Vol9, No
I,
January - March2000 New PSA and PSADcutoffpoint
35New Cutoff point
of
Prostate-Specific
Antigen
(PSA)
and
PSA
Density
(PSAD)
to
enhance
diagnostic
specifTcity
for prostate cancer (Pca)
in
country
with
low prostate
cancer
incidence
Djoko
Rahardjo, Siti Tersiani
Kamil
GardianAbstrak
Tujuan
penelitian
ini
ialah
untuk menentukannilai
ambangbaru untuk
PSAdan
PSADdi
Indonesia. Telahditeliti
344penderita dengan keluhan
prostat
tanpa retensi yang dikonfirmasi denganbiopsi
dan/atau pemeriksaan histopatologik. Terdapat 332 (96,5Vo) pasien pembesaran prostatjinak
dan 12 (3.5%) pasien kanker prostal. Menggunaknnnilai
ambang ),ang diterima secara internasionalyaitu
4
ng/ml dannilai
intermadiet antara 4,1-10 ng/ml, ditemukan16l
(47Vo) pasien dengannilai
PSA kurang atau sama dengan 4 ng/ml tanpa satu pun penderita kanker, 102 (30Vo) pasien dengannilai
4,1-10ng/ntl dimana hanya ditemukan
I
penderita kanker (PSA=8,3; PSAD=0.21); sedangkanlI
dari 8l
pasien (13,6Vo) dengannilai
PSA lebihdari I0
ttg/ml menderita kanker. Dengan nteningkatkannilai
ambang menjadi 8 ng/ml dannilai
intermeciietntenjadi 8.1-30 ng/nt, pada kelompok pasien yang sama ditemukan 236 (68,6Vo) pembesaran prostat
jinak
masih tanpa adakanker
untuk
PSAlebih kecil
sama dengan8
ng/ml;
89 pembesaran prostatjinak
dan
I
kankerpada
nilai
intermediet, sedangkan penderita kankerlainnyl (l I dari
18 pasien atau 6lVo) mempunyainilai
PSA diatas 30 ng/nil. Ditemukan korelasiantara rata-rata
nilai
PSA dengan usia dan besar prostat (p<0.01, r=0.242&
0.429 padanilai
PSA < 4.0 ng/ml; r=0.265 &0.452
pada
nilai
PSA <I
ng/ml, r=0.261
& 0.020
pada
PSA> I0
ng/ntl). Kemampuannilai
ambangbaru
ini
untuk nteningkatkan deteksi kankerprostat
dievaluasi dengan analisisunivariat dan
menggunakankurva
Receiving OperatingCharacteristic (ROC). Dengan nilai
ambangbaru
ini
didapatkansesitivilas I00Vo untuk
deteksikanker,
sementaraspesifisitasnya 85,8Vo. Penggunaan
nilai
PSAD Lebihdari
0.20 meningkatkan spesifisitas hingga 94.9Vodan
menaikkan kenrungkinan deteksi kanker (positive predictive value)dari
12.97o menjadi 157o. Area dibawah kurva meningkatkandari
0.970 ntenjadi 0.974 r.tntuk PSA dan 0.987 menjadi 0.989 untuk PSAD dibandingkan dengannilai
ambang standar. Dengannilai
ambcng baru didapatkan penurunanjtmlah
biopsi hingga 42.4Vo tanpa menghilangkan kemampuan deteksi kankerAbstract
The purpose
of
this studyis
to determine new cutoffpoint of
PSA and PSADin Indonesia.
Three hundred andforty
four
patie.nts with prostate complain without urinary retention confirmed by biopsies and/or h),stopathological examinations were analyzed. There were 332 (96.5Vo) patients histologically conflrmed benign prostate hyperplasia andl2 (3.5Vo) had prostate
cancer (Pca). Using cutoff
levelfor
PSA of 4 ng/ml and intermediate value of 4.1-10 ng/ml, there were 161 (477o) patients hadPSA level less or sanxe as 4 ng/ml and none of them had Pca, 102 (30Eo) patients had intermediate PSA level (4.1 to
I0
ng/ml) and onlyI
confirmed Pca (PSA 8.3, PSAD 0.21) while I Ifrom
8l
patients (13.6%)with
PSA abovel0
ng/ml had Pca. Raising tlte curoff point to 8 ng/ml and intermediate value of 8.1 -30 ng/ml,from
the same group of patients we found 236 (68.6Vo) BPH patients stilL with no Pcain
PSA less or same as 8.0 ng/ml: 89 BPH patients andI
Pcain
intermediate PSA level, while therest Pca patients ( I
l
amongI8
or
6lVo) patients) had PSA above 30 ng/ml. We found correlation between mean PSA level with age and prostate volunte(p<O.il,
r=0.242&
0.429 in patientswith
PSA < 4 ng/ml; r=0.265&
0.452in
PSA<
8 ng/ml,aril
r=0.261&
0.020in
PSA> I0
ng/ml). The abilityof
this new cutoff to enhance rhe power in detecting Pca was cvaluatedb), using wtivariate analysis and Receiving Operating Characteristic (ROC) curves. By using new cutoff
point
produced asensitivitl,
of
l00Voin
detecting Pcal, while specificityis
85.8Vo. The applicationof
PSAD greater than 0.20 enhanced thespecificitl, to 94.9% and increased the possibilitlt to detect Pca (positive predictive value)
from
I 2.9Vo to I 5Vo. Area under thecurve has also increased
from
0.970 to 0.974for
PSA and 0.987 to 0.989for
PSAD compared with standard cutoff points. With îhe new cutoff level there was a decrease of the number of biopsies up to 42.4Vo without ntissing any cancer detectionKeywords: PSA, PSAD, prostate cancer, new cutoffpoints, ROC curve
36
Rahardjo and GardianProstate cancer has become the commonest malignancy
of
themale urinary tract
andis the
second commonest cancerin
Europeansment. In United
Stateit
is thefirst
cornmonest neoplasmin
men and second leading causeof
cancer
death.Data
in
1996 revealedthat Pca
was 40Vofrom
all
new
malignant
diseasesin
men and
it
gave
14
Vo mortality
in
men due
to
malignancy2.During his
life,
20Voof
men
will
have possibility of
having
Pca.
