This thesis is submitted in partial fulfillment of the requirements for the degree Master of Medical Sciences (Microbiology and Immunology). In the present study, we subjected 394 such independent strains, representing 34.0% of the total CRE encountered, to a detailed analysis that involved the determination of their antibiotic susceptibility profile, of the type and alleles of the carbapenemases produced, of the pulsotypes and multi included locus. sequence types of the strains, respectively. The emergence and spread of these clones significantly influenced the local epidemiology of CRE, as they were generally more likely to be XDR or PDR than the rest of the collection.
Introduction
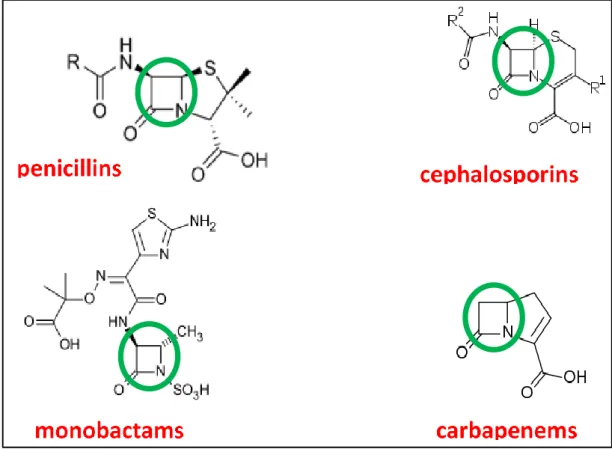
Beta-Lactam Antibiotics
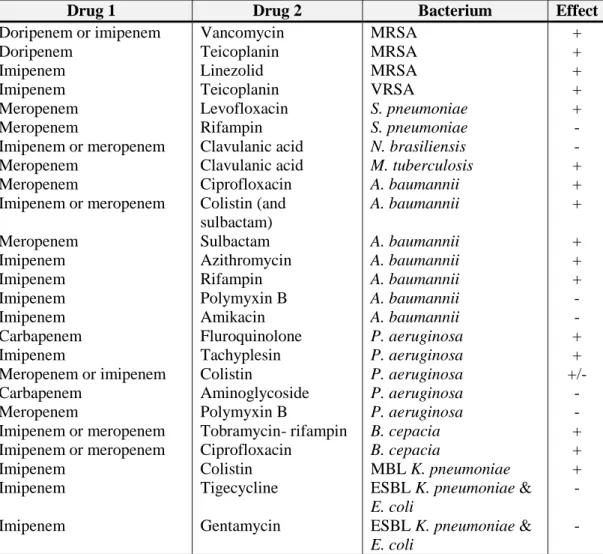
The third and fourth generations are called extended-spectrum cephalosporins, while fifth-generation antibiotics are also active against methicillin-resistant Staphylococcus aureus (MRSA) (Andes and Craig, 2010). Carbapenems are resistant to several hydrolytic enzymes, exhibiting the broadest antibacterial spectrum among all beta-lactam drugs. In the presence of beta-lactam drugs, cell wall synthesis will be disrupted and autolytic cell wall hydrolases will be activated leading to cell death.
Beta-Lactamases
They bind to and interfere with the function of the penicillin-binding proteins (PBPs), which are transpeptidases, transglycosylases and carboxypeptidases.
Beta-Lactamase Inhibitors
Currently, only avibactam of the non-beta-lactam group is approved for clinical use (Bush, 2015).
Carbapenems
- The Discovery of Carbapenems
- Mechanism of Action, Spectrum and Pharmacology
- Carbapenems in Therapy
- Side Effects
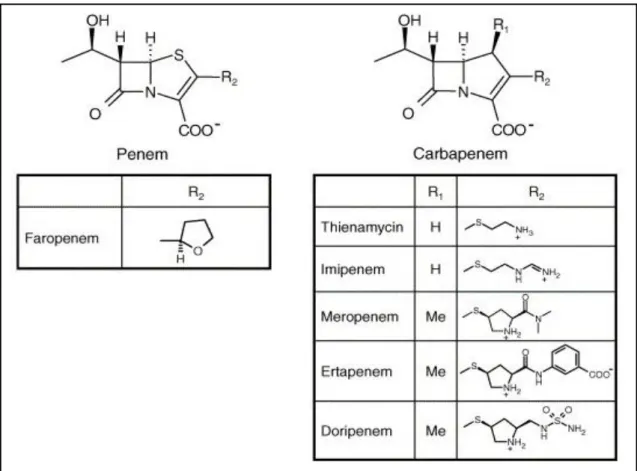
Other carbapenems such as meropenem, biapenem and doripenem were soon discovered (Figure 2) (Branch et al., 1998). Carbapenems are broad-spectrum antibiotics in vitro compared to available penicillins, cephalosporins and beta-lactam/beta-lactamase inhibitor combinations (Bassetti et al., 2009). The excitatory potential of carbapenems is panipenem > imipenem > biapenem > meropenem > doripenem (Dalhoff et al., 2006).
