FULL PAPER
RADIOACTIVE IODINE ABLATION IN YOUNG
ADULTS WITH DIFFERENTIATED THYROID
CARCINOMA
Jelani YT and
Kartamihardja AHS
Department of Nuclear Medicine,
School of Medicine Universitas Padjadjaran, Dr. Hasan Sadikin Hospital,
Bandung, Indonesia.
POSTER PRESENTATION
4
thInternational Conference on Radiopharmaceutical Therapy
New World Hotel, Ho Chi Minh City, Vietnam
RADIOACTIVE IODINE ABLATION IN YOUNG ADULTS
WITH DIFFERENTIATED THYROID CARCINOMA
Yustia Tuti Jelani andAHS Kartamihardja
Department of Nuclear Medicine
Faculty of Medicine Universitas Padjadjaran/Dr. Hasan Sadikin Hospital. Bandung, Indonesia
Introduction. The prevalence of thyroid carcinoma in young adults is about 10% of
thyroid malignancy cases. We reported our experience in using radioactive iodine
(NaI-131) ablation for young adults with post-total thyroidectomy differentiated
thyroid carcinoma.
Material and Methods. A retrospective study was conducted in young adults subjects
with differentiated thyroid carcinoma who has undergone post-total thyroidectomy
and followed by radioiodine ablation therapy.Data was collected from 25 medical
records in our department from 1998 to 2010. Histological and laboratory findings
(serum TSHs, thyroglobulin/Tg and Anti-Thyroglobulin Antibody/ATA levels) were
noted until at least six months after ablation. Only 15 patients were eligible.Complete
response after ablation was defined if Tg serum level < 3 ng/ml, with TSHs serum
level > 30 µIU/ml and no detected ATA level; outside this level was defined as
residual disease.
Results. Of 15 subjects (12 females and 3 males, aged 13-21 years.), 9 subjects
werepapillary thyroid carcinoma / PTC (60%) and 6 subjects werefollicular thyroid
carcinoma / FTC(40%). Metastases were found in in 5subjects (33.3%) with
locoregional lymphatic metastases, 3 subjects (20%)with pulmonary metastases, one
tissue. The first ablation I-131 dose was given between 80-100 mCi. Next I-131 were
given after 6-12 months or more, if needed,by increasing the dose to 150 mCi. Three
subjects (1 PTC, 2 FTC) hadcomplete response after first ablation, one subject (1
PTC) after second dose, and one subject (1 PTC) after third dose. Four of five
subjectshad thyroglobulin serum level < 10 ng/dl. Eighteen months after radioiodine
ablation, 10 subjects (66.6%) were categorized as residual cases with thyroglobulin
serum level more than 10 ng/dl. There was no side effect observed in all subjects.
Discussion. The mainstream management of differentiated thyroid carcinoma is total
thyroidectomy, followed by radioactive iodine (I-131) ablation and suppressive doses
of thyroid hormone.Complete response was found in 3 subjects after six months
radioactive iodine ablation. Other studies used thyroglobulin serum level < 3 ng/dl as
the criteria of good response to therapy. Based on this criteria, good response was
found in four patients with thyrogobulin serum level < 3 ng/dl.
Papillary thyroid carcinoma in young adult has a favorable prognosis. The favorable
prognosis is associated with lymphocytic infiltration, as an anticancer reaction during
the imunologic activity.Young adults usually have more advanced tumors, with local
and distant metastases, higher recurrence rates. Children under 10 years of age have
very high mortality rates.
In conclusion. It seems that age, histopathology classification, and distant nodal
metastases are important factors for non-responsiveness of well differentiated thyroid
Introduction
Thyroid carcinoma is the most common malignancy in endocrinology. In 1999
more than 19.000 new cases was reported in United State of America and increased in
number compared to 11.300 new cases 1989. Based on histopathological type, thyroid
carcinoma divided into well differentiated, medullar and others type 90%, 7% and 3%
respectively.Among well differentiated thyroid carcinoma, papillary type was found
in 75% cases and the other 25% was follicular type.(1)Well differentiated thyroid
carcinoma has two peak incidence based on aged. Peak of incidence was in 3rd and 4th
decades, and the incidence in female patients was found 3 times compared to
male.(2)Prevalence of thyroid carcinoma in young adults is about 10% of thyroid
malignancy cases.
