Breastfeeding and
Human Lactation,
Third Edition
Jan Riordan, EdD, RN, IBCLC, FAAN
JONES AND BARTLETT PUBLISHERS
TeAM
YYePG
Jones and Bartlett Series in Breastfeeding/Human Lactation
Case Studies in Breastfeeding: Problem-Solving Skills and Strategies,Cadwell/Turner-Maffei
Clinical Lactation: A Visual Guide, Auerbach
Coach’s Notebook: Games and Strategies for Lactation Education, Smith
Comprehensive Lactation Consultant Exam Review, Smith
Core Curriculum for Lactation Consultant Practice, Walker, editor
Counseling the Nursing Mother: A Lactation Consultant’s Guide, Third Edition,Lauwers/Shinskie
Impact of Birthing Practices on Breastfeeding: Protecting the Mother and Baby Continuum,Kroeger with Smith
The Lactation Consultant in Private Practice: The ABCs of Getting Started,Smith
Reclaiming Breastfeeding for the United States: Protection, Promotion and Support, Cadwell
Ten Steps to Successful Breastfeeding: An 18 Hour Interdisciplinary Breastfeeding Management Course for the United States, Cadwell/Turner-Maffei
Breastfeeding and Human
Lactation
Third Edition
Jan Riordan, EdD, RN, IBCLC, FAAN
Professor
School of Nursing
Wichita State University
Wichita, Kansas
Lactation Consultant
Via Christi Regional Medical Center
St. Joseph Campus
World Headquarters
Jones and Bartlett Publishers 40 Tall Pine Drive
Sudbury, MA 01776 978-443-5000 info@jbpub.com www.jbpub.com
Copyright © 2005 by Jones and Bartlett Publishers, Inc. Cover image © InJoy Productions, Inc.
All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission from the copyright owner.
Library of Congress Cataloging-in-Publication Data
Breastfeeding and human lactation / [edited by] Jan Riordan.— 3rd ed. p. ; cm.
Includes bibliographical references and index. ISBN 0-7637-4585-5 (hardcover)
1. Breast feeding. 2. Lactation.
[DNLM: 1. Breast Feeding. 2. Infant Nutrition. 3. Lactation. 4. Milk, Human. WS 125 B8293 2004] I. Riordan, Jan.
RJ216.B775 2004
649'.33—dc22 2003022400
Printed in the United States of America
08 07 06 05 04 10 9 8 7 6 5 4 3 2 1
Jones and Bartlett Publishers Canada 2406 Nikanna Road
Mississauga, ON L5C 2W6 CANADA
Jones and Bartlett Publishers International
Barb House, Barb Mews London W6 7PA UK
Chief Executive Officer:Clayton Jones Chief Operating Officer:Don W. Jones, Jr. President of Jones and Bartlett Higher Education and Professional Publishing:Robert W. Holland, Jr. V.P., Design and Production:Anne Spencer V.P., Manufacturing and Inventory Control: Therese Bräuer
V.P. of Sales and Marketing:William Kane Acquisitions Editor:Penny M. Glynn Production Manager:Amy Rose
Editorial Assistant: Amy Sibley
Associate Production Editor:Jenny L. McIsaac Director of Marketing:Alisha Weisman Marketing Manager:Edward McKenna Manufacturing Buyer:Amy Bacus Cover Design:Anne Spencer
Composition:Modern Graphics Incorporated Printing and Binding:Malloy Inc.
S E C T I O N 1
H
I STOR ICAL AN D
W
OR K
P
E R S P ECTIVE S
T A B L E O F C O N T E N T S
Preface xxi Chapter Authors xxiv
Acknowledgements xxiii
C H A P T E R 1
Tides in Breastfeeding Practice
3
Evidence About Breastfeeding Practices 3
Large-Scale Surveys 3
Other Evidence 4
The Biological Norm in Infant Feeding 5
Early Human Evolution 5
Early Breastfeeding Practices 5
The Replacement of Maternal Breastfeeding 5
Wet-Nursing 5
Hand-Fed Foods 6
Timing of the Introduction of Hand-Feeding 7
Technological Innovations in
Infant Feeding 8
The Social Context 8
The Technological Context 9
The Role of the Medical Community 9
The Prevalence of Breastfeeding 12
United States, England, and Europe 12
Developing Regions 13
The Cost of Not Breastfeeding 15
Health Risks of Using Manufactured
Infant Milks 16
Economic Costs of Using Manufactured
Infant Milks 16
The Promotion of Breastfeeding 18
Breastfeeding Promotion in the
United States 19
International Breastfeeding Promotion 20
Private Support Movements 23
Summary 24
Key Concepts 25
Internet Resources 26
References 27
C H A P T E R 2
Work Strategies and the
Lactation Consultant
31
History 31
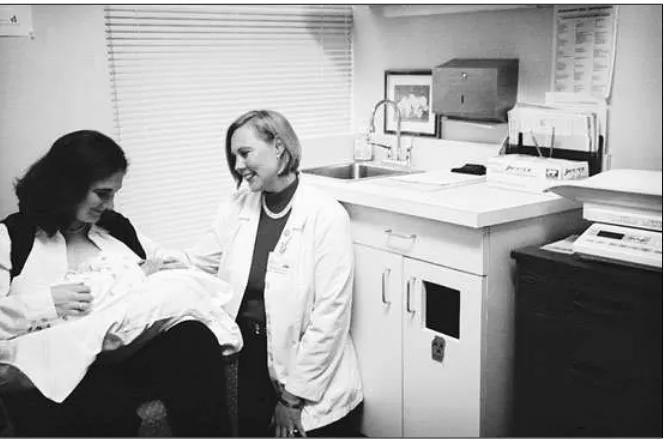
Do Lactation Consultants Make a
Difference? 32
Certification 32
Getting a Job as a Lactation Consultant 35
Interviewing for a Job 36
Gaining Clinical Experience 36
LC Education 37
Lactation Programs 38
Workload Issues 41
Developing a Lactation Program 41
Marketing 44
The Unique Characteristics of Counseling
Breastfeeding Women 44
Roles and Responsibilities 45
Stages of Role Development 46
Lactation Consultants in the
Community Setting 47
Medical Office 47
Lactation Consultants and
Volunteer Counselors 48
Networking 48
Reporting and Charting 49
Clinical Care Plans 50
Legal and Ethical Considerations 51
viii Breastfeeding and Human Lactation
Reimbursement 53
Insurance and Third-Party Payment 53
Coding 56
Private Practice 57
The Business of Doing Business 57
Payment and Fees 58
Partnerships 59
Summary 60
Key Concepts 61
Internet Resources 62
References 62
S E C T I O N 2
A
NATOM ICAL AN D
B
IOLOG ICAL
I
M P E RATIVE S
C H A P T E R 3
Anatomy and Physiology
of Lactation
67
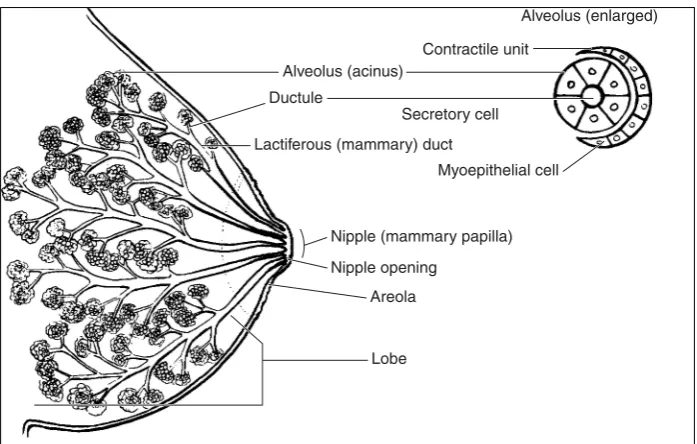
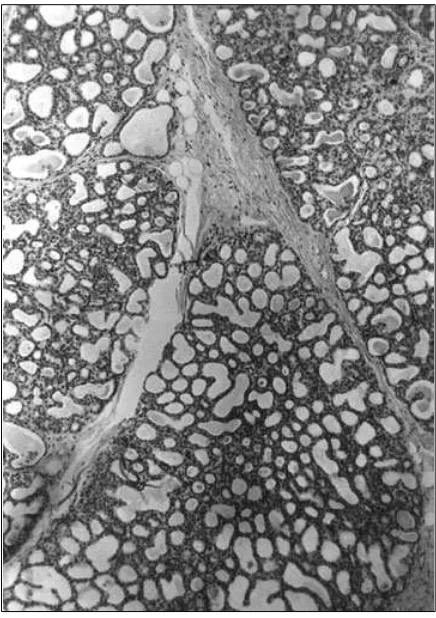
Mammogenesis 67
Breast Structure 69
Variations 72
Pregnancy 72
Lactogenesis 73
Delay in Lactogenesis 74
Hormonal Influences 74
Progesterone 75
Prolactin 75
Cortisol 77
Thyroid-Stimulating Hormone 77
Prolactin-Inhibiting Factor 77
Oxytocin 78
Milk Production 79
Autocrine Versus Endocrine 79
Galactopoiesis 80
Galactorrhea 80
Clinical Implications: Mother 80
Breast Assessment 80
Classification of Nipple Function 82
Concepts to Practice 82
Newborn Oral Development 83
Suckling 85
Breathing and Suckling 87
Frequency of Feedings 89
Summary 90
Key Concepts 90
References 92
C H A P T E R 4
The Biological Specificity
of Breastmilk
97
Milk Synthesis and Maturational Changes 98
Energy, Volume, and Growth 98
Caloric Density 99
Milk Volume and Storage Capacity 100 Differences in Milk Volume
Between Breasts 102
Infant Growth 103
Nutritional Values 103
Fat 103
Lactose 105
Protein 106
Vitamins and Micronutrients 106
Minerals 108
Preterm Milk 110
Anti-infective Properties 111
Gastroenteritis and Diarrheal Disease 111
Respiratory Illness 112
Otitis Media 114
Contents ix
Chronic Disease Protection 115
Childhood Cancer 116
Allergies and Atopic Disease 116
Asthma 117
The Immune System 117
Active Versus Passive Immunity 117
Cells 118
Antibodies/Immunoglobulins 119
Nonantibody Antibacterial Protection 120 Anti-inflammatory and Immunomodulating
Components 121
Bioactive Components 122
Enzymes 122
Growth Factors and Hormones 123
Taurine 124
Implications for Clinical Practice 124
Summary 126
Key Concepts 126
Internet Resources 127
References 128
Appendix 4-A: Composition of Human Colostrum and Mature Breastmilk 136
C H A P T E R 5
