Vol9, No I, January - March2000 Clinical pattem of hospitalized strokes 29
Clinical
pattern
of hospitalized strokes
in
28
hospitals
in
Indonesia
J.Misbach, A.
Wendra
Abstrak
Stroke merupakan penyebab kecacatan dan kematian yang semakin meningkat di Indonesia. Pola kLinis stroke yang dirawat di rumah sakit belum banyak dilaporkan. PeneLitian ini merupakan salah satu bagian dari ASNA Stroke Epidemiological Study yang bertujuan untuk meneliti pola klinis stroke di 7 negara ASEAN termasuk Indonesia dengan protokoL yang sama. Dari 2065 penderita stroke akut yang dirawat di 28 rumah sakit di seluruh Indonesia, usia rata rata adaLah 58,8 + I3,3 (SD) tahun, (rentangan I8-95 tahun). Dua belas koma sembilan persen berusia dibawah 45 tahun, dan 3 5,8 Vo diatas 65 tahun. Pria lebih banyak dari wanita. Waktu tiba di rumah sakit rata rata 48,5 + 98,8 jam ( berkisar I -968 jam) setelah serangan stroke .Sebagian besar tiba di rumah sakit di atas 6 jam setelah serangan. Alasan keterLambatan ini antara lain kztidaktahuan (56,3 Vo) dan kesuLitan transportasi (21.5 Vo). Gejalayang paLing menonjol adalnh kelumpuhan dan gangguan bicara / bahasa. Faktor resiko tersering adalah hipertensi, penyakit jantung, merokok dan diabetes mellitus. Stroke berulang dijumpai pada sekitar 20 Vo kasus. Jenis stroke terbanyak adalah stroke iskemik. Sebagian besar keluar rumah sakit
dalam keadaan hidup dan membaik
Abstract
Stroke is the increasing cause of morbidity and mortality in Indonesia. Data on clinical pattern of hospitalized Indonesian stroke patients is still not available. This study is a part of ASEAN Neurological Association (ASNA) Stroke Epidemiological Study aimed to investigate clinical profile of stroke in 7 ASEAN countries with the same protocol. From 2065 acute stroke patients admitted to 28 hospitals all over Indonesia, mean age was 58.8 + 1 3.3 (SD ) year (range : l8-95 years). I 2.9 7o were younger than 45 years, and 3 5.8 7o were older than 65 years. There were tnore men than women. Mean admission lime was 48.5 + 98.8 hours (range: I -968 hours). Most of them arrived at hospital more than 6 hours from the onset of stroke. The reasons
for
deLayed admission were unawareness of stroke symptoms and Iong dislance transportation. The mostfrequent stroke symploms were motor disability. The most common riskfactors were hypertension, heart diseases, cigarette smoking and diabetes mellitus. Recurrent stroke was found in nearly 20 Vo patients. Ischemic stroke was the mostfrequent and the majority of the study subjects were discharged alive and improved .Keywords : Stroke , clinical pattern , hospital- based study
Stroke is
still
themajor cause
of
death anddisabilities
in
developed countries, although
recentepidemiologi-cal
datashowed a
decreasing tendencyof
strokemor-tality in
those
countri"r.l
Iidon"sia
as a developingcountries
with
thepopulation of
more than 200million
people
(thefourth
largestpopulation
of
theworld)
haslittle
documented
nation-wide data
of
stroke
epidemiology, either hospital
or
community-based
statistics.
A
limited
hospital-based
stroke
survey
revealed
the growing
tendency of^stroke
casesespe-cially
in urbanhospitals in
Jakarta.'The availability
of
accurate
stroke
data are
very important
for
national
stroke combating programs
all
over Indonesia. This
is thefirst
large scalehospital-based
stroke studyinvolv-ing
the urban
andrural
areasin
Indonesia.
This
studyDepartment of Neurology, Faculty of Medicine University
of
I n don e s i a/ D r. C ip to M an g unkus umo H o sp i tal, J akar t a, Indonesia
is
a partof ASNA
Stroke
Epidemiological
Study
per-formed
in
sevenASEAN
memberCountries by
ASNA
Standing Committee
For
Stroke,
from October
1996until March
1997.This article
presents
descriptively
the
demographic
characteristics,
clinical pattern,
risk
factors, type
of
stroke,arrival time,
lengthof hospital stay and hospital
discharge status of strqkepatient
in Indonesianpopula-tlon.
