See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/7277433
Microleakage of porcelain veneer restorations
bonded to enamel and dentin with a new
self-adhesive resin-based dental cement
Article
in
Dental Materials · March 2007
DOI: 10.1016/j.dental.2006.01.013 · Source: PubMed
CITATIONS
70
READS
265
4 authors
, including:
Gabriela Ibarra
Oregon Health and Science University
11
PUBLICATIONS201
CITATIONSSEE PROFILE
All content following this page was uploaded by Gabriela Ibarra on 16 December 2016.
a v a i l a b l e a t w w w . s c i e n c e d i r e c t . c o m
j o u r n a l h o m e p a g e : w w w . i n t l . e l s e v i e r h e a l t h . c o m / j o u r n a l s / d e m a
Microleakage of porcelain veneer restorations bonded to
enamel and dentin with a new self-adhesive resin-based
dental cement
Gabriela Ibarra
a,∗, Glen H. Johnson
a, Werner Geurtsen
a, Marcos A. Vargas
baSchool of Dentistry, Department of Restorative Dentistry, University of Washington, Seattle, WA, USA
bCollege of Dentistry, Department of Operative Dentistry, University of Iowa, Iowa City, USA
a r t i c l e
i n f o
Article history:
Received 29 September 2005 Received in revised form 19 December 2005
Accepted 10 January 2006
Keywords:
Self-adhesive resin cement Ceramic veneers
Microleakage Dentin adhesion Enamel adhesion
a b s t r a c t
Cementation technique of bonded ceramic restorations is a time-consuming and technique-sensitive procedure critical to long-term success.
Objective.Evaluate the performance of a self-adhesive, modified-resin dental cement (Rely-X UniCem, 3M-ESPE) for the cementation of ceramic veneer restorations without previous conditioning of the tooth surface, and in combination with a one-bottle adhesive and a self-etching adhesive.
Methods.Thirty-six premolars received a veneer preparation that extended into dentin. Leucite-reinforced pressed glass ceramic (Empress 1) veneers were cemented follow-ing manufacturers’ instructions, accordfollow-ing to the followfollow-ing treatment groups (n= 9): (1) Variolink–Excite Ivoclar–Vivadent (V + E control), (2) Unicem + Single Bond 3M-ESPE (U + SB), (3) Unicem + Adper Prompt L-Pop 3M-ESPE (U + AP), (4) Unicem 3M-ESPE (U). After 24 h stor-age at 37◦C, teeth were thermocycled (2000 cycles) at 5 and 55◦C, immersed in ammoniacal silver nitrate for 24 h, placed in a developer solution overnight and sectioned using a slow-speed saw. Three 1 mm longitudinal sections were obtained from each tooth and evaluated for leakage with a microscope (1×to 4×). Imaging software was used to measure stain pen-etration along the dentin and enamel surfaces.
Results.ANOVA with SNK (˛= 0.05) revealed that on dentin, U had significantly less leakage
than U + SB and U + AP, but no different than V + E; on enamel U had leakage values that were significantly greater than the groups with adhesives.
Significance.The self-adhesive cement U gave low leakage on dentin that was comparable to the cement that employed an adhesive for sealing dentin, whereas this cement benefits from use of an adhesive when cementing to enamel.
© 2006 Academy of Dental Materials. Published by Elsevier Ltd. All rights reserved.
1.
Introduction
The use of bonded ceramic restorations in dentistry has increased appreciably due to the development of adhesive
∗Corresponding author at: Department of Restorative Dentistry, University of Washington, 1959 N.E. Pacific Street, Box 357456, Seattle, WA 98195-7456, USA. Tel.: +1 206 543 5948; fax: +1 206 543 7783.
E-mail address:[email protected] (G. Ibarra).
materials that allow for more conservative restorative tech-niques as well as the ability of achieving excellent esthetic appearance and adequate strength[1]. Among these bonded ceramic restorations, ceramic veneers have gained popularity
0109-5641/$ – see front matter © 2006 Academy of Dental Materials. Published by Elsevier Ltd. All rights reserved. doi:10.1016/j.dental.2006.01.013
2
d e n t a l m a t e r i a l s x x x ( 2 0 0 6 ) xxx–xxxas a conservative restoration, where a thin ceramic covering is bonded, preferentially to enamel, after minimal preparation on tooth structure[2,3].