Unlike
in
westem countries,
Pca
isrelatively
rarein
Indonesia.Although
Pca was includedin
the ten highestmalignancy in
men,the
second mostfrequent malignancy
in
urology clinic
and
it
was
the most commonform of male'
cancer, the cases collectedbetween
1990-1994from
different
hospitals wereonly
28-33 per
y"at'.
Prostate-specific antigen
(PSA) is clinically
the
mostuseful
tumor marker
to detect
prostatecancer
(Pca)4.Combining PSA
with
PSAD
in
intermediate
serumPSA
level,
will
increase
the specificity
in
Pcadetection. PSA is specific
for
prostate tissue,it
is not
prostate cancer-specific.
An
elevated serum
value doesnot
always denote prostate cancer.It
has been
demonstrated
that
I g of
benignhyperplastic tissue gives
rise to 0.2 ng/ml
of
PSA in
the
seruma.Even though currently
used, PSA
alonecould not
give ideal
sensitivity
or
specificity
inscreening Pca. Numerous investigators used PSAD,
defined as
serumPSA level per
prostatevolume,
for
those with
intermediate serum
PSA
level.
This
determinant
can
help
to
distinguish men
with
early
Pcafrom those with BPH only. Despite the
vast usedof
the recommendedcutoff level
of PSA
andPSAD in
Pcadetection, the appropriate PSA
andPSAD cutoff
level
for
Indonesian,
as country
with low
Pcaincidence remains
unrevealed. Screening modalities
andtheir combination
is lack
in
sufficient
specificity
resulting
in a
high ratio
between
the
number of
biopsies and thenumber of positive
detected Pca.In Cipto
Mangunkusumo General Central
Hospital
and Sumber Warashospital
wefound
meanPSA level
of Benign
prostatehyperplasia (BPH)
patientswithout
urinary retention was
still
above
4
ng/ml,
i.e.
6,8ng/ml. While for
Pcait
was
118.53nglml. Until now
the interpretation
of
PSA
value
is still
controversial.
Therewere
some patientswith
Pcawithout
increasingPSA level, while
therewere
also alot of
patientswith
BPH
with high PSA
value.The purpose
of
this study
is to
know the profile of
PSA
andPSAD
in BPH
and Pca patients,to know
theMetl J Indones
correlation
in
eachvariable
(age, prostate volume,.PS andPSAD)
andto
searchfor new cutoff point of PSA
andPSAD
in
Indonesia basedon
the dataavailable in
order
to
enhance
diagnostic
specificity.
Receiving
Operating Characteristic
(ROC)
curves
were
used toshow the relative
intrinsic discriminatory potential
of
various
parameters aspredictor
for
a positive biopsy
result. The predictors were
estimated as afunction of
the
various continuous parameters
and
of
binary
parameter, such asPSA
andbiopsy, by the
meansof
logistic
regression analysis.sMETHODS
From
September 1994 toAugust
1997,34
consecutivepatients
age4l-90
years who had
prostate symptomswithout
acute urinary retention
from
Sumber
WarasHospital
(private hospital)
and Cipto
MangunkusumoGeneral
Central Hospital
(public
hospital)
were evaluated. Data collected included age, prostate volume measuredby
trans rectal
ultrasonography,
PSA
and PSAD, and histopathological examination.Transrectal ultrasonography
was
performed
usingScanner
200 (Pie
Medical, Netherlands)
with
7.5MHz
transducer and the prostate size was
measuredusing the prolate ellipse
formula,
i.e.
prostatevolume
("*t)
-
(width x height
x
length
in cm
) x
0.52. PSA
was
measured
using
PSA
Enzyme
Immunoassay(EIA),
IMX
PSA Assay Abbott
Laboratories, (North
Chicago,
IL
IRMA
Count Assay, Diagnostic product,
Los Angeles,
CA)
using
PSA monoclonal antibody.