METHODS
Over
a6-month
period from October
1996to
March
l99J,we
prospectively
evaluated consecutive seriesof
acute strokepatients
admitted
to
28hospitals
all
over
lndonesia.
These
hospitals
represented
most
of
theareas
with
dense
population
in
Indonesia involving
Thir-30
Misbach and Wendrateen
hospitals located
in
Jakarta and 15hospitals
wereoutside Jakarta. The
participating
hospitals
consistedof
l4 University-affiliated
hospitals
and 14private or
semiprivate
hospitals
in
urban
areas.Diagnosis
of
stroke was madeclinically
by
participat-ing neurologists in
those
hospitals using the World
Health Organization criteria,
i.e. "rapid
developing
clinical
signsoffocal
or global disturbancesofcerebral
function
lasting
more than 24 hours or leading to deathwith no
apparent
causesother than that
of vascular
origin".
If CT
scanis
available
,it
should be done
for
confirmation.
All
the subjects
were
assesed by
participating
neurologists
and thefollowing
parameters were noted:demographic characteristics
(age, sex, and etc.),hospi-tal arrival time,
reasonsfor
delayed admission
(morethan
six
hours),
clinical
features,
risk
factors, type
of
stroke(by CT Scan), length of hospital
stay andhospi-tal
discharge
status.Clinical
data were storedin
a prepreparedfloppy
disk
and
descriptive
statisticswere applied using
Statistical
Program
For
Social Science
(SPSS)6.2for
Windows
95.
RESULTS
Demographic characteristics
During
theperiod of
the study, 2065 patientswith
acutestroke have been evaluated.
Mean
age was 58.8+
13.3years
(ranged
18-
95), higher
in
women (60.4
+
13.8years) than
in
men
(57.5
+
12.7years).
The
agedis-tribution
showed that12.9Voof
thestrokepatients
wereyounger than 45 years
old
and35.8Vo above 65 years.The sex
distribution
showed aslight
prevalence of men (53.8Vo vs 46.2Vo).(Table
1)Hospital admission time
The mean time between onset
of symptoms
andhospi-tal
arrival was 48.5 + 98.8 hours (ranged
I -
968hours).
Cumulatively,2l.l%o of
the patients were
ad-mitted
within 3
hours, 32.lVo
within 6
hours,
44.8Vowithin l2
hours
and 50.2Vowithin
24 hours from stroke onset.(Table
l)
The
reason
for
delayed admission
were
asfollows
:56.3Vo unawareness
of
having
a stroke, 2l .SVo
transportation problems,
ll.87o taking traditional
medicine,
4.2Vo
visiting traditional healer
and
6.2Vounknown (Table 2)
Table
l.
Characteristics of study subjectsMed.I Indones
No. of patients Mean age, y (SD)
<45
45-65
>65Sex,M/F
Mean Admission Time, h (SD)
<3
h3-6
h6-12
h 12-24
h>24
hMean Length of hospital stay, d (SD)
l-7
d7-21
d2t
-28
d>28
d2065 58.8 (13.3)
12.9Vo 5O.SVo
35.\Vo
tl08
I 944 48.s (98.8)2t.t%
I l.6Vo 12.lVo5.4Vo 49.8Vo
lo.9 (9.6) 42.8Vo
46.lVo
5.6Vo
Table 2. Reasons for delayed admission
No. of delayed patients Unawareness of having a stroke Transportation problem Taking traditional medicine Vi siting traditional healer Unknown
I 385
56.3Vo 2l.5Vo ll.8Vo 4.2% 6.2Vo
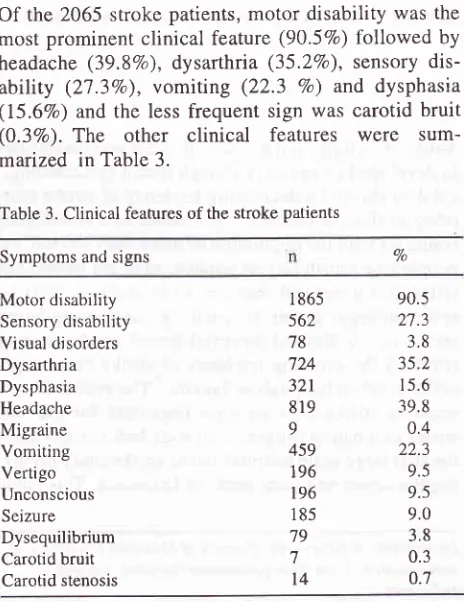
Signs
and Symptoms
Of
the 2065 stroke patients,
motor disability
was the
most
prominent clinical
feature
(90.5Vo)followed
by
headache (39.8Vo),
dysarthria
(35.2Vo), sensory
dis-ability (27.3Vo),
vomiting (22.3
Vo)
and
dysphasia(15.67o)
andthe
less
frequent sign
was
carotid bruit
(0.3Vo).