Carbapenem Resistance
- Modifications of the Target Site
- Expressing Enzymes with Low Carbapenemase Activity
- Porins
- Efflux Pumps
- Carbapenemases
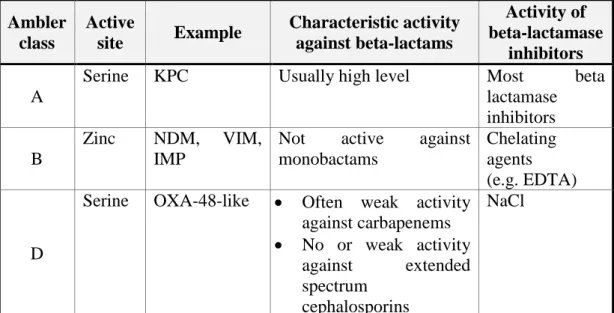
- Class A Carbapenemases
- Class B Carbapenemases (Zinc Dependent
- Class D Carbapenemases
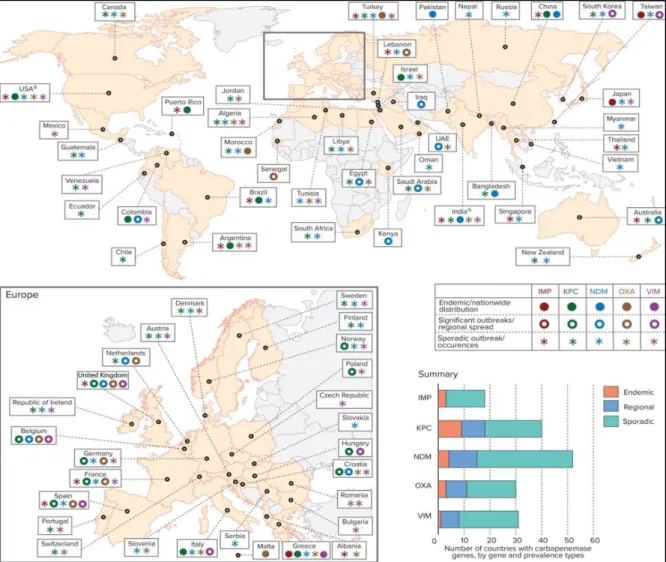
- Global Distribution of Carbapenemases of
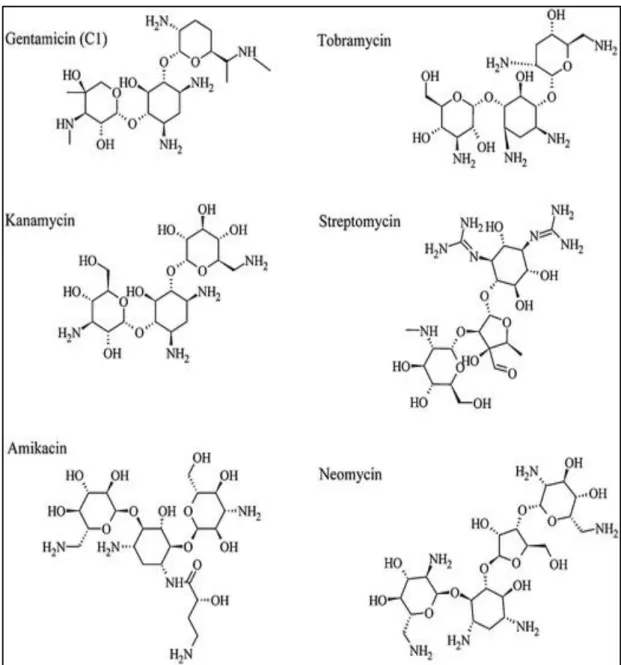
- Aminoglycosides
- Mode of Action
- Mechanisms of Resistance
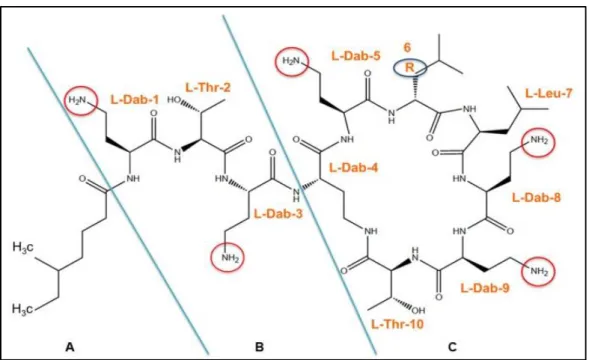
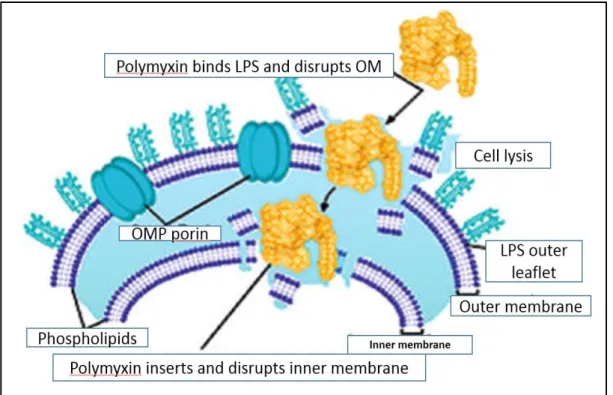
- Polymyxins
- Mode of Action