Drug Therapy
and Breastfeeding
137
The Alveolar Subunit 138
Drug Transfer into Human Milk 139
Passive Diffusion of Drugs into Milk 140
Ion Trapping 141
Molecular Weight 141
Lipophilicity 142
Milk/Plasma Ratio 142
Maternal Plasma Levels 142
Bioavailability 143
Drug Metabolites 143
Calculating Infant Exposure 143
Unique Infant Factors 144
Maternal Factors 146
Minimizing the Risk 146
Effect of Medications on Milk Production 146
Drugs That May Inhibit Milk Production 146 Drugs That May Stimulate
Milk Production 148
Herbs 149
Review of Selected Drug Classes 149
Analgesics 149
Antibiotics 150
Antihypertensives 153
Psychotherapeutic Agents 153
Corticosteroids 157
Thyroid and Antithyroid Medications 157
Drugs of Abuse 158
Radioisotopes 159
Radiocontrast Agents 159
Summary 161
Key Concepts 162
Internet Resources 162
References 162
C H A P T E R 6
Viruses and Breastfeeding
167
HIV and Infant Feeding 167
Exclusive Breastfeeding 168
What We Know 168
Treatment and Prevention 170
Health-Care Practitioners 171
Counseling 171
Herpes Simplex Virus 172
Chickenpox/Varicella 173
x Breastfeeding and Human Lactation
Rubella 176
Hepatitis B 176
Hepatitis C 176
Human Lymphotropic Virus 177
West Nile Virus 177
Implications for Practice 178
Summary 179
Key Concepts 179
Internet Resources 180
References 181
S E C T I O N 3
P
R E NATAL
, P
E R I NATAL
,
AN D
P
OSTNATAL
P
E R IODS
C H A P T E R 7
Perinatal and
Intrapartum Care
185
Breastfeeding Preparation 185
Early Feedings 186
Feeding Positions 191
Latch-on and Positioning Techniques 191
The Infant Who Has Not Latched-On 192
Plan for the Baby Who Has Not
Latched-On Yet 194
Establishing the Milk Supply 194
Assessment of the Mother’s
Nipples and Breasts 196
Baby Problems That May Cause
Difficulty with Latch-on 196
The 34 to 38 “Weeker” 197
Feeding Methods 198
Cup-Feeding 198
Finger-Feeding 199
Nipple Shields 200
Hypoglycemia 201
Cesarean Births 204
Breast Engorgement 205
Breast Edema 206
Hand Expression 207
Clinical Implications 209
Breastfeeding Assessment 209
Discharge Planning 210
Basic Feeding Techniques 210
Signs That Intervention Is Needed 211
Discharge 211
Summary 212
Key Concepts 212
Internet Resources 214
References 214
C H A P T E R 8
Postpartum Care
217
Hydration and Nutrition in the Neonate 217
Signs of Adequate Milk Intake 218 Milk Supply––Too Much or Too Little 218 Temporary Low Milk Supply or
Delayed Lactogenesis 220
Effect of Pharmaceutical Agents on
Milk Supply 220
Too Much Milk 221
Nipple Pain 221
Treatments for Painful Nipples 225
Nipple Creams and Gels 225
Engorgement + Milk Stasis = Involution 228
Breast Massage 228
Clothing, Leaking, Bras, and
Contents xi
Infant Concerns 230
Pacifiers 230
Stooling Patterns 231
Jaundice in the Newborn 232
Breast Refusal and Latching Problems 232
Later Breast Refusal 234
Crying and Colic 234
Multiple Infants 236
Full-Term Twins or Triplets 237
Preterm or Ill Multiples 237
Putting It All Together 238
Partial Breastfeeding and Human
Milk Feeding 239
Breastfeeding During Pregnancy 240
Clinical Implications 241
Summary 242
Key Concepts 242
Internet Resources 242
References 243
C H A P T E R 9
Breast-Related Problems
247
Nipple Variations 247
Inverted or Flat Nipples 247
Absence of Nipple Pore Openings 248
Large or Elongated Nipples 248
Plugged Ducts 248
Mastitis 250
Treatment for Mastitis 251
Types of Mastitis 252
Breast Abscess 254
Breast and Nipple Rashes, Lesions, and
Eczema 254
Candidiasis (Thrush) 255
Treatment 256
Breast Pain 260
Vasospasm 260
Milk Blister 261
Mammoplasty 261
Breast Reduction 261
Mastopexy 263
Breast Augmentation 263
Breast Lumps and Surgery 265
Galactoceles 266
Fibrocystic Disease 267
Bleeding from the Breast 267
Breast Cancer 268
Lactation Following Breast Cancer 269
Clinical Implications 270
Summary 271
Key Concepts 271
Internet Resources 273
References 273
C H A P T E R 1 0
Low Intake in the Breastfed
Infant: Maternal and
Infant Considerations
277
Factors That Influence Maternal
Milk Production 277
Normal Milk Intake and Rate of Gain 279
US Growth Curves 280
Current Growth Curves Still
Underrepresent Breastfeeding 280
Low Intake and Low Milk Supply: Definit-ions and Incidence of Occurrence 282
Confusing Terminology and
Nonstandardized Research 282
The Infant’s Presentation 283
The Mother’s Presentation 285
Abnormal Patterns of Growth: The Baby
Who Appears Healthy 286
Inadequate Weight Gain in the
First Month 286
xii Breastfeeding and Human Lactation
Oral-Motor Dysfunction
(Ineffective Suckling) 286
Gastroesophageal Reflux/Cow Milk
Allergy/Oversupply 290
Nonspecific Neurological Problems 291 Ankyloglossia (Tight Frenulum,
Tongue-Tie) 291
Abnormal Patterns of Growth:
The Baby with Obvious Illness 292
Maternal Considerations:
The Mother Who Appears Healthy 293
Delayed Lactogenesis 293
Stress 293
Inverted Nipples 294
Nipple Shields 294
Medications and Substances 294
Hormonal Alterations 294
Breast Surgery 295
Insufficient Glandular Development
of the Breast 295
Psychosocial Factors 296
Maternal Nutrition 296
Maternal Considerations:
Obvious Illness 296
History, Physical Exam, and
Differential Diagnosis 296
History 296
Physical Examination 296
Differential Diagnosis 297
Clinical Management 297
Determining the Need
for Supplementation 297
Intervention 297
Reducing the Amount
of Supplementation 300
Family and Peer Support 300
When Maternal Milk Supply Does
Not Increase 300
Special Techniques for Management of
Low Intake or Low Supply 300
Breast Massage 300
Switch Nursing 300
Feeding-Tube Device 301
Test Weighing 303
Galactagogues 303
Hindmilk 304
Summary 305
Key Concepts 306
Internet Resources 307
References 307
C H A P T E R 1 1
Jaundice and the
Breastfed Baby
311
Neonatal Jaundice 312
Assessment of Jaundice 313
Postnatal Pattern of Jaundice 314
Breastmilk Jaundice 314
Breast-Nonfeeding Jaundice 314
Bilirubin Encephalopathy 316
Evaluation of Jaundice 316
Diagnostic Assessment 317
Management of Jaundice 318
Key Concepts 319
Internet Resources 320
References 320
C H A P T E R 1 2
Breast Pumps and
Other Technologies
323
Concerns of Mothers 323
Stimulating the Milk-Ejection Reflex 324
Hormonal Considerations 328
Prolactin 328
Clinical Implications 329
Oxytocin 330
Pumps 330
Contents xiii
Compression 331
The Evolution of Pumps 331
A Comparison of Pumps 332
Manual Hand Pumps 333
Battery-Operated Pumps 335
Electric Pumps 336
Simultaneous and/or
Sequential Pumping 338
Flanges 338
Miscellaneous Pumps 342
Pedal Pumps 342
Clinical Implications Regarding
Breast Pumps 342
When Pumps Cause Problems 345
Sample Guidelines for Pumping 345
Common Pumping Problems 347
Nipple Shields 349
Review of Literature 350
Types of Shields 351
Shield Selection and Instructions 351
Weaning from the Shield 352
Responsibilities 352
Breast Shells 354
Feeding-Tube Devices 355
