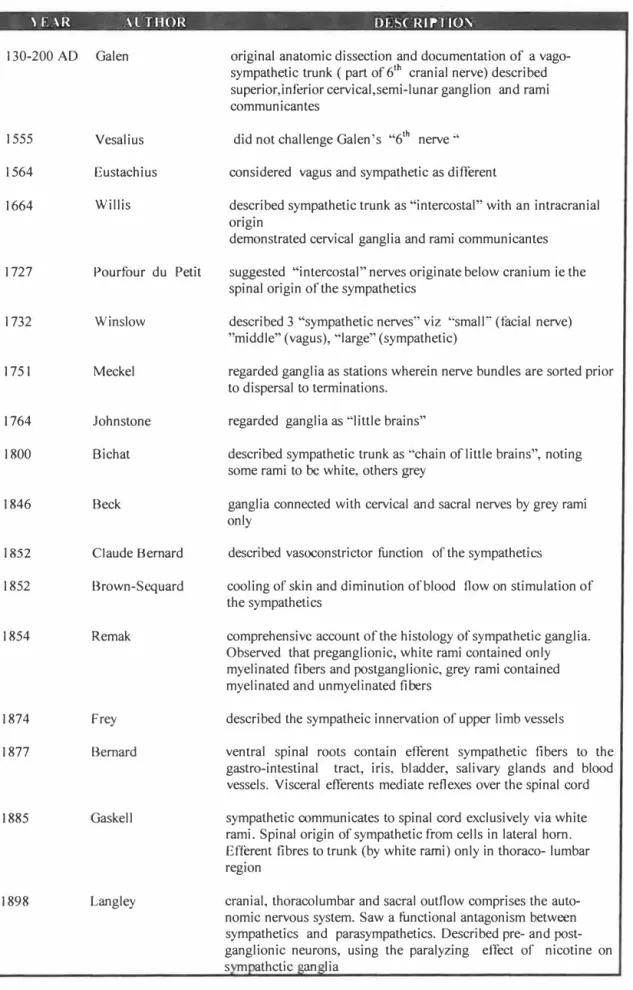
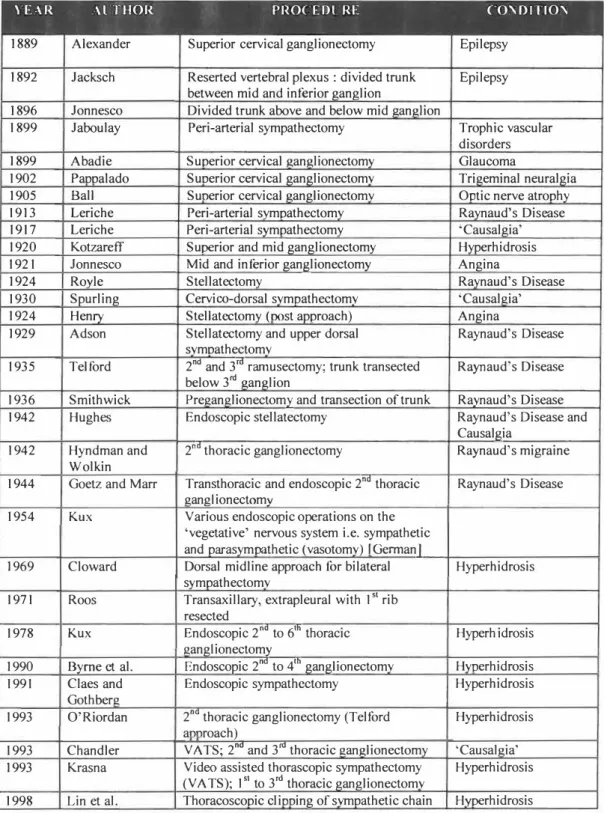
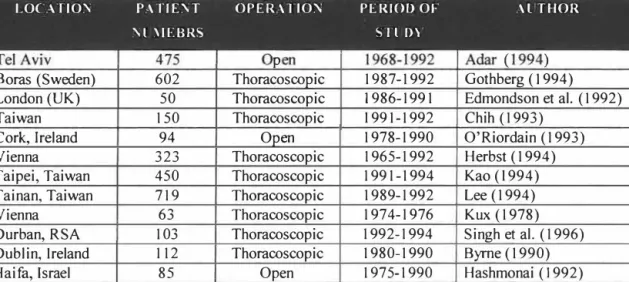
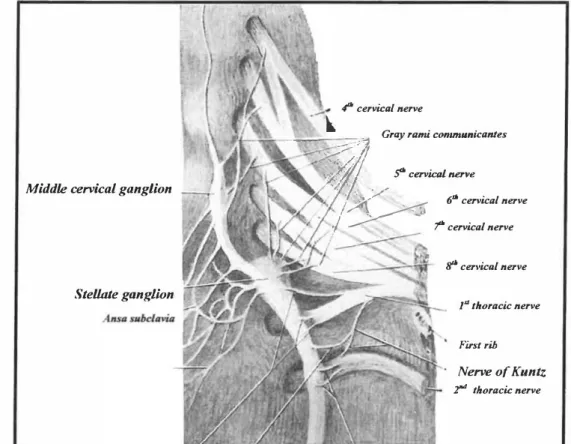
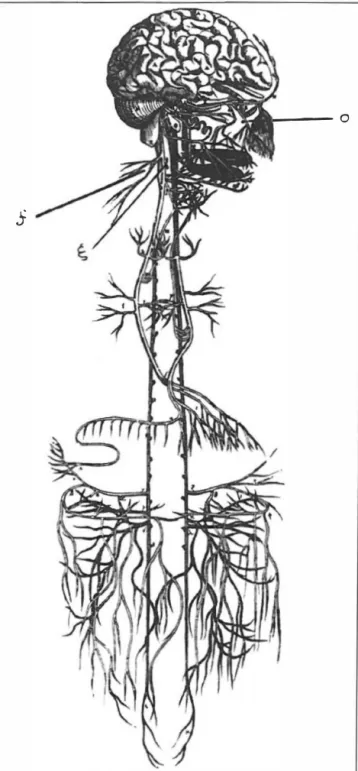
Cases of failed sympathectomy are often attributed to the anatomical arrangement of the sympathetic chain. Thoracic origin of the sympathetic supply to the brachial plexus: the "nerve of Kuntz" revisited. Pioneering surgical efforts of the sympathetic nervous system were associated with an unpredictable outcome.
