Women with Schizophrenia: Positive Effect on
Negative Symptoms?
Laurie A. Lindamer, Dawn C. Buse, James B. Lohr, and Dilip V. Jeste
Background: Some studies of premenopausal women suggest that the severity of psychopathology associated with schizophrenia may be related to levels of estrogen.
Methods:We examined psychopathology in community-dwelling postmenopausal women with schizophrenia who had received (n524) versus had never received (n528) hormone replacement therapy.
Results: Users of hormone replacement therapy and nonusers did not differ significantly with respect to age, ethnicity, education, age of onset, duration of schizophre-nia, global cognitive functioning, or neuroleptic-induced movement disorders. The hormone replacement therapy users received lower average daily doses of antipsychotic medication; they had similar levels of positive symptoms but significantly less severe negative symptoms compared with hormone replacement therapy nonusers, independent of differences in antipsychotic dosage.
Conclusions:Our results suggest that the use of hormone replacement therapy in conjunction with antipsychotic medication in postmenopausal women with schizophrenia may help reduce negative, but not positive, symptoms.
Biol Psychiatry 2001;49:47–51 ©2001 Society of Biolog-ical Psychiatry
Key Words: Psychosis, aging, estrogen, positive and negative symptoms, antipsychotics
Introduction
S
everal studies of gender differences in psychopathol-ogy associated with schizophrenia suggest that women with schizophrenia tend to have more severe positive symptoms and less severe negative symptoms than men (Andia et al 1995; Goldstein and Link 1988; Gur et al 1996; Lindamer et al 1999; Shtasel et al 1992). The dataon gender differences in depressive symptoms are incon-sistent (Addington et al 1996; Goldstein and Link 1988). Several explanations for the gender differences in psycho-pathology have been proposed, including psychosocial factors (Seeman 1997), cerebral lateralization (Seeman 1981), and levels of estrogen (Hafner et al 1993; Lindamer et al 1997; Seeman 1997).
Some of the evidence supporting a role of estrogen comes from studies of changes in psychopathology during different phases of the menstrual cycle in premenopausal women with schizophrenia (Seeman 1996). Researchers have generally found lower scores on measures of psycho-sis and general psychopathology (Hallonquist et al 1993; Riecher-Rossler et al 1994) or better treatment response (Gattaz et al 1994) during phases of the menstrual cycle when estrogen levels are higher. No relationship of estra-diol levels to measures of depression has been observed in women with schizophrenia. The relationship with negative symptoms of schizophrenia has received little attention, however, except for a report of an inverse association between estradiol levels and anergia (Riecher-Rossler et al 1994).
An open-label treatment study of 18 premenopausal women (Kulkarni et al 1995) found a more rapid response in general psychopathology and positive symptom scores in women receiving estrogen supplementation of their antipsychotic medication relative to a group that received only antipsychotic medication. At the end of the 45 days, however, no significant differences between the groups on measures of psychopathology were present. Although there have been studies of estrogen effects on depression (Morrison and Tweedy 2000) and tardive dyskinesia (Glazer and Nasrallah 1988), to our knowledge there have been no published studies examining the association be-tween use of hormone replacement therapy (HRT) and psychopathology in postmenopausal women with schizophrenia.
We investigated the relationship between the use of HRT and psychopathology in community-dwelling post-menopausal women with schizophrenia in a cross-sec-tional study. It was hypothesized that compared to
non-From the Department of Psychiatry, University of California, San Diego (LAL, JBL, DVJ), Psychiatry and Psychology Services, VA San Diego Healthcare System (LAL, JBL, DVJ), and Veterans Medical Research Foundation (LAL, DCB, JBL, DVJ), San Diego, California.
Address reprint requests to Laurie A. Lindamer, Ph.D., San Diego VAMC 116A, 3350 La Jolla Village Drive, San Diego CA 92161.
Received May 3, 2000; revised July 17, 2000; accepted July 19, 2000.
HRT users, women with schizophrenia who had used HRT would have lower scores on measures of general psycho-pathology and positive and negative symptoms but that both groups would have similar levels of depression.