Situations for Use 355
Summary 357
Key Concepts 358
Internet Resources 361
References 361
Appendix 12-A: Manufacturers/
Distributors of Breast Pumps 365
C H A P T E R 1 3
Breastfeeding the
Preterm Infant
367
Suitability of Human Milk for Preterm
Infants 367
Mothers of Preterm Infants 368
Rates of Breastfeeding Initiation and
Duration 370
Research-Based Lactation Support
Services 370
The Decision to Breastfeed 370
Facilitating an Informed Decision 370 Alternatives to Exclusive, Long-Term
Breastfeeding 370
Models for Hospital-Based Lactation
Support Services 371
Initiation of Mechanical Milk Expression 372
Principles of Milk Expression 372
Selecting a Breast Pump 372
Milk-Expression Technique 373
Milk Expression Schedule 374
Written Pumping Records 374
Maintaining Maternal Milk Volume 376
Expressed Milk Volume Guidelines 376
Preventing Low Milk Volume 376
Skin-to-Skin (Kangaroo) Care 377
Evidence-Based Guidelines for Milk
Collection, Storage, and Feeding 378
Guidelines for Collection and Storage
of Expressed Mother’s Milk (EMM) 378 Preparing Expressed Mother’s Milk
for Infant Feeding 379
Special Issues Regarding the Feeding
of EMM 380
Volume Restriction Status 382
Commercial Nutritional Additives 382
Hindmilk Feeding 382
Methods of Milk Delivery 383
Maternal Medication Use 383
Feeding at Breast in the NICU 384
Suckling at the Emptied Breast 384 The Science of Early Breastfeeding 385 Progression of In-Hospital Breastfeeding 390 Milk Transfer During Breastfeeding 390
Discharge Planning for
Postdischarge Breastfeeding 396
Getting Enough: Determining the Need
xiv Breastfeeding and Human Lactation
Methods to Deliver Extra Milk Feedings
Away from the Breast 398
Postdischarge Breastfeeding Management 398
Summary 399
Key Concepts 399
Internet Resources 400
References 401
Appendix 13-A: The Preterm Infant
Breastfeeding Behavior Scale (PIBBS) 407
C H A P T E R 1 4
Donor Human Milk Banking
409
Defining Donor Milk Banking 409
A Brief History of Human Milk Banking 409
Foundations of Donor Human Milk
Banking: Pre-1975 409
Donor Human Milk Banking in the
United States: Post-1975 410
Potential Hazards of Informal Sharing of
Human Milk 411
Donor Human Milk Banking Beyond
North America 412
The Impact of Culture on Donor
Milk Banking 413
The Benefits of Banked Donor
Human Milk 413
Species Specificity 413
Ease of Digestion 413
Promotion of Growth, Maturation,
and Development of Organ Systems 414
Immunological Benefits 414
Clinical Uses 414
Distribution of Banked Donor Milk:
Setting Priorities 414
Classifying Clinical Uses: Is Donor
Milk Food or Medicine? 415
Current Practice 420
Donor Selection and Screening 420
Collection 422
Pasteurization 422
Packaging and Transport 425
Costs of Banked Donor Milk 425
Policy Statements Supporting the
Use of Banked Donor Human Milk 425
Summary 426
Key Concepts 427
Internet Resources 427
References 427
Appendix 14-A: Storage and Handling
of Expressed Human Milk 432
S E C T I O N 4
B
EYON D
P
OSTPARTU M
C H A P T E R 1 5
Maternal Nutrition
During Lactation
437
Maternal Caloric Needs 438
Maternal Fluid Needs 439
Weight Loss 439
Exercise 440
Calcium Needs and Bone Loss 441
Vegetarian Diets 442
Dietary Supplements 442
Foods That Pass Into Milk 443
Caffeine 443
Food Flavorings 443
Allergens in Breastmilk 443
The Goal of the Maternal Diet
Contents xv
Nutrition Basics 446
Energy 446
Macronutrients 447
Carbohydrates 447
Protein 447
Fat 448
Micronutrients 448
Vitamins 448
Minerals 449
Clinical Implications 449
Summary 453
Key Concepts 453
Internet Resources 454
References 454
C H A P T E R 1 6
Women’s Health
and Breastfeeding
459
Alterations in Endocrine and
Metabolic Functioning 459
Diabetes 459
Thyroid Disease 461
Pituitary Dysfunction 462
Polycystic Ovarian Syndrome 462
Theca Lutein Cysts 462
Cystic Fibrosis 463
Acute Illness and Infections 463
Tuberculosis 464
Group B Streptococcus 464
Dysfunctional Uterine Bleeding 465
Maternal Immunizations 465
Surgery 465
Donating Blood 466
Relactation 467
Induced Lactation 467
Domperidone, Metoclopramide,
and Sulpride 468
Autoimmune Diseases 470
Systemic Lupus Erythematosus 470
Multiple Sclerosis 471
Rheumatoid Arthritis 471
Physically Challenged Mothers 472
Seizure Disorders 473
Headaches 475
Postpartum Depression 476
Clinical Implications 477
Medications and Herbal Therapy
for Depression 478
Support for the Mother with
Postpartum Depression 480
Asthma 480
Smoking 480
Poison Ivy Dermatitis 481
Diagnostic Studies Using Radioisotopes 481
The Impact of Maternal Illness
and Hospitalization 482
Summary 482
Key Concepts 483
Internet Resources 484
References 484
C H A P T E R 1 7
Maternal Employment
and Breastfeeding
487
Why Women Work 487
Historical Perspective 488
The Effect of Work on Breastfeeding 488
Strategies to Manage Breastfeeding
and Work 489
Prenatal Planning and Preparation 489
Return to Work 491
Hand Expression and Pumping 492
Human Milk Storage 493
Fatigue and Loss of Sleep 496
Maintaining an Adequate Milk Supply 496
xvi Breastfeeding and Human Lactation
Workplace Strategies 497
Lactation Programs in Work Sites 498
The Employer’s Perspective 500
Community Strategies 501
Health-Care Providers and
Lactation Consultants 501
Breastfeeding Support Groups 501
National and International Strategies 501
Legislative Support and
Public Advocacy 501
International Labour Organization 503
Clinical Implications 503
Summary 505
Key Concepts 506
Internet Resources 507
Other Resources 507
References 507
C H A P T E R 1 8
Child Health
509
Developmental Outcomes and Infant
Feeding 509
Growth and Development 511
Physical Growth 511
Weight and Length 512
Senses 513
Reflexes 514
Levels of Arousal 514
Theories of Development 514
Nature Versus Nurture 514
Social Development 517
Language and Communication 517
Attachment and Bonding 520
Temperament 523
Stranger Distress 523
Separation Anxiety 523
Clinical Implications 525
Immunizations 525
Vitamin D and Rickets 527
Dental Health and Orofacial
Development 527
Solid Foods 528
Introducing Solid Foods 528
Choosing the Diet 529
Choosing Feeding Location 531
Delaying Solid Foods 531
Obesity 532
Co-Sleeping 532
Long-Term Breastfeeding 533
Weaning 533
Implications for Practice 534
Summary 535
Key Concepts 535
Internet Resources 536
References 536
C H A P T E R 1 9
The Ill Child:
Breastfeeding Implications
541
Team Care for the Child with
Feeding Difficulties 541
Feeding Behaviors of the Ill Infant/Child 541
What to Do If Weight Gain
Is Inadequate 544
What to Do When Direct Breastfeeding
Is Not Sufficient 544
Alternative Feeding Methods 546
Care of the Hospitalized Breastfeeding
Infant/Child 548
Home from the Hospital:
The Rebound Effect 550
Perioperative Care of the Breastfeeding
Infant/Child 551
Contents xvii
Care of Children with
Selected Conditions 552
