Endocrinology is an expanding science with new concepts and ideas appearing in the literature almost daily. The term “endocrine” denotes internal secretion of biologically active substances. Basically, the endocrine system uses hormones to convey information between different tissues. Hormones are released by endocrine glands and transported through the bloodstream to tissues where bind to specific receptor molecules and regulate the target tissues function. In addition to this traditional views, hormones can also act locally by binding to receptors that are expressed by cells that are close to the site of release, remain in the membranes of the one cell, acts on receptors located in the same cell, or can act inside the cell without being released. The action is called paracrine, juxtacrine, autocrine, or intracrine.
In this block, we will learn about the basic of hormone synthesis, release and action, continue with discussing of each endocrine organs and their hormones and diseases including pituitary organ and disorders, diabetes mellitus, lipid metabolism, energy balance: obesity and metabolic syndrome, thyroid and parathyroid gland and disorders, adrenal gland and disorders, and also congenital hypothyroid and ambiguous genital.
This block will take 16 meeting to be completed, each meeting consist of introductory lecture continued by individual learning, single group discussion and self assessment, ending with plenary session. In each topic there will be a list of tasks to discuss which some of them are based on a case that commonly find in clinical practice. There will also a simple clinical problem that you need to discuss and respond, each part will be given a cut of clinical information for you to be responded.
Evaluation in this block will be formative and summative. The formative evaluation is directive and will take as checklist and peer assessment, while summative will be conducted at the end of this block.
We believe that the basic of endocrinology that you will learn in this block will impulse you to learn more about it to help you dealing with endocrine problems in patients.
Good luck, Planner team
List
Page
no.
1. Cover2. Preface 2
3. List of Contents 3
4. Planners Team 4
5. Facilitators 5
6. Seven General Core Competency 6
7. Curriculum Block: The endocrine system, metabolism, and disorders 7
8. General Learning Outcome 10
9. Time Table 11
10. Meeting of student representatives 14
11. Assessment method 14
12. Content outline 15
13. Learning Tasks 19
14. Problem Based Learning 31
15. Clinical skills 32
16. References 38
17. Standard of medical competence 39
18. Block evaluation form 40
19. Paper (article review) format 43
20. Article review assessment form 45
21 Final examination question plan 46
2. LIST OF CONTENT
No. NAME DEPARTEMENT PHONE
1. Dr. dr. Made Ratna Saraswati, SpPD-KEMD (Head)
Internal Medicine 08123814688 2. Dr. dr. Desak Made Wihandani, M.Kes
(Secretary)
Biochemistry 081338776244
3. Dr. IGN Mayun, PHK Histology 08155715359
4. Prof.Dr.dr. Ketut Suastika,SpPD-KEMD
Internal Medicine 0811380916 5. Prof.Dr.dr. AAG
Budiartha,SpPD-KEMD
Internal Medicine 0811398205 6. Dr. dr. Wira Gotera,SpPD-KEMD Internal Medicine 08155736480 7. Dr. Pande Dwipayana, SpPD Internal Medicine 08123657130 8. Dr. Made Arimbawa, SpA Pediatric 081338596115
9. Dr. I Wayan Bikin Suryawan, SpA Pediatris 081338465525 10. Dr. I Wayan Surudarma, M.Si Biochemistry 081338486589 11. Dr. IA Dewi Wiryanthi, M.Biomed Biochemistry 081239990399
Regular Class
NO NAME GROUP DEPT PHONE ROOM
1 dr. Ni Nyoman Mahartini, Sp.PK A1 Pathology Clinical 081337165577 3R.3.01rd floor
2 dr Ni Nyoman Metriani Nesa, M.Sc.,Sp.A A2 Pediatric 081337072141 3R.3.02rd floor
3 dr. I Dewa Ayu Inten Dwi Primayanti, M.Biomed. A3 Fisiology 081337761299 3R.3.03rd floor
4 dr. I Wayan Surudarma, M.Si A4 Biochemistry 081338486589 3R.3.04rd floor
5 dr. I Wayan Niryana, Sp.BS, M.Kes. A5 Surgery 08179201958 3R.3.05rd floor
6 Dr.dr. Susy Purnawati, MKK A6 Fisiology 08123989891 3R.3.06rd floor
7 dr. Anak Agung Ayu Yuli Gayatri, Sp.PD A7 Interna 08123803985 3R.3.07rd floor
8 dr. I Gede Ngurah Harry WijayaSurya, Sp.OG A8 Obgyn 0814386935 3R.3.08rd floor
9 Dr. dr. Made Sudarmaja, M.Kes A9 Parasitology 08123953945 3R.3.20rd floor
10 dr. I Wayan Juli Sumadi, Sp.PA A10 PathologyAnatomy 082237407778 3R.3.21rd floor
11 dr. Anak Agung Mas Putrawati Triningrat, Sp.M (K) A11 Opthalmology 08123846995 3R.3.22rd floor
12 dr. I Gusti Ngurah Pramesemara , M.Biomed A12 Andrology 081338605087 3R.3.23rd floor
English Class
NO NAME GROUP DEPT PHONE ROOM
1 Dr. dr. A.A. Ayu Putri laksmidewi, Sp.S(K) B1 Neurology 0811388818 3R.3.01rd floor
2 dr. Ni Made Renny Anggreni Rena , Sp.PD B2 Interna 081803651656 3R.3.02rd floor
3 dr. I G A Dewi Ratnayanti , M.Biomed B3 Histology 085104550344 3R.3.03rd floor
4 dr. I Ketut Mariadi, Sp.PD B4 Interna 08123853700 3R.3.04rd floor
5 dr. Ida Bagus Alit, Sp.F, DFM B5 Forensic 081916613459 3R.3.05rd floor
6 Dr. dr. Made Ratna Saraswati,
Sp.PD-KEMD-FINASIM B6 Interna 08123814688
3rd floor R.3.06
7 dr. Anak Agung Wiradewi Lestari , Sp PK B7 PathologyClinical 08155237937 3R.3.07rd floor
8 dr. Putu Budhiastra, Sp.M(K) B8 Opthalmology 085238238999 3R.3.08rd floor
9 dr. Ida Ayu Kusuma Wardani, Sp.KJ, MARS B9 Psychiatry 08123813831 3R.3.20rd floor
10 dr. Sri Laksminingsih Sp. Rad A10 Radiology 08164745561 3R.3.21rd floor
11 dr. Tjok. Istri Anom Saturti, Sp.PD A11 Interna 081916253777 3R.3.22rd floor
12 dr. I Made Suka Adnyana, Sp.BP-RE B12 Surgery 081236288975 3R.3.23rd floor
1. Patient care
Demonstrate capability to provide comprehensive patient care that is compassionate, appropriate, and effective for the management of health problems, promotion of health and prevention of disease in the primary health care settings.
2. Medical knowledge base
Mastery of a core medical knowledge which includes the biomedical sciences, behavioral sciences, epidemiology and statistics, clinical sciences, the social aspect of medicine and the principles of medical ethics, and apply them
3. Clinical skill
Demonstrate capability to effectively apply clinical skills and interpret the findings in the investigation of patient.
4. Communication
Demonstrate capability to communicate effectively and interpersonally to establish rapport with the patient, family, community at large, and professional associates, that results in effective information exchange, the creation of a therapeutically and ethically sound relationship.
