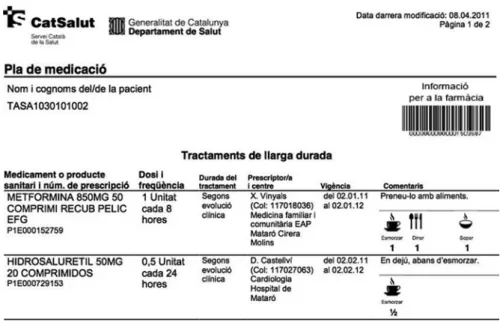
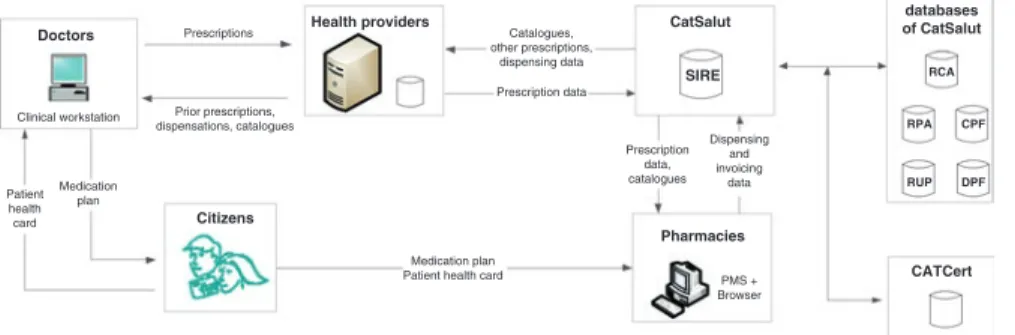
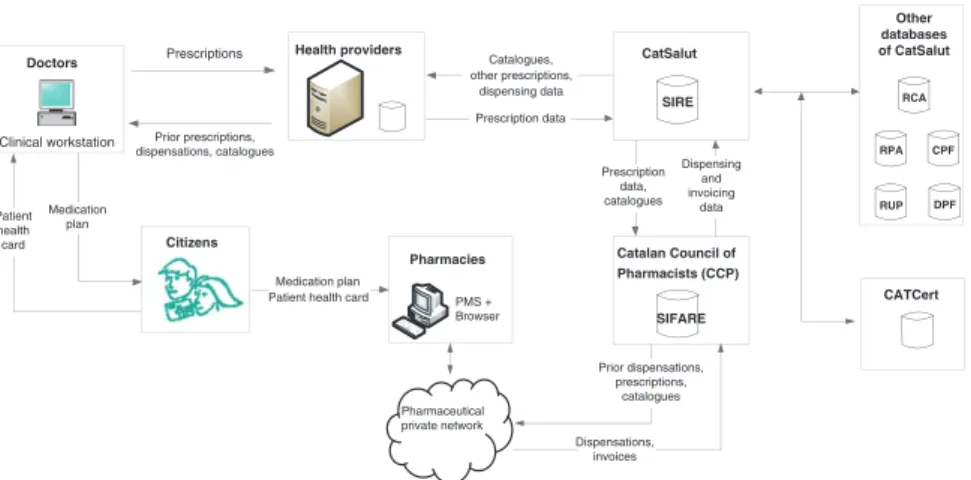
A CCP vice president linked the pharmacy model to the VPN in the following terms: “We are a network [the pharmacy model in Catalonia] that needs a network [the VPN]. So after some negotiations, the CatSalut bowed to the interests of the CCP and the pharmacists, and accepted the CCP's model in May 2005.