Infection 552
Gastroenteritis 552
Respiratory Infections 554
Pneumonia 555
Bronchiolitis 555
Respiratory Syncytial Virus 556
Otitis Media 556
Meningitis 556
Alterations in Neurological Functioning 557
Down Syndrome or Trisomy 21 560
Neural Tube Defects 560
Hydrocephalus 561
Congenital Heart Disease 561
Oral/Facial Anomalies 563
Cleft Lip and Palate 563
Pierre Robin Sequence 566
Choanal Atresia 568
Gastrointestinal Anomalies
and Disorders 568
Esophageal Atresia/Tracheoesophageal
Fistula 568
Gastroesophageal Reflux 569
Pyloric Stenosis 571
Imperforate Anus 571
Metabolic Dysfunction 571
Phenylketonuria 572
Galactosemia 572
Congenital Hypothyroidism 574
Type I Diabetes 575
Celiac Disease 575
Cystic Fibrosis 575
Allergies 576
Food Intolerance 579
Lactose Intolerance 579
Psychosocial Concerns 579
Family Stress 579
Coping with Siblings 581
Chronic Grief and Loss 581
The Magic-Milk Syndrome 581
The Empty Cradle...When a Child Dies 582
Caring for Bereaved Families 582
Summary 583
Key Concepts 583
Internet Resources 584
References 585
C H A P T E R 2 0
Infant Assessment
591
Perinatal History 591
Gestational Age Assessment 591
The New Ballard Score 594
Indicators of Effective Breastfeeding
and Assessment Scales 598
Breastfeeding Behaviors
and Indicators 598
Breastfeeding Scales and Tools 598 Summary of Breastfeeding
Assessment Scales 600
Physical Assessment 600
Transitional Assessment 600
Skin 604
Birthmarks 605
Head 606
Ears/Eyes 606
Nose 607
Mouth 607
Neck 608
Chest 608
Abdomen 609
Genitalia 609
Back and Spine 609
Extremities 609
Elimination 610
Behavioral Assessment 611
Sleep-Wake States 614
Neurobehavioral Cues and Reflexes 614
Summary 616
Key Concepts 616
xviii Breastfeeding and Human Lactation
Appendix 20-A: Infant Breastfeeding
Assessment Tool (IBFAT) 618
Appendix 20-B: LATCH
Assessment Tool 618
Appendix 20-C: Mother-Baby
Assessment Scale 619
Appendix 20-D: Via Christi Breastfeeding
Assessment Tool 620
C H A P T E R 2 1
Fertility, Sexuality,
and Contraception
During Lactation
621
Fertility 621
The Demographic Impact
of Breastfeeding 621
Mechanisms of Action 622
Lactational Amenorrhea 623
The Suckling Stimulus 624
The Repetitive Nature of the Recovery
of Fertility 628
The Bellagio Consensus 630
Sexuality 632
Libido 632
Sexual Behavior During Lactation 637
Contraception 639
The Contraceptive Methods 639
Clinical Implications 645
Summary 647
Key Concepts 647
References 648
S E C T I O N 5
S
OCIOCU LTU RAL AN D
R
E S EARCH
I
SS U E S
C H A P T E R 2 2
Research, Theory,
and Lactation
655
Theories Related to Lactation Practice 655
Maternal Role Attainment Theory 656 Parent-Child Interaction Model 656 Bonding and Attachment Theory 657 Theory of Darwinian and
Evolutionary Medicine 657
Self-Care Theory 658
Self-Efficacy Theory 658
Theory of Planned Behavior and
Theory of Reasoned Action 658
Types of Research Methods 659
Qualitative Methods 659
Quantitative Methods 660
Additional Methods and Approaches
for Breastfeeding Research 662
Elements of Research 663
Research Problem and Purpose 663
Variables, Hypotheses, and
Operational Definitions 665
Review of Literature 667
Protection of the Rights of Human
Subjects 667
Method 668
Data Analysis 669
Application of Methods to
Qualitative Approaches 669
Sampling 669
Data Collection 670
Data Analysis 670
Trustworthiness of Qualitative Research 671
Application of Methods to
Quantitative Approaches 671
Sampling and Sample Size 671
Data Collection 672
Reliability and Validity 672
Data Analysis 674
Results, Discussion, Conclusions,
and Dissemination 677
Contents xix
Using Research in Clinical Practice 680
Perspectives of Research Methodologies 680
Positivist and Postpositive Perspective 681 Naturalistic, Humanistic, or
Interpretive Perspective 681
Critical or Emancipatory Perspective 681
Summary 682
Key Concepts 683
Internet Resources 684
References 684
Appendix 22-A: Research Terms 687
C H A P T E R 2 3
Breastfeeding Education
689
Educational Programs 689
Distance Learning and Web Courses 690
Learning Principles 690
Adult Education 691
Curriculum Development 692
Parent Education 692
Prenatal Education 694
Early Breastfeeding Education 694
Continuing Support for
Breastfeeding Families 697
How Effective Is
Breastfeeding Education? 697
Teaching Strategies 698
Small Group Dynamics 700
Multimedia Presentations 700
Slides 701
Transparencies 701
Television, Videotapes, and DVDs 701
Compact Discs 702
Educational Materials 702
Education for At-Risk Populations 703
Adolescents 704
Older Parents 705
Educational Needs and Early Discharge 706
Continuing Education 706
Objectives and Outcomes 707
The Team Approach 708
Childbirth Educators 708
Nurses 708
Lactation Consultants 709
Physicians 709
Dietitians 709
Community Support Groups 709
Summary 709
Key Concepts 710
Internet Resources 711
References 711
C H A P T E R 2 4
The Cultural Context
of Breastfeeding
713
The Dominant Culture 714
Ethnocentrism Versus Relativism 714
Assessing Cultural Practices 715
Language Barriers 715
The Effects of Culture on Breastfeeding 716
Rituals and Meaning 719
Colostrum 719
Sexual Relations 719
Wet-Nursing 720
Other Practices 720
Contraception 720
Infant Care 721
Maternal Foods 722
“Hot” and “Cold” Foods 722
Herbs and Galactogogues 723
Weaning 723
Types of Weaning 724
Implications for Practice 725
Summary 726
xx Breastfeeding and Human Lactation
Internet Resources 727
References 727
C H A P T E R 2 5
Families
729
Family Forms and Functions 729
Family Theory 730
Social Factors that Influence
Breastfeeding 731
Fathers 733
The Adolescent Mother 736
The Low-Income Family 737
Lack of Information 737
Hospital Practices 738
The Importance of Peer Counselors 739
The Downside of Family Experience 739
Violence 740
Childhood Sexual Abuse 741
Summary 742
Key Concepts 742
Internet Resources 743
References 743
APPENDIXES 747
A. Clinical Competencies for
IBCLC Practice 749
B. Code of Ethics 754
C. Summary of Eligibility Pathway Requirements to Become Certified
by IBLCE 756
D. Prototype Lactation Consultant
Job Description 758
E. Tables of Equivalencies and Methods
of Conversion 761
F. Infant Weight Conversion Table 762 G. Breastfeeding Weight Loss Table 763
H. Patient History 764
Glossary 773
Index 785
I have worked in the field of lactation since the early 1960s, first as a La Leche Leader and later as a lactation consultant when it became a professional practice discipline in 1985. As I look back over those years I am struck both by how different things are now and by how much things have stayed the same. Although the breastfeeding initiation rate in the United States has risen to almost 70 percent––a vast improvement from 20 percent in the 1960s!––it still takes time and patience to help a new breast-feeding mother get her baby onto the breast.