The other clinical
features
were
sum-maized in
Table
3.Table 3. Clinical features of the stroke patients
Symptoms and signs Vo
Motor disability Sensory disability Visual disorders Dysarthria Dysphasia Headache Migraine Vomiting Vertigo Unconscious Seizure Dysequilibrium Carotid bruit Carotid stenosis
I 865 562 78 724 321 819
9 459 196 196 185 '19 7
t4
90.5
2'1.3
3.8 35.2 15.6
[image:2.595.228.560.82.428.2] [image:2.595.345.577.432.733.2]Vol9, No
I,
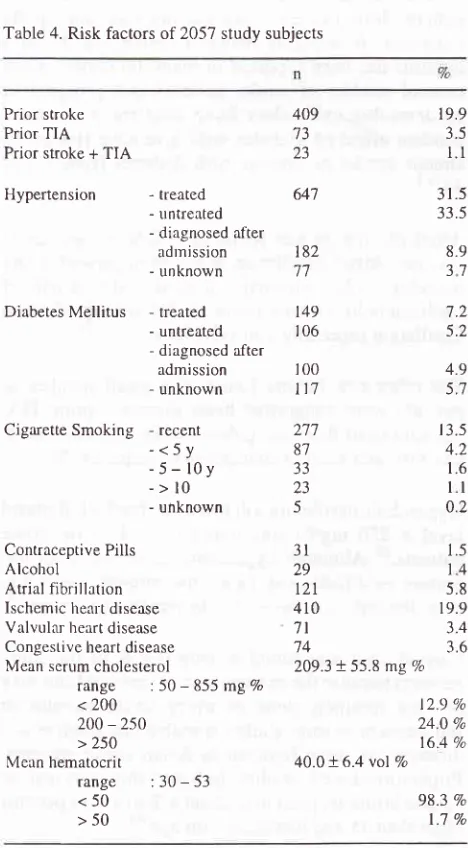
January - March 2000Risk Factors
The most common
risk
factors
for
stroke
in
our
studywere hypertension
(73.9Vo). Thirty one point fiveper-cent
of
the hypertensive stroke patients were
treated,33.5Vo
untreated
and 8.9Vo diagnosedafter
admission.Smoking was the
second
most frequent
risk
factor
(20.47o)
and 13.5Voof
them
were recent smokers. Theother major
risk
factors were
prior
stroke, ischemic
heart di sease and diabetes mellitus (19 .9Vo, 19.9Vo and
lJ.3Vo, respectively).
Sevenpoint two
percent
of
thediabetic
stroke patients
were
treated,
5.2Vo untreatedand 4.97o diagnosed
after admission.
The mean serumcholesterol
level
was 209.3
+
55.8 mgVo(range 50
-855)
and 31.27o below 200 mgVo,26.0Voin the range
of
200
-
250
mgVo andonly
l6.4Va
above 250 mgVo.Mean
hematocrit value
was 40.0 + 6.4 vol Vo(range30
-
53) and l.7Va of the
subjects
had the
hematocrit
above 50 vol%o.
(Table
4)Table 4. Risk factors oT 205'l study subjects
Prior stroke Prior TIA Prior stroke + TIA
Hypertension
Clinical pattem of hospitalized
strokes
3I
Classifrcation
of
stroke
CT
scan was done on6l.9Vo
of the
study patients
andthe
mean
time from
onset
to CT
was
2.9
+
3.9
day(median
1.0 and
range
I -
48 day). The
diagnostic
classification based on CT finding,
were non lacunar
anterior circulation
(27.}Vo),
lacunar l7.JVo,
in-tracerebral hemorrhage
(185%),
non lacunarposterior
circulation 4.27o, slbarachnoid hemorrhage
(l.4Vo)
and 38.17o
undetermined
(without
CT).