Extent of ganglionectomy for upper limb sympathetic
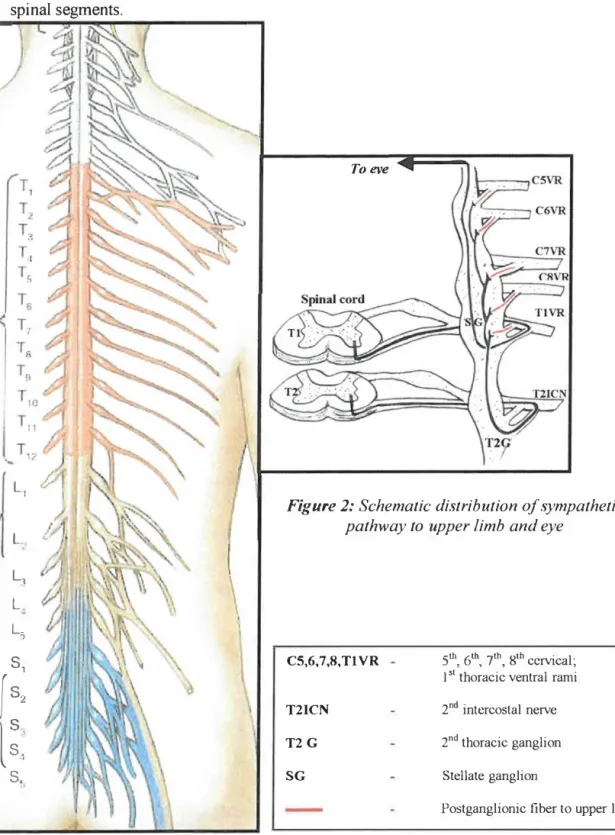
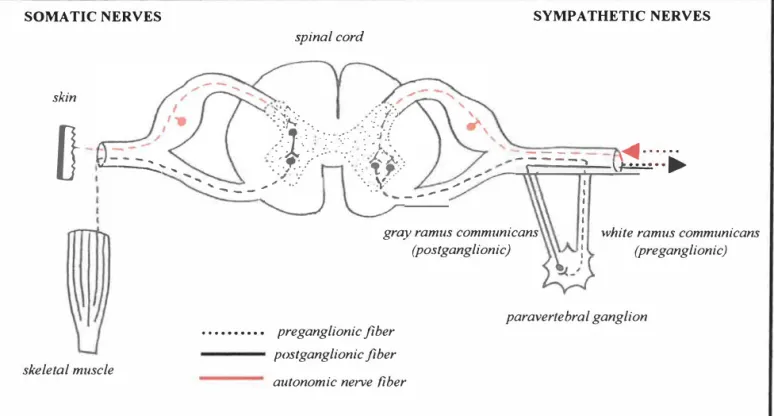
A successful (or positive) SGB in the context of CRPS is defined in our practice as the development of a transient IJorner Syndrome [with even minor, disappearing eye signs] with relief of CRPS upper limb pain. This, in itself, represents a failure to appreciate that the sympathetic pathway to the upper limb is effectively independent of the stellate ganglion. Adequate and complete treatment of precipitating