The cementation technique, which is a time-consuming and technique-sensitive procedure, is key to the long-term success of these types of restorations. The strength and the durability of the bond between the porcelain, the luting cement and the enamel/dentin interface play an important role in the outcome of ceramic veneers, particularly when dentin is involved[3]. It is not uncommon that, particularly in the gingival third of a veneer preparation, dentin will be exposed due to the thin layer of enamel present at this site[4]. In this case, the cementation procedure becomes even more critical because high failure rates in veneers have been associ-ated to large exposed dentin surfaces and the cervical margin has been regarded as a problematic area to achieve perfect marginal adaptation[3].
A self-adhesive, resin-based dental cement (Rely-X UniCem, 3M-ESPE), which advocates no pre-treatment of tooth surfaces, thus simplifying the cementation proce-dure, has recently been introduced. This cement has an organic matrix composed of multi-functional phosphoric acid methacrylates, which react with inorganic fillers (72 wt.%) that are basic in nature or with hydroxyapatite from tooth structure. Water that is released from the setting reaction is thought to play a role in its neutralization, raising the pH value from 1 to 6. The setting of the cement is based on a free radical polymerization reaction initiated by either photoactivation or a redox system[5,6].
The cement has been recommended for luting all metal-based and ceramic crowns, as well as partial coverage ceramic and indirect composite restorations, with the exception of veneers[5,6].
Good marginal adaptation of all-ceramic crowns cemented with Rely-X UniCem to dentin has already been documented
[5]. Preliminary studies have shown good results when bond-ing pressed ceramic inlay restorations to dentin and enamel margins[7].
If the self-adhesive cement could be used predictably for the cementation of ceramic veneer restorations, it would serve as a user-friendly universal cement. However, more studies are needed before final recommendations for the clinical use of this cement can be made.
The clinical success of cemented restorations has been evaluated by measuring marginal fit and microleakage for many years, in spite of the fact that there is no restoration or luting material able to achieve a complete marginal seal
[8,9]. In the case of all-ceramic restorations, microleakage has been correlated with the loss of the integrity of the bond to tooth structure, and this has been associated with other problems such as secondary caries, post-operative sensitivity, pulpal inflammation, staining and plaque accumulation[9–11]
due to the clinically undetectable passage of bacteria, fluids, molecules or ions between tooth structure and the cemented restoration[12].
The aim of this study was to test the hypothesis that the application of a new self-adhesive resin cement, used as a luting agent, would result in good marginal integrity of ceramic veneers to dentin as well as enamel, without prior conditioning of the tooth surface or in combination with
other adhesive systems that previously condition enamel and dentin.
Altogether, the hypothesis tested was that the microleak-age of the new self-adhesive luting cement is similar to a conventional resin cement when bonding a porcelain veneer to enamel and dentin.
2.
Materials and methods
Thirty-six human premolars, previously stored in a NaN3+ NaCl solution for no more than 6 months, were
prepared for porcelain veneer restorations. The preparations were made with a #834 016 bur (Brasseler, Savannah, GA 31419, USA) to establish a 0.3 mm depth cut, and finished with a fine rounded tip diamond #6844 016 (Brasseler, Savan-nah, GA 31419, USA). The preparation’s margins ended as butt joint at the incisal edge and a chamfer that extended approximately 1 mm beyond the CEJ. An impression of each of the preparations was made with a vinyl polysiloxane impression material (Aquasil LV and Aquasil, Caulk, Dentsply; Lot 020608) using copper rings for material retention. The teeth were then stored in artificial saliva solution and the impressions were sent to a commercial laboratory (Nakan-ishi Dental Laboratory Inc., Seattle, WA). Leucite-reinforced pressed ceramic (Empress I) porcelain veneer restorations were fabricated in an A-1 shade based on the Vita shade guide, etched with hydrofluoric acid and silanated in the laboratory.
