detail in Specific Exa m ple). This should include input from a variety of fields of physiology (renal, endocrine, gastro-intestinal, respiratory, cardiovascular), biochemistry (energy metabolism, metabolic regulation), and clini-cal areas to emphasize the relevance of the problem (Fig. 1). Hence, each faculty member will be stressed initially to know even more about the subject matter and to be able to guide students to the best sources of information. Although the content area used to exem-plify our approach in the present paper is that of the physiology of water, we believe that the approach is broadly applicable to other content areas (seeAPPENDIX Afor an example).
Importance of Deductive Reasoning
first evolved (hence the term ‘‘Paleolithic’’ curricu-lum), they can figure out how the system is likely to operate in other settings. If such an emphasis on deduction can be developed and expanded through-out the course, students will be able to a nticipa te what is coming next; this should make a subsequent teaching and learning session more memorable. Fur-thermore, students can be challenged to employ a similar process of deduction by trying to predict the characteristics of disease states that result from either 1) a deficit or surplus of the ‘‘control element’’ or2) modern settings in which the stimuli differ from those which prevailed when the control system evolved. We believe, on the basis of our experience with students, that this deductive process will be recapitu-lated by the students when they are confronted by similar problems in the future, a model somewhat related to classic PBL (2).
Focus on Contr ol Mechanisms
We place great emphasis on the principles of control so that students can deduce what portion of a meta-bolic or renal system is the most important one. Among the principles to be stressed is that if one can recognize the function of a process, one can deduce its likely controls. Two examples are provided to help demonstrate this point (seeAPPENDIX B).
SPECIFIC EXAMPLE
General Considerations
Attract inter est of students.The first objective is to capture the interest of the students. Because we know that the topic is water and that our Paleolithic analysis may not be the best way to capture the students’ imaginations as a first step, we begin with a setting in which a disease state or recreation provides the entre´e.
Use of a clinica l exa m ple.The first strategy is to use a clinical situation as the focus; we might begin by showing a kidney stone and asking, ‘‘Do you know how much pain this caused? Why did the stone form? What could you do to prevent it from forming?’’ This will begin a series of vertical integrations between
metabo-lism (uric acid), endocrinology (calcium), renal physi-ology (urine volume and pH), and gastrointestinal physiology. There is also vertical integration, because one must be able to give sound advice to a patient that depends on basic science principles. In the stages of the example to follow, a student might relate the problem of living without food and water in Paleo-lithic times to diseases such as diabetes mellitus, obesity, or, in this particular case, kidney stones.
Use of sporting events.The second strategy is to use a recreational event as the focus; we might ask, ‘‘In ga m e 7, how long can a basketball superstar continue to perform at an elite level in that hot arena? Note how much he sweats. Is this dangerous? If so, why and how? What should the kidneys do? How will they know what to do?’’ In fact, his ideal responses were developed by humans in Paleolithic times while living in the hot Savannah when there was a limited supply of water, so we begin by trying to understand how this problem was solved in this setting.
No matter which style of entre´e is used, we move toward the control of the physiology of water balance. The leader could introduce the topic by asking, ‘‘Which is more important, a lack of food or a lack of water? What experimental data would you need to answer this question? What control mechanisms evolved in Paleolithic times when a lack of food and water was a common and critical event? How might the formation of a kidney stone be prevented at a time when there is little water in the urine? Any problems with your strategy?’’ A second introductory set of questions might be, ‘‘What effect might a surplus of food or water (in our modern era) have when their conserva tion was the rule of survival?’’ Other ques-tions such as, ‘‘How can one ensure that just enough water will be excreted to avoid development of a kidney stone when there is a deficit of water?’’ might redirect the discussion back to the theme. Finally, at the end of each lecture, one must return to the scenario that provided the entre´e and see how the concepts that were advanced help to solve that particular problem.
evolved in prehistoric times, imagine how your ances-tors existed back then. For example, a problem such as dealing with an inadequate amount of water was probably solved in many different ways by individual species that are currently flourishing today (3). We propose to examine the way this problem was ‘‘solved’’ by the human species. Our premise is that strategies developed then have been incorporated into our genetic database. Thus the control mechanisms de-signed at that time are the foundation of our current physiology. Derangements in any of these systems, or the presence of modern demands that differ from those in Paleolithic times, could lead to responses that were appropriate then but that lead to diseases now (see APPENDIX A for a different example to see the breadth of this approach).
