Infertility
Intraoperative Distal Vasal Flushing—Does
It Improve the Rate of Early Azoospermia
Following No-scalpel Vasectomy? A
Prospective, Randomized, Controlled Study
Dharamveer Singh, Nandan S. Dasila, Pawan Vasudeva, Divakar Dalela,
Satyanarayan Sankhwar, Apul Goel, Vishwajeet Singh, Anjana Singh, Abhishek Jain,
Bhupendra P. Singh, and Nisar Ahmed
OBJECTIVE To assess the impact of intraoperative distal vasal flushing during no-scalpel vasectomy on hastening the sperm clearance from the vas deferens and subsequent postvasectomy time to azoospermia.
MATERIAL AND METHODS
A total of 906 men undergoing vasectomy at our center from October 2007 to August 2008 were included in this prospective, randomized, controlled study. Patients were alternately allocated to 1 of 2 groups. Group A were patients who underwent no scalpel vasectomy alone; Group B patients, in addition to no scalpel vasectomy, underwent flushing of the distal vasal segment with 30 mL of sterile water. Postvasectomy semen analysis was done at 4, 8, and 12 weeks. The age, operative time, number of ejaculations, and proportion of patients’ azoospermic at 4, 8, and 12 weeks after vasectomy were compared between the 2 groups.
RESULTS A total of 727 men were available for final analysis. A significantly higher proportion of patients in group B were azoospermic at 4 and 8 weeks when compared with group A (group B: 53.40% and 80.68%; group A: 33.86% and 49.6% at 4 and 8 weeks, respectively). There was no statistically significant difference in the mean age, operative time, and number of ejaculations between the 2 groups.
CONCLUSIONS Distal vasal flushing with 30 mL of sterile water may shorten the time to azoospermia for between 20% and 30% of vasectomy patients. Thus, this procedure may be an option for some who choose the vasal flush to avoid the long duration of postvasectomy alternate contraceptive methods. UROLOGY
76: 341–346, 2010. © 2010 Elsevier Inc.
A
lthough no-scalpel vasectomy (NSV) is an easy, safe, cost-effective, and reliable method of male contraception, a potential drawback of the pro-cedure is that the patient does not become infertile immediately after surgery but does so after a variable time lag, necessitating the use of an alternate contraceptive method for a variable period. This delay has been attrib-uted to the time it takes for clearance of sperm residing in the distal vas.1Various authors have tried to accelerate the onset of azoospermia by distal vasal flushing at the time of NSV using various solutions. These are thought to act by mechanical flushing and, in the case of sterile water, additional modes of action, including sperm lysisvia an osmotic effect and immobilization of the sperms, have been proposed.2Currently, no consensus exists on the usefulness of distal vasal flushing as an adjunct to tradi-tional NSV. The purpose of this study was to assess the impact of intraoperative distal vasal flushing on hasten-ing the sperm clearance from the vas deferens and sub-sequent time to azoospermia after vasectomy.
MATERIAL AND METHODS
This study was undertaken after approval from the institutional ethics committee. Consecutive patients undergoing NSV at our center from October 2007 to August 2008 were included in this prospective, randomized, controlled study, with blinding of both the participants and the outcome assessor. Surgeons were not blinded. Exclusion criteria included (a) patients who did not adhere to the post-NSV evaluation protocol as described later, and (b) patients who did not give consent for the study. Included patients were alternately allocated to one of the 2 groups, and sequentially numbered, opaque, sealed envelopes were used for allocation concealment.
From the Centre of Excellence for No-Scalpel Vasectomy; and Department of Urology, CSM, Medical University (Upgraded King George’s Medical College), Uttar Pradesh, India
Reprint requests: Dr. Dharamveer Singh, Centre of Excellence for no-scalpel vasec-tomy, Department of Urology, CSM, Medical University (Upgraded King George’s Medical College), Lucknow-226 003, UP, India. E-mail:drdharamveersingh@yahoo. co.in;[email protected]
© 2010 Elsevier Inc. 0090-4295/10/$34.00 341
Vasectomy Technique
Group A (control group) underwent NSV as described by Li et al. along with segmental excision of vas and fascial interposition between the suture ligated cut ends.3 Group B (intervention
group), in addition to NSV, underwent bilateral flushing of the distal vas. This was accomplished on each side by gently push-ing in 30 mL of sterile water via a 20-G intravenous cannula inserted for a distance of about 1.5 cm through the open cut end of the distal vas. Once flushing was completed, the distal vas was ligated just beyond the cannula and the segment of distal vas proximal to the ligature was excised. Vasectomy in both groups was performed under local anesthesia by 3 experienced surgeons (certified NSV trainers).