Methods and Materials
Fifty-seven outpatient women over the age of 45 with the DSM-IV (American Psychiatric Association 1994) diagnosis of schizophrenia or schizoaffective disorder were included in our study. Details of clinical evaluation in our research center have been described elsewhere (Jeste et al 1995). Briefly, exclusion criteria were a history of moderate to severe head trauma or other neurologic disorder, current alcohol or other substance abuse or dependence meeting DSM-IV criteria (American Psychiatric Association 1994), and any systemic medical disease that was judged likely to affect central nervous system functioning. Our study was approved by the University of California at San Diego Human Subjects Committee, and all the patients signed a voluntary written informed consent for research participation. They were interviewed about their gynecological and reproduc-tive history, which included information regarding menopausal status and the use of HRT. Five women who were not yet postmenopausal, as defined by the absence of a menstrual cycle for at least 6 months, were excluded. Of the remaining 52 women, 28 had never received HRT, and 24 had received HRT for at least 1 year.
The following rating scales were used: Brief Psychiatric
Rating Scale (BPRS; Overall and Gorham 1988) (including the total score and depression, hostility, disorganization and negative symptom subscales), Scales for the Assessment of Positive and Negative Symptoms (SAPS and SANS, respectively; Andreasen 1981, 1984), Positive and Negative Syndrome Scale (PANSS; Kay et al 1987) (including the positive, negative, and general symptoms subscales), Hamilton Depression Rating Scale (HAM-D; Hamilton 1967), modified Simpson–Angus Scale (Simpson and Angus 1970), Abnormal Involuntary Movement Scale (AIMS; National Institute of Mental Health1976), and the Mini-Mental State Examination (MMSE; Folstein et al 1975). All clinical assessments were performed by raters who were blind to the hormonal status of the subjects.
Continuous variables were transformed, when necessary, to meet the assumptions of normality. Independent t tests were performed to compare the patient groups on continuous vari-ables, andx2tests were used to compare the groups on
categor-ical variables. Statistcategor-ical analysis was performed using SPSS (Norusis 1993), and all the statistical tests were two-tailed.
Results
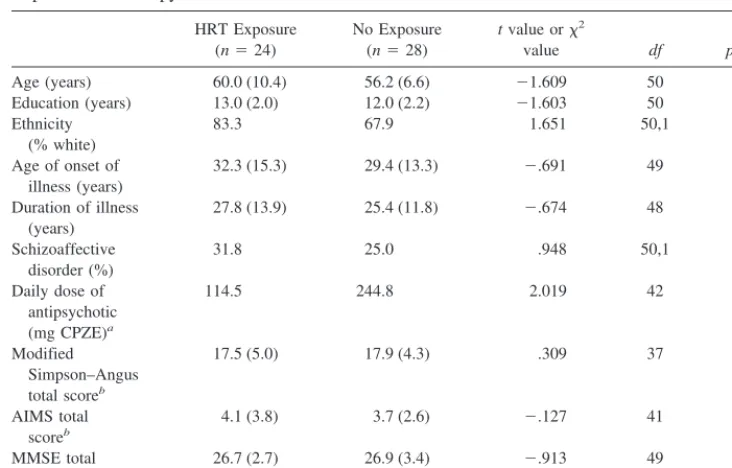
Patients who had ever received versus never received HRT were similar with respect to age, ethnicity, diagnosis, education, age of onset, duration of illness, severity of extrapyramidal symptoms and dyskinesia, and global cog-nitive function (Table 1). Similar proportions (approxi-Table 1. Comparisons (Means and SDs) on Demographic and Clinical Variables in
Postmenopausal Women with Schizophrenia Ever Treated versus Never Treated with Hormone Replacement Therapy
HRT Exposure (n524)
No Exposure (n528)
tvalue orx2
value df pvalue
Age (years) 60.0 (10.4) 56.2 (6.6) 21.609 50 .114
Education (years) 13.0 (2.0) 12.0 (2.2) 21.603 50 .115
Ethnicity (% white)
83.3 67.9 1.651 50,1 .199
Age of onset of illness (years)
32.3 (15.3) 29.4 (13.3) 2.691 49 .493
Duration of illness (years)
27.8 (13.9) 25.4 (11.8) 2.674 48 .503
Schizoaffective disorder (%)
31.8 25.0 .948 50,1 .330
Daily dose of antipsychotic (mg CPZE)a
114.5 244.8 2.019 42 .050
Modified Simpson–Angus total scoreb
17.5 (5.0) 17.9 (4.3) .309 37 .759
AIMS total scoreb
4.1 (3.8) 3.7 (2.6) 2.127 41 .899
MMSE total scorec
26.7 (2.7) 26.9 (3.4) 2.913 49 .366
CPZE, chlorpromazine equivalent; AIMS, Abnormal Involuntary Movement Scale; MMSE, Mini-Mental State Examination.