mJury [event debridement, fracture mobilization, repair of associated soft tissue injury (including nerve injury) and treatment of any infection].
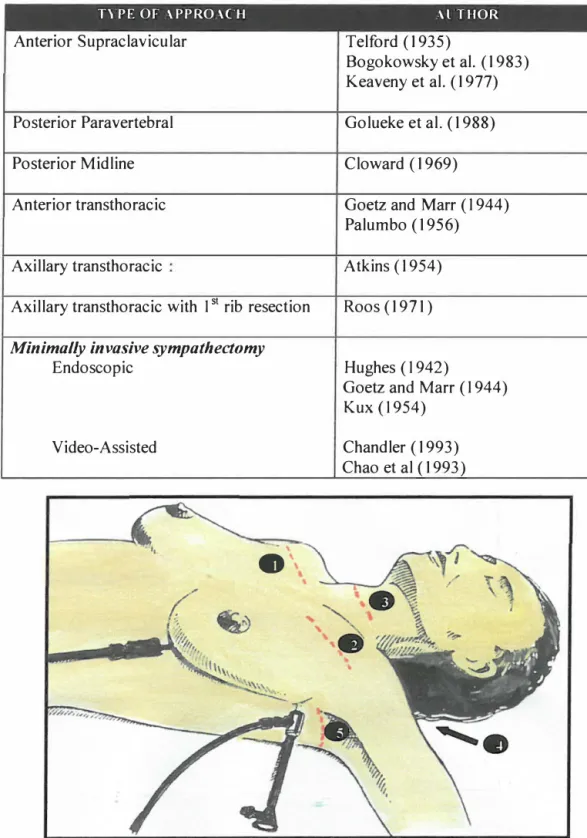
Both procedures involved excision of the second thoracic ganglion that was sent for histopathological evaluation. A midline incision is made from the lower border of the mandible to the angle of the sternum. In the 4th patient, a dense pleural reaction extending from the region of the stellate ganglion to the third rib was observed.