5. Information management
Demonstrate capability to manager information which includes information access, retrieval, interpretation, appraisal, and application to patient’s specific problem, and maintaining records of his or her practice for analysis and improvement
6. Professionalism
Demonstrate a commitment to carrying out professional responsibilities and to personal probity, adherence to ethical principles, sensitivity to a diverse patient population, and commitment to carrying out continual self-evaluation of his or her professional standard and competence
7. Community –based and health system- based practice
Learning
Outcome Learning Objectives
Educati-onal strategy Learning Resourc es Student assess ment 1. Comprehend
the hormone action
1.1. Describe the transport of hormone in the blood
1.2. Describe the control of hormone secretion
1.3. List the endocrine disease
1.4. Mention the therapeutic strategies in endocrine disorders 0 Intro.le c 1 IL 2 SGD 3 Pleno Refferen ces MCQ
2. Summarize the pituitary gland function and provide initial management and/or refer patient with pituitary disorders
2.1. Recognize the anatomy of pituitary 2.2. Summarize the pituitary hormone
axis
2.3. Recognize the type of pituitary tumor and differential diagnosis of pituitary tumor
2.4. Interpret the endocrine tests of hypothalamic-pituitary function 2.5. Describe the clinical features of
pituitary adenoma
2.6. Summarize the course and the condition associated with pituitary adenoma, including prolactinoma, acromegaly, gigantisme, growth hormone deficiency.
2.7. Summarize the normal physiologic hormone function of posterior pituitary 2.8. Describe the clinical features of
diabetes insipidus 4 Intro.le c 5 IL 6 SGD 7 SE 8 Pleno MCQ
3. Summarize the insulin action, provide initial management and/or refer patient with diabetes mellitus (DM)
3.1 Recognize the characteristics of pancreas and the secretory product associated with each cell type 3.1. Understand major stimuli and inhibitors of insulin secretion. Summarize the cellular mechanism involved in glucose-induced insulin secretion
3.2. Understand major biologic actions of insulin and the target organs. Able indicate which metabolic pathways of fuel metabolism are affected by insulin
3.3. Explain how the blood glucose control by insulin
3.4. Recognize the major biologic actions of glucagon and the target organs, indicate which metabolic pathway of
9 Intro.le c 10 IL 11 S GD 12 Pl eno PBL 13 MCQ
6. CURRICULUM BLOCK:
3.5. Summarize the pathophysiologic basis for the major symptoms of diabetes mellitus
3.6. Mention the diagnostic criteria of prediabetes and diabetes
3.7. Describe the clinical features of type 1 and type 2 diabetes and other types of diabetes
3.8. Summarize the pathogenesis of beta cell dysfunction and insulin resistance (glucose toxicity and lipotoxicity of the beta cell)
3.9. Recognize the acute and chronic complication of diabetes
3.10.Plan the prevention of type 2 diabetes
3.11.Plan the strategy of therapy in diabetes
3.12.Recognize the drugs use in treatment of diabetes (insulin secretogogues, insulin sensitiziser,
thiazolidinediones, alfa glucosidase inhibitor)
3.13.Summarize the acute and chronic complication of diabetes
3.14.Plan the management of hypoglycemia and acute hyperglycemia
4. Summarize and select the appropriate drug in patient with lipid metabolism disorders
4.1. Summarize the lipid transport and the role of plasma lipoprotein
4.2. Recognize the disorders of lipoprotein metabolism
4.3. Summarize the mechanism of action of drugs in lipid disorder
4.4. Describe the prevention of lipid disorder
4.5. Plan a rational drugs treatment regimen based on a set of baseline serum lipid values
14 In tro.lec 15 IL 16 S GD 17 Pl eno 18 C BL MCQ
5. Summarize the energy balanced and heat metabolism, and provide management in patient with obesity and metabolic syndrome
5.1. Summarize the mechanism of heat production and body heat loss 5.2. Summarize the energy metabolism 5.3. Define the criteria obesity
5.4. Describe the pathogenesis of obesity 5.5. Recognize the complication of
obesity
5.6. Define the criteria of metabolic syndrome
6. Provide initial management and/or refer patient with thyroid disorders
6.1. Summarize the organization of the thyroid and secretory cells present in thyroid
6.2. Recognize the function of a thyroid follicle cells and follow the different process involved in this function with particular emphasis on the location of each action within the cell or follicle 6.3. Summarize the biosyntesis, transport,
and autoregulation of thyroid hormone
6.4. Explain the thyroid hormone action 6.5. Recognize the disorder of thyroid
gland, including problem of over/undersecretion and thyroid nodule
6.6. Describe the clinical features (symptoms, signs, and laboratory findings) and the management of Grave’s disease
6.7. Describe the clinical features and management of hypothyroidism
24 In tro.lec 25 IL 26 S GD 27 P leno 28 C BL MCQ
7. Summarize the mineral metabolism (calcium and phosphate) and parathyroid hormone functions
7.1. Summarize the mineral metabolism, including calcium and phosphate and the rule of hormones
7.2. Describe the secretion and action of PTH
7.3. Summarize the rule of PTH, Ca, vit D, and calcitonin. 29 In tro.lec 30 IL 31 S GD 32 P leno
8. Provide initial management and/or refer patient with adrenal disorders
8.1. Summarize the regulation of synthesis and secretion of cortisol, aldosterone, and the weak androgen DHEA.
8.2. Summarize the major actions of glucocorticoid on metabolism, inflammation, permissive effects and the stress concept..
8.3. Summarize the mechanisms of action for mineralocorticoids
8.4. Summarize the pathophysiology and clinical features of cushing syndrome 8.5. Recognize the diagnostic test for
cushing syndrome 33 In tro.lec 34 IL 35 S GD 36 P leno
9. Provide initial management and/or refer patient with congenital hypothyroid and ambiguous
9.1. Recognize clinically, laboratory and provide initial management, and refer patient with abnormalities in sexual determination and differentiation
41
42 Note: Intro. Lec = Introductory lecture 0 IL = Individual learning
1 SGD = Single group discussion 2 Pleno = Plenary lecture
Mastery of Basic Knowledge with Its Clinical and Practical Implication
1. Comprehend the hormone action
2. Summarize the pituitary gland function, provide initial management, and/or refer patient with pituitary disorders
3. Summarize, provide initial management, and/or refer patient with diabetes mellitus 4. Summarize and select the appropriate drugs in patient with lipid metabolism
disorders
5. Summarize the energy balanced and heat metabolism, and provide management in patient with obesity and metabolic syndrome
6. Provide initial management and/or refer patient with thyroid disorders
7. Summarize the mineral metabolism (calcium and phosphate) and parathyroid hormone function
8. Provide initial management and/or refer patient with adrenal disorders
9. Provide initial management and/or refer patient with congenital hypothyroid and ambiguous genital
Skills
1. History taking
2. Physical examination of metabolic syndrome (waist circumference, body mass index), thyroid nodule
3. Interpreting the laboratory result of blood sugar, A1C, lipid profile, hormone level 4. Communication with patient, family and community
5. Assessing data base, extracting relevant information Personal behavior
Awareness to:
1. Lifestyle as a risk factors of diabetes mellitus and metabolic syndrome
2. Early treatment and proper management of metabolic disease to prevent chronic complication of diabetes mellitus, metabolic syndrome, and other hormonal disorder. Community aspect:
1. Risk assessment and disease screening of diabetes mellitus and metabolic syndrome
2. Cost effectiveness of prevention, screening, and treatment of the disease 3. Utilization of health system facilities
4. Health prevention and health promotion
Day Date Topic Learning
situation English Class Regular Class PIC 1 Monday, Oct, 26, 2015 Introduction (The hormone action) Intro. Lect IL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Suastika/Ratna
2 Tue, Oct, 27, 2015
Histology and Anatomy of the endocrine system
Intro. Lect Intro. Lect IL & L task SGD SP Pleno 08.00-08.45 08.45-09.30 09.30-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-09.45 09.45-10.30 10.30-12.30 12.30-14.00 14.00-15.00 15.00-16.00 Yuliana Mayun 3 Wed, Oct, 28, 2015
The pituitary gland
