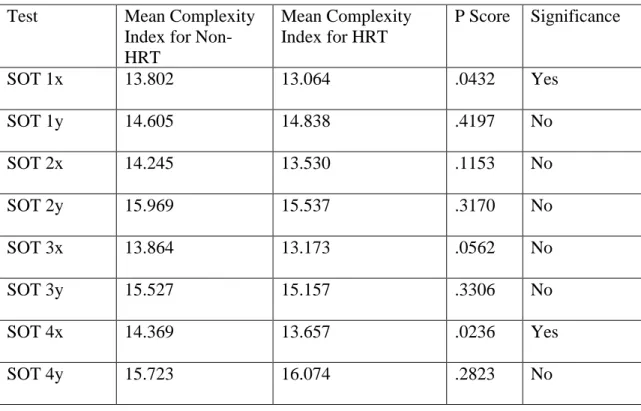
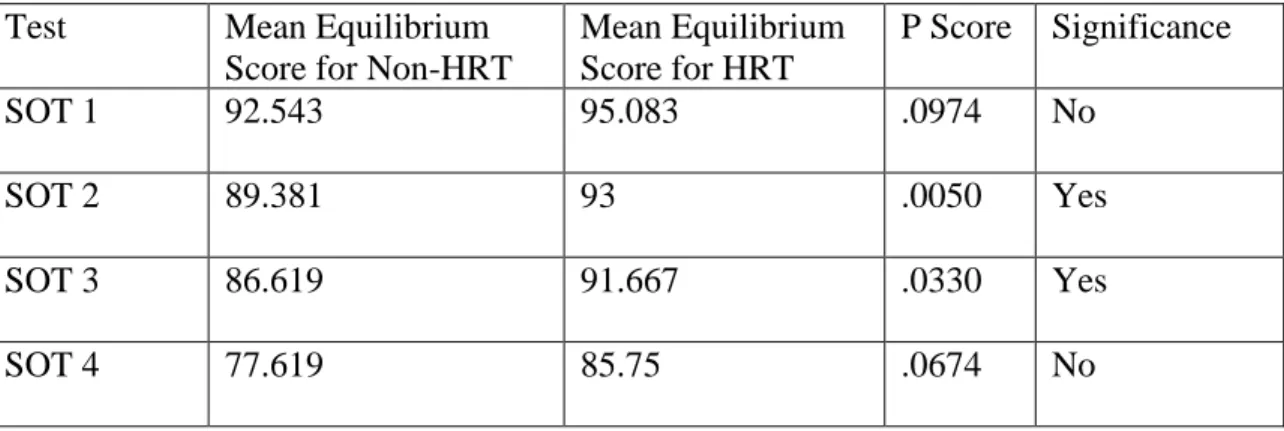
Postural stability was measured with the NeuroCom Equitest and using conditions 1-4 of the Sensory Organization Test (SOT). The MSE analysis method was able to significantly differentiate postural stability between non-HRT and HRT subjects in SOT 1 (p=0.0432), while the NeuroCom Equitest did not. The effect of estrogen on maintaining postmenopausal stability in postmenopausal women may provide further evidence for the.
Hormone replacement therapy (HRT) has been introduced as a preventive measure against falls and fractures by increasing postmenopausal women. Although postmenopausal women have shown an increase in postural stability while performing resistance training, they have shown the same results while receiving HRT alone [11, 12]. However, because resistance training can maintain muscle strength and connective tissue, the role of estrogen in maintaining postural stability is best explained as an effect on the central nervous system [11].
This reduction in function ultimately leads to inadequate use of the somatosensory and vestibular systems, leading to a decrease in postural stability [11]. To our knowledge, postmenopausal women, using or not using HRT, have not been examined with non-linear analysis. The present study aims to build on the consideration that the effect of estrogen on the central nervous system plays a crucial role in maintaining postural stability [11, 12].
Through nonlinear analysis of exercise variability in postmenopausal women, we expect that a decrease in estrogen in postmenopausal women results in a decrease in postural stability and an increase in fall risk compared to postmenopausal women using HRT.
TESTING STABILITY
For each of the four conditions, three trials of twenty seconds each are performed. At the beginning of the trial, the subject is also counted down and receives confirmation that the trial has started [24]. If the subject's balance score is close to 100, he experienced minimal sway and sufficient postural stability (green bars).