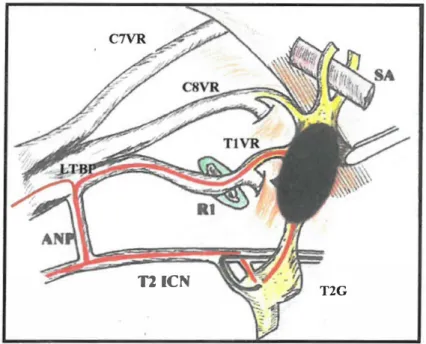
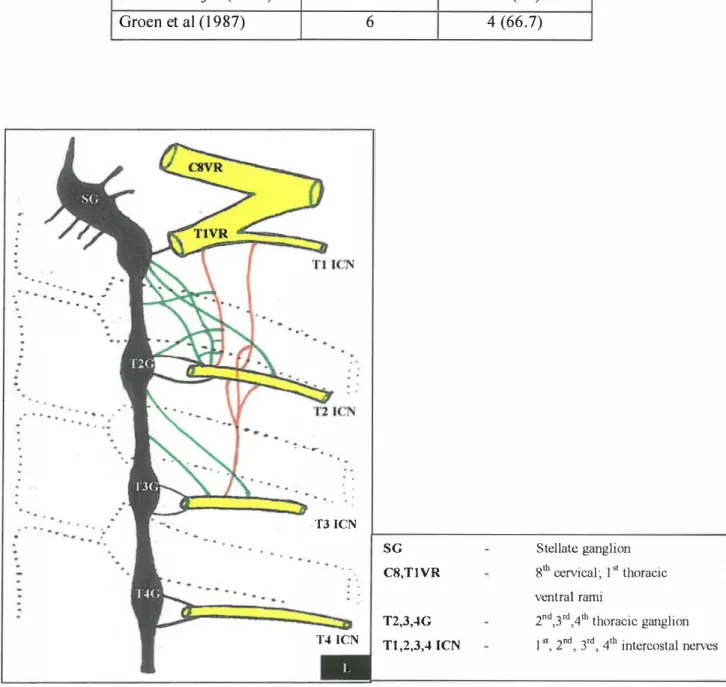
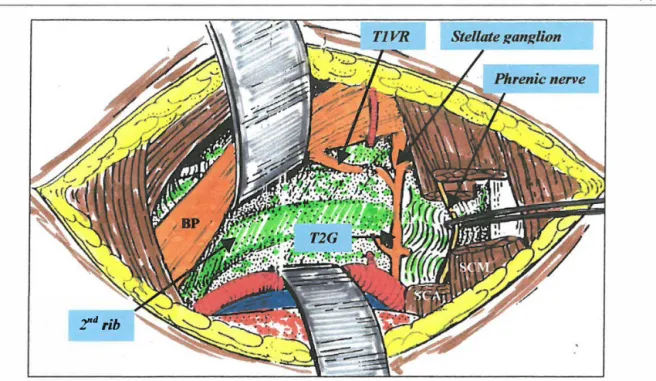
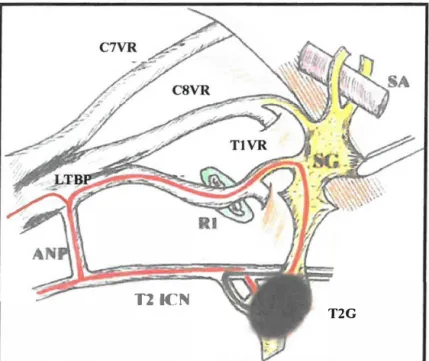
It also underscores the anatomical significance of the 2nd thoracic ganglion for upper limb sympathetic supply. In this series, 3 of the 7 patients with severe compensatory hyperhidrosis regretted having the procedure (even though their palms were now anhidrotic). If alternative neural pathways are to be defined, our technique is to begin dissection medial to the sympathetic chain in the region of the 2nd intercostal space (rather than over the 2nd rib) (Plate 24).
Further definitions of the sympathetic chain and its variations contribute to the body's knowledge of the sympathetic nervous system. Various methods have been used to test the efficacy of sympathetic blockade of the upper limb. The sympathetically mediated effects that accompany CRPS are most likely due to the inflammation of the sympathetic ganglia.
Outcome to thoracoscopic sympathectomy
Stellate ganglion block : an anatomical re-appraisal
The role of the sympathetic nervous system – both in conjunction with and subsequent to DRG pathology, has not previously been considered. The spectrum of hyperhidrosis present was further categorized as mild (1-3), moderate (4-6), or severe (7-10). The hook was then used to strip the pleura to expose the sympathetic chain up to the superior border of the third rib.
In the early period of the study, a more extensive ganglionectomy - up to the 3rd thoracic ganglion - was routinely performed. The telescoping cannula is steadily withdrawn in front of the re-expanding lung. At the initial assessment, patient demographics (age and gender) and prevalence of hyperhidrosis were recorded.
In all patients, excision of the second thoracic ganglion was performed either at thoracoscopy or open surgery. In the first patient with rSA, a video recording of the re-thoracoscopic procedure was made simultaneously. Dissection of the undissected sympathetic chain distal to the superior aspect of the 2nd rib revealed a cord-like structure associated with the stellate ganglion (Plate 14).