and disorders Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 Ratna 4 Thursday , Oct, 29, 2015
Carbohydrate
metabolism Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Dewi Wiryanthini 5 Friday, Oct, 30, 2015 Insulin secretion,
insulin action. Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Suastika/Ratna 6 Monday, Nop, 02, 2015 Pathogenesis and diagnosis of diabetes Intro. Lect Intro. Lect IL & L task SGD SP Pleno 08.00-08.45 08.45-09.30 09.30-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.30-10.15 10.15-11.00 11.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Suastika/Ratna 7 Tue, Nop,03, 2015 Management of
Diabetes Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Suastika/Pande 8 Wed, Nop, 04, 2015 PBL 1
Clinical skills 1: Insulin injection SGD Pleno SP Clinical Skills 08.00-09.30 09.30-11.30 11.30-12.00 12.00-15.00 11.00-12.30 13.00-15.00 12.30-13.00 08.00-11.00 Budhiarta Pande
9 5 Nop Management of Diabetes in Children
Intro. Lect IL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Bikin/Arimbawa 10 Thursday , Nop, 05, 2015
Acute and chronic complication of diabetes
Intro. Lect IL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Budhiarta
11 Monday, Nov, 09, 2015
PBL2
Clinical skill 2: self monitoring blood glucose SGD Pleno SP Clinical Skills 08.00-09.30 09.30-11.30 11.30-12.00 12.00-15.00 11.00-12.30 13.00-15.00 12.30-13.00 08.00-11.00 Wiragotera Pande 12 Tue, Nov, 10, 2015
Lipid metabolism Intro. Lect IL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Surudarma 13 Wed, Nov, 11, 2015 Lipid metabolism
and disorder Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Suastika/Pande 14 Thursday , Nov, 12, 2015 The energy
balance Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Adiputra 15 Friday, Nov, 13, 2015 PBL3
Clinical skills 3: Diabetic Foot Examination SGD Pleno SP Clinical Skills 08.00-09.30 09.30-11.30 11.30-12.00 12.00-15.00 11.00-12.30 13.00-15.00 12.30-13.00 08.00-11.00 Suastika/Ratna Pande 16 Monday, Nov, 16, 2015 Obesity and metabolic syndrome Intro. Lect IL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Budhiarta 17 Tue, Nov, 17, 2015 Iodine metabolism, and thyroid hormon function
Intro. Lect Intro. Lect IL & L task SGD SP Pleno 08.00-08.45 08.45-09.30 09.30-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.30-10.15 10.15-11.00 11.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Wihandani 18 Wed, Nov, 18, 2015 Calcium, phosphate, and vitamin D metabolism, PTH function Intro. Lect Intro. Lect IL & L task SGD SP Pleno 08.00-08.45 08.45-09.30 09.30-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.30-10.15 10.15-11.00 11.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Sutadarma 19 Thursday , Nov, 19, 2015
The thyroid and parathyroid hormone disorders
Intro. Lect Intro. Lect IL & L task SGD SP Pleno 08.00-08.45 08.45-09.30 09.30-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.30-10.15 10.15-11.00 11.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Wira Gotera 20 Friday, Nov, 20, 2015
The Adrenal gland and adrenal hormone function
21 Monday, Nov, 23, 2015
Cushing syndrome
Adrenal Crisis Intro. LectIL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Ratna 22 Tue, Nov, 24, 2015 Congenital hypothyroid and disorder of sex development (DSD)
Intro. Lect IL & L task SGD SP Pleno 08.00-09.00 09.00-11.30 11.30-13.00 13.00-14.00 14.00-15.00 09.00-10.00 10.00-12.30 13.30-15.00 12.30-13.30 15.00-16.00 Bikin/ Arimbawa 23 Wed, Nov, 25, 2015 PBL3
Clinical skills 4: Thyroid Nodule Examination SGD Pleno SP Clinical Skills 08.00-09.30 09.30-11.30 11.30-12.00 12.00-15.00 11.00-12.30 13.00-15.00 12.30-13.00 08.00-11.00 Suastika/Ratna Pande 24 Thursday , Nov, 26, 2015 PBL 4
Clinical Skills 5: Lab result interpretation (case studies) SGD Pleno SP Clinical Skills 08.00-09.30 09.30-11.30 11.30-12.00 12.00-15.00 11.00-12.30 13.00-15.00 12.30-13.00 08.00-11.00 Suastika/Ratna Pande 25 Friday. Nov, 27, 2015
Student project
presentation Pleno 08.00-13.00 08.00-13.00 Lecturers and Fasilitators
26 Monday, Nov, 30, 2015
Meeting of the student representatives
One student from each group discussion will invited to discuss the block activities with members of the block planners every Saturday, in block-coordinator’s room.
Meeting of the facilitators
The meeting between block planners and facilitators will take every Saturday after meeting of the student representatives, in block-coordinator’s room.
Assessment in this thema consists of:
SGD : 5%
Paper (review article) : 15% Final examinations : 80%.
Final exam will be carried out on (Monday, 29th November 2015). There will be 100
questions consisting mostly of Multiple Choice Questions (MCQ) and some other types of questions. The minimal passing score for the assessment is 70.
The requirement for taking the final exam: - join 75% of total student activities
- uniform: white shirt, black trouser/skirt, shoes - bring student ID card with photo
- be present 15 minute before examination starting time
Other than the examination score, your performance and attitude during group discussions will be considered in the calculation of your average final score.
10. ASSESSMENT METHOD
1.
The hormone action
The endocrine system uses hormones to convey information between different tissues. Hormones derive from the major classes of biologic molecules, this can be proteins (including glycoproteins), peptides or peptide derivatives, amino acid analogs, or lipids. Endocrine hormones are part of a large complement of small intercellular signaling molecules.
The system of internal hormone secretion is subject to complex regulatory mechanisms that govern receptor activity and hormone synthesis, release, transport, metabolism, and delivery to the target cells. Hormones bind specifically to hormone receptors and translate the signal into biologic activity. The receptors can be expressed on the cell surface or within the cell.
Hormone response is regulated by hormone concentration. This in turn is governed by hormone production, efficiency of delivery and metabolism. The classic disorders of the endocrine system arise from state of excess or deficiency of hormones, however resistance to hormones also play a role. Disorders of the endocrine system will discuss in each part of the gland.
2. Pituitary gland (and hypothalamus)
The pituitary gland lies on the base of the skull in a portion of the sphenoid bone called the sella tursica. The hypothalamus and pituitary gland form a unit which exerts control over the function of several endocrine glands: thyroid, adrenal, and gonads, as well as a wide range physiologic activities. This unit constitutes a paradigm of neuroendocrinology: brain-endocrine interactions.
The hypothalamic hormones can be divided into those secreted into hyppophysial portal blood vessels and those secreted by the neurohypophysis directly into the general circulation. The hypophysiotropic hormones regulate the secretion of anterior pituitary hormones, include growth hormone-releasing hormone (GHRH), thyrotropin-releasing hormone (TRH), corticotrophin-releasing hormone (CRH), and gonadotropoin-releasing hormone (GnRH). The six major anterior pituitary hormones are adrenocorticotropic hormone (ACTH), growth hormone (GH), prolactin (PRL), TSH, LH, and FSH. The posterior pituitary hormones are antidiuretic hormone (ADH) and oxytocin.
Hypothalamic and pituitary lesions present with a variety of manifestations, including pituitary hyper- and hyposecretion, sellar enlargement, and visual loss.
PRL hypersecretion is the most common endocrine abnormality due to hypothalamic-pituitary disorders, and PRL is the hormone most commonly secreted in excess by pituitary adenoma. GH-secreting adenomas are second in frequency to prolactinoma and cause the classic syndromes of acromegaly and gigantism.
The major effect of ADH is to increase the water permeability of the luminal membrane of the collecting duct in the kidney. Diabetes insipidus is a disorder resulting from deficient ADH action and is characterized by the passage of amounts of very dilute urine.
3. Pancreas and Diabetes mellitus
The pancreas is made up of two functionally different organs: exocrine and endocrine. The major product of exocrine pancreas is the digestive enzims. The endocrine pancreas consists of 0.7-1 million small endocrine glands – the islets of Langerhans – scattered within the glandular substance of the exocrine pancreas. The product of endocrine pancreas are: insulin, glucagon, somatostatin, and pancreatic polypeptide.