A low score indicates that the subject is rocking to the limit of stability and therefore has poor postural stability (red bars). The condition 2:condition 1 relationship represents the subject's reliance on their somatosensory system to maintain their postural stability. The results of each MCT condition are shown as a weight, latency, and amplitude symmetry scale (Figure 4).
Similar to the balance score chart for the SOT, subject scores for weight symmetry, latency, and amplitude scaling are compared to age-matched normative scores. A weight symmetry score close to 100 indicates that the subject had his weight relatively centered between his two legs before the start of the translation of the force platform. The subject latency score is the time (in milliseconds) between the translation of the force platform and the subject's active force response.
Since Latency is measured in milliseconds, a low Latency score for the subject is indicative of a fast active force response in the legs. The strength of the active force response in each leg as a result of the translations is represented by the value of Amplitude Scaling. This value reflects the subject's ability to produce a response in each leg that is proportional to the force platform translations.
Amplitude scaling results representing sufficient active force response force in proportion to the translation of the force platform will lie between the shaded regions of the graph (Fig. 4) [24]. Using entropy analysis, the complexity of the physiological system can be used as a representation of the level of postural stability in postmenopausal women [21]. Although ApEn measures the predictability of the data, it is quite sensitive to the length of the data [26].
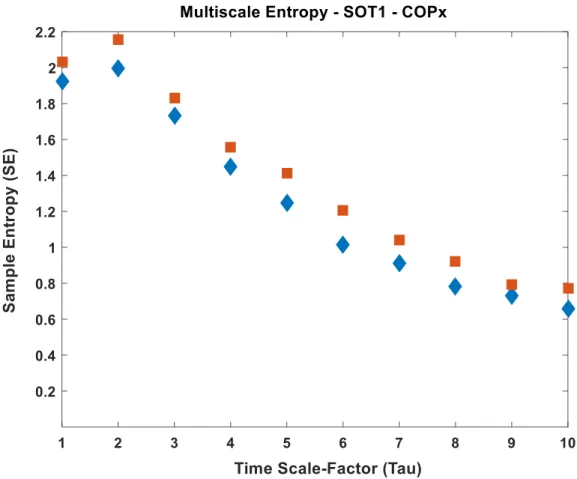
Investigating multiple time scales can reveal the relationship between different elements of the physiological system that contribute to the maintenance of postural stability. The advantages of including multiple time scales are that complexity can be analyzed at shorter or longer time scales and measure the overall complexity of the physiological system [ 21 ].
![Figure 1. The six conditions of the Sensory Organization Test [30]](https://thumb-ap.123doks.com/thumbv2/123dok/10459125.0/13.918.332.700.314.719/figure-1-conditions-sensory-organization-test-30.webp)
SUBJECTS AND METHODS
When a subject would arrive at the Neuromechanics laboratory, an IRB-approved investigator would provide the subject with a consent form, which they then washed. After completing the consent form, the investigator will instruct the subject to stand on the power platform of the NeuroCom Balance Manager. The examiner assisted in placing the subject's feet in the designated place on the platform.
Once the subject was positioned correctly and in a comfortable position, the investigator proceeded to explain each test that the subject will perform (sensory organization test and motor control test). Before the start of each trial for a condition, the investigator would count the subject down and begin the test after saying "go". After the completion of each trial, the investigator would instruct the subject to "relax" before. After completing both the Sensory Organization Test and the Motor Control Test, the investigator gave the subject a $20 gift card to Wal Mart for their participation in the study.