PSAD
wasdefined
asPSA level per
prostatevolume
(cm3). Sextantbiopsy using biopsy gun TRUS-guided
was
performed
rf
malignancy
was
suspected;
ascharacterized
by
hard
nodule
on
digital
rectalexamination, hipoechoic
area,PSA level
greater
than10 ng/ml,
or PSA
level 4.1-10
ng/ml
with
PSAD
greater
than 0.15.
Specimen
for
pathological
examinations
were sent
to
Pathology Laboratory
in
Sumber Waras Hospital
or Cipto
Mangunkusumo
General CentralHospital.
With
these original data, analysis was
performed
tofind
out new cutoff point
of
PSA, PSA intermediate
andPSAD level.
Since thefirst
Pca case revealedwith
PSA 8.3 ng/ml
and
PSAD of
0.21,
we
proposedcriteria
of
PSA
lessor
sameas 8.0
ng/ml
asno
Pca (unnecessaryto
dobiopsy), PSA
8.1 to 30nglml
as anintermediate
level, and PSAD
above
0.20
asindication
fbr
biopsy; and PSA
above
30.0 nglml
asVol9, No
I,
January - March2000(ROC)
curves
of
total
serum PSA and PSAD
wereconstructed
for
all
ll8
men underwent
biopsy with
PSA 4.1 to l0 ng/ml with PSAD
above0.20
andPSA
above l0
ng/ml, including
l2
patients with
Pca.This
procedure also constructed
for
the new cutoff point.
ROC
curves
in which chart the sensitivity
versus
1-specificity
of the test along a range
of
cutoff
value, were constructedfor
eachPSA group. Sensitivity
wasdefined
as equal
to
the
nnmber
of
true
positive
divided
by
the
sum
of
true
positive
plus
falsenegative.
Specificity was defined
as
equal
to
the numberof
true negativedivided by
the sumof
the truenegative plus false positive. Positive
predictive
valuewas
the
likelihood
of
prostate prediction
beingcorrect. Points closest to the upper left
corner
of
thegraph (100Vo
sensitivity
and
100Vo
[1-specificity])
provided
the bestdistinction
between subjectwith
andwithout
diseasesStatistical analysis
of clinical
variables,
which
wereage,
PSA, prostate
volume
and PSAD
betweenpatients
with positive
biopsies and negative
biopsieswere
performed
using
Students t-test.
To
testcorrelation between parametric variables,
we
used Pearsoncorrelation
test.For all
testprobability
valuep<0.01
was consideredstatistically significant.
RESULTS
During
theperiod of
3 years (September 1994-August1997)
we
found 344 cases with prostate
symptomwithout urinary retention
which
consistsof
332 BPH
patients and
12 Pcapatients.
Patientswere retrieved
from both Urology
Clinic
in
SumberWaras Hospital
and Cipto Mangunkusumo General Center Hospital.
For
diagnostic procedure
all
of
them
underwent
physical, laboratory
(which
include
PSA),
Trans-rectal ultrasonography
(TRUS)
and
uroflo-metry
examinations.
Patients' variables were
catego-rizedinto BPH
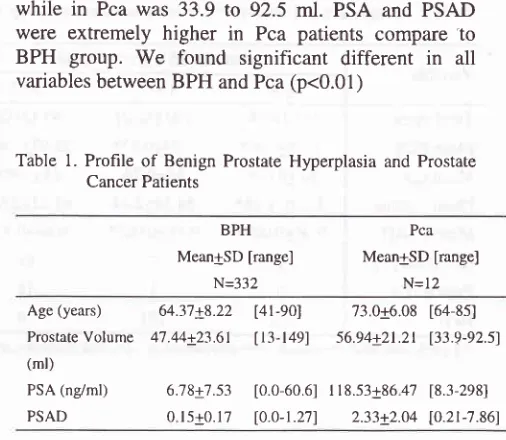
and Pcaprofile. Table
I
shows comparisonof
age, prostate volume, PSA and PSAD
betweenBPH
and Pcapatients. BPH patient's median
age was65
and
the mean was 64.37
while Pca patient's
median
agewas 12.5
andthe
meân was73
years old.Prostate
volume range
in
BPH was 13
to
149 ml,
New PSA and PSAD
cutoffpoint
37while
in Pca was 33.9 to 92.5
ml. PSA and PSAD
'ffere extremely higher
in
Pca patients
compare
'toBPH
group.
We
found
significant different
in
all
variables betweenBPH
and Pca(p<0.01)
Table
l.