For mat.A given problem in our ‘‘Paleolithic’’ curricu-lum can be addressed during a single week-long ‘‘unit.’’ Our suggestion is to have a large, nonstruc-tured group discussion at the beginning of the week in which a leader interacts with the students. This discussion can occur in the setting of a lecture hall, and the whole class should be present. In the first formal presentation to the students, the leader must be prepared to consider issues in a number of organ systems, integrate basic biochemistry and physiology, and then relate them to relevant clinical medicine. Material can be presented in advance to explain major concepts. Whereas written formats (textbooks, lec-ture notes) are one possible type of material, we prefer to supplement them with another approach, an interactive computer program was written for this purpose, one that is self-contained and requires no input from the faculty [an example can be down-loaded as shareware from the Internet (http:// www.interlog.com/,feabe)].
Once the students identify the issues that are critically important to their understanding of the basic control mechanisms, these could be expanded in a combina-tion of ways: further lectures, small group discussions, problem solving exercises, interactive computer ses-sions, and relevant textbook chapters or sections. In the course of these subsequent learning exercises, ample opportunity to interact with tutors is needed to
ensure that students are addressing relevant questions and, therefore, are on the right track.
Ex ample
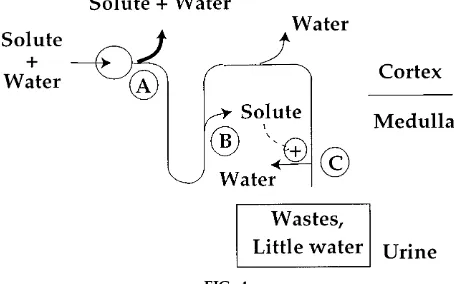
We propose to begin by identifying the most impor-tant issue in our setting of total deprivation of food and water. We could guide the students to obtain some facts to help formulate their ‘‘key question;’’ the facts are provided in Box 1 and Fig. 2.
BOX 1 Backgr ound
The following data can be provided to the student at the appropriate time in the introduc-tory lecture.
Need for water and food
Humans can survive 8 weeks without food, but they usually die from a total lack of water intake after close to 8 days.
Composition
The bulk (about 60%) of body weight is water. Chemical reactions occur in an aqueous solution. Many wastes are usually excreted in an aqueous solution (urine).
Appr oach
Think initially in mass balance terms (Fig. 2). Decide where the greatest leverage for controls should be, on input or output.
Think of the consequences of your imposed ‘‘solution’’ to the problem.
Anticipate the trade-offs by doing a risk/benefit analysis.
FIG. 2.
Stage 1: Develop an initial synopsis.The students, after a brief interaction, should be able to come up with the following synopsis of the problem.
Most im porta nt need.Because a deficit of water will kill long before a lack of food, the most important
‘‘strategy for survival’’ is to minimize the loss of water in this setting.
Stra tegy for surviva l.The only way a deficit can be replaced is with an input. Therefore, the most impor-tant way to repair a deficit of water is with water intake. Hence, the body must now sense that a deficit is present and then have ‘‘response elements’’ to react to the deficit (Figs. 3 and 4). In this case, the response is to first trigger the thirst mechanism (Box 2). Second, it will be important to curtail any excessive loss of water. The question remains, ‘‘How much of the daily loss of water is excessive?’’
BOX 2
Challenges concer ning a deficit of water
Basic
How would you design a cell to ‘‘sense’’ a deficit of water?
What are the response elements to deal with this deficit?
Clinical
What would the main problem(s) be if you know that a patient has a deficit of pure water? Which organs(s) are primarily affected? Why?
Assignment
Please describe at least 3 different clinical scenarios where a deficit of pure water could be present in a patient.
Stage 2: Decide how much water to lose. The student must also decide to minimize losses; loss of water occurs by sweat (heat dissipation), lungs (dry air enters and humid air exits), and the urine. The decision is made to focus on urine, because this is usually the largest site for water loss and one that can be regulated without compromising defense of a critical function (e.g., body temperature). The ques-tion becomes, ‘‘What volume of urine is best to excrete each day as the deficit of water increases progressively?’’ For the first part of the answer, we must ask, ‘‘Should the design be to eliminate the loss of water in the urine or permit the loss of some water in the urine, or is there no need to panic and we can keep the same volume of urine today as we had yesterday?’’
FIG. 3.