aMedian, analysis performed on log-transformed values of means. bSquare root transformed.
mately 90%) of subjects in each group were on antipsy-chotics (including atypical agents in about a third of the patients) and anticholingeric medications (approximately 20%). More women who had received HRT had a history of hysterectomy (67% vs. 19%,x259.617,p5.002). In addition, the women who had received HRT were on lower mean daily doses of antipsychotic medication.
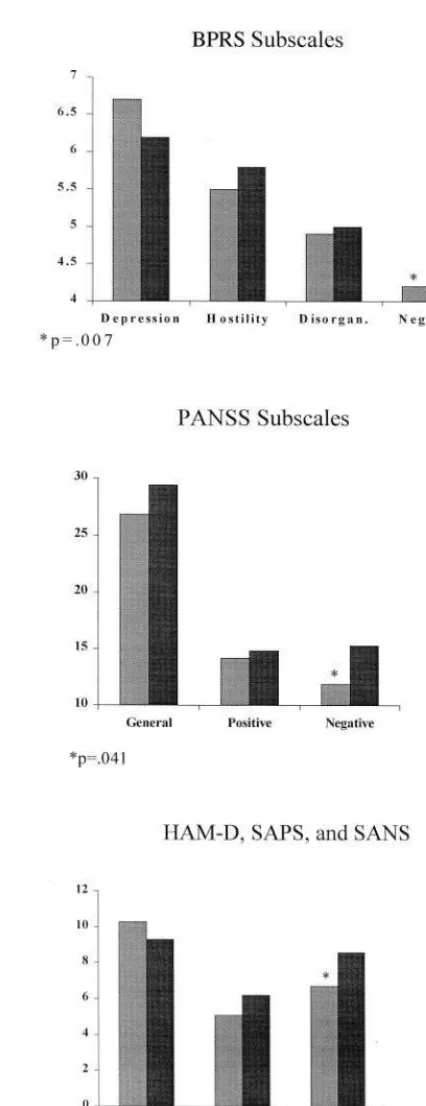
There were no significant differences between the groups on general measures of psychopathology (BPRS total score or the PANSS general score), measures of depression (BPRS depression subscale or HAM-D), or positive symptoms (BRPS disorganization and hostility subscales, SAPS total, or PANSS positive subscale; Figure 1). The HRT users had lower scores on measures of negative symptoms that were significantly different for the BPRS negative subscale [t(1,49)52.800,p5 .007] and PANSS negative syndrome scale [t(1,45) 5 2.104,p 5 .041] and at a trend level for the SANS total [t(1,45) 5 1.886,p5 .066].
Because the HRT users and nonusers differed on the mean current daily dose of antipsychotic medication, the analysis was rerun using an analysis of covariance, with daily neuroleptic dose (mg chlorpromazine equivalent or CPZE; Jeste and Wyatt 1982) as a covariate, on the BPRS negative subscale, the SANS total, and the PANSS nega-tive syndrome scores. The association with the BRPS negative subscale remained significant (F 5 6.409, p5 .015), whereas the results on the PANSS (F53.329,p5 .075) and the SANS (F 5 2.968, p 5 .092) became nonsignificant trends.
Discussion
No significant differences between women with schizo-phrenia who had received or had never received HRT were found on measures of overall psychopathology, positive or depressive symptoms, extrapyramidal symptoms, or dys-kinesia. Use of HRT appeared to be related to the severity of negative symptoms, however. Women who had never received HRT had higher scores on negative symptoms even when controlling for the amount of antipsychotic medication. The less severe negative symptoms seen in the HRT users could not be explained by group differences in the use of atypical antipsychotic medication because comparable proportions of both groups were taking atyp-ical antipsychotics. Women using HRT required lower doses of antipsychotic medications. Although data are sparse, hormonal status may affect pharmacokinetics of antipsychotic metabolism (Yonkers and Hamilton 1996); however, covarying for the antipsychotic dose did not neutralize the significant difference in BPRS negative symptoms subscale, which has been shown to have
ity in older outpatients with schizophrenia (McAdams et al 1996).