Profileof
Benign Prostate Hyperplasia and Prostate Cancer PatientsBPH Mean+SD [range]
N=332
Pca
MeantSD [range]
N=12
Age
(years)
64.37+8.22[41-90]
73.0a6.08 [64-85]ProstateVolume 47.44+2?.61
u3-1491
56.94+21.21 133.9-92.51(ml)
PSA (ndml)
PSAD
6;78+7.53 [0.0-60.6] I 18.53+86 4'7 18.3-2981
0
ls+0.17 l0.o-1.271
2.33+2.04 [0.21-7.86)+ AII variubles were rigni|icuntl)'tlillerent (p<0 0l ), determined br t-test
Since the first PSA
value
of
the
Pcapatient was
8.3nglml
and PSAD value was 0.21, we try to
use
8ng/ml
as anew cutoff
level
for PSA
and8.1-30 ng/rnl
as intermediate
level
with
PSAD
of
0.20 as
anindication
toperform
biopsy.To
compare
the
two
cutoff
levels, patients
werestudied
using
standard
and
proposed
cutoff
level
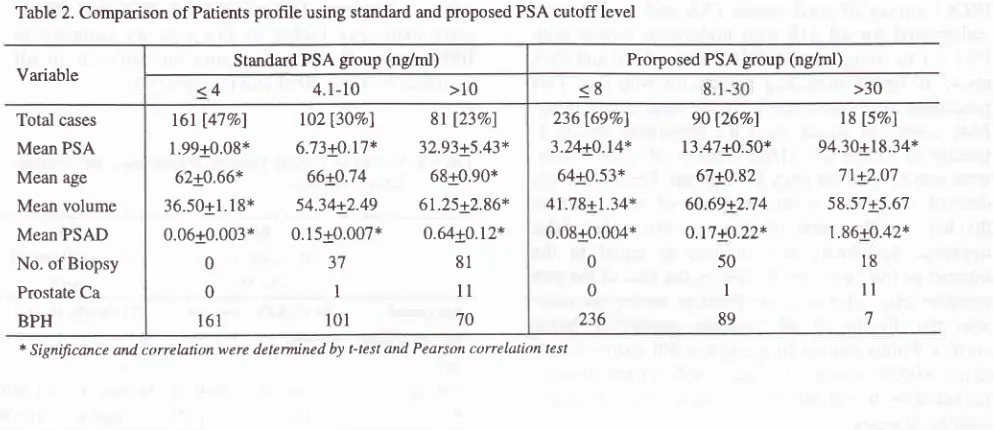
(Table
2).Using
standardgroup
therewere
161 (47Vo) caseswith PSA
level below or
same as4 nglrrl,
102 (30Vo) casesin intermediate range (4.1-10 ng/ml)
and8l
(23Vo) caseswith
PSA more than
10ng/ml.
From
all the
161with PSA < 4 ng/d,,
there were no prostatebiopsy performed and were
assumedto be free from
cancer based
on
the digital
rectal
and
TRUS
examinations
and
the
result
of
pathologiccal
. [image:3.595.329.582.90.310.2]38
Rahnrdjo and GardianTable 2. Comparison of Patients profile using standard and proposed PSA cutoff level
Variable
Med J Indones
Prorposed PSA group (ng/ml)
236169%) 3.24+0.14* 64+0.53* 41.78+1.34* 0.08+0.004*
0
0 236
9O 126%ol
13.47+0.50* 67+0.82 60.69+2.74 0.17+0.22*
50 I
89
18 [5Vo]
94.30+18.34* 71+2.07 58.57+5.67 L86+0.42*
l8
ll
1intermediate
PSA level with PSAD
greater than
0.20 andPSA
above30 ng/rnl respectively.
If we
used theinternational
cutoff
on the
new cutoff,
there were
25,75
and 18biopsies
(totally
118biopsies)
in PSA
of
8nglrnl; 8.1-30 ng/ml and above 30
ng/ml
(data
not
showed). The
twentyfive
biopsies
in PSA
of
8
ng/ml
becoming zero
assuffred asno
Pca cases,75
biopsiesbecoming 50
becauseof
the
increasein PSAD (from
0.15
to 0.20), the 18 biopsies was
stil
the
same becauseof
the
samecriteria
in
performing
biopsies.Therefore there
would
be
50
unnecessary
biopsies(42.4Vo)
could
be
saved
withourt missing any
Pca cases.By
using the
new cutoff point
produced
a
sensitivity
of
l00Vo
in
detecting Pca,
and specificity
of
85.8Vo.The application
of PSAD
greater than 0.20
enhancedthe
specificity
to
94.9Voand
increasedthe
possibility
to
detect Pca
(positive predictive value) from
l2.9%oto
15Vo(Table
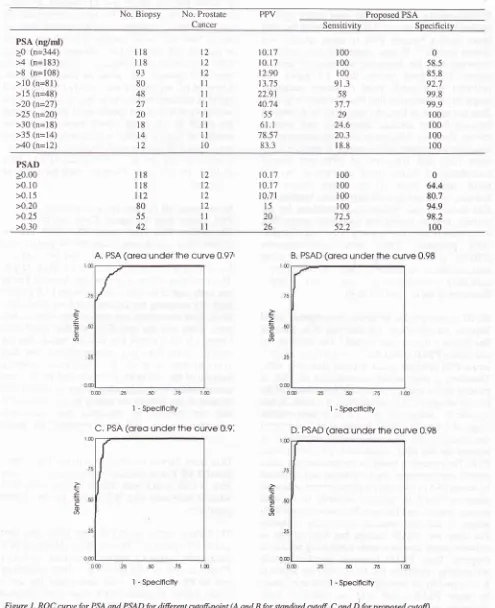
3).