Semen Analysis.Evaluation protocol in the follow-up period consisted of semen analysis at 4, 8, and 12 weeks after NSV, irrespective of the findings of semen analysis. The participants were asked to produce a semen sample in a private room at the laboratory. Semen samples were examined within 1 hour of collection. An aliquot was examined by phase-contrast micros-copy at high-power magnification (400x) to estimate sperm concentration. Based on the estimated concentration, dilutions were prepared to assess exact sperm concentration and motility. The concentration and motility of each sample were deter-mined using a Neubauer hemocytometer. Samples with no sperm (azoospermia) on the initial unspun semen analysis were centrifuged for 15 minutes at 600 g and then reassessed for sperm concentration and motility as described before.
Study Outcomes.The primary outcome measure was azoosper-mia (no detectable sperm on spun semen analysis), either as the rate at postvasectomy follow-up visits or the time to azoosper-mia. Secondary outcomes included were the incidence of inter-mittent sperm reappearance in the ejaculate after a period of azoospermia, number of ejaculations, operating time, and ad-verse events. Further, patients were instructed to record all episodes of ejaculation post-NSV for a period of 12 weeks. The 2 groups were compared with regard to age, operative time, number of ejaculations, frequency and type of complications, and the proportion of patients azoospermic at 4, 8, and 12 weeks after NSV. For the purpose of this study, all patients whose semen sample was negative for sperm (azoospermia) at 4 and/or 8 weeks still underwent semen analysis at 12 weeks to see the incidence of early intermittent reappearance of sperm.
Sample Size Estimation and Statistical Analysis Methods.An a priori sample size calculation was done and our plan was to enroll at least 300 participants in each group to get 80% power to detect a difference between the groups, with a two-sided test and an alpha of 0.05. Data analysis was done using SPSS software (version 11.5, SPSS, Inc., Chicago, IL) and a two-sidedPvalue of⬍0.05 was considered statistically significant. Fisher’s exact test was used for comparisons of the dichotomous (azoospermia) variables and Welch’s correctedt-test was used to compare the means.
RESULTS
A total of 1566 men underwent NSV during the study period. Of these, 906 patients gave consent for the study. One-hundred seventy-nine (19.76%) of the 906 men were subsequently excluded because of nonadherence to the follow-up evaluation protocol, leaving 727 (80.24%)
men (group A: 375 men; group B: 352 men) available for final analysis (Fig. 1). Mean age, mean operative time, and mean frequency and type of complications did not differ significantly between the 2 groups. Complications were hematoma, infection, chronic orchalgia, palpable nodule (sperm granuloma), and dissatisfaction with sur-gery. None of the patients in both groups complained of symptoms suggestive of “clinical” prostatitis, such as fe-ver, dysuria, and voiding or storage lower urinary tract symptoms. Two patients in group B and 1 patient in group A complained of self-limiting painful ejaculation between days 5 and 9; however, none had clinical hema-tospermia. A transient desire to urinate was described by most patients in the irrigation group.