Detection system for a water deficit. Questions for stu-dents could be, ‘‘What does the ‘sensor’ detect and how does it do this?’’ ‘‘What ar e the r esponse elements?’’ ‘‘At the effector or gan level, what ar e the actions of the messenger on the kidney?’’ ‘‘On what portion of the nephr on does the messenger act?,’’ and ‘‘Should the r enal loss of water ever be zer o?’’ AVP, vasopr essin.
FIG. 4.
Responses.We expect the debate to revolve around the first two options suggested in the preceding paragraph. The group leader could ask two questions to direct the discussion to its most relevant issues.1) Will there be water-soluble wastes to excrete? Why must there be water-soluble wastes?2) If the volume of the urine is too low, what might happen to urinary constituents that are sparingly soluble in water (Box 3)?
BOX 3
Questions concer ning a urine volume that is very low
Basic
What are the metabolic wastes that must be excreted?
Are any of these wastes sparingly soluble in water?
Clinical
Who is most likely to develop a kidney stone?
Assignment
Describe the most fundamental issues related to the volume and composition of the urine when water must be conserved maximally (this point is developed in more detail in the com-puter program supplied with this lecture).
Clinica l exercise. The following idea can be intro-duced at the appropriate time. There are some compo-nents of the urine that are sparingly soluble. Some are inorganic and others are organic compounds. Know-ing what they are will help students decide who is likely to develop a kidney stone. Someone might be assigned to ‘‘research’’ this issue and report back to the group.
Stage 3: Events at the level of the kidney. The students should have decided that there must be a small, but not exceedingly tiny, volume of urine so that the risk of kidney stones is minimized. Now, the theme changes to the following question, ‘‘How can the kidneys be ’smart’ enough to excrete a small, but not too small, volume of urine?’’ Stated another way, the problem they must face is to design a system whereby this ‘‘ideal’’ minimum volume of urine is excreted. The students will be encouraged to obtain the facts described in Box 4 from the instructor to formulate their question or theme for a strategy for survival.
BOX 4
Backgr ound: A deficit of water
In response to a deficit of water, the sensor in Fig. 3 ‘‘sensed’’ it and sent a messenger to the kidney which ‘‘said’’ to the kidney, ‘‘Do not excrete water.’’
To help with their reading, the students should be told that the name of the messenger is either antidiuretic hormone (ADH), named because of its renal effect to curtail the excretion of pure water, or vasopressin (AVP), named because of its other biological action, which is to prevent a fall in blood pressure (ask ‘‘Why is this function needed?’’). Both names are retained in common use.
Assignm ent.The students are asked to describe a way to ensure that there is a ‘‘good’’ volume of urine despite ‘‘perfect’’ renal function and an abundant amount of antidiuretic hormone or vasopressin.
Hint. Please describe the volume of urine as a ‘‘ge-neric’’ mathematical equation (Eq. 1); there are three components to consider for this equation.
Volume5
Number of solutes/concentration of solutes (1)
Stage 4: Retur n to the lar ger pictur e.At a practical level, this portion of the session could be supple-mented with the interactive computer program men-tioned earlier and designed for this purpose; its use should decrease preparatory work by the faculty. The time allotted for this part of the course will depend on constraints within each curriculum.
BOX 5 Solutes in urine
Solutes in the urine are water soluble; they can be conveniently thought of in two categories:
Or ganic solutes
Because fat is not water soluble and sugar or its metabolic products do not normally appear in the urine, the only organic solute present in the urine in significant amounts is the nitrogenous waste product from protein oxidation (urea).
Electr olytes
The most abundant electrolytes in the urine are sodium (Na1) and chloride (Cl2); potassium
(K1) is also ex c reted in reasonably large
amounts. The quantities excreted reflect the amounts consumed. With no intake, none of these ions should be excreted in steady state.
Consequences of a deficit of
NaCl A loss of extracellular fluid (and plasma) volume
K1 Electrical instability at the cell
membrane
Assignment
What solutes can be spared to cause a urine volume when there is no intake?