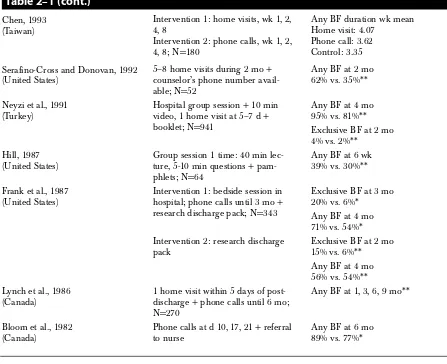
New knowledge has changed the field. Re-search studies now verify that breastfed children are more intelligent and that not breastfeeding costs the U.S. health care system billions of dollars annually. Because of the new awareness of the importance of breastfeeding, the number and influence of lacta-tion consultants has expanded. The Internalacta-tional Board of Lactation Consultants has certified more than 10,000 health care workers in 36 countries. Most hospitals, large and small, offer lactation ser-vices of some type and employ lactation consul-tants. Lest anyone question the powerful, positive influence of interventions by health care workers on breastfeeding, they only need to review the table of intervention studies in Chapter 2. At the same time, lest we follow that conflicted path that led to the medicalization of childbirth, we must listen to voices that warn of the danger of lactation consul-tants medicalizing infant feeding.
Other changes affect lactation practice. The in-surance industry now drives the health care system, reversing the reward system in favor of short hospi-tal stays, which are now two days or less in the U.S. for vaginal births. While these short stays mean that breastfeeding mothers and babies return home less likely to be exposed to hospital infections and to supplementary feedings, this brief time allows al-most no opportunity to ensure that the baby is breastfeeding effectively. Mothers still needing care themselves return home to assume full-time child-care before they feel physically able to do so. Fol-low-up care of a new family at home should be universal, yet many mothers of preterm and “near-term” breastfed infants who are developmentally
immature leave the hospital without any plan for as-sistance.
This text brings together in a single volume the latest clinical techniques and research findings that direct evidence-based clinical practice. I have been fortunate in being able to enlist a dozen breastfeed-ing experts recognized around the world to help with the writing of this extensive volume. Dr. Kathleen Auerbach, the much-missed former co-author of this book, remains as co-author of two chapters.
Over 1,000 research studies support the clinical recommendations in this book. The Internet and MEDLINE made the literature searches so much easier for this edition––a sea of change from writing the first two editions. The Internet also made possi-ble quick correspondence with colleagues and chapter authors as this book progressed. Addresses of helpful resources on the Internet have been added to each chapter.
Like the earlier editions, the third edition of this text has a clear clinical focus. A new chapter on in-fant assessment reflects current expectations that the health care worker working with the breastfeed-ing dyad can perform a total assessment of the baby. Nearly every chapter contains a clinical im-plications section. Important concepts discussed in chapters are summarized at the end of each chapter––a new feature that will make studying eas-ier. Throughout the book are new references deemed by the authors to be the most important from the vastly expanded research and clinical lit-erature. Some older references that introduced new ideas that are now accepted common knowledge have been regretfully removed to make room for new research. The glossary of key terms relating to lactation has been expanded in this edition.
Section 1contrasts the past and present. Chap-ter 1 presents the history of breastfeeding by plac-ing lactation and breastfeedplac-ing in its historical context. Chapter 2 fast-forwards to the work of the present-day health care worker who specializes in lactation and breastfeeding, and it addresses the re-ality of work-related issues of lactation consulting.
Section 2 focuses on basic anatomic and bio-logic imperatives of lactation. Clinical application of
P R E F A C E
xxii Breastfeeding and Human Lactation
techniques must be based on a clear understanding of the relationships between form, function, and bio-logical constructs. Thus this section, too, provides the background upon which to understand other as-pects of lactation and breastfeeding behavior.
Section 3is the clinical “heart” of the book that describes the basics of whatto do, whento do it, and how to do it when one assists the lactating mother. Section 3 thus concerns itself with the perinatal pe-riod in the birth setting and concerns during the postpartum period following the family’s return home—notably breast problems, neonatal jaundice, and infant weight gain. This section also addresses special needs of preterm babies and their mothers, and it critically evaluates breastfeeding devices and recommends how and when they are most appro-priately used. It concludes with a review of the de-velopment and current activities of human milk banking.
The first part of Section 4 focuses on the mother: maternal nutrition, the mother’s health, and returning to work. The topics then turn to the infant and child’s health and special health needs. The techniques of infant assessment are explained
and demonstrated with photographs in a new chap-ter. The section ends with a discussion of maternal sexuality and fertility.
Section 5begins with a careful look at research–– how it is conducted, why ongoing research is needed, and how research findings can be applied in clinical settings. The principles of education, the cor-nerstone of clinical practice, are explored next. The book concludes with the socio-cultural context of the breastfeeding family and explores the different ways in which the breastfeeding family functions within that context.
I gratefully acknowledge the contributions to this book made by the following individuals:
Judy Angeron BA, RN, IBCLC, Coordinator, Lac-tation Services, Via Christi Regional Medical Cen-ter, Wichita, Kansas
Kathleen G. Auerbach PhD, IBCLC, Ferndale, Washington
Suzanne Bentley MSN, CNM, IBCLC, Clinical Nurse Specialist, University of Kansas, Clinical In-structor, University of Kansas, School of Nursing, Kansas City, Kansas
Belinda Childs MN, ARNP, CDE, Clinic/Re-search Coordinator, Mid-America Diabetes Associ-ates, Wichita, Kansas
Mary Margaret Coates MS, IBCLC, TechEdit, Wheat Ridge, Colorado
Amy Ellington RN, BSN, Lactation Consultant, Via Christi Regional Medical Center, Wichita, Kansas
Barbara Gabbert-Bacon, La Leche League, Wi-chita, Kansas
Lenore Goldfarb, B.Comm, B.Sc, IBCLC, Herzl Family Practice Centre, Sir Mortimer B. Davis-Jewish General Hospital, Montreal, Quebec, Canada
Robert T. Hall MD, Professor, Children’s Mercy Hospital and Clinics, Kansas City, Missouri Eileen Hawkins MSN, ARNP, Wichita State Uni-versity, School of Nursing, Wichita, Kansas
Kerstin Hedberg-Nyqvist PhD, RN, IBCLC, Assis-tant Professor in Pediatric Nursing, Department of Women’s and Children’s Health, Uppsala Univer-sity,Uppsala, Sweden
Heather Hull MSN, PNP, Instructor, Wichita State University, Wichita, Kansas
Voni Miller RN, IBCLC, Lactation Consultant, Phoenix Children’s Hospital, Phoenix, Arizona Gerald Nelson MD, The University of Kansas School of Medicine, Wichita, Kansas
Amal Omer-Salim, MSc, Nutritionist, International Maternal and Child Health, Department of
Women’s and Children’s Health, Uppsala Univer-sity, Uppsala, Sweden
Virginia Phillips, IBCLC, Brisbane, Queensland, Australia
Christina M Smillie MD, FAAP, IBCLC, Breast-feeding Resources, Stratford, Connecticut
I am especially grateful to La Leche League Inter-national for providing the foundation for my breast-feeding education and to those institutions which encouraged and supported me in writing the book: the School of Nursing, Wichita State University, and Via Christi Regional Medical Center, both of Wichita, Kansas.
Finally, thanks to my family: Hugh, Michael, Neil and Shirley, Brian, Quinn and Rika Riordan, Teresa Riordan and Richard Chenoweth, Renee and Don Olmstead and our 11 (breastfed) grand-children.