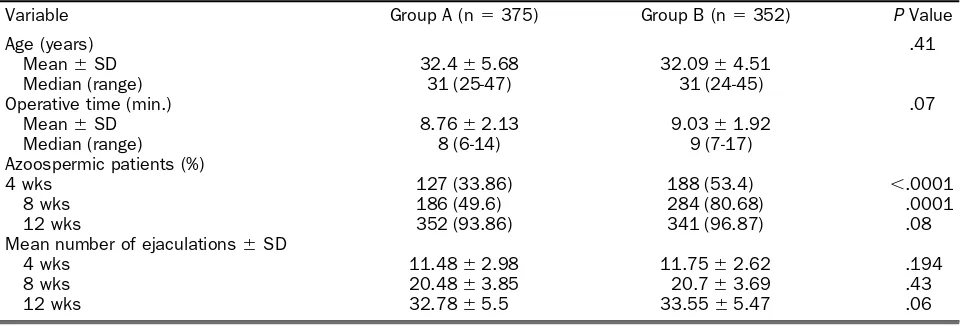
A significantly higher proportion of patients in group B were azoospermic at 4 and 8 weeks when compared with group A (group B: 53.40% and 80.68%; group A: 33.86% and 49.6% at 4 and 8 weeks, respectively). The propor-tion of azoospermic patients at 12 weeks did not differ significantly between the 2 groups. The mean number of ejaculations at 4, 8, and 12 weeks did not differ signifi-cantly between the 2 groups (Table 1).
COMMENT
Although NSV is rapidly gaining in acceptance as a contraceptive method, the delay in achieving “infertile status” is a factor that affects the patient acceptability of the procedure. Further, a major cause of vasectomy fail-ure/unwanted pregnancy, especially in developing coun-tries, is an ill-informed or negligent patient who assumes that he is sterile shortly after the procedure. Any method that would help in achieving rapid sperm clearance would in part address the those issues.
Figure 1. Study participant disposition flow chart.
Currently, there is little consensus about whether flushing of the distal vas helps to achieve azoospermia earlier. Sommer et al, in a study of 59 patients, used 40 mL of sterile water for vasal flushing and reported a significantly shorter time to azoospermia.4Roshani et al, in a study of 126 patients, also reported significantly higher azoospermic rates of 100% at 12 weeks and 88.1% at 16 weeks in patients who underwent distal vasal flush-ing with 40 mL of sterile water and saline solution, respectively, when compared with patients in whom va-sal flushing was not used (26.2% azoospermic at 16 weeks).5 In contrast, studies by Mason et al (200 men
undergoing vasectomy with or without vasal lavage using 10 mL of sterile water) and Eisner et al (106 men under-going vasectomy with or without vasal flush using 10 mL of normal saline) failed to demonstrate any benefit of distal vasal flushing insofar as hastening azoospermia was concerned.2,6 Although it may be argued that these 2 studies may not have been able to demonstrate a signif-icant difference in outcomes because the quantity of fluid used to flush the vas was suboptimal in both (10 mL), a nonrandomized, controlled study of 72 patients by Pearce et al, in which 50 mL of normal saline was used for vasal flushing, also did not demonstrate any benefit in terms of hastening azoospermia.7In addition, the possible
expla-nation could be that all of these trials were poor quality and relatively small and therefore underpowered. None of the previously cited studies mentioned about the method of semen analysis (spun vs unspun sample), ex-cept Mason et al, used a centrifuged semen sample for postvasectomy semen analysis.
Another reason for discrepancies between the results of various studies may be that these studies did not take into account the number of ejaculations during the fol-low-up period, because time to infertility also depends on the frequency of postoperative ejaculations.4The number of ejaculations after NSV is also important in addition to the time period to achieve azoospermia; approximately 80% of patients are azoospermic after 3 months and after about 20 ejaculations.8In our study, the mean number of
ejaculations between the 2 groups did not differ signifi-cantly at any point in the follow-up and hence it seems reasonable to presume that it was the vasal flushing that resulted in a significantly higher percentage (between 20% and 30%) of patients being azoospermic at 4 and 8 weeks postvasectomy.