Ana lysis of solutes. ‘‘What purpose do the solutes present in the urine have in the body?’’ The inorganic electrolytes are critical for survival (Box 5 for the instructor). Therefore, it is organic molecules that can potentially be spared as solutes in the urine, and the function of the urine is to ensure a minimum urine volume for any given osmolality, as determined from Eq. 1. In this area, the question is, ‘‘What is the most abundant and least essential class of organic com-pounds: protein, carbohydrate, or fat?’’ Having de-cided with some guidance that the answer is fat, the students would then explore how to make fat soluble in water (so that it can be excreted in the urine); the strategy is to create a smaller ionic version, or a ‘‘fat-derived ion.’’ The next question might be, ‘‘When an anion is produced due to partial oxidation of fat, what else must be produced as well?’’ This introduces the students to the principles of electroneutrality and of H1and the idea that H1must be eliminated by the
kidney. Suffice it to say for now that to excrete fat-derived ions, there is a need to excrete a cation in
the urine (NH41) that removes H1 from the body.
These and other aspects can be explored at a later time in sessions on acid-base balance, but the empha-sis on integration is reinforced at this point.
Stage 5: A mor e in-depth analysis of r enal physi-ology of water homeostasis. At this point, we demonstrate one more strategy to find a point to complete our discussion. The example we choose is to ask the students the following question: ‘‘What is needed within the kidneys to conserve water (pure water, not salt-water) maximally?’’ We can foresee them developing a ‘‘strategy for the nephron.’’ In point form, they should be able to deduce the follow-ing, especially if they have access to the supplement to this approach as supplied on the computer pro-gram mentioned earlier:
1) To excrete less water, should one filter less or reabsorb more of the filtered water (Fig. 5)?
2) To reabsorb pure water, should this occur at the beginning and/or the end of the nephron (Fig. 5)? What are the characteristics of the nephron segment in which pure water is reabsorbed?
FIG. 5.
3) If a greater conservation of water is desired, what properties would be given to a special area of the kidney? What must the net effect be? Where must it be located? What properties must its membranes have? What about its blood supply?
Bottom line.At the end of this session, the students should have constructed a kidney, as shown in Fig. 4, in which an upstream segment pumps solute into the compartment adjacent to the last part of the nephron. The former must be sparingly permeable to water and solutes, whereas the latter is permeable to water but not to solutes. The students are now ready for the lecture on renal water handling and an introduction to the concept of a countercurrent system as well as to disease states in which this physiology does not function properly.
Assignm ent. Other questions, both more basic and clinical, should be left for independent exploration such as:
1) Would a solute that is very permeable in the last portion of the kidney cause more water to be ex-creted?
2) A person ‘‘in the cave’’ who may soon be unable to get access to water because of a planned expedition drinks enough water so that there is now a small surplus. Should that surplus be excreted promptly? If not, what is needed to prevent its excretion?
3) What would be the consequences of too much or too little of the ‘‘water-saving’’ messenger (ADH) shown in Fig. 3 ?
Stage 6: Retur n to original scenario.If we return to the scenario of the elite athlete, we would emphasize the differences among body fluid compartments. We would show that the blood volume is very small, whereas the volume of water inside cells is very large. We would ask, ‘‘Where should the water lost in sweat come from? Why did the athlete need sweat anyway? What do sweat glands do—how do they work to ensure that we use water from inside cells for evapora-tion?’’ The disease cystic fibrosis impacts significantly on this process. Because this disease affects the composition of sweat, ‘‘What are the consequences for the patient with cystic fibrosis? Think of how we
detect a lack of water and what the response elements to it should be.’’ These and many other questions will introduce future lectures or small group sessions.
Stage 7: Student assessment.Assessment is a crucial element of curricular planning; it can be used both as a basis for feedback and also to motivate and guide students’ learning. We suggest that students be given a written (or computer based) scenario, related to, but not the same as, what they have considered during the unit. They should then be asked to indicate what they feel are the crucial issues to be resolved in the course of solving the problem, to determine what informa-tion they would need to know to solve it, and to propose tentative solutions.
CONCLUDING REMARKS
APPENDIX A
Ex ample of ‘‘Paleolithic’’ Appr oach
The blood coagulation system evolved to avoid excessive blood loss from a hemorrhage. In modern times, when the life span is longer, many disease processes are brought on by inappropriate coagula-tion (e.g., coronary artery occlusion, deep vein thrombosis). There-fore, therapies for these diseases are directed at preventing clotting and platelet aggregation.