Hospital discharge
status
Table
5
shows
that
56.9Voof our
study patients
\ilerealive-with
improved
condition whereas
4.3Vopattents
had a
worsening condition.
The
overall
mortality
of
the strokepatients
was 23 .3Vo.The death rate was higher
in hemorrhagic (28.4Vo)than
in ischemic stroke
(21.2Vo).
The patient
with
nonlacunar
anterior circulation
showed
higher mortality
(l5.2Vo) than
patients
with
posterior
circulation
[image:3.595.81.315.310.734.2](2.5Vo),
while the
lacunar
infarction
patients
showed avery
low death rate
(3.5Vo).Table 5. Type
of
stroke and hospital discharge status ofthe study subjects
Total subjects
No. of patients with CT Scan - abnormal - normal
Type of stroke
2057
1274
(61.9%)ll}2
(53.6Vo)172
(
8.3Va) 409't3
23
- treâted - untreated - diagnosed after
adrnission - unknown
Diabetes
Mellitus
- treated - untreated - diagnosed afteradmission - unknown
Cigarette Smoking - recent
-<5y
-5-l0y
->10
- unknown
Contraceptive Pills Alcohol
Arrial fibrillarion Ischemic healt disease Valvulal heart disease Congestive heart disease Mean scrum cholesterol
range
: 50-
855 mg 7, < 200200
-250
> 250 Mern hematocritrange
:30-53
<50 >50 64'7 19.9 3.5l.l
31.5 33.5 8.9 37 7.2 5.2 4.9 5.7t 3.5 4.2 1.6
ll
0.2 1.5 14 5.8 19.9 3.4 3.6 182 1a t49 106 100l\7
277 87 33 23 53l
29t2l
410 7l 74209.3 + 55.8 mg Vo
- lacunar
- non lacunar anterior circulation - non lacunar posterior circulation - subarachnoid hemorrhage - lobar hemorrhage - ganglionic hemorrhage - brainstem hemonhage - cerebellum hemorrhage - unknown (without CT)
Hospi tal discharge status - alive - improved - alive - unchanged - alive - worsened - âlive status not recorded - dead
- unknown
ll.7%
27.ÙVo 4.2Vo l.4Vo 8.8Vo 7.lVo l.7Vo 0.9Vo 38.1Vo 56.9Vo l.6Vo 4.3Vo 5.|Vo 23.3Vo 9.7Vo t2.9 %24.0 Va 16 4 o/o
40.0 + 6.4 vol Vo
98.3 Vo
1.7 Vo
Length of hospital
stay
Overall
meanlength
of
hospital
stay
was 10.9
t
9.6 [image:3.595.343.575.408.676.2]32
Misbach and Wendralength of hospital
staywas
I 1 daysfor
ischemic
strokeand
17 daysfor
hemorrhagic
stroke.DISCUSSION
Most
of
the hospitalized stroke patients
in this
studywere
in
the
agegroup
of
45-65
years
with
the slight
prevalence
of
men. Stroke
in
theyoung
adults
andin
the
old
agepeople comprised
of 12.9
Vo and35.8
7orespectively.
This
findin.qs were not
sodifferent from
the western
literatures3-6ir
someAsian
count.ies.T'8The majority
of
stroke patients arrived at
hospitalsmore than
six
hours
after
stroke onset
andonly
one-fifth
of
thepatients arrived
within
less thansix
hours.The
reasonsfor
delayed admission were
unawarenessof
having
a stroke
andtransportation problems. This
fact
showedthat most
of
our people
werenot
familiar
with
strokesymtoms
and unawareof
the emergencyof
this brain
attack. Some
foreign
investigations
on
thearrival
time
of
stroke
also showed the sameproblems.