A C K N O W L E D G E M E N T S
xxiv
Kathleen G. Auerbach,PhD, IBCLC Ferndale, Washington
Lois D. W. Arnold,PhD (C.), MPH, IBCLC National Commission on Donor Milk Banking East Sandwich, Massachusetts
Debi Leslie Bocar,PhD, RN, IBCLC Perinatal Educator, Mercy Health Center Director, Lactation Consultant Services Oklahoma City, Oklahoma
Yvonne Bronner,ScD, RD, LD
Professor and Director, Public Health Program Morgan State University
Baltimore, Maryland
Mary Margaret Coates,MS, IBCLC TechEdit
Wheat Ridge, Colorado
Lawrence M. Gartner,MD Professor Emeritus
Departments of Pediatrics and Obstetrics/ Gynecology
The University of Chicago Chicago, Illinois
Kathy Gill-Hopple,MSN, RN Instructor
Wichita State University, School of Nursing Wichita, Kansas
Thomas W. Hale,PhD, RPH Professor of Pediatrics
Texas Tech University, School of Medicine Amarillo, Texas
Marguerite Herschel,MD Associate Professor of Pediatrics
Medical Director, General Care Nursery The University of Chicago
Chicago, Illinois
Roberta J. Hewat,PhD, RN, IBCLC Associate Professor
University of British Columbia, School of Nursing,
Vancouver, British Columbia, Canada
Kay Hoover, MEd, IBCLC
Philadelphia Department of Public Health Philadelphia, Pennsylvania
Nancy Hurst,RN, MSN, IBCLC
Director, Lactation Program and Mother’s Own Milk Bank
Texas Children’s Hospital Assistant Professor of Pediatrics Baylor College of Medicine Houston, Texas
Kathy I. Kennedy,MA, Dr.PH
Director, Regional Institute for Health and Envi-ronmental Leadership,
University of Denver Associate Clinical Professor of Preventive Medicine,
University of Colorado Health Sciences Denver, Colorado
Mary Koehn,PhD, RN, MSN Assistant Professor
Wichita State University, School of Nursing Wichita, Kansas
Paula Meier,DNSc, RN, FAAN
NICU Lactation Program Director, Department of Maternal-Child Nursing,
Associate Director for Clinical Research, Section of Neonatology,
Rush-Presbyterian-St Luke’s Medical Center Chicago, Illinois
Sallie Page-Goertz,MN, CPNP, IBCLC Assistant Clinical Professor,
KU Children’s Center/Kansas University School of Medicine
Overland Park, Kansas
Nancy Powers,MD
Medical Director, Lactation Services Pediatrix Medical Group
Chapter Authors xxv
Wailaiporn Rojjanasrirat,PhD, MSN Research Assistant Professor
University of Kansas, School of Nursing Kansas City, Kansas
Linda J. Smith, BSE, FACCE, IBCLC Bright Future Lactation Resource Centre Ltd. Dayton, Ohio
Marsha Walker,RN, IBCLC Lactation Associates
Executive Director, National Alliance for Breast-feeding Advocacy
Research, Education, and Legal Branch Weston, Massachusetts
Karen Wambach,PhD, RN, IBCLC Assistant Professor
Just as the breastfeeding course flows and ebbs in
a woman’s life, so breastfeeding has experienced
flows and ebbs through the centuries. It takes a
vil-lage to return to breastfeeding, and community-based
programs that promote breastfeeding are successfully
and steadily increasing the rate of breastfeeding
around the world.
As more mothers choose to breastfeed, the need for
specialized help increases also. The visibility and
ac-ceptance of lactation consulting as an allied health
profession offers opportunities for practice in
hospi-tals, the community, and in private practice.
Ran-domized clinical trials consistently demonstrate that
lactation consultant services lengthen a mother’s
breastfeeding course and save money through
health-ier mothers and babies.
Historical and Work Perspectives
1
S E C T I O N
3
1
C
H
A
P
T
E
R
Throughout the world today, an infant is apt to re-ceive less breastmilk than at any time in the past. Until the 1940s, the prevalence of breastfeeding was high in nearly all societies. Although the feed-ing of manufactured milks and baby milks had begun before the turn of the century in parts of Eu-rope and North America, the practice spread slowly during the next decades. It was still generally lim-ited to segments of population elites, and it in-volved only a small percentage of the world’s people. During the post–World War II era, how-ever, the way in which most mothers in industrial-ized regions fed their infants began to change, and the export of these new practices to developing na-tions was underway.
Evidence About Breastfeeding
Practices
How do we know what we “know” about the preva-lence of breastfeeding? (The wordprevalenceis used here to mean the combined effect of breastfeeding initiation rates and breastfeeding continuance rates.) Before attempting to trace trends in infant feeding practices, let us consider the nature of the evidence.
Tides in Breastfeeding Practice
Mary Margaret Coates and Jan Riordan
Large-Scale Surveys
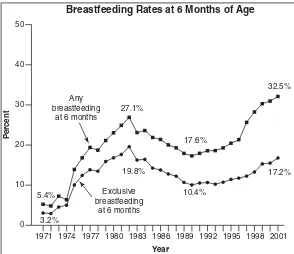
National surveys that produce the kind of represen-tative data that allow statistical evaluation have been available only since 1955. These surveys consist pri-marily of national fertility or natality surveys and of marketing surveys conducted by manufacturers of artificial baby milk. For most, exclusive breastfeed-ing is not a separate statistic. However, the percent-age of exclusive breastmilk feedings at hospital discharge can be found in state birth certificate data-bases (Feldman-Winter et al., 2002). A brief descrip-tion of nadescrip-tional surveys conducted in the United States follows (Grummer-Strawn & Li, 2000):
● National Health Interview Survey:A personal in-terview is conducted in 43,000 households. Questions about incidence and duration of breastfeeding are asked.
4 Historical and Work Perspectives
● Pediatric Nutrition Surveillance System (PedNSS): Statistics of breastfeeding incidence and duration in low-income populations are collected in pub-lic health clinics and reported annually. National, state, county, and clinic data are analyzed.
● WIC Participant Characteristics Study: Data on breastfeeding are collected each even-num-bered year by the Department of Agriculture.
● Ross Laboratories Mothers Survey: Questionnaires are mailed to new mothers whose names are obtained from a national sample of hospitals and physicians. For marketing purposes, data on type of milk fed is collected for up to 12 months for a given cohort. Data are published on an ad hoc basis. The survey currently func-tions as a baseline and monitoring data source for breastfeeding goals in Healthy People 2010.
● Mead-Johnson Longitudinal Study of Infant Feeding Practices:For marketing purposes, a panel of in-fants is followed for 12 months. Data is col-lected on incidence of, duration of, and changes in breastfeeding frequencies.
Outside the United States, representative data for countries in Latin America, Asia, Africa, and the Middle East are derived from three sources. World Fertility Surveys are sponsored by the Office of Population within the United States Agency for In-ternational Development (USAID), the United Na-tions Fund for Population Activities, and the United Kingdom Office of Development Assistance (Light-bourne, Singh, & Green, 1982). The World Health Organization began ongoing surveys on infant feeding in the mid-1970s. Its Global Data Bank on Breast-Feeding pools information garnered from well-designed nutrition and breastfeeding surveys around the world; on the basis of these data, breast-feeding practices are periodically summarized. The most recent summary appeared in 2000 (WHO, 2000). Finally, demographic and health surveys were initiated in 1984; these ongoing surveys are sponsored jointly by USAID and governments of host countries in which the surveys are made.
Other Evidence
Until the last several decades, breastfeeding was the unremarkable norm. Thus what we “know” about
breastfeeding from much earlier times often must be inferred from evidence of other methods of feeding infants. Most historical material available in English-language literature derives from a rather limited ge-ographic area: Western Europe, Asia Minor, the Middle East, and North Africa. Written materials, which include verses, legal statutes, religious tracts, personal correspondence, inscriptions, and medical literature, extend back to before 2000BC.
Some of the earliest existing medical literature deals at least in passing with infant feeding. An Egyptian medical encyclopedia, the Papyrus Ebers (c. 1500 BC), contains recommendations for
increas-ing a mother’s milk supply (Fildes, 1986). The first writings to discuss infant feeding in detail are those of the physician Soranus, who practiced in Rome aroundAD100; his views were widely repeated by
other writers until the mid-1700s. It is not immedi-ately apparent to what degree these early exhorta-tions either reflected or influenced actual practices. Many writings before AD 1800 deal primarily with
wet nurses or how to hand-feed infants.
Archeological evidence provides some informa-tion about infant feeding prior to 2000BC. Some of
the earliest artifacts are Middle Eastern pottery fig-urines that depict lactating goddesses, such as Ishtar of Babylon and Isis of Egypt. The abundance of this evidence suggests that lactation was held in high re-gard (Fildes, 1986). Such artifacts first appear in sites about 3000 BC, when pottery making first became
widespread in that region. Information about infant feeding may also be derived from paintings, inscrip-tions, and infant feeding implements.
Modern ethnography has a place of special im-portance. By documenting the infant feeding prac-tices of present-day nontechnological hunter-gath-erer, herding, and farming societies, ethnographers expand our knowledge of the range of normal breast-feeding practices. At the same time, they provide a richer appreciation of cultural practices that enhance the prevalence of breastfeeding. Such studies are also our best window into breastfeeding practices that may be the biological norm forHomo sapiens sapiens.
Tides in Breastfeeding Practice 5
FIGURE 1–1. The antiquity of lactation. The bottom line shows the approximate times of first appearance of lactating precursors of modern humans and of reg-ular use of nonhuman animal milk by humans.