Clinical diabetes mellitus is a syndrome of disordered metabolism with inappropriate hyperglycemia due either to absolute deficiency of insulin secretion or a reduction in the biologic effectiveness of insulin (insulin resistance), or both. Type 1 diabetes is the severe form of diabetes mellitus and is associated with ketosis in the untreated state. While type 2 diabetes – previously classified as non-insulin-dependent-diabetes (NIDDM) afflict patient with insulin resistance who generally have relative insulin deficiency. There are also other types of diabetes. Patient with diabetes needs a proper diet, exercise, and also pharmacologic agent, such as insulin or oral anti diabetes. Oral anti diabetes fall into three categories: 1) drugs that stimulate insulin secretion, 2) drug that alter the insulin action, 3) drug that principally affect absorption of glucose.
In most patient with diabetes, a number of pathologic changes occur at variable intervals during the course of the disease. There are also acute complications either cause by hypoglycemia or hyperglycemia.
4
. Lipid metabolism and disorders
The clinical importance of dislipidemia is mainly from the role of lipoprotein in atherosclerosis. Because lipid are relatively insoluble in water, they are transported in association with proteins. The simplest complexes are those formed between unesterified or free, fatty acids (FFA) and albumin, which serve to carry the FFA from peripheral adipocytes to other tissue. Cholesterol in the atheroma originates in circulating lipoprotein. Atherogenic lipoproteins include low-density (LDL), intermediate density (IDL), very low density (VLDL), and Lp(a) species.
Initial treatment in all forms of hyperlipidemia is an appropriate diet. Patient with severe hypercholesterolemia will require drug therapy. The increased risk of acute pancreatitis associated with hypertriglyceridemia is another indication for intervention.
5.
Energy balance and metabolism disorder, obesity and metabolic syndrome
The energy balance equation is dynamic and this may explain why there is a long-term relative stability of body weight and fat stores. The three determinants of body fat stores are intake, expenditure, and nutrient partitioning, each under complex control.
Obesity is a disorder of body composition defined by relative or absolute excess of body fat and characterized by several remarkable features. It is difficult to certain the relationship between obesity and disease, because it is confounded by many metabolic and hormonal that either contribute to or derive from excess adiposity. Obesity and abdominal obesity are closely associated with dyslipidemia, hypertension, insulin resistance, and diabetes. The abdominal adipose tissue has several features of interest in connection with the metabolic syndrome. This is the reason of The ATP III definition of the metabolic syndrome lists the waist circumference as a diagnostic factor of the metabolic syndrome. 6
. Thyroid gland
Thyroid gland is the largest organ specialized for endocrine function in the human body. The major function of thyroid gland is to secrete a sufficient amount of thyroid hormones, which promote normal growth and development, regulate a number of homeostatic function including energy and heat production.
7. Mineral metabolism and parathyroid gland
Four parathyroid glands located adjacent to the thyroid gland. The two superior glands are usually found near the posterior aspect of the thyroid capsul, and the inferior glands are located most often located near the inferior thyroid margin. The parathyroid gland composed of epithelial cell and stromal fat. The epithelial cell consist of chief cell and oxyphil cell, both contain of parathyroid hormone (PTH). The function of PTH is to regulate serum calcium levels by concerted effects on three target organs: bone, intestinal mucosa, and kidney.
8.
Adrenal gland and disorders
The adrenal cortex produces many steroid hormones, the most important are cortisol, aldosterone, and the adrenal androgen. Disorders of the adrenal glands lead to a classic endocrinopathies such as Cushing’s syndrome, Addison’s disease, hyperaldosteronism and the syndrome of congenital adrenal hyperplasia.
The adrenal medulla is a specialized part of the symphathetic nervous system that secretes catecholamines. Pheochromacytoma is tumors that arise from the adrenal medulla, may present at any age. Screening for pheochromacytoma should be considered for such patients with severe hypertension and also for hypertensive patients with suspicious symptoms, e.g., headache, palpitation, sweating episodes, or unexplained bouts of abdominal or chest pains.
9.
Congenital hypothyroid and ambiguous genital
Congenital hypothyroidism (CH) occurs in babies who are born without the ability to produce adequate amounts of thyroid hormone. Thyroid hormone is important for normal function of all of the body's organs and is essential for normal brain development. CH affects about one in every 3,500 babies. The most common cause of primary CH is dysgenesis (various abnormalities in the formation of the thyroid gland). If detected early a child will develop normally. Treatment is thyroid medication daily. Deficiency of thyroid hormone may result in mental and growth retardation. If CH is not diagnosed and treated early in life, most infants will still appear clinically normal before 3 months of age, by which time some brain damage has usually occurred.
Symptoms or signs, when present, may include prolonged neonatal jaundice, constipation, lethargy and poor muscle tone, poor feeding, a large tongue, coarse facies, wide fontanelle, distended abdomen and umbilical hernia. Ideally a neonatal screening (TSH screening) for CH should be routinely done in all children as treatment of affected infants within 45 days of birth leads to normal mental development. The TSH should be done 3 to 5 days after birth and patients with TSH levels more than 20-25 mU/L should be assessed further.
Disorder of sex development
(
DSD
)
In human sexual development, the female phenotype represents the default pathway. therefore, a failure of testis determination results in the development of the female phenotype, while genetic alterations resulting in partial testicular development can give rise to a wide spectrum of masculinization. In addition to defects in peptide hormones and their receptors, timing of hormonal exposure is also critical to appropriate development. Genital anomalies are estimated to occur in 1 in 4500 births.
Disorder of sex development
(
DSD
) is a medical term referring to "congenital
conditions in which development of chromosomal, gonadal, or anatomical sex is atypical. Patients with ambiguous genitalia have disorders of sexual development (DSD), that previously termed intersex conditions. The term DSD in lieu of potentially pejorative and confusing terms such as intersex, pseudohermaphroditism, hermaphroditism, sex reversal, and gender-based diagnostic labels. For clinical purposes, DSDs in newborns are classified according to karyotype. Based on the various steps of sex differentiation and development, we suggest the following classification: (A) DSD with a 46,XY karyotype (formerly referred to as male pseudohermaphroditism, undervirilization of an XY male and undermasculinization of an XY male. In 46,XY DSD the bipotential gonads differentiate to variable degrees into testes), (B) DSD with a 46,XX karyotype (formerly referred to as female pseudohermaphroditism or masculinization of an XX female. In 46,XX DSD the bipotential gonads usually differentiate into ovaries but with abnormally increased androgen exposure and (C) DSD with an unusual karyotype such as mosaicism (45,XO/46,XY or 46,XX/46,XY), transposition of genes (46,XX, SRY+) or chromosome deletions that include one of the genes necessary for sex determination and differentiation.For optimal clinical management of individuals with DSD, the consensus statement recommends the following: Avoid gender assignment in newborns before expert evaluation. Conduct evaluation and long-term management at a center with an experienced multidisciplinary team, including pediatric subspecialists in endocrinology, surgery or urology or both, psychology/psychiatry, gynecology, genetics, neonatology, and, if available, social work, nursing, and medical ethics. Give a gender assignment to all individuals. Openly communicate with patients and families and encourage their participation in decision making. Respect patient and family concerns, and address them in strict confidence.
10. Drug treatment in endocrine disorders
Case : A woman with decreased body weight
A woman 22 year old, complained of reduced body weight aggressively in a few weeks, tremble, and diarrhea 2 or 3 times a day. She has slightly enlargement of her neck. Laboratory result showed high level of thyroid hormone (FT4/free thyroxine) and very low level of thyroid stimulating hormone (TSHs).
Learning Task:
1. Explain the classical endocrine glands and each hormone be secreted.
2. Explain the concept of endocrine, paracrine, and autocrine in hormone action; and each examples of hormone or molecules
3. Explain the concepts of ligand, receptor, effector, and second messenger
4. Based on location of receptor in hormone action, how many kinds of hormone are there? Explain briefly the mechanism each hormone action and example of its hormones
5. Explain two major types of control of endocrine gland function
6. Associated with hypothalamic-pituitary-target gland system, what level of the disorder was occurred (at hypothalamus, pituitary or thyroid gland) in above case? Draw a figure of the disorder and explain briefly.