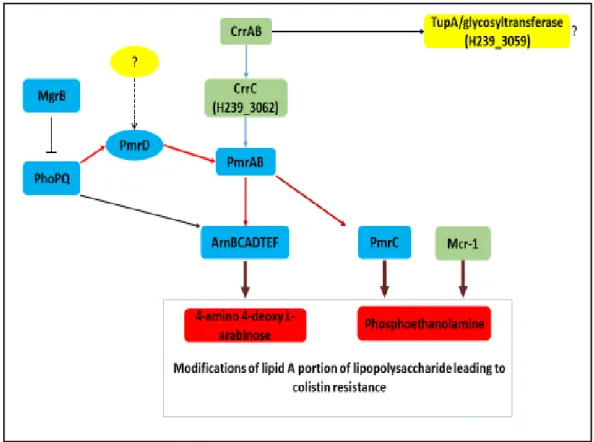
- Mechanisms of Resistance
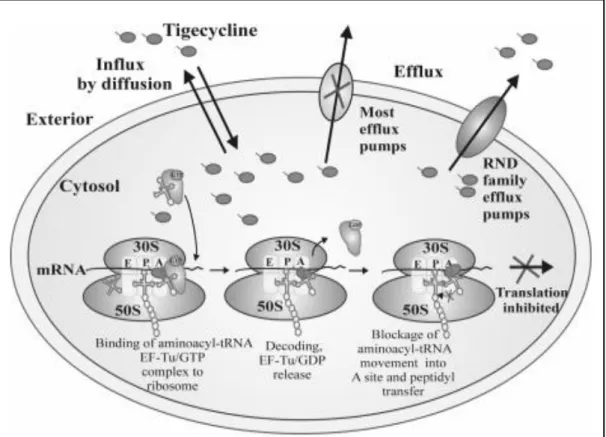
- Tigecycline
- Mode of Action
- Mechanisms of Resistance
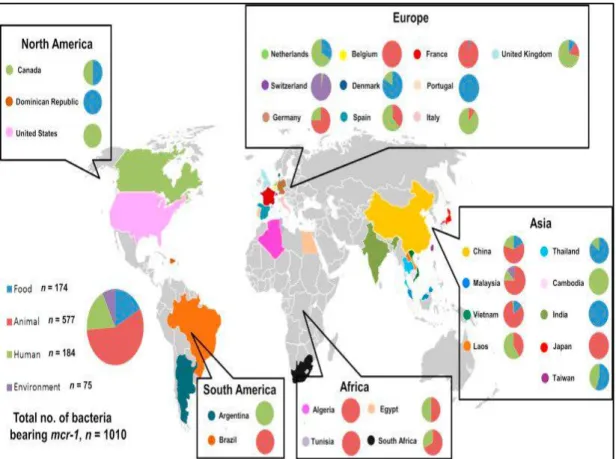
Mediterranean to countries such as Greece, where the situation is currently endemic (Giakkoupi et al., 2011). From China, a plasmid carrying the colistin resistance gene, mcr-1, was identified from Enterobacteriaceae in November 2015 (Liu et al., 2016). Four more alleles of the mcr gene have since been described (Xavier et al., 2016), mostly from sporadic cases.