The management mainstream of differentiated thyroid carcinoma is total
thyroidectomy, followed by radioactive iodine (RAI-131) ablation and suppressive
doses of thyroid hormone.2,3The use of RAI-131 in the management of well
differentiated thyroid carcinoma is remain controversial.
The respond of thyroid carcinoma treatment is depends on several factors, such
as age, characteristic of cancer its self and technical surgery (near/total
thyroidectomy).
We reported our experience on using radioactive iodine ablation in young
Material and Methods
A retrospective study was conducted in Department of Nuclear Medicine Dr.
Hasasn Sadikin General Hospital Bandungfrom 1998 to 2010. Subject was young
adultpatients with differentiated thyroid carcinoma who has underwent post-total
thyroidectomy and followed by radioiodine ablation. Datas were collected from
medical records in our department. Histological and laboratory findings, such as
TSHs serum level, thyroglobulin (Tg)and Anti-Thyroglobulin Antibody (ATA) levels
were noted until at least six months after radioiodine ablation. Complete response
after ablation was considered, if Tg serum level < 3 ng/ml, with TSHs serum level
>30 µIU/ml and no detected ATA level; outside this level was considered as residual
disease.
Results
Twenty five subjects were included in this study, but only 15 subjects were
eligible, and the other 10 subjects were excluded due to uncompleted data. Eligible
subjects consist of 12 (80%) females and 3 (20%) males, age ranged 13-21 years
old.Papillary thyroid carcinoma (PTC) was found in9(60%)subjects and follicular
thyroid carcinoma (FTC) in6(40%)subjects.Locoregional lymphatic metastases was
found in 5(33.3%) subjects, pulmonary metastases in 3(20%) subjects, bone
metastases one(6.6%) subject and one (6.6%) subject with soft tissue metastases
(table 1). The first radioiodine ablation dose was given between 80-100 mCi
(3000-3700 MBq). In case repeated radioiodine should be given after 6-12 months later for
treatment, the dose of I-131 should be increazed to 150 mCi (5500 MBq). Complete
after second dose in 1 subject with PTC, and after third dose in 1 subject with PTC.
Four out of 5 subjects with complete response showed thyroglobulin serum level < 10
ng/dl. This study showed 10 (66.6%) subjects were categorized as residual cases 18
months after radioiodine ablation. Allof these 10 subjects showed thyroglobulin
serum level more than 10 ng/dl.
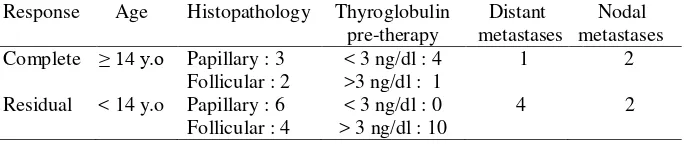
Table 1. Comparison of clinical features and outcome therapy RAI ablation of DTC in Hasan Sadikin Hospital and Theagenion Cancer Hospital.
Dr. HasanSadikin Hospital
Follow up 6-18 months 12-72 months
Complete
(60%) than follicular thyroid carcinoma type (40%).(1)This result is not much different
compare to the other study in literatures. The etiologyof papillary thyroid carcinoma
could be related to molecular aspect and history of radiation. BRAF was activated by
RAS mutation (RAS*), and BRAF will directly activate MEK. MEK will activate
ERK, then activate nuclear transcription factor (TF).5 Riesco-Eizaguirre, et al in 2006,
stated that BRAF mutation influence cancer cell aggressiveness and led to recurrent.(4)
External radiation to the neck area increased incidence of papillary thyroid carcinoma
particularly during childhood.The incidence of papillary thyroid carcinoma was
observed in 9% children 20 years after radiation exposure for hypertrophy of tonsil or
thymus enlargment. There was no correlation between history of radioiodine ablation
with incidence of papillary thyroid carcinoma.(5)
Number of female subjects in this study was 12 subjects. This results was in
accordance with literature that the incidence of thyroid carcinoma in female is 3 times
of male.(2)
Metastases of differentiated thyroid carcinoma could be found in locoregional
lymph node and distance metastases. Locoregional lymph node metastases in neck
area were found in 20-50%. This study showed 4 subject with papillary thyroid
carcinoma had Locoregional lymph node metastases, but there was no subject with
follicular thyroid carcinoma showed locoregional lymph node metastases.