Self assessment:
1. What is the hormone function in our body, and give example of hormone for each function?
2. Explain the differences between signaling by hormones, local mediators, and neurotransmitters!
3. Describe the transport of hormone in the blood!
4. What do you know about ligand, receptor, effector, first-second messenger? 5. Explain about the control of hormone secretion! Give an example of feed back
negative mechanism of hormone secretion! 6. Make a list of the endocrine disease!
Learning Task:
1. Discuss the structure of thyroid and parathyroid gland, include the vascularisation and identify their position in the neck
2. Discuss anatomical structures of pituitary gland and hypothalamus 3. Discuss anatomical structures of pancreas
4. Discuss anatomical structures of adrenal gland Self assessment:
1. Decribe the structure of thyroid and parathyroid gland, include the vascularisation and identify their position in the neck
2. Describe anatomical structures of pituitary gland and hypothalamus 3. Describe anatomical structures of pancreas
4. Describe anatomical structures of adrenal gland
12. LEARNING TASKS
Day 1.
The hormone action
Learning Task Histology:
1. Discuss the general characteristic of endocrine glands!
2. Discuss pancreas as exocrine and endocrine organ! Types of cells in its endocrine part and hormone produced.
Case : a woman with increasing shoe size
A 40 year old female has noticed an increase in her shoe size from 38 to 42, and her weight also increased excessively from 62 to 84 kg. Her menstrual period has stopped 6 months ago.
Physical examination found her 158 cm. Although a large woman, she doesn’t look obese. Her blood pressure was 140/80 mmHg. Neck demonstrated diffuse thyromegaly, but the TSHs and FT4 test was normal. Her face demonstrated thickening of the nasolabial fold and prominence of the supraorbital ridge. Compare to her picture 5 years before, her face showed a striking change in facial feature. She did not show hirsutism. Her hands and feet had a rubbery consistency.
Learning task:
1. What is the most likely disorder of this woman? 2. What may cause this disorder?
3. What laboratory and radiology test would you do for the patient to workup the diagnosis?
4. Is she has thyroid problem? Why? 5. Why she stopped menstruating? Self assessment:
1. Explain the hypothalamus – pituitary – target organ axis.
2. Summarize the course and the condition associated with pituitary adenoma, including prolactinoma, acromegaly, gigantisme, growth hormone deficiency. 3. Summarize the normal physiologic function of posterior pituitary hormone. 4. Describe the clinical features of diabetes insipidus.
Learning Task:
1. Red blood cell is the simplest cell in the body in term of its structure and metabolism. Please elaborate that statement!
2. What are the differences of carbohydrate metabolism in red blood cell compare to brain cell or hepatocyte?.
3. Explain what happened during investment stage, splitting stage and yield stage on glycolisis.
4. What enzymes are regulating glycolisis and what are their functions?
5. Explain about glycogenesis, glycogenolysis and hormonal control of glycogenolysis! 6. Where is Pentosa phosphate pathway started and what are the main products?
Explain why its called “shunt”?
7. How many ATP produced from one molecule glucose metabolized at Kreb’s cycle?
Day 3.
The Pituitary gland and disorders
Self assessment:
1. Explain, why is NaF as the most preferred anticoagulant used for glucose examination?
2. Like in Munir case, as indicated by autopsy results undergone at Netherland, revealing arsenic concentration above normal level as the cause of death. Explain, why arsenic can be so fatal if exist in high concentration in blood?
3. Explain, how the mechanism of bacteria extermination by phagocytosis? 4. Why hemolytic anemia can be caused by deficiency of G6PDH enzyme? 5. Explain about HbA1c and its normal concentration.! Why normal blood glucose
concentration result not directly follow by normal concentration of HbA1c? 6. Explain pathogenesis process of chronic complication of DM?
7. Explain the role of glycated protein to longterm complication of DM
Case : a man with weight loss and polyuria
Data 1
Mr. AB, 43-year-old male has no prior medical problems feel fatigue this last few months. On further questioning, he admitted having incessant thirst, and polyuria over the last month with a 6-kgs weight loss (before he was 76 kg, 160cm in height). He denied having any history of diabetes. He did not realize any family history with diabetes.
Generally examination is unremarkable. A rountine urinalysis demonstrates 4+ glycosuria. Learning Task:
1. Does this man has diabetes mellitus? a. Explain why and why not?
b. What are other conditions may cause glycosuria? c. How to establish the diagnosis of diabetes? Data 2
A glucometer reading was unmeasureable. This was confirmed by blood glucose serum 580 mg/dL. He does not feel ill and this week he planned to start his new job.
Learning Task:
2. Does he have diabetes mellitus?
If so, does he have type 1 diabetes or type 2 diabetes? Self assessment:
1. Explain the cells types and hormone secreted by islets of Langerhans! 2. Describe how insulin secretion is regulated!
3. Describe the metabolic action of insulin!
4. Describe how glucagon release is regulated and summarize its main action! 5. What is the major symptom of diabetes mellitus?
6. Mention the diagnostic criteria of prediabetes and diabetes!
7. What is the clinical features difference of type 1 and type 2 diabetes?
Case: A man with diabetes
Mr. C, 45-year-old, has diabetes since 3 months ago, at that time his random blood glucose was 212mg/dL .
His glucometer reading yesterday was unmeasureable. This was confirmed by blood glucose serum 580 mg/dL. He feels like lack of energy during the day, and difficulty to sleep due to frequent urinating. Generally examination is unremarkable.
Learning Task:
1. What should you do for Mr C:
a. Should you admit him to the hospital or send him home with some medication? Explain your answer.
b. What is your plan for treatment?
c. What is the choice of treatment for his diabetes: insulin or oral antidiabetes? Self assessment:
Explain the management of diabetes! Refer to the available guideline.
PBL 1: A man with high blood sugar, fever and vomiting Introduce trigger
A man 52 years old, government employee, visited a general practitioner due
to loss of body weight about 7 kg in last two months.
a. Search any information of some kind of health problems or diseases
related relatively weight loss abruptly
b. How the mechanisms of weight loss in each suggested diseases
Case: A man with diabetes for 12 years.
Mr. B has been diagnosed with diabetes for 12 years. His fasting blood sugar normally between 90-120 mg/dL, with medication: glibenclamide 5 mg twice a day. Sometime in the day, he feels shaky and trembeling, followed by blurred visión and headache, which normally resolved after he has lunch.
Last laboratory result showed A1C was 9.1%, urinalysis revealed a proteinuria +1. Other result, including lipid profile, renal function and liver function, still in aceptable range. Learning Task:
1. What is the acute complication of diabetes? 2. What is the chronic complication of diabetes?
3. In above case, list the possible acute and chronic diabetes complication.
4. Mention the 4 strategy therapy in diabetes and explain the concept of each strategy! 5. List the name of four major classes of OAD (oral anti diabetic) agents, and describe
the mechanism of action of each class.
Day 8.
PBL 1 and Clinical skills 1: Insulin injection
n
Day 7.
Management of Diabetes
Day 9.
Acute and chronic complication of diabetes
Case: A lady with hypothyroid
Ms. N has been diagnosed with hypothyroid for 2 years, after a total thyroidectomy. She has levothyroxine a day for her thyroid hormone replacement.
Learning Task:
1. Describe the principles of hormonal and anti hormonal drugs used for patient with endocrine disorders
2. Describe the side effects of hormonal and anti hormonal drugs used for patient with endocrine disorders
3. In above case, when would be the best time to take levothryoxine? 4. Differentiate pharmacodynamic of insulin and OAD
5. Differentiate pharmacokinetic of insulin and OAD
6. Make a scheme which summarized the differences between pharmacodynamic and pharmacokinetic of insulin and OAD
7. Describe pharmacodynamics and pharmacokinetic of hypolipidemic drugs
Learning Task:
1. Explain about beta and alpha oxidation of lipid metabolism! 2. Explain the relation between carbohydrate and lipid metabolism!