It
was concluded that community
education
for
theearly
sign
of
stroke and ambulance service
for quick
hospitalisation
have thekey role in
saving the patients.Anticipation
of
thethrombolysis
andneuroprotective
therapy
for
stroke
will
give
best results
if
it
is
donewithin
3 hoursfrom stroie
onset.T-l-lClinical Features
Clinical
features
of our
stroke patients
showedmotor
disability
as aprominent clinical
feature
followed
by
headache,
dysarthria,
sensory disorders and dysphasiarespectively. This
findings showed
theimportance
of
physical
rehabilitation
and
speech
therapy
for
In-donesian
which
must be doneintensively
and asearly
aspossible
in
accordancewith
theclinical stability, in
order to improve
the
quality
of
life and
to avoid
thesevere
disability
as a sequelaeof
stroke
. Headache isa common symptom
in
stroke
and
it was
found in
nearly
40 Vo of the stroke patientsin this
study.Vester-gaard
K
revealed that
headacheoccurred
in
50
Voof
patients
with
intracerebral hemorhage,
in
26
Vowith
infarction,
and
in
15
Vo ofpatients
with
lacunar
stroke.15
Further
study
is
reqriired
to
investigate
headache
characteristics in Indonesian
stroke patients,Risk
factors
Hypertension was
the
most prominent
risk
factor
(73.9Vo)
and almost
half
of
the
hypertensive
strokepatients were not treated.
Hypertension
as a strongrisk
factor
for
stroke was undebatable.
Many
studies
Med J Indones
showed the
consistent
closerelationship between
thehypertension
and theoccurrence
of
stroÊe.15-19Smoking
is
the
second
most frequent
risk
factor in
Indonesian
strokepatients
and several studies showedthat cigarette
smoking is closely
associatedwith
theoccurrence
of
cerebrovar.ulu,
âiseases2Oand
it
hasbeen
considered to
be anindependent
modifiable risk
factor.2l
Ischemic
heart
diseasewas
found
in
19.9
7oof
thestudy
subjects.In
Framingham Study
, ifmultivariate
analysis was used ,
risk
of stroke was increasedtwofold
in
the
presenceof
coronary heart
disease
and
three-fold
with
electrocardiographic
left ventricular
hyper-trophy.
So,prevention
of
theserisk
factors
representsa cornerstone
of
cardioembolic stroke
prevention.'-Diabetes
mellitus
was
found
in ll
.3Voof
our
strokepatients.
Most of
thediabetic patients
wereunproperly
controled. Association between stroke and
diabetesmellitus
hasbeen reported
in
many literatures.
Casecontrol
studies
of
stroke patients and
prospective
epidemiological
sudies have
confirmed an
inde-pendent
effect
of
diabetes
with
a relative
risk
of
is-chemic
stroke
in
nersons
with
diabetes
from
1.8
to3.0.2s
Atrial fibrillation
was
found
in
5.8
Voof
our
strokepatients.
Atrial fibrillation
is the most powerful
andtreatable
cardiac
precursor
of
stroke, almost half
of
cardioembolic
strokes
occur
in
the settins
of
atrial
fibrillation
especially non
valvular
ryp".23'24The other
risk
factors
found
in a
small number of
patients were congestive heart
disease
,
prior
TIA,
valvular
heart diseases,policythemia, oral
contracep-tive pills
andalcohol consumption, respectively.
Hypercholesterolemia (defined
as
total
cholesterol
level
>
250
msVo\
was found
in
16.4
7o of strokepatients.26
Alth-ough hypercholesterolemia
is
an
im-portant
modifiable
risk factor for coronary
heart
dis-èase, thelink
toischemic stroke remains
uncertain.2TCarotid
bruit
was found
in
only 0.3
7oof
the
studysubjects because the
examination of cervical
bruit
maybe
not routinely done
on
every stroke patients in
Indonesia or as some studies revealed that
small
vesseldiseases
are
more frequent
in
Asian
stroke
patients.Vol9, No 1, January - March2000
Stroke recurrence
Stroke
recurrence
was found
in
19.9Voof
patients.This finding
showedthat recurrent stroke
washigher
in Indonesian stroke
patients
compared
with
thatreported
in
some literatures.2eType
of
stroke
Because
CT
Scanswere
not
available
in all
hospitals,especially
in rural
areasin
Indonesia,
only 6l
.9
o/oof
the study patients were confirmed
by
CT
scan.
Is-chemic
strokes accounted
lor
42.9
Voand these
in-cluded lacunar
infarction
(11.1
Vo),
non
lacunar
anterior
circulation
(21 .0 Vo) and non lacunarposterior
circulation
(4.2
Eo).Hemorrhagic stroke
was detectedin
18.5 Vo,whereas subarachnoid hemorrhage was rare(l.4Vo). About
39.1Voof patients were
with
undeter-mined
causeof
stroke
becauseCT scans
were not
done.