Area under
the
curve has
alse increasedfrom
0.970
to
0.974
for
PSA
and 0.987
to0.989
ibr
PSAD
compared
with standard cutoff
points.
(Fig.
1)>30
<8
Total cases
Mean PSA Mean age
Mean volume Mean PSAD No. of Biopsy
Prostate Ca BPH
The
mean age was
increased
significantly in
eachPSA
subgroup
from the
standardand
proposedPSA
group. There were also significance difference
andcorrelation between
PSA with
age, appearedin
PSA
less
or
same as4.0 ng/ml, PSA
less
or
sameas
8.0ng/ml
andPSA
greaterthan
10ng/ml (r=0.242;0.265
and
0.261 respectively). Other significance difference
and correlation were
also
seen
between
PSA
and prostatevolume, in PSA < 4.0 ng/ml
and
PSA
<
8.0ng/rnl. (r=0.429 and 0.452).
But
between
PSA
in
subgroup greater
than
10
ng/ml
and prostate volume
we found week correlation (r=0.020).
Consequentlythere was also
an
increase
of
PSAD
in
every
subsetPSA
group
(p<
0.01,
r=0.65;
0.43;
0.91;
0.72',0.57
and
0.56 respectively)
becausePSAD
was defined
asquotient
of
serum PSAdivided
with
prostate volume.With new cutoff point,
most patients
(697o) hadPSA
less
or
same as 8ng/ml
and noneof
them
had Pca.In
intermediate
PSA level
(8.1-30
nglrnl), we found
90 patients,with only
I
patient
had Pca.In PSA
above 30ng/ml
11from
18patients
(6lVo)had
Pca. There were50 and 18 biopsies (totally 68
biopsies,
table
2)
in
Standard PSA group (ng/nù)
<4
4.1-10
>10t6t
[47vo]
102[30Eo]
8t
î23%l1.9910.08* 6.73!J.17*
32.93+5.43*6210.66* 66!J14
6810.90*36.50+1.18* 54.3412.49
61.25+2.86*0.0610.003*
0.15t0.007*
0.64+0.12*0
37
810
I
ll
161
l0l
70 [image:4.595.76.573.91.306.2]Vol 9, No 1, January - March 2000 New PSA and PSAD cutoff point 39
Table
3.
Sensitivity, specificity and Positive Predictive Value (PPV) foi ditTèrçnt PSA and PSAD from all parienrsNo. Biopsy No. Prostate Cancer
PPV Proposed PSA
Sensitivity
Specificity PSA (ng/ml)>0
(n=344)>4
(n=183)>8
(n=108) >10 (n=81) >15 (n=48) >20 (n=27) >25 (n=20) >30 (n=18) >35 (n=14) >40 (n=12)118 118 93 80 48 27 20 18
t4
12
t2
l2
l2
il
lt
ll
ll
ll
ll
l0
10.17 10.17 12.90
13.7 5 22.91 40.74
55
6t.l
78.57 6J-t
r00 r00 r00 91.3 58 37.7
29 24.6 20.3 r8.8
0 58.5 85.8 92.7 99.8 99.9 100 100 100 100
PSAD >0.00 >0.10 >0.15 >0.20 >0.25 >0.30
l8 l8 t2
80 55 42
t2 I2
l2
lz
ll
ll
100 r00 100 100 72.5 52.2
to.t7
10.17 10.71 15
20 26
0 64.4 80.7 94.9 98.2 100
r
È
=c
o È
c
0)
A. PSA
(oreo
underthe
curve 0.97tI - Speclficity
C. PSA
(oreo
underthe curve
0.9,B. PSAD
(oreo
underthe
curve 0.98I - Speclflclty
D. PSAD
(oreo
underthe
curve 0,98È
=
co
6
È
È c o
a
50 75
I - Speclflclty
tæ 50 75
[image:5.595.73.568.104.712.2]I - Specificity
40
Rahardjo and GardianDISCUSSION
Prostate-specific
antigen
is
the most tumor
specific
antigen
known. However,
it
isfar
from
being
theideal
tumor marker
because
PSA
is
organ specific,
not
disease specific.2'7
To
date, serumPSA level is
still
animportant
tool
for
diagnostic
screening
of
prostatecancer.
PSA level
greater
than
4.0 ng/ml
still
indicated
as
a cutoff point
to
pursue
additional
diagnostic evaluation
to find
Pca.Unfortunately, PSA
does
not
appearto
have
the specificity to
distinguish
between
benign prostate hyperplasia
and
prostate cancer. Thereis
adifficulty in
selecting patients as thecandidate
of
prostate needle
biopsy
if
they clinically
show signs and
symptoms
of
BPH with
normal
consistency
of digital
rectal
examination.
