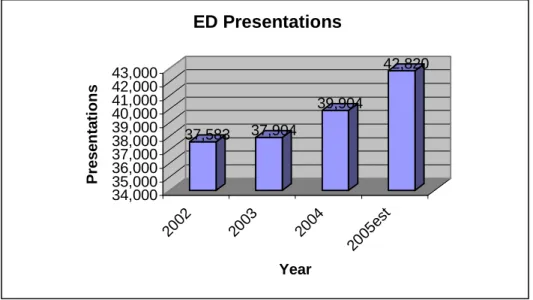
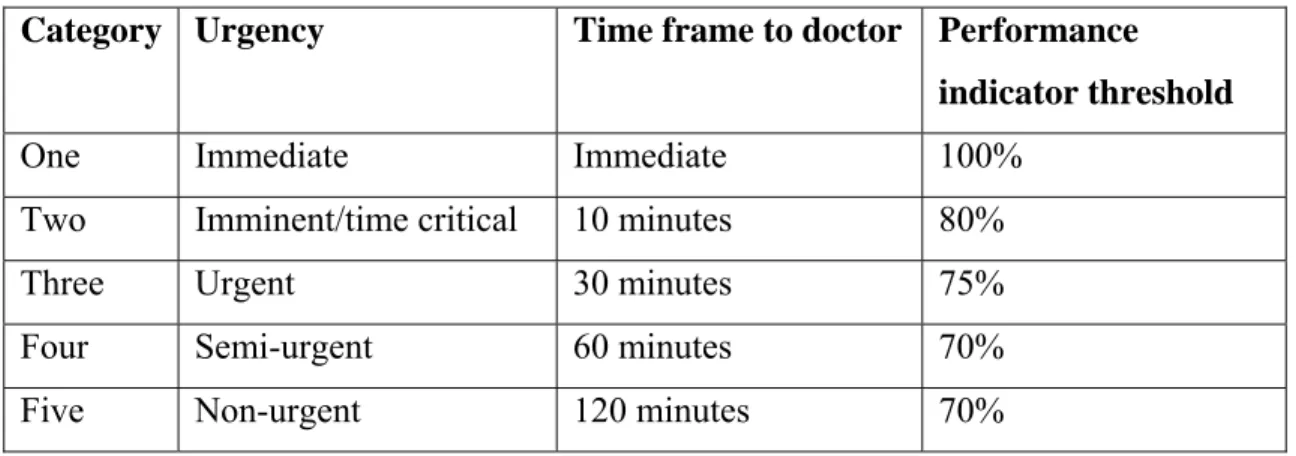
The staff of the Department of Emergency Medicine who have given their time to discuss various aspects of our processes and how they can be improved. Longer waiting times for any patient category are considered a lack of access and quality (Australasian College for Emergency Medicine, 2002). However, due to the increasing problems of ED overcrowding, category 3 persons at risk of deterioration in health status and category 4 and 5 persons often have increased wait times.
Many authors have examined alternative patient flow processes in the ED, nurse-initiated x-rays, and still others have focused on the problems of the triage process itself. I have included case examples of the experiences of two patients as they move through the department.
Triage - nature and origins
During the 1950s and 1960s in the US, EDs began to appear at the front door of the hospital, as opposed to the basement or a consulting room somewhere inside. Nurses were now providing frontline care, assessing people as they arrived at the front door of the hospital (ED). Triage also allows the allocation of the patient to the most appropriate area of the department (patient flow).
This is where the nurse's judgment and decision-making skills come into play. There is an argument that the triage process will have a beneficial impact on waiting times and patient flow, but while the waiting room guarantees 'known quantities', the triage nurse cannot influence things like access blocking. Experience shows that when the ward is overloaded and there are many patients from the lower category in the waiting room, the triage nurse often begs to place these patients among the sicker patients.
It is very unpleasant to be in the waiting room in full view trying to triage and calm waiting people.