In the 41 sides analyzed, the 2nd thoracic ganglion was consistently located in the 2nd intercostal space in 37 dissections (90.2%), in 4 dissections (9.8%) the T2 ganglion was identified as follows: -.
Clinical perspective
- Palmar hyperhidrosis
- Chronic Regional Pain Syndrome
- Raynaud's Disease
- Peripheral Vascular Disease
The incidence of recurrent hyperhidrosis varies between 1 and 5%, occurring between 2 and 48 months after sympathectomy (Hashmonai et al., 1992). No long-term respiratory complaints were reported voluntarily by any patients in this series; Herbst et al. 1992) also did not report respiratory problems after sympathectomy. This was substantiated by Molho et al. which showed a change in pulmonary function after sympathectomy.
I994) reported in his series of 67 patients (mean age 14 years, range 5.5 to 17 years) that there was a successful outcome of transaxillary sympathectomy in all but two patients. the reported successful outcome of open sympathectomy in children, should thoracoscopic sympathectomy be offered more widely in this population. The latter include oral agents (phenoxybenzamine) and transdermal agents (clonidine) (Byas. Smith et al., 1995). Furthermore, if performed in the early or acute phase, the procedure itself may prove to be therapeutic (Mokus et al., 1987; Abu Rahma et al., 1994).
Contrary to the experience of others (Mockus et al., 1987; Abu Rahma et al., 1994), this was not the case. Gifford et al., (1958) concluded that no definitive advantage could be attributed to sympathectomy over medical treatment.
Issues in technique
Anesthetic considerations : Single lumen endotracheal intubation
Limited ganglionectomy: a prospective evaluation
It is related to the problem of compensatory hyperhidrosis and the appropriate management of axillary hyperhidrosis. In addition, most series cannot quantify the degree or severity of the compensatory hyperhidrosis. Despite this, reducing the extent of the sympathetic ganglionectomy was associated with a lower incidence of compensatory hyperhidrosis.
An incidence of compensatory hyperhidrosis of up to 64% has been reported when the ganglionectomy is extended to the 5th or 6th thoracic ganglion. In contrast, limiting the extent of the ganglionectomy to the 2nd thoracic ganglion was associated with a reduction in compensatory hyperhidrosis to between 22 - 24%. Assessment of compensatory hyperhidrosis is based on subjectivity, rather than on objective sweat production analysis.
It is suggested that the rate of compensatory hyperhidrosis can be significantly reduced by meticulous dissection and resection of the second thoracic ganglion alone. Furthermore, this approach can cure axillary hyperhidrosis and, more importantly, reduce the incidence of debilitating compensatory hyperhidrosis.
Outcome ofthoracoscopy for palmar hyperhidrosis
It forces us to consider the likelihood of misinterpretation of anatomy as a major cause of persistent sympathetic function. Furthermore, too little emphasis is placed on learning the surgical anatomy of the sympathetic chain and its variations during standard surgical training. In such situations, extensive en bloc excision of the 2nd and 3rd intercostal nerves with their spinal ganglia and surrounding tissue has been proposed as a useful option in open surgery (van Rhede van der Kloot and Jorning, 1990).
Regenerating nerve fibers establish contact between the divided ends by thin strands that can grow into the caliber of the sympathetic chain. The return of sympathetic activity depends on the extent of the regeneration process and the proportion of sympathetic fibers that successfully restore a functional pathway. To avoid this pitfall, it is necessary to understand the surgical anatomy of the 2nd thoracic ganglion, which is located in the 2nd intercostal space, somewhat distal to the thoracic ganglion.
Electrophysiological stimulation to confirm the location (and appropriate ganglionic level) of the sympathetic chain has been suggested; this expensive, time-consuming and complicated maneuver has, not surprisingly, not gained wide acceptance in surgical practice (Lindquist et al., 1989). Given the potential of the sympathetic chain to regenerate, it is a moot point whether the described case in this series truly reflects the phenomenon.