The teeth were then divided into four treatment groups according to the cementation procedure (Table 1). Group 1: restorations cemented using a conventional resin-based cement and its proprietary adhesive system as a con-trol (Variolink II [Base Yellow 210/A3, Lot E 43489; Cata-lyst Lot E 34696] and Excite [Lot E41824], Ivoclar/Vivadent). Group 2: restorations cemented using self-adhesive, modified-resin dental cement (Rely-X UniCem Maxicaps, 3M-ESPE; Lot 143650) in combination with enamel and dentin con-ditioning with phosphoric acid and a one-bottle adhe-sive system (Single Bond, 3M-ESPE). Group 3: restorations cemented using a self-adhesive resin-based dental cement (Rely-X UniCem Maxicaps, 3M-ESPE; Lot 143650) in combi-nation with a self-etching adhesive system (Adper Prompt L-Pop, 3M-ESPE; Lot 147563) to condition enamel and dentin. Group 4: restorations cemented with a self-adhesive resin-based dental cement (Rely-X UniCem Maxicaps, 3M-ESPE; Lot 143650) without previous conditioning of enamel and dentin.
Before cementation, all veneers were tried-in, cleaned with phosphoric acid and re-silanated (Rely-X Ceramic Primer; Lot 2721) in accordance with clinical practice.
Light-curing of the adhesives and the cement was carried out with a Demetron 401 light unit (Demetron/Kerr, Dan-bury, CT) as indicated in Table 1. Light output was mea-sured every six samples to ensure proper resin polymerization (750 mW/cm2).
The specimens were stored in artificial saliva at 37◦C for
72 h and were thermocycled in 5 and 55◦C water temperatures
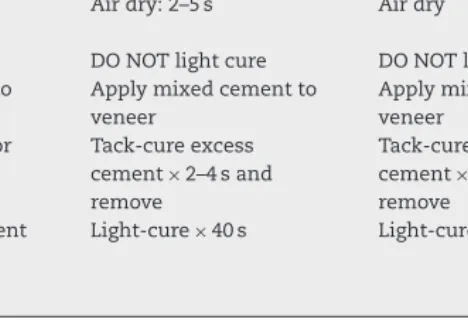
Table 1 – Application technique for seating ceramic veneer restorations with different adhesive systems and luting cements
Treatment Materials
Excite/Variolink Single bond/Unicem Prompt L-pop/Unicem Unicem
Veneer preparation Etch with H3PO4×60 s Etch with H3PO4×60 s Etch with H3PO4×60 s Etch with H3PO4×60 s
Rinse×30 s Rinse×30 s Rinse×30 s Rinse×30 s
Air dry Air dry Air dry Air dry
Silanate internal
Air-thin Air-dry for 2–5 s Air-thin
DO NOT light cure DO NOT light cure DO NOT light cure Substrate preparation H3PO4: etch
enamel×15–30 s and
dentin×10–15 s
H3PO4: etch enamel and dentin×10 s
Slightly dry surface Leave dentin and enamel surface moist/glossy Rinse: 5 s at least Rinse: 30 s Adhesive: lightly scrub
one layer on enamel
Adhesive: apply 2 coats Adhesive: apply a second coat without rubbing
Air-dry: 1–3 s. Avoid pooling
Air dry: 2–5 s Air dry
Cure: 20 s DO NOT light cure DO NOT light cure Seating instructions Apply base cement to
veneer and tooth
Light-cure×40 s Light-cure×40 s Light-cure×40 s
Light-cure×40 s
2.1. Microleakage evaluation
The apices of the roots were sealed with an acrylic resin (Duralay Inlay Pattern Resin, Reliance) and the teeth were then coated with two layers of quick dry nail varnish that extended up to 1 mm from the margins of the ceramic veneer restora-tions. Care was taken not to over dry the enamel surrounding the margins while the nail varnish dried.