Patient flow systems
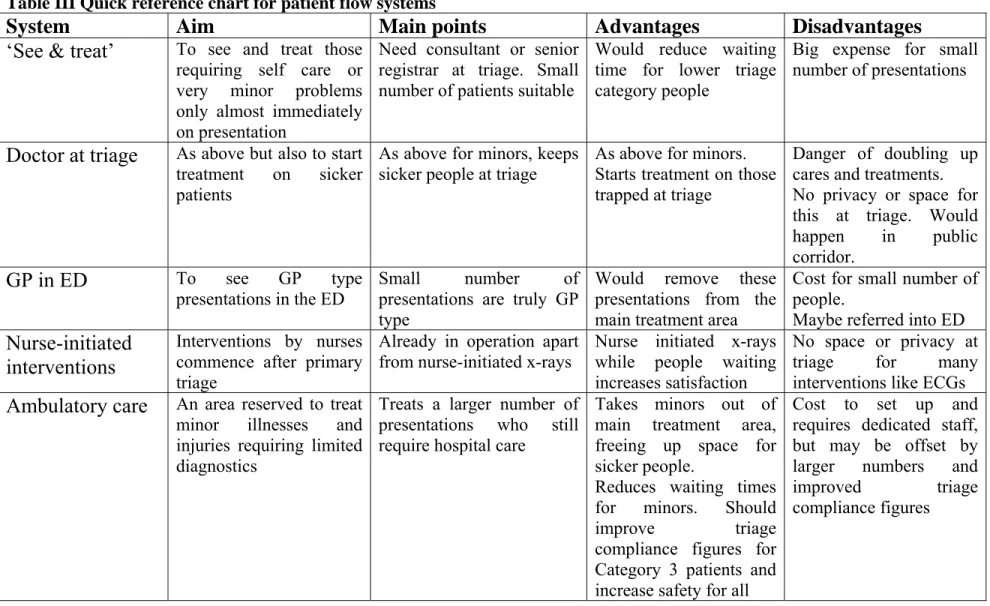
Parish and Lipley (2002) argue that all patients should be triaged shortly after arrival into minors (who require very few diagnostic tests, ie minor injuries and illnesses) and majors so that there are no unassessed patients in the waiting room. Perhaps in the future, when emergency rooms in New Zealand are staffed with nurses who can assess, treat and discharge patients without referral to medical staff, the underlying economics may change. Adjacent to the ambulance triage area is one triage assessment room, which is normally occupied by a wheelchair-bound patient awaiting a treatment area on the main ward.
Another risk is the potential for duplication of treatments or a lack of vital information from the primary physician to staff in the treatment area. In the UK there are now many 'walk-in centres', where people can access primary care without an appointment. It found that there was a drop of over 30% in the number of patients waiting over an hour to be seen and that category 3 patients also had reduced waiting times.
Such clinics are widely used in the UK and US, with most in the UK run by nurses. There is great variation throughout the UK and the US in the training of these nurses. Such is the success of the units in the UK that one survey of 269 patients suggested that 98% of patients were satisfied with the care given by nurses (Mabrook & Dale, 1998), and that there were.
Patients in the UK are used to the full care of nurses and are likely to be more accepting of them. It was found that there was no difference in the accuracy of radiological interpretation or treatment, that there were no adequate follow-up rates, and that waiting times were significantly shorter for the nurse group (mean 19 minutes versus 56.4 minutes for the ED -group). This practice has been practiced internationally for many years, mainly in the United Kingdom (UK), Canada and Australia.
When this practice was introduced abroad, one of the main concerns of medical staff and radiologists was that the number of X-rays ordered would increase. Their waiting times may be shortened, but since they can wait in the waiting room, the waiting times for sicker category three patients would be little different.
A ‘snapshot’ of the ED today
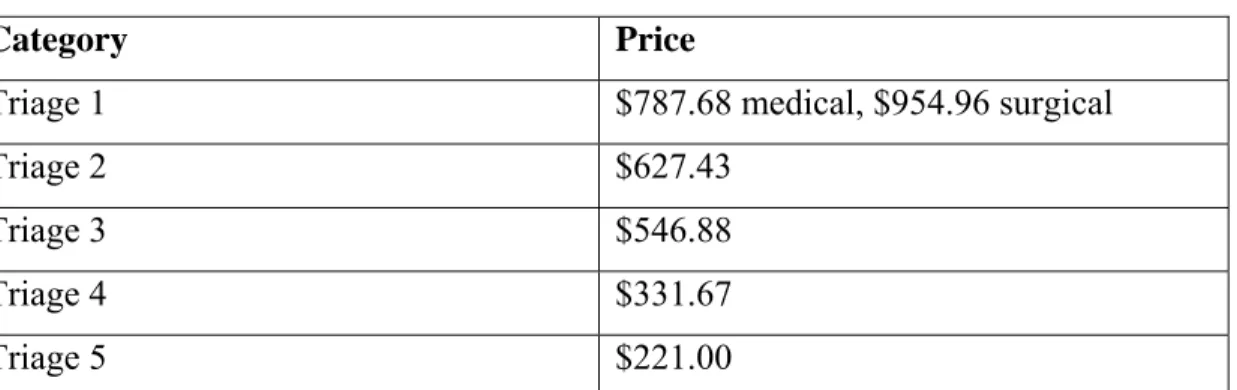
After triage, category four and five patients are briefed by a receptionist and in most cases directed to sit in the waiting room. The highest category patients on trolleys have details taken from receptionists in the triage corridor or at the bedside in the case of category one and two patients. Senior ED consultants do not have the authority to accept, although this may change in the future.