The
frequency
of
stroke type
or
subtypein
this
study was rather
low
compared
with
theother
inves-tigator.3O
This might
be causedby the different
clas-sification
usedby
the investigators
andlarge number
of patients
without
CT
scaninvestigation
in
our study.Stroke
outcome
Although
most of stroke patients were dischargedalive
and
improved
from
the
lrospitals,
however,
hospital
mortality
wasfound
in
21 .2Vofbr
ischemic stroke
and28.2Vo
for hemorrhagic stroke.
This
data
showedhigher
results
thanin
western
literature.3l'32Length of hospital
stay
Mean
length
of
stay
of
survived
stroke
victims
was11
daysfor
ischemic stroke
and
19
daysfor
hemor-rhagic
stroke.
The result
revealed
that
non-medical
bed-days were
low
in most of the hospitals inIndonesia
because majority
of
our
patients were
low
social economy and no insurance coverage.Mayo
et al(1991)
reported thatnon-medical
bed-days werehigh in
strokepatients
with
he^qlthinsurance
status andhigh
socialeconomic
strata.33In
conclusion, we
have presented theclinical
data onstroke
profile involving most
of
the
hospitals in
In-donesia and
this descriptive
data
will
be
the
srartingpoint of further
investigations on various nation-wide
stroke
researchesin
Indonesia.Acknowledgments
We wish to thank
the
participating
neurologists
asfbllows:
Clinical pattem of hospitalized
strokes
33Jakarta
:Dr. Andradi
S ,Dr.
Teguh
Ranakusuma,Dr.
Wendra
Ali,
Dr.
A.Munandar,
Dr.
Rumaléan
Dr.Anwar Wardy, Dr. Ayub, Dr. Surjo Atmodjo, Dr.
Sukono,
Dr.
Susesty,
Dr.
Jusuf
Misbach,
Dr.Edy
Sunarto;
Medan
:
Dr.
Darulkutni; Banda Aceh
:Dr.
Syahrul;
Padang
:
Dr.Basjiruddin;
Palembang:
Dr.Margono; Bandung: Dr.Dede
Gunawan, Dr.
Adelyna Yaumir;
Semarang:
Dr.Sudomo
Surabaya:Dr.
Fauziah Baosier, Yogyakarta:
Dr.
Rusdi
Lam-sudin,
Bali: Dr.
Wayan Kondra;
Ujung
Pandang:Dr.Amiruddin;
Manado: Dr.
Siwi;
Pontianak: Dr.
Melani.
REFERENCES
1. WHO MONICA Project, Principal Investigators. The World
Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major inter-national collaboration. J Clin Epidemiol 1988 ;41 : 105-14. 2. Misbach J , Suryamiharja A , Malik MS , Sandia IN. Pattem
of
Hospitalized Strokein l0
Hospitalsin
Jakarta. Survey Reportby
Dept.of
Healthof
Indonesia, 1995.3.
Gillum RF. The
epidemiology
of
stroke
in
NativeAmericans. Stroke. I 995;26:2222-7
4. Bogousslavsky J, Melle GV, Regli F. The Lausanne Stroke Registry: an analysis of 1000 consecutive patients with first
stroke. Stroke. I 988; I 9: I 083-92.
5. Caplan LR, Kargman DE, Gu Q, Zamanillo MC. Race, sex and occlusive cerebrovascular disease: a review. Stroke.
I 986;1 7:648-55.
6. Chambers BR, Donnan GA, Baldin PF. Pattern of stroke: an
analysis of the first 700 consecutive admisssion to the Austin
Hospital stroke unit. Aust N
ZJ
Med. 1983;13:57-64 7. Shi F, Hart RG, Sherman DG, Tegeler CH. Strokein
thePeople's Republic of China. Stroke 1989;20: 1581-5. 8. Hu,HH, Sheng WY, Chu FL, Lan CF, Chiang BN. Incidence
of Stroke in Taiwan. Stroke 1992;23:123'7-41.
9. Turney TM, Garraway WM, Whisnant JP. The natural his-tory of hemispheric and brainstem infarction in Rochester, Minnesota. Stroke 1984 :15 :790
-94.
10, Gogelholm R, Murros K, Rissanen A, Ilmavirta M. Factors, delaying hospital admission after acute stroke. Stroke. 1996
',27:398-400.
I
L
Anderson NE, Board JB, Bonita R. Delays in hospitaladmis-sion and investigation in acute stroke.
BMI.