The teeth were placed in 50 wt.% ammoniacal silver nitrate for 24 h, rinsed extensively with water, and placed in freshly mixed developer solution (Kodak Developer D-76, CAT 1464817, 0251 C5 02749) under a strong light for 12 h. After rinsing them with water and sand blasting the porcelain sur-face carefully, a 1 mm layer of composite was bonded to the veneer (All Bond 2, Bisco, Lot 0200002521; Filtek Z 250 B 1 shade, 3M-ESPE, Lot 9BB) to provide sufficient bulk for handling, and light-cured for 40 s. The roots were removed and the crowns were sectioned in a cervical–incisal direction with a diamond blade to obtain three slices (∼1 mm) from each tooth (Fig. 1).
Sections were analyzed for leakage at the cervical and incisal margins by means of a light microscope (Nikon Eclipse E400, Japan) at 1×, 2×and 4×, using an image analysis
4
d e n t a l m a t e r i a l s x x x ( 2 0 0 6 ) xxx–xxxputer program (Meta Vue, Universal Imaging Corp., Downing-town, PA). Microleakage values were obtained by measuring stain penetration for the total surface length, separately for dentin and enamel, and were expressed as a percentage of the total length of the veneer preparation.
2.2. Statistical analysis
Since there were four different cement-bonding combinations (i.e., treatments) and samples were independent, a single-factor analysis of variance model was employed to test for significant main effects, separately for dentin and for enamel. If main effects were significant (˛= 0.05) and test for equal
vari-ance was not significant, the Student–Newman–Kuel’s post hoc test for multiple comparison of means was conducted to determine which means differed. When the assumption of equal variances was not met, the Games–Howell post hoc test was used to identify which means differed. All hypothesis testing was conducted at the 95% level of confidence.
2.3. SEM evaluation
After cementation, one tooth from each group was prepared for SEM evaluation. The teeth were stored in water for 4 weeks and were fixed for 72 h in 2.5% glutaraldehyde in 0.1 M Na-cacodylate buffer. Cross-sections of an approximate thickness of 1 mm (Fig. 1) were obtained from the teeth using a water-cooled slow-speed diamond saw (Buehler Isomet 1000TM,
Buehler Ltd., Lake Bluff, IL, USA) and each section was sequen-tially polished with 600 and 800 grit of silicon carbide paper, 6 and 1m diamond slurries and 0.04m aluminum oxide. The
specimens were dehydrated in an ascending series of ethanol and critical-point dried with HMDS, mounted on aluminum stubs and gold-sputter coated to prepare them for analysis under a field-emission scanning electron microscope (FE-SEM, Hitachi S-4000).
3.
Results
3.1. Microleakage analysis
A total of 144 specimen sections were available for evaluation of microleakage at the interface. Three sections were obtained from each of the 48 teeth and information was gathered from both sides of each section. Microleakage was observed in most of the specimens, especially on the dentin side, which is con-sistent with existing evidence[13–18].
Mean microleakage values for the dentin side were 44.1% in the Variolink and Excite group (E + V), 55.5% in the Single Bond and Unicem group (SB + U), 54.7% in the Prompt and Unicem group (AP + U) and 28.1% in the Unicem group (U) (Fig. 2). ANOVA test was significant and the test for equal vari-ances was not significant. The Student–Newman–Kuel’s (SNK) test to compare means (˛= 0.05) revealed that on dentin: U
had significantly less leakage than SB + U and AP + U but was not different than E + V and that E + V, SB + U, AP + U were not shown to differ.
The microleakage values for the enamel side were 2.5% in the E + V group, 3.1% in SB + U group, 2.2% in the AP + U group
Fig. 2 – Mean percent microleakage values between porcelain veneers and dentin. The numbers identify mean subsets not shown to differ at˛= 0.05. The vertical bars show the value of a single standard deviation.
and 10.8% in the U group (Fig. 3). ANOVA test for main effects was again significant, as was the test for equal variances due to a higher standard deviation associated with enamel microleakage for U. For this reason, the Games–Howell test (˛= 0.05) was employed to compare means. This test revealed
that on enamel, U had leakage values that were significantly greater than any of the groups where an adhesive system was used in combination with the luting cement. In the latter groups, leakage was minimal and no statistically significant difference was found amongst them (Fig. 3).