Carbapenem Resistant Enterobacteriaceae in the Arabian
In the region, there is a characteristic controversy between the level of the curative segment of local health systems and the level of control over antibiotics and, to some extent, control over antimicrobial drugs. The biggest difference between countries on the peninsula and western countries with a similar level of clinical medicine is the antimicrobial control systems, which are quite underdeveloped in the region. The first publicly available data appeared in the Communicable Disease Bulletin of HAAD 1st quarter summary report (HAAD, 2017).
The effectiveness of this call as it has affected the subject of this thesis will be discussed in the Results section of this thesis. The only exception to this trend was a temporary increase in the number of VIM-positive strains in Kuwait (Jamal et al., 2013; Sonnevend et al., 2015). As for colcitin resistance in the region, surveillance data generated by the microdilution method is completely lacking.
The only study that compared the results of different regional countries using the E-test method showed that colistin resistance among CRE was 4.1%, the highest in KSA (7.5%) (Sonnevend et al., 2015). Of note, small-scale outbreak-causing omniresistant strains with insertionally inactivated mgrB leading to colistin resistance have been described in the UAE (Sonnevend et al., 2017). To date, no comprehensive study has addressed the issue of mobile colistin resistance in the region, although the gene has been detected in the UAE, Bahrain and KSA, including CRE isolates (Sonnevend et al., 2016).
Recently, the mcr-1 gene was also detected in an isolate from Oman, (Mohsin et al., 2017) and in the faecal culture of pilgrims returning from Hajj (Leangapichart et al., 2016).
Aims and Objectives
Long Term Aims
Specific Objectives
Materials and Methods
- Strain Collection
- Antibiotic Susceptibility Testing
- Genotyping of the Strains by PCR
- Extraction of Bacterial Genomic DNA for PCR
- PCR
- Determination of Carbapenemase Production
- Molecular Typing of the Strains
- Macrorestriction Analysis of the Genome by Pulsed
- Multi Locus Sequence Typing (MLST)
- Identification of the Clones
- Sequencing
- Statistical Analysis
- Ethical Considerations
Interpretation of the test results was also performed according to the same standards, except for colistin, for which no breakpoint values are currently available in this system. The minimum inhibitory concentration (MIC) of the drug was determined as the lowest concentration that prevented visible growth of the test organism. One μl of this suspension was delivered by the multipoint inoculator, i.e. approx. 104 CFU/spot were inoculated.
To group strains according to their level of resistance, the following arbitrary categories were used: Pan-drug resistant (PDR): not susceptible to any of the antibiotics tested; Extremely drug resistant (XDR): susceptible to only one antibiotic or multiple antibiotics of the same class. To determine the alleles of the respective bla genes, they were amplified and sequenced using the primers shown in Table 9. Carbapenemase production of strains not carrying any of the carbapenemase genes tested was assessed by the CarbaNP assay, as described ( Nordmann et al., 2012 ).
500 μl bacterial suspensions, 25 μl proteinase K (Invitrogen) (20 mg/ml) and 525 μl 1% plug agarose were combined, mixed and transferred to 1 ml syringes and stored for 15–30 min at room temperature to allow solidification of the agarose. After digestion, the restriction mixtures were removed and the plugs were incubated in 250 μl of 0.5X TBE buffer for 30 min at room temperature. Sequencing was performed using Big Dye Cycle Terminator V.3.1 (Applied Biosystems, USA) according to the manufacturer's instructions.
No samples were taken for the sake of the study, but only according to clinical indications.
Results
Characteristics of the Collection
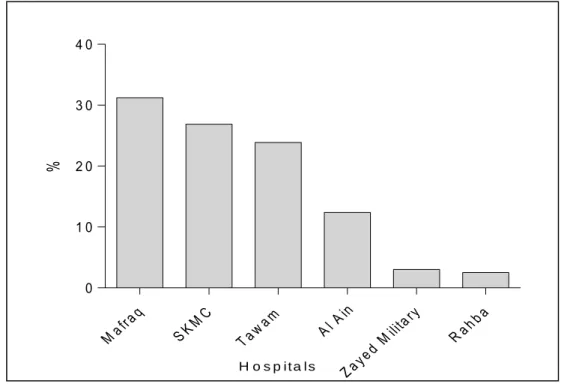
According to their sizes and coverage areas, the majority of isolates were received from four major hospitals, viz. almost 80% of the strains isolated from known sample types were obtained from clinical samples, while the rest were from screening samples taken to detect the intestinal carrier (rectal and perianal samples). We did not know whether these screening samples were collected from patients or from healthy contacts.