3. What are the function of carnitin and what happened if carnitin deficiency occured? 4. Explain the interrelation between obesity and lipid metabolism!
Case Data 1
A 45 years, male patient with history of diabetes type 2 since 5 years carried out routine laboratory examination. Serum total cholesterol result is 259 mg/dL
Learning Task:
What other laboratory assay you will suggest to patient to complete lipid profile of this patient? How to interpret each of it?
Data 2
Lipid profile results as follow : Total cholesterol 250 mg/dL Cholesterol LDL 110 mg/dL Cholesterol HDL 17 mg/dL Trigliserida 210 mg/dL
Day 12. Lipid metabolism
Day 11.
PBL 2 and Clinical skills 2: Self monitoring blood
glucose
n
Day 13.
Lipid metabolism disorders
Day 10.
Drug treatment in endocrine disorders
Learning task:
1. Interpretate those results!
2. Explain the treatment that you recommend to patient! 3. Explain the targets to manage this patient lipid profile!
Self assessment:
1. Describe the lipid transport and the role of plasma lipoprotein! 2. Mention the disorders of lipoprotein metabolism!
3. List the name of drugs treatment of lipid disorder and describe the mechanism of action of each class!
Learning Task:
1. Explain adenosine triphosphast (ATP) functions as an “energy” in metabolism
2. Explain phosphocreatine functions as an accessory storage depot for energy and as ATP buffer
3. Explain aerobic and unaerobic energy 4. Explain about metabolic rate
5. Explain energy metabolism –factors that influence energy output 6. Describe the mechanism of heat production
7. Explain the body temperature is controlled by balancing heat production against heat loss
8. Explain the mechanism of bodily heat loss 9. Describe the pathogenesis of obesity
Data 1
A 45 years male patient, complain body weakness and sometime difficulty in breathing when sleeping. On physical examination, body weight 92 kg, height 162 cm and waist circumference 105 cm. Patients has 1 brother and 1 sister. His brother died due to heart attack at age of 52 year. All of them are fat since they were child. Patient weight increases since he married and starts to neglect exercise.
Learning Task:
1. What are the problems of this patient?
2. What are factors contribute to those problems?
3. What are the possible risks that this patient will face in the future? Data 2
Further examination reveals that blood pressure 145/90 mmHg, fasting blood glucose concentration 129 mg/dl, 2 hour post prandial blood glucose concentration 185 mg/dl, trigliserida 165 mg/dl, cholesterol-HDL 32 mg/dl and cholesterol LDL- 235 mg/dl.
Day 14.
The energy balance
Day 16.
Obesity and metabolic syndrome
Learning Task:
1. What syndrome is this patient suffered?
2. How the mechanism that this syndrome could occur?
3. What factors contribute to the increase of blood glucose in this patient? 4. Explain briefly about the management of this patient!
Data 1 .
A 36 years male patient, complain snoring and difficulty in breathing when sleeping. Almost all patient family are fat. Patient himself alredy fat since he was child and his body weight even more increasing after he married. His present body weight is 98 kg with height 165 cm, and waist circumference 108 cm. Patient feel less self confidence due to dark appearance on the neck skin just like untreated well..
Learning Task:
1. What are the problems of this patient?
2. What are additional data that you need to diagnose this patient? Data 2.
Patient blood pressure 150/90 mmHg.
Random blood glucose concentration 130 mg/dL, 2 hour post prandial 180 mg/dL, but he never complain frequent urinating or thirsty. Trigliserida 170 mg/dL, HDL 25 mg/dL, cholesterol LDL 250 mg/dL
Learning Task:
1. What is the síndrome that this patient suffered? 2. What are the causes of this syndrome?
3. Explain the management of this patient? Self assessment:
1. Define the criteria of obesity for Asia Pacific region!
2. Explain the pathogenesis of obesity (nutrient balance or homeostatic model)! 3. What is the complication of obesity?
4. Mention the criteria of metabolic syndrome by adult treatment panel III – National Cholesterol Education Program (ATP III-NCEP)!
5. Explain the treatment of metabolic syndrome!
Learning Task:
1. Explain step by step the synthesis of thyroid hormone !
2. What is thyroglobulin? What is the function in synthesis of thyroid hormone? 3. What is meant by iodinize and deiodinize in thyroid gland?
4. Explain the secretion process of tiroksin! 5. Explain the transport of thyroid hormone! 6. Explain how thyroid secretion is controlled 7. Explain the main action of thyroid hormone
8. Describe the main consequence s of abnormal thyroid function
Day 17.
Iodine metabolism, thyroid hormone synthesis and
Self assessment:
1. Explain about the axis of hypothalamic-pituitary-thyroid system and its regulatory function of thyroid hormone secretion!
2. Describe the schema of biosynthesis of thyroid hormone! 3. Explain about transport of thyroid hormone in the blood!
Learning Task:
1. Explain about secretion and mechanism of action of parathyroid hormone 2. Explain about the synthesis and mechanism of action of vitamin D.
3. What do you know about calcium as second messenger and why extracellular (Ca++)
in tightly regulation (main consequences of abnormal Ca control)?
4. List the essential mineral and vitamin for normal bone growth and osteoporosis prevention!
5. Describe the main consequence s of abnormal parathyroid function
Case : a lady with increasing body weight and first degree AV block
Data 1.
A 45 year female patient come clinic with complaining weakness, difficult to concentrate and increase of body weight. On physical examination, blood pressure 100/70mmHg, pulse 52 x/minutes,regular with edema at both legs. Laboratory result reveal that total cholesterol 460 mg/dL.
Learning Task:
1. What is the diagnose of this patient?
2. What are other examinations that you need to confirm the diagnose? (3 items) Further laboratory examination reveals FT4, FT3, TSHs concentration below normal value. ECG reveal first degree AV block.
Learning Task:
3. What is the diagnose of this patient?
4. What other examination requiered to locate the disorder? Data 3.
Serum TRH level within normal range. Learning task:
5. What is your conclusion regarding the location of hormonal disorder of this patient? Case: a young female with sweating and decreasing body weight
Data 1.
22 years, young female patient come with palpitation, both hands shaking frequently with
Day 18. The Parathyroid hormone function
Calcium and phosphate metabolism
she eats a lot. She felt her neck enlarge since 3 month but she can’t palpate any lump. She also feel that her eyes are more prominent than her coworkers that made her less confident. Learning Task:
1. What is the possible diagnose of this patienti?
2. What are other examination required to confirm the diagnose?
Data 2.
ECG reveal AF (atrial fibrilation) with fast response 130 times per minutes.
Laboratory examination result FT4 serum concentration is high and TSHs concentration below normal value.
Learning Task:
3. What is the posible diagnose of this patient?
4. What are other examination required to determine the cause of this case? 5. What are your management plan to this patient?
Self assessment:
1. Identify the diseases caused by: over secretion and under secretion of thyroid hormone!
2. Mention the clinical condition associated with thyrotoxicosis!
3. Describe the clinical features (symptoms, signs, and laboratory findings) of Graves’ disease!
4. List the drug treatment of Graves’ disease and explain the mechanism of action and side effect of each drug!
5. Describe the course and complication of hyperthyroidism (thyroid crisis) 6. Describe the diagnostic algorhythm of hypothyroidism
7. Explain about the treatment of hypothyroidism!
Learning Task:
1. Explain the gross structure of the adrenal gland and mention the adrenal hormone produced by each part!
2. Describe the regulation of cortisol synthesis and secretion through hypothalamus, pituitary and adrenal axis!
3. Explain the inflammatory properties of cortisol!
4. Explain the role of physical and emotional stress in cortisol secretion!
Learning Task:
Case: A young lady with moon face
Data 1.
A 22 years,female patient come with complaining her cheek getting fatter (moon face) and in some of her body like shoulder,upper part of her back and tummy, also getting fatter than before. On skin of her tummy also appear lines like pregnant woman.
Blood pressure was 140/90 mmHg, random blood sugar was 220 mg/dL.
Day 20. The Adrenal gland and Adrenal Hormone Function
.