Another area of controversy is when to label a man infertile after NSV. There is no absolute standard of care when it comes to declaring a patient sterile. Follow-up semen analysis at least 2-3 months after vasectomy, with the goal of obtaining at least 1, and preferably 2, abso-lutely azoospermic specimens 4-6 weeks apart, is recom-mended.8-11Because intermittent reappearance of sperm usually occurs early after vasectomy, for the purpose of this study, patients whose semen sample was negative for sperm at 12 weeks were finally considered infertile. For those who achieved azoospermia earlier, subsequent sam-ples as per protocol were still taken to ensure that the patient’s semen remained sperm-negative. The study end point was taken as completion of 12 weeks’ follow-up after NSV regardless of azoospermic status. Three pa-tients in group A and 2 papa-tients in group B whose semen sample was negative for sperm at 4 weeks had reappear-ance of sperm during semen analysis at 8 weeks. Semen analysis at 12 weeks showed that all 5 patients again became azoospermic, so they were considered infertile, the timing of infertility being taken as 12 weeks in all 5. One patient in group A who had a semen sample nega-tive for sperm at 8 weeks showed sperm in his semen sample at 12 weeks and was considered not to have become infertile as per study protocol. Thus, reappear-ance of sperm was seen in 6 patients during the whole follow-up period of 12 weeks. It is controversial whether this early intermittent reappearance of motile sperm in semen is the result of transient early recanalization or residual sperm in the distal vas. Regarding vas irrigation, some experts believe that the presence of motile sperm in semen after 4-6 weeks is more likely to be the result of transient early recanalization rather than residual sperm in the distal vas.12The chances of recanalization are less
Table 1. Comparison of variables and results of semen analysis between group A and B
Variable Group A (n⫽375) Group B (n⫽352) PValue
Age (years) .41
Mean⫾SD 32.4⫾5.68 32.09⫾4.51
Median (range) 31 (25-47) 31 (24-45)
Operative time (min.) .07
Mean⫾SD 8.76⫾2.13 9.03⫾1.92
Median (range) 8 (6-14) 9 (7-17)
Azoospermic patients (%)
4 wks 127 (33.86) 188 (53.4) ⬍.0001
8 wks 186 (49.6) 284 (80.68) .0001
12 wks 352 (93.86) 341 (96.87) .08
Mean number of ejaculations⫾SD
4 wks 11.48⫾2.98 11.75⫾2.62 .194
8 wks 20.48⫾3.85 20.7⫾3.69 .43
12 wks 32.78⫾5.5 33.55⫾5.47 .06
when fascial interposition is used along with excision and ligation of vas, because an international multicenter trial of vasectomy with and without fascial interposition dem-onstrated a 2-fold reduction in failure rates using fascial interposition.13 Although uncommon, the late failure rate has been reported to be 0.04%-0.08%, and recana-lization is usually only discovered after pregnancy in the female partner.14 However, so far we have not received report of any pregnancy.
The findings of azoospermia differ in the whole semen (unspun) versus the spun specimen. The laboratory should examine a freshly produced seminal fluid specimen by direct microscopy and if no sperm are seen, the centri-fuged sample should be examined for the presence of motile and nonmotile spermatozoa.15Semen centrifuga-tion should be performed in all men considered to have azoospermia by routine semen analysis because studies have demonstrated the presence of motile and nonmotile sperm in a significant number of men considered to have azoospermia by routine semen analysis.16
Our study shows that distal vasal flushing with sterile water does shorten the time to azoospermia in a statisti-cally significant number (between 20% and 30%) of patients at 4 and 8 weeks after NSV. For developing countries, it may also be important from an economic point of view, to reduce the 1-month cost of barrier methods because semen analysis at 8 weeks was negative for sperm in more than 80% of cases of vasal flushing. Vasal flushing may also reduce, to some extent, the chances of unwanted pregnancies in uneducated, poor, and neglected communities of developing countries in addition to increasing the acceptance rate for vasectomy. Although no formal survey was conducted regarding whether the difference of 4 weeks had any importance to these patients in choosing vasectomy, the clients often raised concerns about the long duration of postvasectomy condom usage. After this study, our current “clinical” protocol for post-NSV semen analysis is a single semen analysis at 8 weeks. If the patient is sterile (azoospermic on spun semen analysis) at 8 weeks, we do not pursue further semen analysis in these patients and an additional semen analysis is done monthly until azoospermia is achieved or up to 6 months in patients who had sperm in their semen samples at 8 weeks.