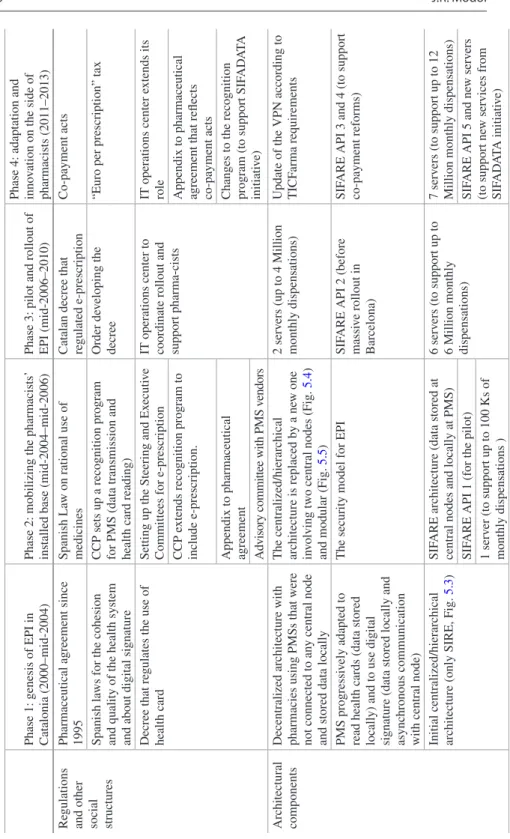
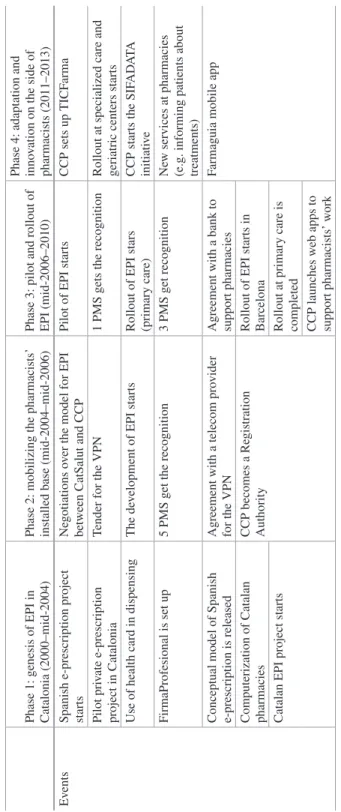
Phase 3: Pilot and Rollout of EPI (Mid-2006–2010)
A major concern for the CCP was the cost of the technical infrastructure for the CCP and pharmacists. Similarly, in 2008, the CCP received a grant from the Catalan government's Center for Innovation and Development.
Phase 4: Adaptation and Innovation on the Side of Pharmacists (2011–2013)
The rationale for these services was consistent with CCP's vision of the EPI model. Therefore, PMS vendors became key players in CCP's new professional services strategy.
Analysis and Discussion
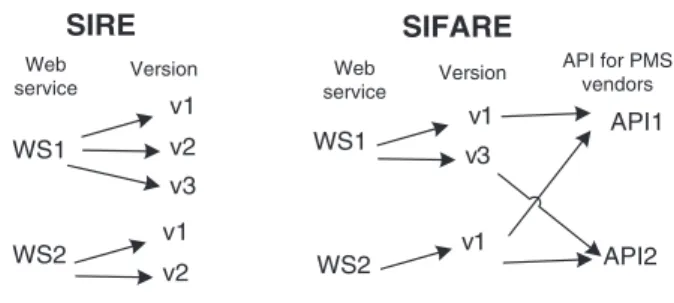
At the same time, KPK increased the use of SIFARE and VPN and strengthened its role as a service provider for pharmacists. CCP has found that to implement these professional services, the agreement and cooperation of PMS vendors is much more critical.
The ePrescription Initiative and Information Infrastructure
- Introduction
- The Norwegian Health Care Sector
- Case Narrative
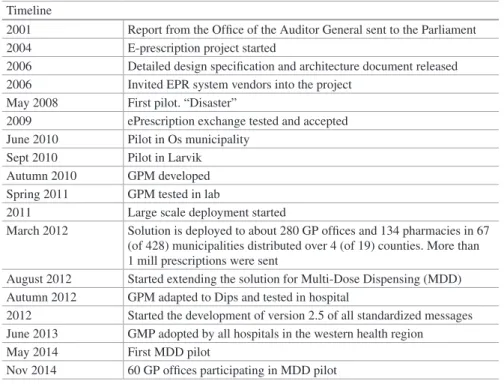
- Establishment and Diffusion of a Solution for GPs
- The Hospital Sector
- Adding Multi-dose Dispensing
- Other Developments
- Operations and Governance
- Concluding Discussion: Installed Base Strategy
This is true for both existing applications and the platforms (PC hardware, operating system, network technologies, etc.) on which the applications ran. The new version of the messaging standards is implemented first in the PE and GP modules.