The adrenal gland and adrenal hormone function
Day 21. Cushing Syndrome
Learning Task:
1. What is the possible syndrome that this patient suffered?
2. Is there any additional information that you need from this patient? Data 2.
Before these symptoms appear, she often complains a lot of sneezing and running nose in the morning, along with allergic symptoms whole bodies: redness and itchy. Each time she felt this symptom she always see a dNopor at Primary Health Centre. She has been treated with dexametasone. This tablet worked good on her symptoms. She did not visit the dNopor regularly. Each time she stopped the tablet, symptoms often recurrent. She increased the dose by herself. She prepared herself with this tablet that she bought from pharmacy. Therefore, if she suffered from her allergic symptoms, instead of visited the dNopor, she treated herself.
3. What is the most possible diagnosis to this patient? 4. What would you do to confirm the diagnosis? 5. What is your plan toward for this patient? Self assessment:
1. Mention the classification of cushing syndrome! 2. Explain the pathophysiology of cushing syndrome! 3. Describe the clinical features of cushing syndrome!
Learning Task:
1. Explain factors to determine gender!
2. Explain gender differentiation process intrauterine! 3. Explain about DSD/interseks classification!
4. Explain the etiology of neonatal DSD! Case:
A 23 days baby referred to Child endocrine outpatient clinic with diagnose Ambigous Genitalia. When the baby turns to 14 days, he/she vomiting, less drinking and very weak. One week later he/she vomit again and hospitalized. Laboratory result revealed low natrium
Day 25. Congenital hypothyroid and ambiguous genital
Day 22.
Clinical skill 4: Thyroid gland physical
examination
and student project presentation 1
Day 23. Clinical skills 5: Lab result interpretation and student
project presentation 1
Day 24. Student Project Presentation 3, PBL 4
external genetalia examination finding reveal enlargement of clitoris, hipospadia and unpalpable testicles.
From the following statements, which are TRUE and FALSE?
1. First step must be done is evaluating blood 17-OH progesterone concentration.
2. Chromosome assay unnecessary to be performed.
3. Others supporting evaluation are ultrasound and genitography examination.
4. This baby possibly suffering Congenital Adrenal Hiperflasia (CAH)
5. This baby categorized as 46XX DSD (female pseudhermaphroditism) according to DSD/intersex classification.
6. This baby does not need surgery.
PBL:
PROBLEM BASED LEARNING 2015
BLOCK: ENDOCRINE SYSTEM AND METABOLISSM AND ITS DISORDERS Objective
1. To understand that excessive urination and thirsty is one of chief complaints of patients in medical practice
2. Capable to search underlying diseases related to excessive urination and thirsty 3. To know several diseases as the most important causes of excessive urination and
thirsty and capable to differentiate them based on the probability
4. Capable to confirm diagnosis the certain disease and exclude other diagnosis by history taking, physical examination and supporting studies (electrocardiography, laboratory and imaging studies)
5. Capable to manage the patient as a primary care physician 6. To understand the clinical course of the disease without treatment
Learning Task
There are four sessions to completely discuss the case, starts from distributing the trigger problem at the first meeting and ends by the plenary session to overcome the case problem based on students discussion.
Trigger problem: Excessive urination and thirsty
A female 22 years old, study in university, visited a general practitioner due to excessive urination since last two weeks. She had problem in concentrating to her campus activity since she need to go toilet many times. She was feeling thirsty all the time and almost every 30 minutes she had to drink a bottle of water (about 750cc) and preferred sugary drink. Her body weight lost 2 kg in 1 week.
c. Search any information of health problems or diseases related to excessive urination and thirsty.
d. Explain the mechanisms of excessive urination in each disease that you suggested.
First Session
Small Group Discussion: discuss Task 1a and 1b and prepare group presentation in plenary meeting.
BASIC CLINICAL SKILLS TEACHING PROGRAM BLOCK ENDOCRINE
Topics:
1. Insulin injection
2. Self monitoring blood glucose
3. Measurement of Obesity: Waist circumference and BMI calculation 4. Thyroid gland physical examination
5. Laboratory result interpretation
Clinical Skill 1. Insulin injection
14. CLINICAL SKILLS
Learning task:
1. Define the site of subcutaneous insulin injection
2. Practice preparing and administering insulin using insulin needle 1 cc 1. 8 unit of rapid human insulin
2. Mixed of 6 unit rapid insulin and 14 unit NPH insulin
Clinical Skill 2. Self monitoring blood glucose
Self monitoring blood glucose (SMBG) is an important component of modern therapy for diabetes mellitus. SMBG is recommended for people with diabetes and their health care professionals in order to achieve a specific level of glycemic control and to prevent hypoglycemia.
The test most commonly involves pricking a finger with a lancet device to obtain a small number of blood sample, applying a drop of blood onto a reagent strip, and determining the glood glucose concentration by inserting the strip into a reflectamce photometer for an automated reading.
Test results are then recorded in a logbook or stored in the glucose meter’s electronic memory.
People with diabetes can be taught to use their SMBG to correct any deviations out of a desire range by changing their carbohydrate intake, exercising, or using more or less insulin.
Learning task:
1. Practice measuring blood glucose using glucometer. 2. Below are data of a diabetes patient.
Mr. B, 48 years old, diabetes for 7 years. Now on glibenclamide 5 mg twice a day. He has tried metformin and acarbose for few months, then stopped due to diarrhea.
Body weight 78 kg, height 168 cm. Laboratory result:
- Fasting BS 198 mg/dL, 2 hours post prandial 202 mg/dL, A1C 12.0% - Urinalysis: protein +2, creatinin serum 2.0 mg/dL
Task:
a. What do you think about his diabetes control?
Clinical skill 3. Measurement of Obesity : Waist circumference and BMI
calculation
Obesity is defined as a condition in which there is an excess of body fat. The operational definition of obesity and overweight however are based on body size or body mass index (BMI) which is closely related to body fatness.
These BMI cut off point are arbitrary along a continuum of increasing risk with increasing BMI. Cut offs used for the definition of obesity can be based on:
1. Statistical data from reference population
2. or on the excess morbidity and mortality associated with increasing body fat content.
a. BMI (body mass index)
Height and weight are the most simple and commonly used measures. A number of weight for height indices have been developed of which the body mass index (BMI) define as this following formula:
b. WC (waist circumference) and WHR (waist to hip ratio)
To determine the risk associ, we need to measured the distribution of body fat. Abdominal or visceral fat is associated with the cardiovascular rsik of the metabolic syndrome.
For WC, the subject stands with feet 25-30 cm apart, weight evenly distributed.
Measurement is taken midway between the inferior margin of the last rib and the crest of the ilium in the horizontal plane. The measurer sits by the side of the subject and fits the tape snugly but not compressing soft tissues. Circumference is measured to nearest 0.1 cm
For hip circumference the measure is taken around the pelvis at the point of maximal protrusion of the buttocks.
[image:33.595.80.548.603.773.2]Ratio of waist to hip ratio (WHR) is calculate by:
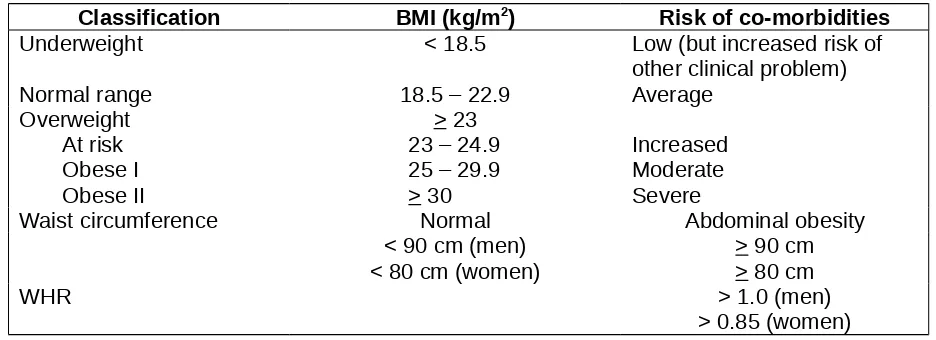
Tabel 1. Classification of Weight by BMI and Waist Circumference in Adult Asians
Classification BMI (kg/m2) Risk of co-morbidities
Underweight < 18.5 Low (but increased risk of other clinical problem)
Normal range 18.5 – 22.9 Average
Overweight At risk Obese I Obese II
> 23 23 – 24.9 25 – 29.9 > 30
Increased Moderate Severe
Waist circumference Normal Abdominal obesity
< 90 cm (men) < 80 cm (women)
> 90 cm > 80 cm
WHR > 1.0 (men)
> 0.85 (women) Body weight (kg)
Height (m)
=
BMI (kg/m 2)Waist circumference
Clinical skill 4. Thyroid gland physical examination
a. Inspect the neck for the thyroid gland
Tip the patient’s head back a bit. Using tangential lighting derected downward from the tip of the patient’s chin, inspect the region below the cricoid cartilage for the gland.