Antibiotic Resistance of the Strains
- Mechanism of Carbapenem Resistance
- Impact of the Mechanism of Carbapenem Resistance on
- Aminoglycoside Resistance
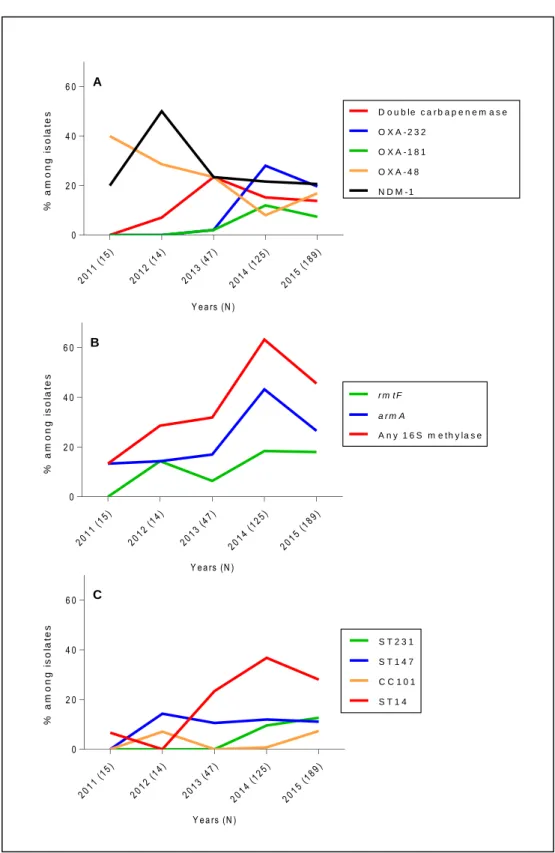
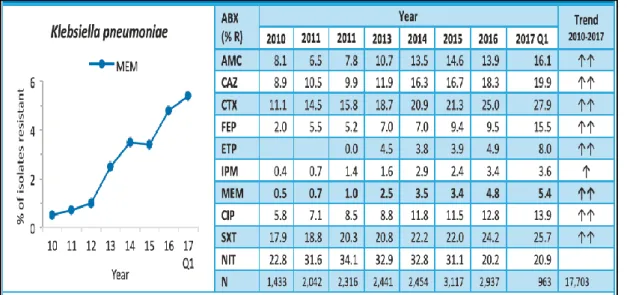
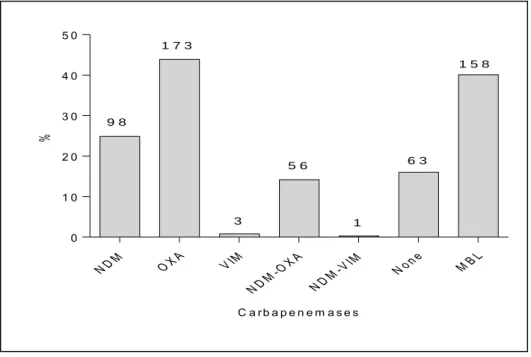
The mechanism of carbapenem resistance in the collection of CRE isolates was determined by PCR-targeting the genes of the five most common carbapenemases, i.e. Regarding the distribution of carbapenemase alleles, among NDM-producing strains only, the NDM-1 allele was the most common (88%) followed by NDM-5 and single isolates of NDM-4 and NDM-7. Of the carbapenems tested, nonsusceptibility to ertapenem was 100%, regardless of the mechanism of carbapenem resistance.
While ertapenem had a uniformly high MIC50 against strains producing one of the alleles, this high MIC was most uniform against OXA-232 producers. Among OXA-48-like carbapenemase producers, some alleles were present in sufficient numbers to allow for comparable comparison (Figure 19). Overall, well over a third of strains fall into the category in which meropenem treatment may still be an option, i.e.
The degree of insensitivity to gentamicin and amikacin, as shown in the table of isolates, showed non-susceptibility to both drugs. Of the strains that showed non-sensitivity to both aminoglycosides, at least one contained a gene encoding a 16S-methylating enzyme. The distribution of the 16S methylase genes was uneven between the groups with different carbapenem resistance mechanisms.