Cultivating the Installed Base
The Introduction of e-Prescription in Greece
- Introduction
- Healthcare in Greece
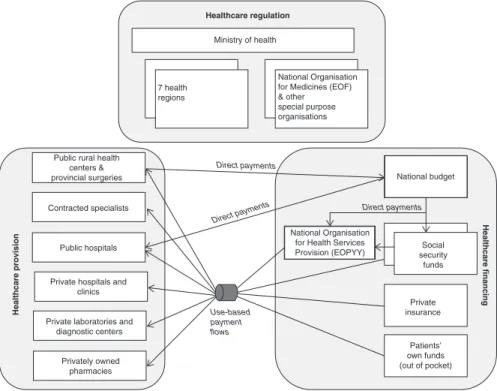
- Overview of the Greek Healthcare System
- Information Systems in Greek Healthcare
- The Introduction of E-Prescription
- Rationale for E-Prescription and Key Milestones
- Information Handling Before the Introduction of E-Prescription
- Information Handling After the Introduction of E-Prescription
- System Evolution
- Discussion: Relationship to the Installed Base
- Building Upon an Installed Base That Is “Good Enough”
- Handling Continuous Exogenous Shifts in the Installed Base
- Installed Base Cultivation vs. Specifications-Driven Development
- Concluding Remarks
Developing a better understanding of the e-prescription solution: On-site observations of e-prescription use in pharmacies. In the following paragraphs we present the process followed, starting with a brief presentation of the situation before the introduction of the new electronic service. For example, in 2005 IKA (the largest social security fund) conceptualized a project for the electronic processing of the white prescription pages received.
For testing the service, almost all pharmacists were enrolled along with doctors contracted by the specific fund (see also Table 7.1). Nevertheless, since smart health cards are part of the national plan, the introduction of e-prescription was linked to the use of the cards and this was clearly indicated when the consultation process for the development of the new electronic prescription services was initiated back in 2010 (the use of PKI-based smart cards was part of the requirements). Gaps in the backbone of the country's information infrastructure caused difficulties for previous e-health initiatives.
These were key characteristics of the new version of the system developed and launched in 2012. The introduction of the new electronic service was legitimized by referring to the expected economic impact (Greek e-Government Center for Social Security 2011; Sfyroeras 2012a; Vassilakopoulou and Marmaras 2015) and commitments to the International Monetary Fund and European institutions.
England’s Electronic Prescription Service
- Introduction
- Primary Care and Health Informatics in England
- Prescribing, Dispensing and Reimbursing Primary Care Drugs
- Computers in English Primary Care
- Early ETP Experiments and Pilots
- Assembling the Electronic Prescription Service
- Transforming the Prescription
- Architecture
- Release Strategy and Deployment
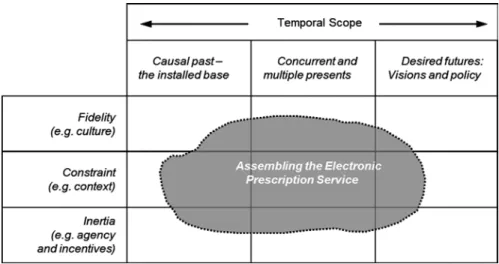
- Assembling EPS as Past, Present and Future
- The Physical and Material in a Digital World
- The Reinvention of Services
- Ruthless Standardization
- What Can the Electronic Prescription Service Teach Us?