APPENDIX B
Basics of Contr ol Mechanisms
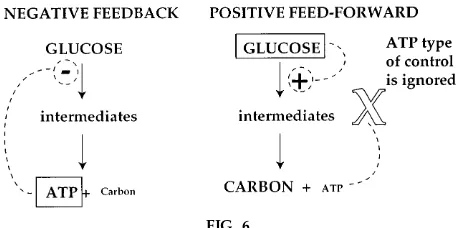
Two examples are presented to compare basic aspects of controls used in energy metabolism and in renal excretions.
Ener gy metabolism.The central function of energy metabolism is to supply an organ with enough fuel to oxidize to perform its work (Fig. 6). On the basis of the simplest example of the red blood cell (RBC), the RBC must take up just enough sugar (glucose), but not a large amount, to make useful energy (ATP) to maintain its shape and integrity. Therefore, controls will be present in the RBC to stop the oxidation of glucose when there is enough ATP (‘‘negative feed-back’’ control by ATP). Moreover, two points can be deduced. First, controls must be exerted at the beginning of a metabolic pathway so that metabolic intermediates do not ‘‘pile up’’ inside the RBC. Second, other organs that also metabolize glucose will have a different form of control because they may have another function. For example, after a meal rich in sugar has been eaten, one organ at least, the liver, must remove this surplus glucose from circulation. Because the function of the liver is to remove onlysurplusglucose, this form of control will be related to a high concentration of glucose in blood; while this concentration is still high, glucose will
be metabolized. As a corollary, when the concentration of glucose in blood falls toward normal, the rate of metabolism of glucose in the liver will decline (this can be described as ‘‘positive feed-forward’’ control related to the concentration of glucose). Just how glucose can be metabolized in the liver despite the presence of a negative feedback control system described for the RBC poses an exciting and challenging problem for the student to work out. This area is explored in more depth in a textbook dedicated to problem solving in this area (5).
Contr ols in the kidney. One can contrast these metabolic controls to those needed for the kidney to function normally (Figs. 5 and 6). The question posed for the students with respect to control of renal function is to identify what is required to ensure, for example, that the daily intake of 1 liter of water will be excreted each day. The options presented to the student are to exert control at the rate of filtration of water, its rate of reabsorption at early nephron sites, and/or its reabsorption at the latest nephron sites. Given the fact that so much water is filtered (180 liters per day) and reabsorbed in the first nephron segment (120 liters per day), the student can readily appreciate that control mechanisms here would be too imprecise to limit water excretion to 1 liter per day (Fig. 5). In fact, it is easy to deduce that the most important control of the excretion of pure water will occur in the terminal area of the nephron. Again, working out just how this can occur is a challeng-ing problem for the students to solve.
Address reprint requests to: M. L. Halperin, St. Michael’s Hospital Annex, Lab No. 1, Research Wing, 38 Shuter St., Toronto, Ontario, Canada M5B 1A6.
Refer ences
1. Albanese, M. A., and S. Mitchell. Problem-based learning: a review of literature on its outcomes and implementation issues.
Aca d. Med. 68: 52–81, 1993.
2. Barr ows, H. S., and R. M. Tamblyn.Problem -Ba sed Lea rning: An Approa ch to Medica l Educa tion. New York: Springer, 1980. 3. Dawkins, R.Clim bing Mount Im proba ble. New York: Norton,
1996, p. 90–91.
4. Halperin, M. L. Renal physiology detective stories. [Online] http://www.interlog.com/,feabe [1998, May 27]
5. Halperin, M. L., and F. S. Rolleston.Clinica l Detective Stories: A Problem -Ba sed Approa ch to Clinica l Ca ses in Energy a nd Acid-Ba se Meta bolism. London: Portland, 1993.
6. Har den, R. M., S. Sowden, and W. R. Dunn. Educational strategies in curriculum development: the SPICES model. Med. Educ. 18: 284–297, 1984.
7. Har den, R. M., and J. M. Laidlaw. Effective continuing education: the CRISIS criteria.Med. Educ. 26: 408–422, 1992. 8. Jobe, P. C., L. E. Adams-Curtis, T. F. Burks, R. W. Fuller, C. C.
Peck, R. R. Ruffolo, O. C. Snead III, and R. L. Woosley.The essential role of integrative biomedical sciences in protecting and contributing to the health and well-being of our nation.
Physiologist37: 79–86, 1994.
9. Muller, S.Physicians for the twenty-first century. Report of the Project Panel on the General Professional Education of the Physician.J. Med. Educ. 59: 1–208, 1984.
FIG. 6.