The incidence of distant metastase was 3-7% patients at the time of diagnosis of
thyroid carcinoma and 4-5% in 10 years after surgery. Distance metastase could be
found in lung, bone and mediastinum. The incidence of lung metastase was higher in
male with 50-60% could uptake I-131. Patient with positive I-131 uptake has longer
survival rate compared to negative uptake. Lung metastase could be observed on CT
as micronodules (<5 mm), macronodules, or non visualized, but positive I-131uptake
post-ablation.(6,7) The incidence of bony metastase was 3.5% of cases and usually after
solid lesion. Bony metastases could be detected using I-131 whole body scintigraphy
and only 60% positive on Tc-99m bone scintigraphy.3,7 In this study showed 5
subjects had distance metastases.
In general the management of differentiated thyroid carcinoma is involving
thyroidectomy, followed by radioactive iodine (I-131) ablation and suppressive doses
of thyroid hormone.8 Although this management is accepted by many experts, but
there is still a controversial on type of thyroidectomy and the use of radioactive iodine
post thyroidectomy. Which type of surgery should be applied depend on stadium and
risk stratification.
Basic principle of radioactive iodine ablation in post thyroidectomy patient with
thyroid carcinoma is normal thyroid tissue as well as its metastases show ability to
uptake radioactive iodine in the similar mechanism. The goal of radioactive iodine
ablation is to ablate remnant normal thyroid tissue and metastases cell with the dose
of 80-100 mCi.8 In case radioactive iodine should be repeated after 6-12 month, the
dose is increased to 150-200 mCi.
Complete response after ablation was considered, if Tg serum level < 3 ng/ml,
with TSHs serum level >30 µIU/ml and no detected ATA level; outside this level was
considered as residual disease. Based on this criteria, in this study a good response
was found in 5 subjects with thyroglobulin serum level < 3 ng/dl, 5 subjects with
papillary type and 1 follicular type. Age of those 5 subjects was more than 14 years
old. (table 2). Papillary thyroid carcinoma in young adult has a favorable prognosis.
The favorable prognosis is associated with lymphocytic infiltration, as an anticancer
tumors, with local and distant metastases, higher recurrence rates. Children under 10
years of age have very high mortality rates.
Conclusion
Radioactive iodine ablation was safe for young adult patient with differentiated
thyroid carcinoma. Age, histopathology type, and distant nodal metastases are
important factors for non-responsiveness radiothyroablation therapy in young adults
patient with well differentated thyroid carcinoma.
Referrences
1. Goldsmith SJ. Thyroid Carcinoma. In Khalkhali I, Nuclear Oncology: Diagnosis
and Therapy. Lippincott Williams & Wilkins 2001: 187-217.
2. Lele RD. Nuclear Medicine in Thyroid Disease. In Principles and Practice of
Nuclear Medicine and Correlative Medical Imaging. Jaypee Brothers Medical
Publishers 2009: 207-224.
3. Oliveira MJ, Oliveira JMP. Treatment of Differentiated Thyroid Carcinoma. In
Eary JF and Brenner W (Eds). Nuclear Medicine Therapy. Informa Healthcare
USA 2007:45-75.
4. Eizaguirre GR, Martinez PG, Cabezas MA, Nistal M, Santisteban P. The
oncogene BRAFV600E is associated with a high risk of recurrence and less
differentiated papillary thyroid carcinoma due to the impairment of Na+/I-targeting
to the membrane. Endocrine-Related Cancer 2006; 16:257-269.
5. Gillespie MB, Hornig JD, Day TA, Noone MC, Goddard JC,Wilhoit CS, et al.
6. Schlumberger M, Pacini F. Thyroid Tumors. 3rd edition. Editions Nucléon, Paris
2006.
7. www.AuntMinnie.com. Papillary Thyroid Carcinoma (Roughly 66%of thyroid
cancers)
8. Masjhur JS, Kartamihardja AHS. Buku Pedoman Tatalaksana Diagnostik dan
Terapi kedokteran Nuklir. Bagian Kedokteran Nuklir, RSHS, FK Univ