The advent of the personal computer in the 1980s, schemes to support the adoption of primary care computers such as the Micros for GPs scheme (Project Evaluation Group 1985), and a reorganization which emphasized the documentation of care provision as well as experiments in GP fund holding , led to the development of computing practices in all seriousness with many providers entering the market (Brennan 2005; Hayes 2008). Computerization of the NHS in the 1980s and 1990s inspired two in-vivo ETP experiments prior to the development of EPS. The right side of the FP10 is a tear-off reorder form for use by the patient.
Prescriptions are provided in the same way as an acute prescription, with the addition of a check by the public pharmacist on the use of the medicine by the patient. The pharmacy team can retrieve the electronic copy of the prescription by scanning the barcode on the paper prescription. The evaluation of the electronic prescription service in primary care: final report on the findings of the evaluation at early implementation sites.
The proposals to include schedule 2 and 3 controlled substances within the scope of the electronic prescribing service: consultation document. Evaluating the electronic prescribing service in primary care: interim report on the findings of the evaluation in early implementer sites.
The Challenges of Implementing
Institute for the Study of Science, Technology and Innovation, The University of Edinburgh, Yards High School, Edinburgh, UK, EH1 1LZ. Center for Medical Informatics, The University of Edinburgh, Door number 3, Teviot Place, Edinburgh, UK, EH8 9AG.
Packaged Hospital Electronic Prescribing and Medicine Administration Systems
Introduction
- The UK Context for Hospital Electronic Infrastructures
Stakeholders managing health systems in many countries have invested significant efforts to implement and deploy electronic or ePrescribing systems (Mozaffar et al. 2014; Cresswell et al. 2013) to support prescribing decisions in health care organizations (Aarts and Koppel 2009; Bates et al. 1998). With over a million employees, the NHS is an unusually large and complex organization (Hibberd et al. 2016). NHS calls to improve the quality, safety and efficiency of healthcare, combined with significant financial support, have generated widespread interest in the timely implementation of HEPMA systems in UK hospitals (Buntin et al.
The move towards local selection of systems has resulted in hospitals being faced with a range of options, none of which however are currently perceived as fully meeting the needs of the English market (Mozaffar et al. 2014). While the first generation of HEPMA systems were developed within hospitals, today we see a marked shift from home-grown solutions to 'packaged' COTS software (Mozaffar et al. 2014). These include the very significant costs associated with developing and maintaining bespoke systems (and the stalled progress and anticipated failure of a major project to jointly develop an integrated solution within/for English hospitals1), the perceived advantages of the solutions packaged (in terms of functionality/price, reliability, maintainability) and problems with limited interoperability between providers (Schiff et al. 2003; Westbrook et al. 2012).
Despite these investments, the HEPMA market in England faces a great deal of uncertainty and is undergoing rapid change and development (Aarts and Koppel 2009; Mozaffar et al. 2014). These factors all contribute to the challenges hospitals face in acquiring, implementing and realizing the benefits of these systems (Wolfstadt et al.
Understanding the Uneven Success of HEPMA
- How HEPMA Systems Are Constituted: Extension of Non- clinical Systems
- Adoption of Systems That Had Been Developed Outside England
- Suppliers’ Configuration and Customization Strategies
- Localized Adopter Practices Versus Generic Systems
In particular, in the process of scaling up the systems, suppliers seemed to underestimate the complexity of HEPMA as a clinical system and the specificity of user activities (a mistake that closely mirrored criticisms of early EC offerings two decades earlier). Some vendors appeared unwilling to invest the significant resources required to implement these changes, particularly where they had little presence in the English market. However, at the time of the study only a handful of hospitals had implemented their system, most of these systems were in the early stages of "anglicization".
And basically where we started were certain items that we knew, we knew would be different, like in the UK. This required them to develop a strategic vision for their software product and its long-term evolution, to maintain control over the overall architecture of their product as it moved forward, despite many requests from adopters. In the case of HEPMA systems in England, suppliers followed different product development strategies but made very uneven progress in developing their strategies.
However, their responses highlight the lack of adequate awareness among users of the needs of packaged applications and in particular the trade-off between the costs of customization versus adapting processes to the functionality in the package. So the companies I've worked for before have always had […] a user who partly worked at the Trust [hospital] and partly worked for them [the selling company] so they're an actual user.