The finding of less severe negative symptoms in post-menopausal women with schizophrenia who received HRT is consistent with the results reported by Riecher-Rossler et al (1994). Estrogen may reduce negative symp-toms by several mechanisms, including modulating dopa-minergic or other neurotransmitter systems involved in pathophysiology schizophrenia or providing neuroprotec-tive effects (Seeman 1996, 1997). The association between postmenopausal HRT use and less severe negative symp-toms in women with schizophrenia may have important clinical implications. The addition of HRT to antipsy-chotic medication in stable outpatients may have the effect of improving negative symptoms.
Contrary to our hypotheses, our study found no signif-icant difference between postmenopausal HRT users and nonusers on positive symptoms. The lack of differences may be due to the fact that this sample consisted of older outpatients who were stable on antipsychotic medication and who had only mild positive symptoms, thereby re-stricting variability and the ability to detect differences. Positive symptoms have been shown to decrease with age possibly because of age-related decreases in dopaminergic activity, whereas negative symptoms persist (Eyler-Zor-rilla et al 2000; Harvey et al 1997; Schultz et al 1997).
This study has several limitations. First, the differences on the SANS and PANSS negative subscale were signif-icant at the trend level only when neuroleptic dose was taken into account. The consistency of the finding of lower scores on the three different negative symptom measures in HRT users was striking, however. The lack of a relationship between HRT and global cognition could reflect our use of a crude measure (i.e., MMSE) that might lack sensitivity to detect such differences. A recent ran-domized controlled trial of estrogen replacement therapy found no effect on cognition in patients with mild to moderate Alzheimer’s disease (Mulnard et al 2000). The cross-sectional design is another limitation of this study. Although we found less severe negative symptoms in HRT users, it is not possible to conclude that this result is due to the use of HRT directly. It is possible that the severity of negative symptoms may affect the interest in or ability to seek medical care, resulting in women with higher negative symptoms not receiving HRT. Finally, this was a sample of convenience, and available information on the type, dosage, or duration of HRT was limited. Conse-quently, the sample may be biased.
Double-blind, placebo-controlled studies of estrogen supplementation in postmenopausal women with schizo-phrenia are needed for more definitive conclusions to be drawn about the effects of estrogen on the psychopathol-ogy and functioning in these patients.
This work was supported, in part, by National Institute of Mental Health Grants Nos. MH43693, MH51459, MH45131, MH49671, and MH01580; by the National Alliance for Research on Schizophrenia and Depression; and by the Department of Veterans Affairs.
References
Addington D, Addington J, Patten S (1996): Gender and affect in schizophrenia.Can J Psychiatry41:265–268.
American Psychiatric Association (1994):Diagnostic and Sta-tistical Manual of Mental Disorders,4th ed. Washington, DC: American Psychiatric Association.
Andia AM, Zisook S, Heaton RK, Hesselink J, Jernigan T, Kuck J, et al (1995): Gender differences in schizophrenia.J Nerv Ment Dis183:522–528.
Andreasen NC (1981):The Scale for the Assessment of Negative Symptoms (SANS).Iowa City: The University of Iowa. Andreasen NC (1984):The Scale for the Assessment of Positive
Symptoms (SAPS).Iowa City: The University of Iowa. Eyler-Zorrilla LT, Heaton RK, McAdams LA, Zisook S, Harris
MJ, Jeste DV (2000): Cross-sectional study of older outpa-tients with schizophrenia and healthy comparison subjects: No differences in age-related cognitive decline.Am J Psychi-atry8:1324 –1326.
Folstein MF, Folstein SE, McHugh PR (1975): Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician.J Psychiatr Res12:189 –198. Gattaz WF, Vogel P, Riecher-Rossler A, Soddu G (1994):
Influence of the menstrual cycle phase on the therapeutic response in schizophrenia.Biol Psychiatry36:137–139. Glazer WM, Nasrallah HA (1988) Neuroendocrine aspects of
tardive dyskinesia: The role of estrogen, prolactin, and dopamine. In: Wolf ME, Mosnaim AD, editors. Tardive Dyskinesia: Biological Mechanisms and Clinical Aspects. Washington, DC: American Psychiatric Press, 181–196. Goldstein JM, Link BG (1988): Gender and the expression of
schizophrenia.J Psychiatr Res2:141–155.