As
theresult,
usually
there
are
too
many
unnecessary biopsies,which
cangive not only logistic
burdens,but
also morbidity and psychological problems
for
thepatients. Besides
having
low
specificity,
serum PSA
could
elevate
not only
in
malignancy,
but
also
afterDRE
procedure,
Trans rectal
ultrasonography
(TRUS),
prostate massage, prostatitis
and
someinstrumentation procedures
such
as
cystoscopy,indwelling
catheterization
and
Trans
Urethra
Resection
of
the Prostate(TUR-P)
PSAD
is
thought
by
numerous investigators
could
improve
the
specificity
for
detec^tingPca,
however
this theory
remains
controversial.' The
rationale
for
calculating
PSAD
is that
Pca tissue produces ahigher
serum
PSA level per
gram
of
tissue than
doesBPH.
Therefore,
a
high
serum concentration
of
PSA
in
patients
with
asmall
prostatecould
be evidenceof
the presentof
cancer.8The
serumPSA,
if
elevate,is
lessspecific
for
malignancy when
it
is
in
inter-mediate
rànge
of 4.1
to
10nglr.,t.n Benson
et
al
r0 developedthe concept
of PSAD,
in
intermediate
serumPSA,
toaccount
for
the BPH contribution
to
elevated
serumPSA. The concept is
basedon the premise that
undernormal
circumstances, each
epithelial
cell
(reflected
by
serumPSA)
will
require
agiven
amountof
stromaltissue (reflected
by
prostate
volume)
to
maintain
normal
structure andfunction. Normal
tissue andBPH
adhere
to
this rule,
whereas
malignancy,
including
Pca does
not.
PSAD concept has been proven
toenhance cancer
detection
while minimizing
numberof
biopsies.
Thus, PSAD
improves specificity while
maintaining sensitivity.
But
PSAD
doesnot
appear to be acceptedby all
investigators.
Catalona et alEfound
by
using PSAD
cutoff
0.15,
as
stated
in
manyliteratures,
enhancedspecificity but
on
theother
handmissed
half
of
the
tumors.
The
inaccuracy
of
theMed J Indones
estimation
of
prostate
weight using TRUS
comparedto
actual prsotate
weight (r=0.61)
become
the
basicreason
of
this
rejection.
So he
recommended
for
needle
biopsy
in
patients
with PSA
greater than
4.0ng/ml.
Shinohara
et
al6confirmed PSAD
was useful
in
patients
with PSA
level
4
to 10
nglml with
normal
DRE
andnormal ultrasonography.
Nevertheless therewere
2OVopatients had cancer
on
prostate
biopsies.Littrup
etalrr
suggestedif
we useonly PSA
cutoff
4.0ng/ml
asindicator to perform biopsy,
it
will
produce asensitivity
of
67Vo and aspecificity
of
93Vo.Lowering
the cutoff
to
2.0
ng/ml,
which
mean
increase
thenumber
of
biopsy, yielded
a
sensitivity
of
9l%o
andspecificity
ll%i.
Labrie et
alr2reported
similar
value: asensitivity
andspecificity of
TlVo
and9lVa
for
PSA
of
4.0
ng/ml;89Vo
and 73Vo respectivelyfor
aPSA
of
2.0 ng/rnl.
In
our
series,all
Pcapatients were
detectedin
serumPSA
greater
than
4.0
ng/rnl.
From
102 patients
in
intermediate
PSA
level
(mean
PSA 6.73)
only
I
(O.98Vo)Pca was
detected
with
PSAD
greater
than0.20,
andin PSA
above
l0
ng/ml
there were
only
11Pca among
8l
(13.6%o)patients (mean
PSA
32.93).This condition
describesthe low
incidence
of
Pca in
our
study, and atthe
sametime
the meanPSA is quite
high.
By
accepting the recommended westem
cutoff
level,
there were numerous
unnecessarybiopsies
hadbeen done, and
the
specificity
of
this cutoff
waslimited
(7l,9Vo
for PSA
less than4.0
ng/rnl,
datanot
shown).
These
data were
incomparable
to
the
datafrom
western countries.
The
differences
probably
because
of
the
low
incidence
of
Pcaand most
of
our
patients
camein
already rather
severeconditions
dueto
most
of
our patients
arebelong
to
low-economical
and
not
covered
by
insurance
and were
low
educational status,
and
they
neglected
the
initial
symptoms
of BPH
or Pca.Data
from Taiwan
reported
by
Yu
and
Lai,rr
they
fotnd
8.4VoPca
in
patients
with
preoperative
serumPSA
4.1-20
ng/ml
with
PSAD
greater
than
0.15 whereas there wereonly
56 Pca casesamong
100.000population.