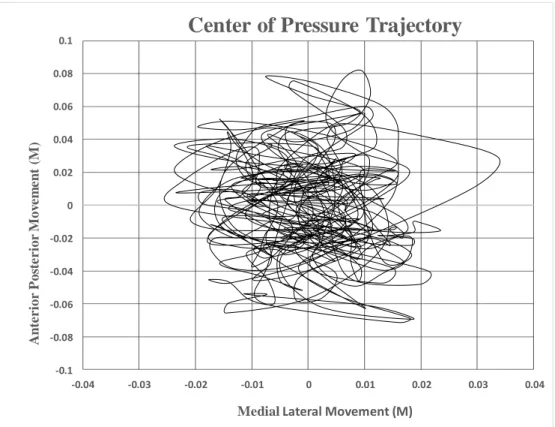
After receiving the gift card, the subject is then instructed by the researcher to complete an "incentive payment list," which verifies that he or she has received a gift card for completing the study. Although both SOT and MCT data were collected for this study, only SOT data will be analyzed and presented as the long time series output of this test is susceptible to entropy processing. Complexity indices for both lateral (medial-lateral – ML) and forward-posterior (anterior-posterior – AP) COP movements were calculated for SOT tests 1-4 and compared to clinical output scores received from the NeuroCom unit after each subject has finished the protocol.
Complexity indices are calculated from the ML and AP time series that form the center of pressure. A Matlab program was created that was an adaptation of the “Multi-Scale Entropy Analysis” program originally created by Costa et al., (2015) via the NIH-operated PhysioNet website [29]. The program “creates a set of coarse-grained series with a user-selected range of scales and calculates SampEn for each coarse-grained series.” A complexity index (CI) is calculated by adding all SampEn scores for all Tau values (area under the curve), as shown in example Fig.
![Figure 6. NeuroCom Balance Equitest [30]](https://thumb-ap.123doks.com/thumbv2/123dok/10459125.0/22.918.314.653.113.495/figure-6-neurocom-balance-equitest-30.webp)
RESULTS
CONCLUSION
For this study, we are interested in determining whether the MSE method can detect a difference between subjects without the need to manipulate conditions to induce a fall. Although the MSE method could not detect more differences than NeuroCom, it was able to detect a significant difference in SOT 1, while NeuroCom did not. To our knowledge, this is the first case of finding a significant difference in postmenopausal stability between non-HRT postmenopausal women and HRT women with conditions present in SOT 1.
Previous studies have not shown these results because their use of traditional assessment methods lacks the required sensitivity to distinguish a HRT subject from a non-HRT subject without attempting to induce a subject's fall [12]. Therefore, using the MSE method to analyze COP data may introduce a higher level of sensitivity needed to assess postural stability as a function of estrogen status. Currently, the MSE method, when used in conjunction with NeuroCom, can produce a more accurate representation of a postmenopausal woman's postmenopausal stability as a function of estrogen presence than previous traditional methods.
Thus, we can use the results from both analysis methods to support the assumption presented by Naessen et al. that estrogen can counteract the deterioration of complexity in movement. Further research into the MSE method and its ability to analyze postmenopausal stability in postmenopausal women may provide further evidence for the role of estrogen as a neuroprotective and protective factor for the risk of falling. Haber, N.E.L., et al., The relationship between age and measures of balance, strength, and gait: linear and nonlinear analyses.
Arnold, C.M., et al., Relationship of intrinsic fall risk factors to recent history of falls in elderly women with osteoporosis. Heikkinen, J., et al., HRT and exercise: effects on bone density, muscle strength and lipid metabolism. Phillips, S.K., et al., Muscle weakness in women occurs at an earlier age than in men, but strength is preserved with hormone replacement therapy.
Prieto-Alhambra, D., et al., Increased rate of falls leads to increased fracture risk in postmenopausal women with self-reported osteoarthritis: a prospective multinational cohort study (GLOW). Cangussu, L.M., et al., Evaluation of postmenopausal balance in postmenopausal women and its relationship with bone mineral density—a cross-sectional study. Figueroa, A., et al., Effects of exercise and hormone replacement therapy on lean and fat mass in postmenopausal women.
![Figure 2. Sensory Organization Test Example Results [30]](https://thumb-ap.123doks.com/thumbv2/123dok/10459125.0/14.918.234.741.531.871/figure-2-sensory-organization-test-example-results-30.webp)
![Figure 3. The Six Condition of the Motor Control Test [30]](https://thumb-ap.123doks.com/thumbv2/123dok/10459125.0/15.918.290.671.432.637/figure-3-condition-motor-control-test-30.webp)
![Figure 5. The Relationship Between Age, Variability, and Complexity [21]](https://thumb-ap.123doks.com/thumbv2/123dok/10459125.0/18.918.265.717.324.734/figure-5-relationship-age-variability-complexity-21.webp)