ABSTRACT Primary Health Care (PHC) is a basic mechanism that brings health care closer to people. Integrating mental health care into its package of services aims to close the treatment gap.
Introduction
Background to the study
The study was the first large-scale descriptive epidemiological study of mental health in SA. Currently, PHC nurses working with mental health care users (MHCUs) are reported to experience problems related to poor infrastructure.
Problem statement
Purpose of the study
Significance of the study
Thus, it is suggested that increased knowledge and understanding of PHC nurses' experiences of this integration and provision of mental health care services in PHC clinics is pertinent to inform policy implementation. However, PHC nurses' experiences of implementing the integration process and providing mental health care services within a PHC setting have not been extensively explored.
Research Objectives
Participants highlighted some fundamental health benefits of integrating mental health care into PZC clinics. What has been your experience with integrating mental health care into this clinic?
Reseach Questions
Operational definitions
Primary Health Care Clinic: For the purpose of this study, a PHC clinic is any clinic that is included in the list of PHC clinics of the EThekwini District Health Care Office (EThekwini District Health Department, 2012). Primary Health Care Nurse: For the purpose of this study, a PHC nurse is any nurse registered with the PHC as a registered general nurse and currently employed in one of the PHC clinics in EThekwini District.
Conceptual Framework and its application to this study
Mental health services: For the purpose of this study, mental health services include all services provided to a mental health service user (MHCU), identified in the Mental Health Act No. 17, of 2002, in a PHC clinic setting . Donabedian argues that less than effective service delivery may be the result of a lack of structure or process standards (Donabedian, 1998).
Summary of the chapter
Introduction
Mental illness, its prevalence and burden
Herman et al., (2009) maintain that mental health is still considered a luxury despite WHO's continued commitment to prioritizing mental health, specifically in low- and low- to middle-income countries. This organization emphasizes that mental health is increasingly viewed as a critical foundation for both physical health and quality of life (Mkhize & Kometsi, 2008; WHO, 2011).
The evolution of PHC
In the health sector this involved the complete transformation of the national health care delivery system and all relevant institutions. Legislation and health-related organizations were revised to bring about transformation within the health care system.
Mental health care integration into PHC
Historically, mental health care in the 1970s was based on institutionalized care, which violated the rights of MHCUs (WHO & UNICEF, 1978). This lack of focus is clearly potentially problematic for community health care (WHO, 2001b).
Current local initiatives for mental health integration
The Psychiatry Act (17 of 2002) was a milestone for change in psychiatry. Psychiatry still receives a modest budget, which is a clear indication that patients with mental illness are not a high priority.
The nurses’ role in the integration of mental health into PHC
In addition, each monthly visit includes assessment by the PHC nurse and, if necessary, cases are referred to the mental health nurse with an accompanying form indicating the reasons for referral and the support required (WHO, 2006). However, nurses have limited information regarding the management of the MHCUs during hospitalization when they are discharged and referred back to the clinics (Petersen, et al., 2009).
Summary of the chapter
The current referral process includes existing and new cases and PHC nurses provide routine follow-up medication to patients with stabilized chronic psychiatric conditions as part of their service (WHO, 2007). As part of their daily routine, PHC nurses transfer patients to regional hospitals for further treatment of psychiatric conditions (Lund & Flisher, 2007).
Introduction
Philosophical underpinnings
Research design
A limitation of the study was that the findings represent the views of a relatively small sample of nurses working in the PHC clinics following the integration of mental health care within the PHC setting. Implementation of the Mental Health Care Act (2002) in district hospitals in South Africa, putting principles into practice.
Research Setting
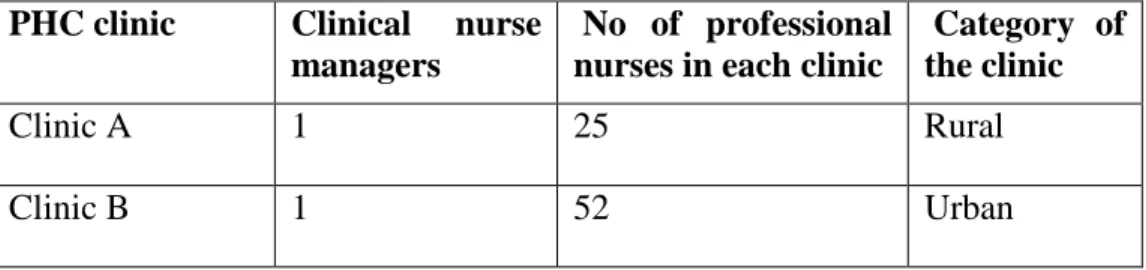
Description of the selected clinics
Clinic A has 25 professional nurses who manage all patients who come to the clinic. However, MHCUs who are actively psychotic are referred from the clinic to the district hospital assigned to its catchment area.