All junior doctors on ward 8 must consult with the duty registrar or consultant before discharging patients. The triage nurse asks her friends to push her into an empty spot in the waiting room and tells Hannah that she will. He joins the other two patients who are waiting on trolleys in the corridor, as the ward is full.
The nurse coordinator of the shift then decides whether she can take potential patients in the clinical section to the corridor to wait for test results or to a bed in the ward, thereby freeing up space for undifferentiated patients in the triage corridor and in the waiting room. . This follow-up contact also has the advantage of "getting to know" the patients, making it easier to communicate with them and feel that someone cares and that they are not forgotten. He would spend another six hours on the ward before being assessed by the medical registrar (who had six other patients in the queue before Ted) and another two hours before a bed would be found on the medical ward.
This scenario reveals the other reasons for long waiting times in the ED that have an impact on triage times. After more than three hours in the waiting room, Hannah is taken to the treatment area, but it is more than 30 minutes before a doctor sees her. Lack of staff and funding have limited efforts to reduce this problem in the past, but the recent significant increase in patient census and the closure of primary care after-hours centers has increased the urgency for a solution.
The choices of patient flow systems
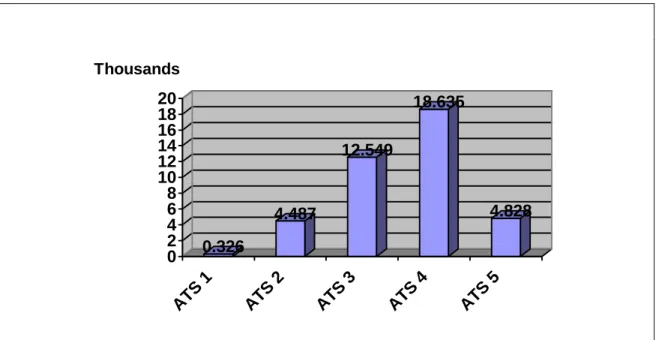
These people have the worst rates of triage compliance (see Table III), and it is hoped that this will improve with the establishment of an ambulatory care clinic, freeing up more space in the treatment room. To make sure the process works, the audit of triage compliance rates and complaint counts can be compared from a certain point in time before the ambulatory care unit opens to a certain point in time after it opens. For this reason, it is imperative that additional nurses are employed to run the ambulatory care unit.
As can be seen from the literature, the higher the rank of the physician leading the area of ambulatory care, the more efficient and safer it is. Because the ambulatory care area would only operate eight to twelve hours a day, among other things, nurse-initiated triage X-rays could help alleviate the stress of waiting for minor patients. When Hannah is triaged to category four and first aid is administered, she is identified on the computer tracking screen as suitable for the ambulatory care clinic.
Twenty minutes after returning home, Hannah is called into the ambulatory care area, where the doctor can examine her and the X-ray together. Based on the current literature and the nature of the department, streaming minors and implementing nurse-initiated x-rays appear to be the most appropriate systems at this stage. There is the potential for other category 4 and 5 patients who are not suitable for the outpatient area to be upset when others are called through before them (this has happened when the informal fast track service has been running ).
The problem could be alleviated by partitioning the waiting room so that all ambulatory care patients sit in one area, close to where they will be called. A review of waiting times and the number of complaints following the introduction of the ambulatory care area will be necessary to ensure continued funding. For this department, expanding nursing practice by introducing X-rays performed by a triage nurse and introducing a separate flow for smaller categories of patients in a dedicated outpatient area with dedicated staff at least eight hours a day should improve waiting times. times for these patients.
TRIAGE
Treatment area
General treatment
Ambulatory care area
Predicted
Innovation in accident and emergency management: establishment of a nurse practitioner-led minor injuries/primary care unit. The effect of a separate minor injury stream on accident and emergency waiting times. The heaviest repeat users of an inner-city emergency department are not general practice patients.
Patients regularly leave emergency departments before medical evaluation: a study of unexpected patients, medical profile, and outcome characteristics. Why we do the things we do: applying clinical decision-making frameworks to triage practice. Adding value to the patient experience in emergency medicine: What features of the emergency department visit are most important to patients.
Improving patient satisfaction in the ED when triage nurses routinely communicate with patients about expectations: the experience of a rural hospital. Study of choice between accident and emergency departments and general practice centers for out-of-hours primary care problems. Nurse-initiated xray of isolated extremity fractures in the emergency department: research results and future directions.
Does lack of a usual source of care or health insurance increase the likelihood of an emergency room visit?