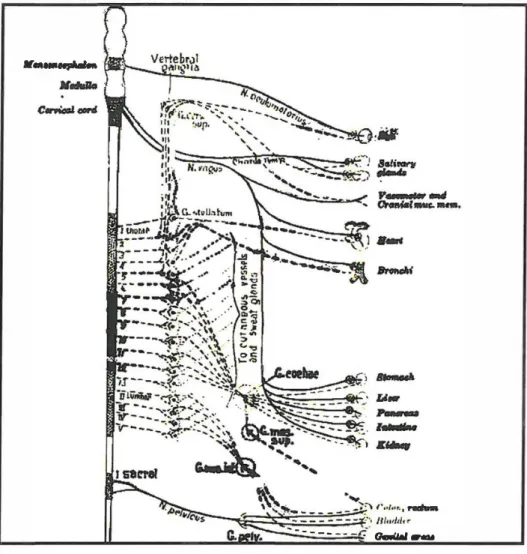
Anatomical considerations
Alternate neural pathways
In the cadaver dissections performed, it was noted that the alternative neural pathways, when encountered, were located a mean distance of 7.66 (range 2.3-30.0) mm lateral to the sympathetic chain along the inferior border of the 2nd rib . It is a moot point whether these alternative neural pathways are located far laterally, outside the enlarged operative field. The persistence of the middle and superior cervical ganglion function (since there are no white rami included) suggests that the white rami must ascend to the stellate ganglion to the middle and superior cervical ganglia.
Avoidance of the Homer effect and facial anhidrosis with T2 ganglionectomy further emphasizes the role of the T2 ganglion (and its white ramus) in upper extremity sympathetic function. Extirpation of the T2 ganglion would interrupt sympathetic outflow proximal to the stellate ganglion and brachia). While alternative neural pathways have long been of interest as an important cause of failed sympathectomy, in the context of current practice, other thoracic ganglionectomies have no surgical significance. An example of this is the role of stellate ganglion block (SGB) in predicting response to sympathectomy in patients with CRPS involving the upper limb.
To achieve accurate sympathetic blockade of the upper limb, it is necessary to block the thoracic ganglion. Although the so-called nerve of Kuntz is clearly visible as an isolated entity, it may show connections with components of the sympathetic chain, medially (with the stellate and 0.2° thoracic ganglion and with the interganglionic segment) and laterally (with the intercostal Tl -segment). nerve or the lateral cutaneous nerve of the axilla).
Stellate ganglion block: an anatomical re-appraisal
This also explains the spread of the injectate to adjacent structures such as the brachia. It has also been suggested that a false positive response may be due to the systemic absorption of the local anesthetic (Hogan, 1992). This explains why a large volume of injection can misdirect the purpose of the injection (Elias, 2000a,b.
It is clear that a large volume can confound the outcome and prognosis of the block. This anatomical study has shown that while the stellate ganglia and the proximal sympathetic chain are continuously blocked, the roots of the lower trunk of the brachia. This may be necessary since the presence of Homer's syndrome does not necessarily indicate a complete interruption of sympathetic outflow to the upper extremity, a situation predisposed when the inferior cervical ganglion is separated from the Tl ganglion.
Of the tests mentioned, temperature measurement is probably the most practical technique to assess the completeness of sympathectomy. Furthermore, sustained sympathetic blockade (especially with large volumes of local anesthetic) can cause fibrosis along the surgically significant component of the sympathetic chain.
Pathological considerations
Palmar hyperhidrosis
Chronic Regional Pain Syndrome
Interrupting the pain cycle early in the disease course in CRPS is essential to influence a satisfactory outcome. The difficulty in providing effective therapy for CRPS stems from the inability to reconcile all the changes that occur in the disease process with a unified pathophysiological process. This prompted the hypothesis that peripheral injury triggered an inflammatory response that recognized self-antigens that are normally sequestered by the immune system and this resulted in the perpetuation of the pain response.
These self-reactive T cells are anergic, either due to a low expression of the self-antigen, or the self-antigens are sequestered from the immune system after location. Another possibility is that this stimulates the neural cells in the ganglion to upregulate the receptors and thus the localization of the response to the affected sympathetic ganglia. The focal nature of the ganglion involvement suggests that the initial injury triggers the expression of MHC alleles not normally expressed by these cells, bypassing a global sympathetic ganglia involvement.
These changes are usually progressive, and the importance of the sympathetic system has long been documented given the historical conditions of the disease, such as Reflex Sympathetic Dystrophy. This can play a central role in the disease process resulting in the disease continuing and progressing.