3.2. Scanning electron microscopy analysis
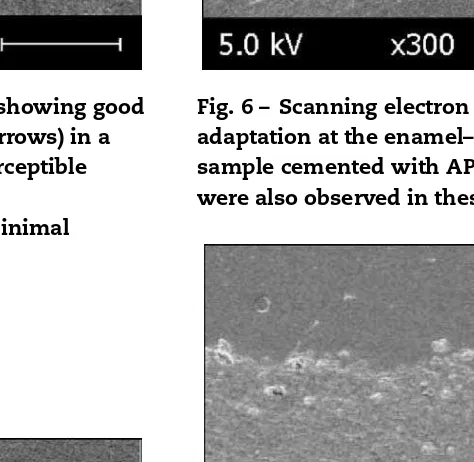
The interface of the samples cemented with E + V, SB + U and AP + U showed good adaptation of the cement to the enamel surface. No gap formation between the cement and the enamel was evident in the E + V group, which is consistent with the microleakage values obtained for these specimens (Fig. 4). It appeared that the use of an adhesive resulted in consistently good adaptation of the cement to the enamel, regardless of the type of conditioning, as was demonstrated by similar leakage values when using phosphoric acid and the self-etching adhesive system (Figs. 5 and 6).
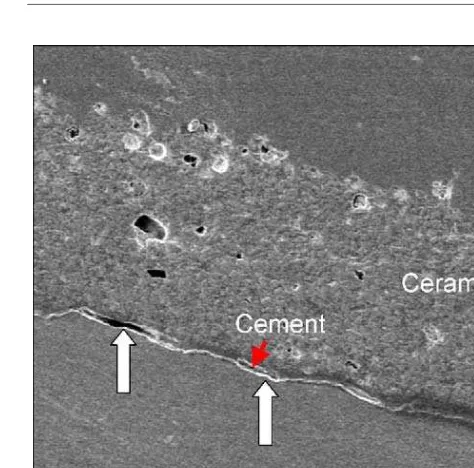
The samples treated only with unicem (U) showed a gap between the cement and the enamel, which is in accor-dance with the high leakage values observed in this group (Figs. 7 and 8).
Fig. 4 – Scanning electron microscopy image showing good adaptation at the enamel–cement interface (arrows) in a sample cemented with E + V. An almost imperceptible transition seemed to take place at the
enamel–cement–porcelain interface, where minimal leakage values were observed.
Fig. 5 – Scanning electron microscopy image showing good adaptation at the enamel–cement interface (arrows) in a sample cemented with SB + U. An almost imperceptible transition seemed to take place at the
enamel–cement–porcelain interface, where minimal leakage values were also observed.
Fig. 6 – Scanning electron microscopy image showing good adaptation at the enamel–cement interface (arrows) in a sample cemented with AP + U. Minimal leakage values were also observed in these set of specimens.
Fig. 7 – Scanning electron microscopy image showing gap formation at the enamel–cement interface (arrows). An imperceptible transition seemed to take place at the cement–porcelain interface, where no leakage was observed.
4.
Discussion
6
d e n t a l m a t e r i a l s x x x ( 2 0 0 6 ) xxx–xxxFig. 8 – Scanning electron microscopy image showing gap formation at the enamel–unicem interface (arrows). An imperceptible transition seemed to take place at the cement–porcelain interface, where no leakage was observed.
[19]. A disadvantage of this tracer is that the silver nitrate particle is an extremely small particle that measures approx-imately 0.059 nm in radius and the solution has an acidic pH of∼4.2[9,20]. Therefore, penetration of the silver particle at the interface is frequently observed and it has been suggested that it may be greater because of dissolution of remnant cal-cium phosphate salts at the adhesive interface, resulting in increased porosity due to a light etching effect by the mildly acidic solution. To avoid this potential drawback, the use of a buffered solution of ammoniacal silver nitrate with a pH of
∼9.5, has been reported[20]and was used in the current study.