The Biological Norm in Infant Feeding
Early Human Evolution
The class Mammalia is characterized principally by the presence of breasts (mammae), which secrete and release a fluid that for a time is the sole nour-ishment of the young. This manner of sustaining newborns is extremely ancient; it dates back to the late Mesozoic era, some 100 million years ago. (See Figure 1–1.) Hominid precursors first appeared about 4 million years ago; the genus Homohas ex-isted for about 2 million years. The currently dom-inant human species, Homo sapiens sapiens, has existed for perhaps 40,000 years. Information about breastfeeding practices among our earliest ances-tors is uncertain, although other information about Paleolithic societies that existed 10,000 or more years ago sheds light on this subject.
Early Breastfeeding Practices
Diets reconstructed by archeological methods re-veal that the Late Paleolithic era, roughly 40,000 to
10,000 years ago, was populated by pre-agricultural peoples who ate a wide variety of fruits, nuts, veg-etables, meat (commonly small game), fish, and shellfish. This diet closely resembles that of twenti-eth-century hunter-gatherer societies. Therefore, the infant-feeding practices of societies today may reflect breastfeeding practices of much earlier (pre-historic) times. Consider the breastfeeding practices of the ¡Kung of the Kalahari Desert in southern Africa (Konner & Worthman, 1980) as well as hunter-gatherer societies of Papua New Guinea and elsewhere (Short, 1984). Among these people, breastfeeding of young infants is frequent (averag-ing four feeds per hour) and short (about 2 minutes per feed). It is equally distributed over a 24-hour period and continues, tapering off gradually, for two to six years. These breastfeeding patterns are considered a direct inheritance of practices that pre-vailed at the end of a long, and dietetically stable, evolutionary period that ended about 10,000 BC.
This assumption is supported by observations of the human’s closest primate relative, the chimpanzee, which secretes a milk quite similar to that of hu-mans, suckles several times per hour, and sleeps with and nurses its young at night (Short, 1984).
The Replacement of Maternal
Breastfeeding
Wet-Nursing
Wet-nursing may not have been the earliest alterna-tive to maternal breastfeeding, but it was the only one likely to enable the infant to survive. Wet-nurs-ing is common, although not universal, in tradi-tional societies of today and (by inference) among ancient human societies. An already-lactating woman may have been the most obvious choice for a wet nurse, but women who stimulate lactation without a recent pregnancy have been described in many traditional societies (Slome, 1976; Wiesch-hoff, 1940).
Wet-nursing for hire is mentioned in some of the oldest surviving texts, which implies that the practice was well established even in ancient times. The Babylonian Code of Hammurabi (c. 1700 BC)
6 Historical and Work Perspectives
for the foundling Moses; the fact that the “wet nurse” was Moses’s own mother is incidental. The epic poems of Homer, written down around 900
BC, contain references to wet nurses. A treatise on
pediatric care in India, written during the second centuryAD, contains instructions on how to qualify
a wet nurse when the mother could not provide milk. The Koran, written about AD 500, also
per-mits parents to “give your children out to nurse.” Although the history of wet-nursing has contin-ued virtually unbroken from the earliest times to the present, the popularity of the practice among the elite classes who used it most has waxed and waned. In England during the 1600s and 1700s and elsewhere in Europe, the middle classes began to employ wet nurses. The use of less attentive nurses and the sending of infants greater distances from home diminished maternal supervision of either nurse or infant. Often infants were not seen by their parents from the time they were given to the nurse until they were returned home after weaning (pro-viding they lived). However, by the latter part of the 1700s wet nursing was on the decline in North America and England (except in foundling hospi-tals), owing to increased public concern regarding the moral character of wet nurses and the quality of the care they provided. In France, government offi-cials and physicians led a campaign against wet nursing. Some women recalling this period of his-tory proudly reported that they nursed their babies themselves (Yalom, 1997). Throughout this long pe-riod, wet nurses were used sometimes because of maternal debility but more often because of the so-cial expectations of the class of women who could afford to hire a wet nurse in order to free them for obligations incumbent upon highborn ladies. Thus the use of wet nurses by social elites foreshadows the demographic pattern later seen in the use of manufactured baby milks.
Hand-Fed Foods
The Agricultural Revolution.
The idea that an-imal milks are suitable foods for human infants is reflected in such myths as that of Romulus and Remus, the mythical founders of Rome, who are usually depicted as being suckled by a wolf. Sur-prisingly, the currently most popular hand-fed in-fant foods––animal milks and cereals––did notbecome part of the human diet until well along in human history. Cereal grains first appeared only about 10,000 years ago, and animal milks some-what later (McCracken, 1971). The widespread adoption of these foods was made possible by the development of agriculture and (later) animal hus-bandry. Perhaps because of the availability of new weaning foods, periods of lactation that normally lasted three to six years were shortened to about two years in farming and herding societies (Schae-fer, 1986).
Gruels.
In much of the world, the soft foods added most commonly to the infant diet have been gruels containing a liquid, a cereal, and other sub-stances that added variety or nutritional value. The cereal might be rice, wheat, or corn. It might be boiled and mashed; ground and boiled; or, as in the case of bread crumbs, ground, baked, crushed, and heated. The liquid might be animal milk, meat broth, or water. Eggs or butter might also be added. If grains are not commonly eaten, similar soft foods for infants are based on starchy plants such as taro, cassava, or plantain.Animal Milks.
Animal milks are a relatively re-cent addition to the human diet; this is implied ge-netically, because children beyond weaning age commonly do not produce lactase, an enzyme needed to digest the milk sugar lactose. In cultures that traditionally do not use animal milks, such as those in Mexico or Bangladesh or Thailand, some children may be lactose-intolerant before 1 year of age; in those cultures that use animal milks abun-dantly, the onset of lactose intolerance occurs con-siderably later––after age 10––in Finland (Simoons, 1980). Adult lactose tolerance is common only in cultures in which animal milks have traditionally been an important part of the diet, such as those of northern Europe and western Asia (McCracken, 1971).Tides in Breastfeeding Practice 7
infant feeding, a small spouted bowl found in an in-fant’s grave in France, is dated c. 2000–1500 bc (La-caille, 1950). Small spouted or football-shaped bowls have been found in infant burial sites in Ger-many (c. 900 bc) and in the Sudan in North Africa (c. 400 bc) (Lacaille, 1950). These utensils suggest that hand-feeding of infants has been attempted for more than three millennia. (See Figure 1–2.)
Timing of the Introduction of
Hand-Feeding
What archeological evidence cannot tell us is why or how much these infants were hand-fed. Neonates may temporarily be offered certain foods as prelacteal feeds; young infants may be offered oc-casional tastes of other foods, and they will be of-fered increasing amounts of soft foods as they make the transition to the adult diet (mixed feeds). Fi-nally, infants may be reared from birth on other foods (artificial feeding).
Prelacteal Feeds.
Many of the world’s infants, even those who later will be fully breastfed, receive other foods as newborns. Of 120 traditional soci-eties (and, by inference, in many ancient preliterate societies) whose neonatal feeding practices have been described, 50 delay the initial breastfeeding more than two days, and some 50 more delay it one to two days. The stated reason is to avoid the feed-ing of colostrum, which is described as befeed-ing dirty, contaminated, bad, bitter, constipating, insufficient, or stale (Morse, Jehle, & Gamble, 1990).Early medical writers in the eastern Mediter-ranean region (Greece, Rome, Asia Minor, and Arabia) and later in Europe––from Soranus through those of the 1600s––also discouraged the use of colostrum for feeding. These writers recommended avoiding breastfeeding for periods as short as one day (Avicenna, c. AD1000) to as long as three weeks
(Soranus, c. AD 100). Commonly, to promote the
passage of meconium, the newborn was first given a “cleansing” food such as honey, sweet oils (such as almond), or sweetened water or wine.
In Europe, the fear of feeding an infant colostrum may have contributed to the undermin-ing of maternal breastfeedundermin-ing, at least among the upper classes, and spread wet-nursing (Deruisseau, 1940). A similar charge has been leveled at the prelacteal bottle feeds commonly given in Western (or Western-style) hospital nurseries; many studies show that early bottle-feeds undermine breastfeed-ing and increase the mother’s use of manufactured baby milk. One can only wonder if Western hospi-tal practices, which include delayed first breastfeed-ing and prelacteal feeds of water or artificial baby milk, are technological vestiges of this widespread traditional “taboo.”