The
PSAD
cutoff point
of 0.15 gives
1007osensitivity
and 94.57o
specificity. This cutoff would
reduce 30Vounnecessary biopsies. Compare
to our
study, proposedPSAD
cutoff point of
0.20
still
give
1007osensitivity
and
94.9Vo
specificity,
with
area under
the
curve0.989. Hence,
it
spared 42.4Vo unnecessary biopsieswithout
missing
any
Pca.
If
we
used
cutoff
value
of
VoL9, No 1, January - March2000
a
sensitivity
of
TOVoand
a
specificity
of
6lVo
for
PSAD
cutoff
0.18
or
greater.
Like
in
Taiwan
andJapan
in
Indonesia Pca incidence
were
also
low.
Sothere were much similarity between
the
published
data and our
finding.
Our
study showed
the
mean
PSA
level
in
BPH
patients
wasquite high, i.e.
6.78+7.53,
aswell
as themean
PSAD,
i.e.
0.15+0.17.
These
finding
weresrmilar
wrth the
Japanese
and Taiwanese
studies.Their
meanPSA
were5.05+2.15
for
the Japanese and1.7+3.1
for
the
Taiwanese,
while
the mean
PSAD
were
0.17
and
0.21 respectively.
While our
meanprostate
volume
(47 .44cc)
wasbigger
than they have,which
were
35 cc
and
35 cc
respectively.
The
meanage
in this
study was 64.37.
exactly
the
same as agereferenced
PSA published by
Mettlin.'t
For the
Pcapatients the
meanvalue
of
PSA,
prostatevolume
andPSAD
(118.53+86.73;
56.94+21.212;
33+2.04)
revealed
significantly ditferent from
the Japanese, theTaiwanese,
and
western
countries.
All of
theparameters
were higher. Once again
this
condition
might
be dueto the lack
of
awarenessof
the diseases.If
we take westerncountries
as comparison, Benson etal'
demonstratedthe
Pca meanPSA
values was only
24.4136.9,
the
mean
of
PSAD
was 0.58110.739
andthe
meanof
prostatevolume
was43.0+21.6,
whereasfbr
BPH
patients, mean
of
PSA, PSAD
and
prostatevolume were 3.7+3.3; 0.044+0.027 and
88.5+57.2respectively.
All
patientswith
PSAD
greater than 0.12had Pca.
Interestingly, Nishiya
et
al'
from
Coloradofound
meanPSA
for BPH
and Pcamuch higher
from
other
westem literature
i.e.
5.23+5.04
ng/ml
and10.39+11.65
ng/ml
respectively.
Djavan
et
alr6
alsofound
hrgher
level i.e.
6.72+1.68
fbr
mean
PSA
in
BPH
patients,
but lower level
for
mean
PSA
in
Pcaparienrs (7.45+1.76).
He
sratedcutofï PSAD
greaterthan 0.20
resulted
in
51.67osensitivity and
80.99Vospecificity.
According
to
our
data, mean Pca
volume
was
muchbigger
than
BPH volume (5694t21.21 cc
comparedto
47.44123.61
cc) This finding
is
the
same as
theresult
of Menlin et
alr-5which is with
38.9+16.41
for
mean Pca
volume
and 33.5+14./,3
for BPH
volume.But
other
investigators
showed
the
contradictory.
Nishiya
fbund
40.5416.56 mean
Pca volume
and42.6+25.04
for
meanBPH
volume.2There
were
correlations between
PSA and age
and betweenPSA
and prostatevolume
in
different
groupof
PSA
value.PSA
increasedwith
agein
PSA level
<
4.0ng/rnl,
<
8.0ng/ml
and>
10ng/ml (p<
0.01,
r=0.242;New PSA and PSAD
cutoffpoint
4'lle 2). Our finding
was(p<0.01,r=0.37)
andSerum
PSA
was
alsofunction
of
prostatevolume.
Strongcorrelation
resultedin
PSA
level
<
4.0 ng/rnl
and
<
8.0
ng/ml (p<
0.01.r=0.429
and
0.452
respectively),
which
is
similar
toCollins
(p<0.01,
r=0.56)
and
Oesterling
(p<0.01,r=0.55). The factor most
likely
to
be responsiblefor
thePSA-related increase
in
ageis
the concomitant increasein
prostatevolume
as men get older.But
between PSA greaterthan
l0
ng/nrl
and
prostatevolume
there
wasweek
correlation (r=0.020). Between
intermediatestandard PSA, proposed
PSA level
and prostate volumethere were also week correlation (r=0.109
&
0.124). Thiswould
seemto
indicate
a
greater
diversity
in
tumor volume and tumor behaviorin
this subgroup of patients.Given
thesecondition,
thefbrmer cutoff level of
PSA
for
BPH
management
has lead
to
too
many unnecessarybiopsy perfbrmed
rn
intermediate PSA
level (4.1
to
l0
ng/ml) with PSAD
value
greater than0. l5
or in
PSA greaterthan
l0
ng/ml.