4.1. Dentin interface
Without any conditioning, the self-etching cement Rely-X Unicem (3M-ESPE) (U) showed improved sealing of dentin at the cervical margin when compared to a conventional resin cement for which the smear layer was removed by the use of phosphoric acid, although this was not statistically signifi-cant in this study. These findings are in accordance with Behr et al.[5]who found similar marginal adaptation based on dye penetration and SEM replica analysis, to that obtained with conventional cements on dentin margins.
The use of two different adhesive systems, a one-step total-etch (Single Bond, 3M-ESPE) and a one-step self-total-etch (Rely-X Adper Prompt, 3M-ESPE), to condition the enamel and dentin prior to cementation, did not improve the sealing ability of (U) in dentin, when compared to the control. De Munck et al.[21]reported similarTBS values when bonding to dentin
using Rely-X Unicem without previously etching the dentin with H3PO4or a conventional cement as a control. However,
when the dentin was etched prior to cementation with Rely-X Unicem, theTBS values significantly decreased. Similarly,
in the present study, when the dentin was pre-treated with either H3PO4or an acidic monomer from the self-etching
sys-tem, increased leakage was observed. Pre-etching may remove all of the buffer capacity of dentin, interfering with its ability to raise the pH of the acidic resin as it sets, thereby lowering its conversion (David Pashley, personal communication).
According to Behr et al.[5], in images obtained with trans-mission electron microscopy, a lack of a hybrid layer is evident at the dentin interface when the self-adhesive cement is used. This agrees with De Munck et al.[21]who reported no evidence of dentin demineralization even considering the initial low pH of the cement (pH <2, according to the manufacturer). This result in the absence of a hybrid layer which, although thinner, is present when self-etching adhesive systems are used[22]. Indeed, if the acid resin cement does not penetrate through the smear layer, the strength of the bond may be limited to the strength of the smear layer.
In this study, the cement was never used alone after etch-ing dentin, but in combination with either a simplified total-etch single-bottle adhesive or a one-step self-total-etching adhe-sive, which coated the pre-treated dentin with a resin layer. In both cases, there were increased leakage values over those seen when the self-adhesive cement was used alone. It is known that the previously reported incompatibility of sim-plified adhesives, especially single-step self-etch adhesives, and dual/auto-cured luting cements may be due, in part, to adverse acid–base reactions between the acidic monomers and the basic tertiary amines that are commonly used as cata-lysts in these systems[23]. The tertiary amines are consumed as they come in contact with the acidic resin monomers due to the absence of an additional adhesive resin layer, which decreases their capacity to generate free radicals for the polymerization reaction. To solve this problem, alterna-tive redox catalyst systems have been introduced, such as the commonly used sodium salt of aryl sulphinic acid[24]. Many single-bottle adhesive systems have an additional bot-tle of an activator solution that contains such a salt. The one-step self-etch adhesives are even more susceptible to this adverse chemical reaction because they are inherently more acidic due to a higher content of acidic resin monomers
[24].
using the adhesive systems was less effective than when the cement was used alone.
Furthermore, it has been reported that the one-step self-etching adhesive system (AP) has shown better sealing when subsequent coats of adhesive are applied. Light-curing the first coat on dentin before applying the second coat, has been recommended to assure adequate resin polymerization[26]. Nevertheless, Tay et al.[25]more recently reported that denti-nal fluid transudation is still observed after additiodenti-nal layers of simplified adhesive systems are applied, even if they are light-cured separately. In the present study, the one-step self-etching adhesive (AP) was used following the manufacturer’s instructions (Table 1) which now recommend application of two consecutive coats of adhesive without light-curing the first coat. Interestingly, there was no statistically significant difference regarding leakage when compared to the conven-tional system but there was a difference when compared to (U) alone. Leakage was observed, in general, between the tooth structure and the cement. We speculate that there was a defi-cient seal probably due to a lack of complete polymerization of the luting cement because of the presence of water at the interface.