Not all published work supports the idea that prelacteal feeds and a delay in initiating breastfeed-ing reduce the likelihood of continued lactation (see Chapter 24). Some authors believe that ensuing breastfeeding is associated with the maternal per-ception that prelacteal feeds are appropriate. They hold that a particular set of culturally approved maternal behaviors follows the commencement of breastfeeding: nearly constant contact with or proximity to the infant; breastfeeding ad lib day and night; and no further use of feeding bottles (Nga & Weissner, 1986; Woolridge, Greasley, & Silpisornkosol, 1985).
Mixed Feeds.
On the basis of current practices of many traditional societies, early mixed feedings may be the most common infant-feeding regimen (Dimond & Ashworth, 1987; Kusin, Kardjati, & van Steenbergen 1985; Latham et al., 1986).Mixed feeding is widely practiced, even during the time when breastmilk forms the foundation of the infant diet. In many regions, such as Africa and Latin America, breastfeeding continues into the sec-ond or third year of life. In non-Western cultures, FIGURE 1–2. An English Staffordshire Spode nursing
8 Historical and Work Perspectives
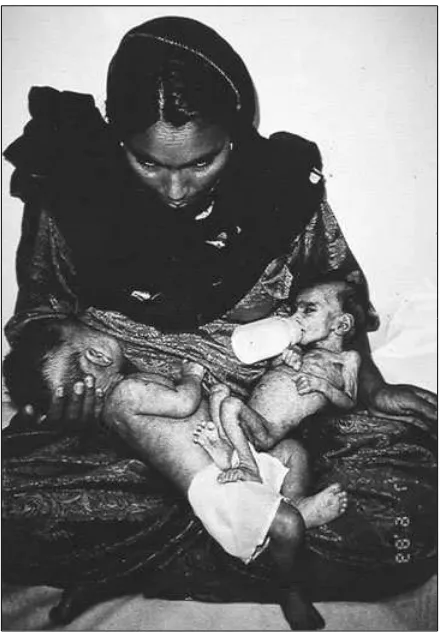
FIGURE 1–3. UNICEF photograph of thriving breast-fed twin and his dying bottle-breast-fed sister. (Courtesy of Children’s Hospital, Islamabad, Pakistan.)
hand-fed foods include tea infusions, mashed fruits, and a variety of starchy gruels or pastes. Where the use of a particular food dominates a culture (e.g., rice in many parts of Asia), that food is usually the principal family food fed to an infant ( Jelliffe, 1962). In some (mostly non-Western) cultures, such foods are offered to weaning infants in such a way that they supplement, rather than replace, breastmilk (Greiner, 1996; Whitehead, 1985) and thus do not appreciably hasten complete cessation of breast-feeding. The use of feeding bottles, however, can shorten the weaning interval, the period between full sustenance by breastmilk and full sustenance by family foods (Winikoff & Laukaran, 1989).
Hand-Feeding from Birth.
In a few regions of northern Europe (e.g., Switzerland, Finland, and Iceland) a cool, dry climate and a tradition of dairy farming permitted the survival of at least some in-fants who were fed cow milk nearly from birth. From at least the 1400s in Switzerland and Finland, breastfeeding was actively discouraged (Fildes, 1986). However, even in climatically optimal areas, hand-feeding was hazardous. In Iceland infants were hand-fed during the 1600s and 1700 despite disastrous results; married women bore as many as 30 infants because so few survived (Hastrup, 1992). In France, some foundlings and infants with syphilis were fed directly from goats; this practice was first described in writings in the 1500s, and it persisted until the early 1800s (Wickes, 1953a). Of necessity, foundling hospitals of the 1700s and 1800s in Europe and the United States hand-fed in-fants but with appalling mortality rates: up to 100 percent died. (See Figure 1–3.) However, by the mid-1900s in industrialized countries, hand-feeding from birth had become the norm and hand-fed in-fants survived and grew. Why did that happen?Technological Innovations in Infant
Feeding
The Social Context
During the late 1800s and the early 1900s, high in-fant mortality, even among inin-fants cared for at home, was a major public concern. Physicians and parents recognized that poorly nourished children were more susceptible to illness. Between 1910 and
Tides in Breastfeeding Practice 9
As women’s aspirations for community service and commercial involvement were rising, Victorian beliefs about modesty discouraged breastfeeding in public. Advertising, which promoted bodily cleanli-ness, may have led to associating breastmilk with body fluids that were unclean or noxious, a notion that persists to this day, at least in North America (Morse, 1989). Advances in the prevention of dis-ease, largely through public health measures re-lated to sanitation, extended an expanding faith in “modern science” in general to “modern medicine” in particular. Women’s magazines developed a wide audience of readers interested in female accom-plishments outside the home, in modern attitudes, and in technological innovations; these same maga-zines reinforced concerns about infant health. An 1880 issue of the Ladies’ Home Journalcontained this statement(Apple, 1986):
If fed from your breast, be sure that the quantity and
quality supply his demands. If you are weak or worn
out, your milk cannot contain the nourishment a
babe needs.
The Technological Context
Between about 1860 and 1910, scientific advances and technological innovations created many new options in infant feeding that appeared to enhance infant survival. The upright feeding bottle and rub-ber nipple, each of which could be cleaned thor-oughly, made artificial feeding easier and safer. New foods to be used with this equipment ap-peared. Large-scale dairy farming produced abun-dant supplies of cow milk, which was marketed first as canned evaporated milk and later in condensed (i.e., highly sweetened to retard spoilage) or dried forms.
This technological ferment, fueled both by the need for improved infant health care and by a pop-ular belief in the ability of science and technology to provide answers, attracted analytical chemists. Around 1850 chemists had begun to turn their at-tention to food products. Early investigations (now viewed as rudimentary) into the composition of human and cow milk convinced them that “the combined efforts of the cow and the ingenuity of man” could construct a food the equal of human
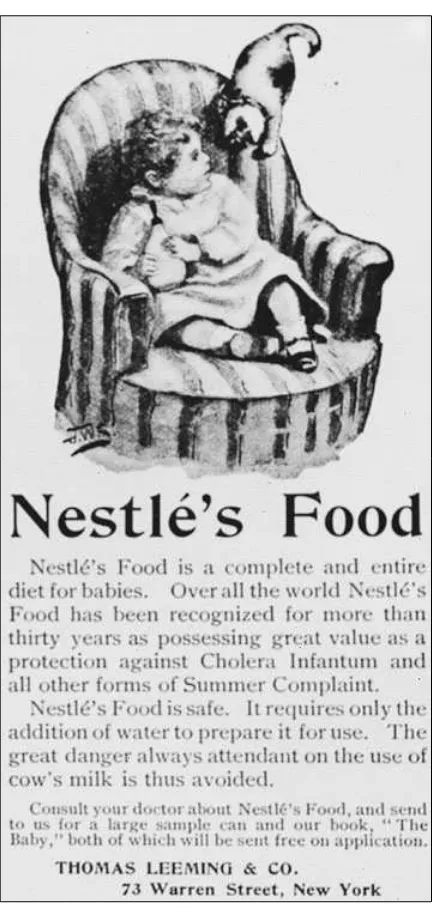
milk (Gerrard, 1974). Patented foods, such as Liebig’s Food and Nestle’s Milk Food, were first marketed in Europe and the United States in the 1860s. The Nestle’s product was a mixture of flour, cow milk, and sugar that was to be dissolved in milk or water before feeding. Milk modifiers, such as Mellin’s Food, and milk foods, such as Horlick’s Malted Milk, were popular in the United States by the 1880s.
Extravagant claims for these foods (Liebig’s Food was called “the most perfect substitute for mother’s milk”) were combined with artful adver-tising that played on fears for the health of the in-fant and faith in modern science (Apple, 1986). (See Figure 1–4.) A hundred years later we see these ad-vertising themes played again and again.
In the 1890s, physician Thomas Rotch devel-oped a complex system of modifying cow milk so that it more closely resembled human milk. Rotch observed that the composition of human milk varies, as do digestive capacities in infants. He devised mathematical formulas to denote the proportions of fat, sugar, and protein in cow milk that some infants required at a particular age (Rotch, 1907). The result was an exceedingly com-plex system of feeding that required constant in-tervention by the physician, who often changed the “formula” weekly. Supervising infant feeding then became a principal focus of the newly emerg-ing specialty of pediatrics.
Commercial advertising promoted the use of manufactured infant milks to both mothers and physicians. The basic themes––a mother’s con-cern for her infant’s health, the perfection of the manufactured product, and the difficulty of breastfeeding––have persisted over the years (Apple, 1986).