In
summarize,
by using the new cutoff
to
8.0
nglml
we
found still no
Pca detectedin PSA
less 8.0 ng/ml
(sensitivity 100%, specificity
85.8Eo).The
used of
PSAD
greater
than
0.20
in
intermediate PSA
level(8.1
to
30
ng/ml) resulted
in
l00%osensitivity
and94.9
specificity. While PSA
greaterthan
30 ng/ml
asupper
cutofTresulted
in
asensitivity
of
24.63Vo and aspecificity
oT
l00%o.
With his
new
recommendedcutofï points, we could
saveup
to
42.4
7o biopsieswithout
missing
any cancer.Further prospective
studyin
hospital-basepatients
or
even
more
in
community
based-population
with
this new
cutoff
level
might
lead
to
better
targeting
for
early detection and
also improvesthis
newcutoff
performanceREFERENCES
l.
BurtonJL,
OakleyN,
Anderson JB. Recent advances in the histopathology and molecular biologyof
prostate cancer. Br J Urol- in press2.
Nishiya
M,
Milter G,
Lookner
DH,
Crawtbrd
ED.Prostate
specific
antigen density
in
patients
withhistologically proven
prostate carcinoma.
Cancer 1994;14:3002-93.
Himawan S, Krisnuhoni E. Urologic cancerin
Jakarta: Pathofogy-baseddata:
1990-1994.Ind
J
Onccology1995;6(2):57-64
4.
OesterlingJE,
Jacobsen SJ,Chute
CG,
Guess HA, Girman CJ, PanserLA
LieberMM.
Serum42
5.
Rahardjo and Gardian
healthy men: Establishmen
of
age-specific references rangesJAMA
199 3 ;27 0 (7 ):860 -4Bangma
CH,
RietbergenBW,
KranseR,
BlijenbergBG,
PetersonK,
Schroder
FH. The free-to-total
prostate specific antigen ratio improves the specivicityot
prostate specific antigenin screening
for
prostate cancer in general population. JUrol
1997; I 57l'2191-6Shinohara
K,
Wolf
JS,
Narayan
P,
Canol
PR. Comparisonof
prostate specific antigenwith
prostatospecific antigen density
for 3
clinical
applications. JUrol1994:'152:1203
Benson
MC,
WhangIS,
PantuckA,
Ring
K,
Kaplan SA, Olsson A, et al. Prostate specific antigen density: amean
of
distinguishing benign prostate hypertrophy and prostate cancer. JUrol
1992;1 47:815-6Catalona
WJ, Richie
JP, deKernioJB,
Ahmann FR,Ratliff TL,
Dalkin
BL,
et al.
Comparisonof
prostatespecific antigen concentration versus prostate specific
antigen density
in
the early
detectionof
prostate cancer: Receiver operating characteristic cueves. J Urol1994;152:2031-6
Benson
MC,
WhangIS,
OlssonCA,
McMahon DJ,Cooner
WH.
The useof prostate
specific density to enhance the predicitive valuein
intermediate levelsof
serum prostate specific antigen. JUrol
1992;147:817-21
Benson
MC,
OlssonCA.
Prostate specific antigen andprostate
specific
antigen density'
roles
in
patient evaluation and management. Cancer 1994;1 4: 1667 -7 3Med J Indones
Yu
HJ,
Lai MK.
The usefulnessof
prostate specificantigen
(PSA)
densityin
patientswith
intermediate serum PSA levelin
a countrywith low
incidenceof
prostate cencer.Urol
I 998;5 I (Suppl 5A): I 20-30Gohji K,
Nomi
M,
EgawaS, Morisue
K,
Takenaka A,OakamotoM
et al. Detectionof
prostate carcinomausing
prostatespecific
antigen,its
density,and
thedensity
of
transition
zone
in
Japanesemen
withintermediate
serum
prostate
specific
antigen concentration. Cancer 1994;1 9 (1 0):1969 -7 6Littrup PJ, Goodman
AC, Mettlin
CJ. The benefit andcost of prostate cancer detection.
CA
1993;43:134-8 Labrie F, DupontA,
Suburu R, CusanL,
Tremblay M,Gomez JL et al. Serun prostate specific antigen as
pre-screening
test
tbr
prostâte cancer.
J
Urol1992;147:846-51
Mettlin C, Littrup
PJ, KaneRA, Murphy
GP, Lee F,chesley A. Relative sensitivity and specificity
of
serum prostate specific antigen(PSA) level
compared withage-referenced PSA,
PSA
density, andPSA
change. Cancer 199 4:7 4: 161 5-20Djavan B, ZloLta AR, Byttebier G, Shariat S, Omar M,
Schulman CC, Marberger
M.
rostate specitic antigendensity
of
the transition zonefor
early
detectionof
prostate cancer. JUrol
1998;160:411-419Cotlins
GN,
Lee RJ,
McKelvie GB,
Rogers CAN,Hehir
M.
Relationship between prostate
specitic antigcn, prostate volume and age in benign prostate.Br
J
Urol
1993;71:445-50l3
t4
6.7
ll
t2
r5
l6
9
t7
8.