When the self-adhesive cement (U) was used on its own, the microleakage values were no different than the values obtained with the conventional cement. According to the information available on this self-adhesive cement, neutral-ization of the acidic reaction takes place as polymerneutral-ization progresses (ESPE-information from the manufacturer). It is important to mention that the small amount of leakage that was observed in dentin may not be indicative of adequate long-term performance of the cement. The durability that self-etching adhesive systems have on cement-dentin bonds after some time, remains to be evaluated.
4.2. Enamel interface
Without any conditioning (U) showed significantly greater leakage at the enamel interface, which was not seen when the cement was used in combination with other adhesive systems or a conventional cement. This may suggest an insufficient etching ability of the cement to smear layer covered enamel, and therefore, the lack of development of adequate microme-chanical retention. The use of the conventional cement as well as the one-bottle and the self-etching adhesive systems were likely to result in good micromechanical retention, since the former used phosphoric acid prior to the adhesive application and the latter was a strong self-etching adhesive (AP) which has been shown to adequately etch enamel[27]. These results are in agreement with DeMunk et al.[21], who reported lower
TBS to enamel that was not acid-etched previous to the use
of Rely-X Unicem, with mostly adhesive failures in the sam-ples, which is probably due to the lack of etching through the smear layer into the underlying enamel. In this same study, theTBS values increased significantly when enamel
was previously etched with phosphoric acid, which obvi-ously resulted in the formation of adequate micromechanical retention.
The role of chemical bonding of the self-adhesive cement with enamel may be insufficient to obtain an adequate seal between the cement and enamel. This is evident in the SEM
images, where previously treated enamel by either a phos-phoric acid conditioner or a strong self-etching adhesive sys-tem, show no evidence of gap formation between the cement and the enamel (Figs. 4–6). However, when the self-adhesive cement was used on its own, an evident gap can be observed (Figs. 7 and 8), which may be due to a combination of fac-tors such as inadequate etching through the enamel smear layer for micromechanical retention on the enamel surface, and the weak cohesive strength of enamel smear layers[28]of the cement.
The inadequate formation of micromechanical retention on enamel may be due to the high viscosity that the cement has after mixing and the short interaction time that it has with the tooth surface before light-curing takes place. The initial low pH (<2) may not be sufficient to etch the enamel if etching time is not adequate, and if neutralization reactions take place rapidly.
Another explanation for the presence of gaps at the enamel interface could be lack of adequate pressure during the cementation procedure. De Munk[21] has reported an improved adaptation of the cement to the substrate when it is applied under pressure due to its thixotropic characteris-tics. In this study, however, the veneers were cemented under pressure that simulated that applied in the clinical setting, and although gap formation was not seen at the dentin interface, it was still evident at the enamel interface.
5.
Conclusions
The seal of the self-adhesive, resin-based cement is compa-rable to cements that employ adhesives for sealing dentin, whereas this cement appears to benefit from the use of a con-ventional conditioner, such as phosphoric acid, or a strong self-etching adhesive system when cementing to enamel.
Due to the excessive enamel microleakage observed in this study when the self-adhesive cement was used alone, the authors would not recommend its use for cementation of ceramic veneers. The hypothesis tested was rejected for enamel substrates.
The lack of adequate performance of this self-etching adhesive cement on enamel suggests the need to more extensively investigate the adhesion mechanism of the self-adhesive cement, surface characterization of the substrate and evaluation of its long-term clinical performance.
Acknowledgements
“This investigation was supported in part by 3M-ESPE”. The authors would like to express their gratitude to OHSU for the thermocycling of the samples and to Dr. David Pashley for his valuable contribution.
r e f e r e n c e s
[1] Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: a review of the current literature. J Prosthet Dent
8
d e n t a l m a t e r i a l s x x x ( 2 0 0 6 ) xxx–xxx[2] Peumans M, Van Meerbeek B, Yoshida Y, Lambrechts P, Vanherle G. Porcelain veneers bonded to tooth structure: an ultramorphological FE-SEM examination of the adhesive interface. Dent Mater 1999;15:105–19.
[3] Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent 2000;28:163–77.
[4] Ferrari M, Patroni S, Balleri P. Measurement of enamel thickness in relation to reduction for etched laminate veneers. Int J Periodontics Restorative Dent
1992;12(5):407–13.