Discussion
- Analysing the Long-Term Evolution of Information Infrastructure
- Analysing the State of the Technology Market/Technology Field
- Is the HEPMA Market Replicating the Path of ERP?
- The English HEPMA Market Is Still in an Emergence Stage The comparison with the ES case suggests that the HEPMA market in England is
- Conclusions
In the mature phase, as dominant designs become established, we find concentration of the market around a smaller number of higher performance products. Our study of the development of the HEPMA market in England shows some interesting and insightful parallels with the earlier history of integrated systems in the commercial sector: ERP and its predecessor CAPM Systems. Suppliers had taken different approaches to meet the different needs of the UK market.
However, England is one of the leading countries with the highest rates of HEPMA adoption (Aarts and Koppel 2009; Behnaz Schofield (Research Fellow, The University of Edinburgh), Prof Richard Lilford (Professor of Clinical Epidemiology, The University of Birmingham), Dr. It also draws important historical insights from two grants from the Economic and Social Research Council: a grant awarded to Neil Pollock 'The Social Study of the Information Technology Marketplace(s)' (RES as well as an earlier research grant to Williams, Pollock and Procter (RES on 'The biography and evolution of standardized software packages'.
Benefits of health information technology: A review of recent literature shows overwhelmingly positive results. Development of the market for commercial computerized physician orders and computerized decision support systems for prescribing.
Medication Infrastructure Development in Germany
- Introduction
- One Step Forward Two Steps Back
- Case Background
- Medication Management for Polypharmacy Patients
- Automatic Dose Dispensing (ADD) as a Key Component for Medication Management
- Attempted Infrastructure Innovation
- Case Presentation
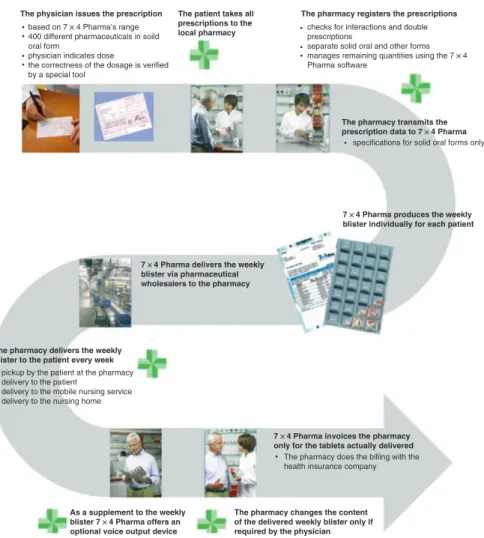
- From Semi-automated Packaging to Industrial Scale ADD In 2000 the first care homes in Germany started to introduce patient-specific blis-
- The Design of the ADD Pilot Infrastructure
- Debates About ADD in Germany
- Status in 2016: Slow Diffusion and Persistent Opposition About 7,5 Mio patients in Germany take five or more medication regularly
- Analysis
- Deficiencies in Installed Base
- An “Installed Base of Opposition”
- Discussion
- Appendix: List of Acronyms
This explanation does not bode well for the government's latest attempt to accelerate the digital transformation of the German healthcare sector. Pharmacists and blister center managers have been lobbying for several years for the official recognition of the advantages of blistering, that is, that the pharmacy changes the contents of the delivered weekly blister only at the request of the doctor as an attachment to the weekly.
The design of the pilot study and the research based on the pilot (Leker and Kehrel 2011) were in accordance with the principles of performance assessment as formulated by G-BA4 and the regulation on pilot projects in the healthcare system SGB V). 4 For more information on the mandate of the G-BA: http://www.english.g-ba.de/legalmandate/. As such, the study would not qualify as evidence under the standards of the Federal Joint Committee (G-BA).
The governance structure of the German healthcare system is based on cooperative consensus building and decision-making prior to regulation. The Federal Joint Committee (G-BA) is the decision-making body of the joint board of doctors, dentists, hospitals and health insurers in Germany (www.english.g-ba.de).