Population and target population
The clinic has a small psychiatric ward where the MHCUs get their repeat medication, but all patients are monitored by the professional nurses.
Sample and Sampling procedures
Participants had to be registered nurses who were employed full-time at the PHC clinics. They had to have a minimum of 2 years working with the MHCUs in the PHC clinic and be available on the day of data collection.
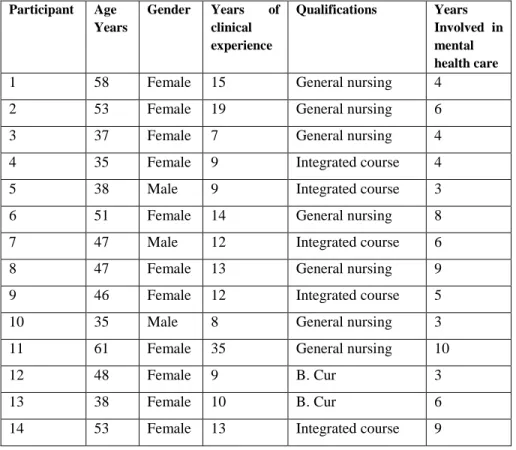
Description of the participants
These include the age and gender of the participants, which clinic they work in, their level of experience in the clinical field, their qualifications and the number of years they have been involved with the MHCU. Their level of experience in general nursing ranged from 7 to 35 years and their involvement in MHCUs ranged from 3 to 10 years.
Positioning of the researcher
Interview schedule and data collection
Data collection, which is explained in detail under the data collection process below, continued past the point of saturation of information, that is when no new data was obtained and there was repetition of data (Polit & Beck, 2008. The reason why the researcher continued to the point of saturation point with the interviews was a result of participants'.
Data Collection process
As described in the data collection process (section 3.9, p. 29), it had been communicated within the participating clinics that the researcher was in the process of collecting data and the nurses were excited to participate. The process of data collection was explained, including the use of the tape recorder to capture information.
Data analysis
The researcher generated codes by organizing all the data into meaningful groups without losing any valuable information. The sixth and final step that the researcher undertakes is to prepare the report, which should include a selection of substantial excerpts from the data to illustrate the presentation and analysis of the data.
Trustworthiness and academic rigor of the study
The researcher ensured credibility or confidence in the “truth” of the data collected by ensuring that the research data was presented accurately (Holloway & Wheeler, 2003). Confirmability was compared to objectivity or neutrality (Tobin & Begley, 2004) and was referred to as the objectivity of the data.
Ethical considerations
Participants' right to full disclosure was addressed by providing an information sheet that outlined the purpose of the study, the data collection process, and the dissemination of information from the study (Appendix D, page 72). During data analysis, only the researcher and the research supervisor had access to the raw data.
Data management
After transcription was complete, the audio recordings were deleted, and electronic copies of the transcribed data were securely stored on the researcher's personal computer, which was password protected (Burns & Grove, 2009).
Dissemination of findings
Summary of the chapter
Introduction
Data analysis process
In preparation for the meeting to discuss the emerging themes, the research supervisor had been given a copy of the raw data. The report presents each theme and a table included to illustrate the categories and subcategories that were identified and led to the definition and naming of the theme.