Goiter is a general term for an enlarged thyroid gland.
Ask the patient to sip some water and to extend the neck again and swallow. Watch for upward movement of the thyroid gland, noting its contour and symmetri
The thyroid cartilage, the cricoid cartilage, and the thyroid gland all rise with swallowing and then fall to their resting positions.
b. Palpation
Steps for palpating the thyroid gland:
- Ask the patient to flex the neck slightly forward to relax the sternomastoid muscles. - Place the fingers of both hands on the patient’s neck so that your index fingers are just
below the cricoid cartilage
- Ask the patient to sip and swallow water as before. Feel the thyroid isthmus rising up under your finger pads. It is often but not always palpable.
- Displace the trachea to the right with the fingers of the left hand; with the right hand fingers, palpate laterally for the right lobe of the thyroid in the space between the displaced trachea and the relaxed sterbomastoid. Find the lateral margin. In similar fashion, examine the left lobe.
The lobe are somewhat harder to feel than the isthmus, so practice is needed. The anterior surface of a lateral lobe is approximately the size of the distal phalanx of the thumb and feels somewhat rubbery.
- Note the size, shape, and consistency of the gland and identify any nodules or tenderness.
Soft in Grave’s disease
Firm in Hashimoto’s thyroiditis, malignancy Benign and malignant nodules
Tenderness in thyroiditis.
Note: The thyroid gland is usually easier to feel in a long slender neck than in a short stocky one. In shorter necks, added extension of the neck may help.
In some persons, however, the thyroid gland is partially wholly substernal and not amenable
Learning task:
c. Auscultation
If the thyroid gland is enlarged, listen over the lateral lobes with a stethoscope to detect a bruit, a sound similar to a cardiac murmur but of noncardiac origin.
A localized systolic or continuous bruit may be heard in hyperthyroidism.
Clinical skill 5. Laboratory result interpretation
Case 1.
Female 15 years old came to hospital with decrease of consciousness. One day before admission, she through up everything she ate and had a very bad pain in her stomach. Since this last one month, she was very weak and could not do her daily activity very well. She had never been diagnosed with any specific illness before.
Laboratory result:
Blood sugar random 645 mg/dL Urinalysis keton +3
Blood gas analysis pH 7.12 (normal: 7.35-7.45) pO2 97 (normal: 80 – 105) HCO3- 3.00 mEq/L (normal: 21-30)
Case 2.
Male 44 years old came to outpatient clinic with an acute swelling and pain of his thyroid nodule.
The first laboratory result was:
TSHs 0.023 uIU/ml (normal range: 0.25 – 5 uIU/ml) FT4 20.51 ug/dl (normal range: 5.13 – 14.06 ug/dl) The second laboratory result after 3 months was:
TSHs 7.23 uIU/ml (normal range: 0.25 – 5 uIU/ml) FT4 2.33. ug/dl (normal range: 5.13 – 14.06 ug/dl)
Learning task:
Try the physical examination of your friend’s thyroid gland and note the size, shape, and consistency of the gland and identify any nodules or tenderness.
Learning task:
1. What is the diagnosis of this case?
2. After insert the intravenous line and rehidration, you decide to give an insulin therapy. Is there any laboratory data that you need before administering insulin in this patient?
Learning task:
Case 3.
Female 22 years old, came to outpatient clinic with chief complain palpitation, nervous, and decrease of body weight. Her eyes look bigger than before since last 6 months.
Laboratory result:
TSHs <0.005 uIU/ml (normal range: 0.25 – 5 uIU/ml) FT4 12.51 ug/dl (normal range: 5.13 – 14.06 ug/dl)
Learning task:
Student Standard References:
Basic & Clinical Endocrinology, 9th ed, Lange Medical Publication
Additional Recommended Reading
1. Essential Clinical Anatomy, 2 nd ed. Lippincott Williams & Wilkins, Philadelphia. 2002. 2. Fawcett DW, Jenish RP : Bloom and Fawcett`s Concise Histology, 2 nd ed, London,
Arnold, 2002. p. 220-221, 251-266.
3. Guyton A. C and Jhon E. Hall Textbook of Medical Physiology:Page: 836-914 4. Harper, 25 ed.p.451-626
5. Baynes J; Dominiczak Marek H. Medical Biochemistry.1999. chapter 12, chapter 17, and chapter 23 page 297-304
6. Robbins Basic Phatology, 7 ed, 2003.p.221-225
7. Henry JB; Alexander ; Eng C D. Evaluation of Endocrine function In : Henry JB Ed. Clinical Diagnosis and Management by Laboratory Method. 19th Ed.1996. p.322-373
8. Gartner LP, Hiatt JL : Color Text Book of Histology, 2 nd ed, Philadelphia, W.B. Saunders, 2001,p. 301-324.
9. Wales J.K H, 1996. Pediatric endocrinology and growth: Abnormal Genitalia; 99-116 10. Styne DM, 2004. Handbooks in Pediatric endocrinology: Disorders of sexual
differentiation; 134-158 Reference Clinical Skills
1. Bickley LS, Szilagyi PG. Bates’ Guide to Physical Examination and History Taking. 8th
eds. Lippincott William & Wilkins. Philadelpia, 2003.
2. American Diabetes Association. Clinical Practice Recommendations 2015. Diabetes Care 2015
Endocrine ,metabolism and disorders
Endocrinological disorders
Diabetes Mellitus tipe 1 4A
Diabetes Mellitus tipe 2 4A
DM tipe lain (intoleransi glukosa akibat penyakit lain atau
obat-obatan) 3A
Ketoasidosis diabetikum nonketotik 3B
Hiperglikemia hiperosmolar 3B
Hipoglikemia ringan 3B
Hipoglikemia berat 4A
Diabetes insipidus 1
Akromegali, gigantisme 1
Defisiensi hormon pertumbuhan 1
Hyperparathyroidism 1
Hypoparathyroidism 3A
Hyperthyroid 3A
Thyrotoxicosis 3B
Goiter 3A
Thyroiditis 2
Cushing's disease 3B
Adrenal Crisis 3B
Addison's disease 1
Precocious puberty 2
Hypogonadism 2
Prolactinoma 1
Thyroid Adenoma 2
Thyroid Carcinoma 2
Expected level of competence:
1. Able to recognise and organized clinical features of disease.
In case, it appeared in literature or correspondence, he knows how to organize these clinical features and how to get further information. This level indicates an overview level. If these clinical features found on patient, dNoper able to recognize it, suspect the diagnosis and reffered immediately.
2. Able to make clinical diagnosis based on physical examination and additional investigation requested by dNoper e.g. routine laboratory assay or X-ray. DNoper able to reffer patient to relevant specialist immediately and capable to follow up afterward.
3A. Able to make clinical diagnosis based on physical examination and additional investigation requested by dNoper e.g. routine laboratory assay or X-ray. DNoper able to decide and give initial treatment also reffer to relevant specialist for non-emergency cases.
3B. Able to make clinical diagnosis based on physical examination and additional investigation
4. Able to make clin