To our knowledge, this is the largest reported randomized, controlled trial addressing the issue of the effect of distal vasal flushing on the time taken to achieve azoospermia. Limitation of our study is lack of long-term follow-up and a high rate of exclusion (19.76%) after randomization because of nonadher-ence to the follow-up evaluation protocol. Loss to follow-up rates greater than 20% may threaten the validity of trials.17
Patient compliance decreases significantly with each subse-quent visit for post-NSV semen analysis,10thus, in our opinion the overall compliance rate of more than 80% in the present study is not unacceptably high. Although extremely rare, there is some theoretical risk that the catheter itself might create risk of recanalization by damaging the vas. Another theoretical
concern is the risk of seminal vesiculitis, prostatitis, and inflam-mation inside the lumen of the distal vas, which may compro-mise the luminal patency of the abdominal vas during future vasectomy reversal. Finally, because these results are based on 1 large trial, the evidence would be stronger if confirmed by a second trial.
CONCLUSIONS
Distal vasal flushing with 30 mL of sterile water may shorten the time to azoospermia to between 20% and 30% of va-sectomy patients. Thus, this procedure may be an option for some who choose the vasal flush to avoid the long duration of postvasectomy alternate contraceptive methods.
References
1. Sukapiriya C, Chanpalakorn N, Chalermsanyakorn P, et al. Sites of residual spermatozoa after irrigation of the distal vas deferens using
normal saline solution during vasectomy in a rat model. Int J
Androl. 2005;28(4):230-233.
2. Mason RG, Dodds L, Swami SK. Sterile water irrigation of the distal vas deferens at vasectomy: does it accelerate clearance of
sperm? A prospective randomized trial.Urology. 2002;59:424-427.
3. Li SQ, Goldstein M, Zhu J, et al. The no-scalpel vasectomy.J Urol.
1991;145:341-344.
4. Sommer F, Eusan A, Caspers HP, et al. Effect of flushing the vasa
deferentia at the time of vasectomy on the rate of azoospermia.BJU
Int. 2001;88(Suppl 1):9.
5. Roshani A, Falahatkar S, Khosropanah I, et al. Vasal irrigation with sterile water and saline solution for acceleration of
postvasec-tomy azoospermia.Urol J. 2008;5:37-40.
6. Eisner B, Schuster T, Rodgers P, et al. A randomized clinical trial of the effect of intraoperative saline perfusion on postvasectomy
azoospermia.Ann Fam Med. 2004;2:221-223.
7. Pearce I, Adeyoju A, Bhatt RI, et al. The effect of perioperative distal vasal lavage on subsequent semen analysis after vasectomy: a
prospective randomized controlled trial.BJU Int. 2002;90:282-285.
8. Griffin T, Tooher R, Nowakowski K, et al. How little is enough?
The evidence for postvasectomy testing.J Urol. 2005;174:29-36.
9. Barone MA, Nazerali H, Cortes M, et al. A prospective study of time and number of ejaculations to azoospermia after vasectomy by
ligation and excision.J Urol. 2003;170:892-896.
10. Badrakumar C, Gogoi NK, Sundaram SK. Semen analysis after
vasectomy. When and how many?BJU Int. 2000;86:479-481.
11. Sivardeen KA, Budhoo M. Post vasectomy analysis: call for a uniform evidence-based protocol.Ann R Coll Surg Engl. 2001;83:177-179. 12. Cook LA, Van Vliet HAAM, Lopez LM, et al. Vasectomy occlusion
techniques for male sterilization.Cochrane Database Syst Rev. 2009;
issue 3;Art. No. CD003991. [10.1002/14651858.CD003991.pub3]. 13. Sokal D, Irsula B, Investigator Study Group, et al. Vasectomy by
ligation and excision, with or without fascial interposition: A
random-ized controlled trial [ISRCTN77781689].BMC Med. 2004;2:6.
14. Alderman PM. The lurking sperm. A review of failures in 8879
vasectomies performed by one physician.J Am Med Assoc. 1988;
259:3142-3144.
15. Hancock P, McLaughlin E. British Andrology Society guidelines
for the assessment of post vasectomy semen samples.J Clin Pathol.
2002;55:812-816.
16. Jaffe TM, Kim ED, Hoekstra TH, Lipshultz LI. Sperm pellet anal-ysis: A technique to detect the presence of sperm in men
consid-ered to have azoospermia by routine semen analysis.J Urol. 1998;
159:1548-1550.
17. Strauss SE, Richardson WS, Glasziou P, et al.Evidence-Based
Med-icine: How to Practice and Teach EBM, 3rd ed. New York: Churchill Livingstone; 2005.