As shown in Table 18, the frequency of the presence of a 16S methylase gene was much lower among CRE without a carbapenemase than among those producing such an enzyme (P<0.0001).
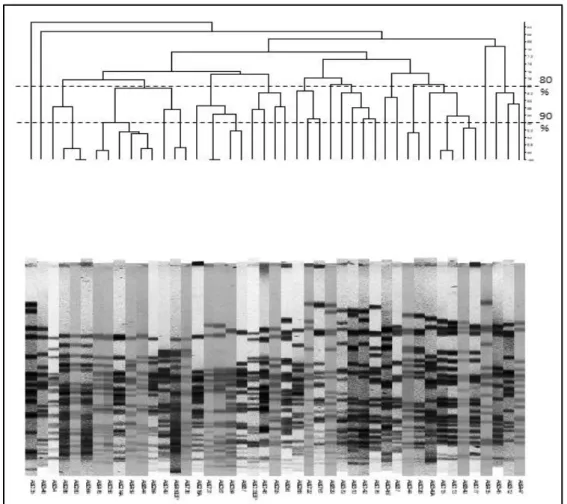
The Clonality of the Strains
Next, we investigated whether any characteristics of the strains could be associated with any of these clones. Over 80% of the strains from Al Ain hospital belonged to this clone and it was also the dominant clone in Zayed Military Hospital and SKMC. About a third of the members of the ST14 clone also carried the gene of this oxacillinase, but among them the expression of NDM-1 as well as the co-expression of these two enzymes were equally common.
93 Table 22: Relationship of the MIC levels of carbapenems with the alleles of OXA-48-like carbapenemases. Alarmingly, while in the case of meropenem, these options were still present for more than half of the sporadic isolates, they were available for a much lower rate of isolates in the four main clones (Table 23). Certain other resistance-related features were also more common among some of the clones than among sporadic isolates.
It should be noted, however, that some of the smaller clones and even one of the larger ones (ST101) did not show high rates in resistance-related numbers (Table 24). While the production of 16S methylases was a common feature among strains belonging to some of the clones (Table 24), the type produced was unevenly distributed (Table 25). As can be seen, while some of the clones did not carry any 16S methylase genes (e.g. ST11, ST45, ST101), others either carried multiple (ST15, CC147) or were characterized by a single type (armA in the case of the largest clone, ST14) present in almost 80% of the members of this clone.
Due to their size and the level of resistance exhibited by most clones, their impact on the rate of some resistance-related functions in the entire collection exceeded their numerical proportion.
The Emergence of CRE and the Change of the Rates of their
34;Biochemical and genetic characterization of carbapenem-hydrolyzing beta-lactamase OXA-229 from Acinetobacter bereziniae." Antimicrob Agents Chemother. 34;Impact of the ST101 clone on mortality among patients with colistin-resistant Klebseiella pneumonia infection." J Antimicrob Chemother. 34;First characterization of heterogeneous resistance to imipenem in invasive nontypeable Haemophilus influenzae isolates.” Antimicrob Agents Chemother.
34;Plasmid-mediated spread of the blaIMP metallo-beta-lactamase gene among clinically isolated strains of Serratia marcescens." Antimicrobials Chemother. 34;Carbapenem activities against Pseudomonas aeruginosa: respective contributions of OprD and efflux systems." Chemother Antimicrobials. 34; Risk factors for the acquisition of imipenem-resistant Acinetobacter baumannii: a case-control study.” Antimicrobials Chemother.
34;Biochemical properties of a carbapenem-hydrolyzing beta-lactamase from Enterobacter cloacae and cloning of the gene into Escherichia coli." Antimicrob Agents Chemother. 34;Penicillin-binding proteins of Rhodococcus equi: potential role in resistance to imipenem." Antimicrobial agents Chemother. 34; Characterization of NDM-7 carbapenemase-producing Escherichia coli isolates in the Arabian Peninsula.” Microb Drug Resist.
34;New variant VIM metallo-beta-lactamase from clinical isolates of Enterobacteriaceae from Algeria." Antimicrob Agents Chemother. 34;Dominance of IMP-4-producing enterobacter cloacae among carbapenemase-producing Enterobacteriaceae in Australia." Antimicrobial Agents Chemother. 34; Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae.” Antimicrob Agents Chemother.