1995;3ll
: 162.12. Feldmann E, Gordon N, Brooks JM, Fayd PB, Sawaya KL,
Nazareno
F,
Levine
SR. Factors associatedwith
early presentation ofacute stroke. Stroke.1993
24:
1805-
10.13. Harper GD, Haigh RA, Potter JF, Castleden CM. Factors delaying hospital admission after stroke in Leincastershire. Stroke. 1992 ; 23 : 835
-
838.14. Biller J, Shephard A, Adams HP. Delay time between onser
of ischemic stroke
&
hospital arrival. Neurology. 1992;42 (suppl 3):250. Abstract.15. Vestergaard
K,
et al.
Headachein
Srrôke. Stroke. 1993;24:1621-24.
16. Rutan GH, KullerLH, James PH, et al,. Mortality associated
hyperten-34
Misbach and Wendrasron among men screened
for
theMultiple Risk
Factor Intervention Trial. Hypertension. 1988;77:504-14.17. Broderick JP. Intracerebral hemorrhage.
In:
Gorelick PB, Alter M, eds. Handbook of Neuroepidemiology. New York.NY: Marcel Dekker Inc; 1994.
18. Mac mahon S, Rodgers A. The epidemiologycal association
between blood pressure and stroke: implication for primary
and secondary prevention. Hypertension. 1994; l7(suppl 1):
s23-S32.
19. Whisnant JP. Effectiveness versus efficacy of treatment
of
hypertensionfor
stroke prevention. Neurology. 1996;46:.301-7.
20. Dyken
ML, Wolf
PA, Barnett HJM, Bergan JJ, Haa WK,Kannel WB, Kuller L, Kurrzke JF, Sundt TM. Risk factor in stroke. Stroke. 1984;15:l
105-ll.
21. Wolf PA, D'Agustino RB, Kannel WB, Bonita R, Belanger
AJ. Cigarette smoking as a risk factor for stroke : the Framin-gham Study. JAMA. 1993;269:232-6.
22. Shinton
R,
BeeverG,
Meta-analysisof
relation betweencigarette smoking and stroke : BMJ. 1989;298:789-94.
23. Wolf PA, Abbot RD, Kannel WB. Arrial flbrillarion as an
independent risk factor for stroke: the Framingham Study.
Stroke. 1991 ;22;983-8.
24. Wolf PA, Benyamin EJ, Belanger AJ, Kannel WB, Levy D,
D'Agostino RB, Secular trends in the prevalence
of
atrialfibrillation
as an independent risk factorfor
stroke: theFramingham Study. Am Hearr J. 1996;131;790-5.
Med J Indones
25. Burchfiel CM, Curb JD, Rodriquez BL, Abbor RD, Chiu D, Yano K. Glucose intolerance and 22 year stroke inciclence;
Honolulu Heart Program. Stroke. I 99 4;25 :9 5 l-7 .
26. Iso H, Jacobs DR Jr, Wenworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality tiom stroke
in 350 977 men screened fbr the multiple risk factor inter-vention trial . N Eng J Med. l989;320:904-
l0
27. Summary of the National Chlolesterol Education Program (NCEP)
Adult
Treatment PanelII
report.JAMA.
1993;269:3015-23.
28.
Wolf
PA, Kannel WB, Sorlie P,
Mc
Namara
P.Asymptomatic neck bruits. N. Eng J Med. 1986;315:860-5.
29. Sacco RL, Wolf PA, Kannel WB, Mc Namara PM. Survival and recurrence
following
stroke: the Framingham study. Stroke. 1 982;1 3:290-530. Batnfbrd J, Sandercock P, Dennis
M,
Burn J, Warlow C.Classifrcation and natural history of clinically indentifiable
subtypes ofcerebral infarction. Lancet
l99l
;337:
l52l
-26.
31. Bamford J, Dennis
M,
Sandercock P, et al. The frequency,causes and timing of death within 30 days of a first stroke:
the
Oxfordshire Stroke Project.J.
Neurol
Neurosurg Psychiatry. 1990;53 :824-9 .32. Ellekjaer H, Holmen J, Indredavik B, et al. Epidemiology of
Stroke in Innherred, Norway, 1994 to 1996: Incidence and
30-day Case fatality Rate. Stroke. 1997;28:2180-4. 33. Mayo NE, Wood-Dauphinee S, Gayton D, et al. Nonrnedical
Bed-Days for Stioke Patients Admitted Acute Care