Presentation of results
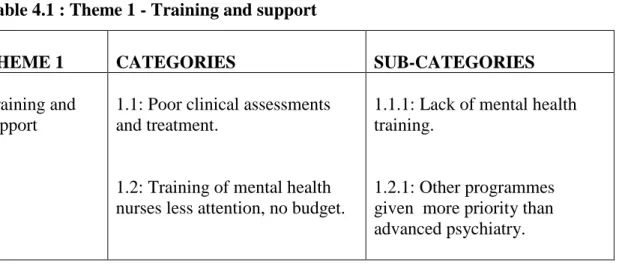
- Theme 1: Training and support
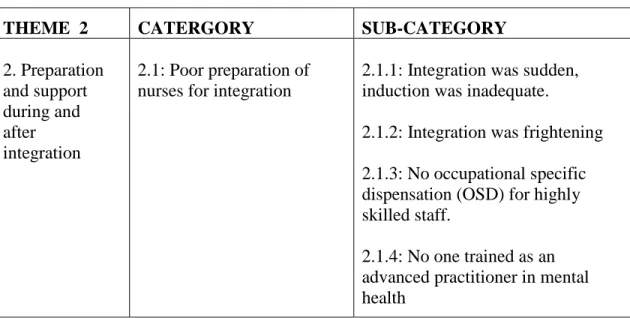
- Theme 2: Preparation for integration
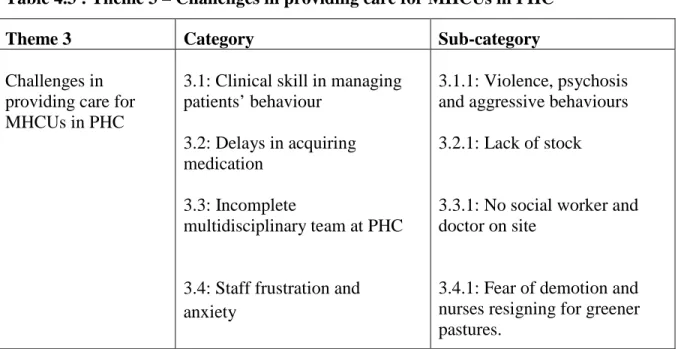
- Theme 3: Challenges in rendering care to MHCUs in PHC
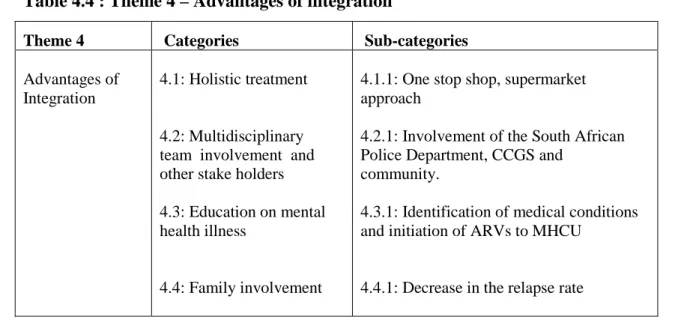
- Theme 4: Advantages of Integration
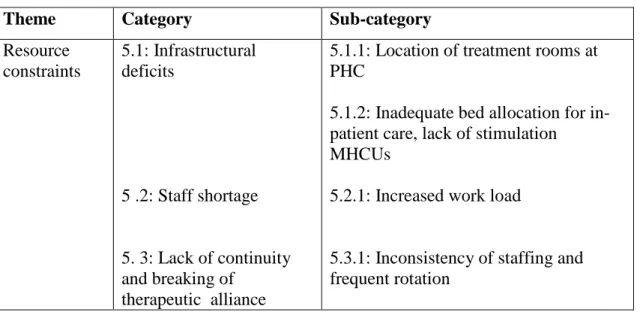
- Theme 5: Resource constraints
Participants indicated that there were some challenges in providing care to mental health service users within the PHC setting, especially with. Participants reported that the majority of PHC nurses were not adequately trained to provide all the services that would need to be provided in the clinics once mental health care was incorporated into the PHCs.
Summary of the chapter
Another problem is that once the MHCU is admitted to the hospital, we never get feedback from the nurses and doctors in the hospital about what happened in the hospital and what was done." From the sample of fourteen PGS nurses in the study, the overall integration of mental health care in PHC was considered beneficial, despite ongoing problems, as it not only improved the quality of the health care system, but also the utilization of PHC institution.
Introduction
Discussion
- Inadequate preparation for initial integration
- Inadequate preparation for ongoing provision of metal health care
- Voluntary counselling and initiation of HAART to MHCUs
However, the preparation for the ongoing integration process and the support of the PHC nurses in providing ongoing care to the MHCUs were reported as inadequate. Participants shared the information about voluntary counseling and initiation of Anti-Retro Viral (ARV) medications with the MHCUs, indicating a different attitude and practice than reported in Jarvis and Smith (2014, in print).
Limitations the study
Two unique findings emerged from this study; support for integration and recognition that MHCUs benefit from HIV/AIDS screening and counseling offered to all patients who attend and may need counseling and screening by PHC clinics. Local research suggests that the PHC setting has been recognized as a setting for voluntary counseling and treatment (VCT) of HIV/AIDS (Jarvis & Smith, 2014 in press).
Recommendations
- Development and support
- Participation in planning
This will reduce uncertainty and fear in the treatment of the MHCUs, while giving the PHCNs the confidence to identify those in need of treatment. The government is in the process of restructuring the PHC, and it is therefore important that all stakeholders at PHC level are given the opportunity to provide input, as this will contribute to the efficient handling of patients within the PHC environment.
Summary
The Durban ICC was told that the government is currently looking positively at mental health issues and intervention. These are indications that the government is trying to address the discrepancies especially for the near future.
Conclusion
Training for Transformation: Reorienting primary health care nurses for mental health care delivery in South Africa. Barriers to improving mental health care services in low- and middle-income countries.
Ethics approval from UKZN