Gur RE, Petty RG, Turetsky BI, Gur RC (1996): Schizophrenia throughout life: Sex differences in severity and profile of symptoms.Schizophr Res21:1–12.
Hafner H, Riecher-Rossler A, an der Heiden W, Maurer K, Fatkenheuer B, Loffler W (1993): Generating and testing a causal explanation of the gender difference in age at first onset of schizophrenia.Psychol Med23:925–940.
Hallonquist JD, Seeman MV, Lang M, Rector NA (1993): Variation in symptom severity over the menstrual cycle of schizophrenics.Biol Psychiatry33:207–209.
Hamilton M (1967): Development of a rating scale for primary depressive illness.Br J Soc Clin Psychol6:278 –296. Harvey PD, Lombardi J, Leibman M, Parrella M, White L,
Powchik P, et al (1997): Age-related differences in formal thought disorder in chronically hospitalized schizophrenic patients: A cross-sectional study across nine decades.Am J Psychiatry154:205–210.
Jeste DV, Wyatt RJ (1982):Understanding and Treating Tardive Dyskinesia.New York: Guilford.
Kay SR, Fiszbein A, Opler LA (1987): The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276.
Kulkarni J, de Castella A, Smith D (1995): Adjunctive estrogen treatment in women with schizophrenia. Schizophr Res15: 157–157.
Lindamer LA, Lohr JB, Harris MJ, Jeste DV (1997): Gender, estrogen, and schizophrenia.Psychopharmacol Bull33:221– 228.
Lindamer LA, Lohr JB, Harris MJ, McAdams LA, Jeste DV (1999): Gender-related clinical differences in older patients with schizophrenia.J Clin Psychiatry60:61– 67.
McAdams LA, Harris MJ, Bailey A, Fell R, Jeste DV (1996): Validating specific psychopathology scales in older schizo-phrenic outpatients.J Nerv Ment Dis184:246 –251. Morrison MF, Tweedy K (2000). Effects of estrogen on mood
and cognition in aging women.Psychiatr Ann30:113–119. Mulnard RA, Cotman CW, Kawas C, van Dyck CH, Sano M,
Doody R, et al (2000). Estrogen replacement therapy for treatment of mild to moderate Alzheimer disease: A random-ized controlled trial.JAMA283:1007–1015.
National Institute of Mental Health (1976): Abnormal Involun-tary Movement Scale. In: Guy W, editor.ECDEU Assessment Manual for Psychopharmacology—Revised,Publication No. (ADM)76-338. Rockville, MD: U.S. Department of Health, Education, and Welfare, 534 –537.
Norusis MJ (1993):SPSS for Windows, V6.0.Chicago: SPSS. Overall JE, Gorham DR (1988): The Brief Psychiatric Rating
Scale (BPRS): Recent developments in ascertainment and scaling.Psychopharmacol Bull24:97–99.
Riecher-Rossler A, Hafner H, Dutsch-Strobel A, Oster M, Stumbaum M, vanGulick-Bailer M, Loffler W (1994): Fur-ther evidence for a specific role of estradiol in schizophrenia? Biol Psychiatry36:492– 495.
Schultz SK, Miller DD, Oliver SE, Arndt S, Flaum M, Andreasen NC (1997): The life course of schizophrenia: Age and symptom dimensions.Schizophr Res23:15–23.
Seeman MV (1981): Gender and the onset of schizophrenia: Neurohumoral influences.Psychiatr J Univ Ottawa6:136 –138. Seeman MV (1996): The role of estrogen in schizophrenia.
J Psychiatr Neurosci21:123–127.
Seeman MV (1997): Psychopathology in women and men: Focus on female hormones.Am J Psychiatry154:1641–1647. Shtasel DL, Gur RE, Gallacher F, Heimberg C, Gur RC (1992):
Gender differences in the clinical expression of schizophre-nia.Schizophr Res7:225–231.
Simpson GM, Angus JW (1970): A rating scale for extrapyra-midal side effects.Acta Psychiatr Scand Suppl212:11–19. Yonkers KA, Hamilton JA (1996): Sex differences in