[5] Behr M, Rosentritt M, Regnet T, Lang R, Handel G. Marginal adaptation in dentin of a self-adhesive universal resin cement compared with well-tried systems. Dent Mater 2004;20:191–7.
[6] Technical data sheet, 3M-ESPE.
[7] Rosentritt M, Behr M, Lang R, Handel G. Influence of cement type on the marginal adaptation of all ceramic MOD inlays. Dent Mater 2004;20:463–9.
[8] Gladys S, Van Meerbeek B, Lambrechts P, Vanherle G. Microleakage of adhesive restorative materials. Am J Dentistry 2001;14(3):170–6.
[9] Alani AH, Toh CG. Detection of microleakage around dental restorations: a review. Oper Dent 1997;22(4): 173–85.
[10] Hekimoglu C, Anil N, Yalcin E. A microleakage study of ceramic laminate veneers by autoradiography: effect of incisal edge preparation. J Oral Rehabil 2004;31:265–70. [11] Cox CF, Felton D, Bergenholtz G. Histopathological
response of infected cavities treated with Gluma and Scotchbond dentin bonding agents. Am J Dent 1988;1:189–94.
[12] Kidd EAM. Microleakage: a review. J Dent 1976;4:199–206. [13] Kanka J. Microleakage of five dentin bonding systems.
Dent Mater 1989;5:415–6.
[14] Lacy AM, Wada C, Du W, Watanabe L. In vitro
microleakage at the gingival margin of porcelain and resin veneers. J Prosthet Dent 1991;67(1):7–10.
[15] Zaimo ˘glu A, Karaa ˘gac¸lio ˘glu L, ¨Uc¸tas¸li S. Influence of porcelain materials and composite luting resin on microleakage of porcelain veneers. J Oral Rehabil 1992;19:319.
[16] Retief DH. Do adhesives prevent microleakage? Int Dent J 1994;44:19–26.
[17] Sim C, Neo J, Kiam Chua EK, Tan BY. The effect of dentin bonding agents on the microleakage of porcelain veneers. Dent Mater 1994;10(4):278–81.
[18] Tay FR, Gwinnett AJ, Pang KM, Wei SHV. Variability in microleakage observed in a total-etch wet-bonding technique under different handling conditions. J Dent Res 1995;74:1168–78.
[19] Hammesfahr PD, Huang CT, Shaffer SE. Microleakage and bond strength of resin restorations with various bonding agents. Dent Mater 1987;3:194–9.
[20] Tay FR, Pashley DH. Water treeing—a potential mechanism for degradation of dentin adhesives. Am J Dent
2003;16(1):6–12.
[21] De Munk J, Vargas MA, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B. Bonding of an
auto-adhesive luting material to enamel and dentin. Dent Mater 2004;20:963–71.
[22] Tay FR, Sano H, Carvalho R, Pashley EL, Pashley DH. An ultrastructural study of the influence of acidity of
self-etching primers and smear layer thickness on bonding to intact dentin. J Adhes Dent 2000;2(2):83–98.
[23] Tay FR, Pashley DH, Suh BI, Carvalho RM, Itthagarun A. Single-step adhesives are permeable membranes. J Dent 2002;30:371–82.
[24] Tay FR, Pashley DH, Peters MC. Adhesive permeability affects composite coupling to dentin treated with a self-etch adhesive. Oper Dent 2003;28(5):610–21. [25] Tay FR, Frankenberger R, Krejci I, Bouillaguet S, Pashley
DH, Carvalho RM, Lai CNS. Single-bottle adhesives behave as permeable membranes after polymerization. I. In vivo evidence. J Dent 2004;32(8):611–21.
[26] Pashley EL, Agee KA, Pashley DH, Tay FR. Effects of one versus two applications of an unfilled, all-in-one adhesive on dentin bonding. J Dent 2002;30:83–90.
[27] Pashley DH, Tay FR. Aggressiveness of contemporary self-etching adhesives. Part II: etching effects on unground enamel. Dent Mater 2001;17:430–44.