The Nursing and Midwifery Content Audit Tool (NMCAT): a short
nursing documentation audit tool
MAREE JOHNSONR N , B A p p S c i , M A p p S c i , P h D1,2, DIANA JEFFERIESR N , B A ( H o n s ) , P h D ( U S y D )3and RACHEL LANGDON B A p p S c i , B A ( H o n s )4
1Director, Centre for Applied Nursing Research, (a joint venture of the SSWAHS and UWS),2Professor of Nursing,
School of Nursing & Midwifery, University of Western Sydney, Sydney,3Nurse Educator-Clinical Research, Centre for Applied Nursing Research, Liverpool and4Research Assistant, Centre for Applied Nursing Research, Liverpool, NSW, Australia
Introduction
Although nursing documentation is a valuable tool for communicating patient information to nurses and other health professionals, it is often difficult for busy
clini-cians to see the benefits (Gropper 1988). Quality doc-umentation details patientsÕproblems, nursesÕactions or interventions and patient outcomes and is Ôan essential
component of professional practiceÕ (Wong 2009,
p. E1). The role of the nurse in assisting the recovery of
Correspondence
Diana Jefferies
Centre for Applied Nursing Research
Locked Bag 7103 Liverpool, 1871 NSW Australia
E-mail:
Diana.jefferies@sswahs.nsw.gov.au
J O H N S O N M . , J E F F E R I E S D . & L A N G D O N R .(2010)Journal of Nursing Management18,832– 845
The Nursing and Midwifery Content Audit Tool (NMCAT): a short nursing documentation audit tool
Background The Nursing and Midwifery Content Audit Tool (NMCAT) was developed to monitor the quality of nursing documentation.
Methods A health care record audit was conducted on 200 records. Using a time-sampling approach, recent nursing documentation was examined. Inter-rater reliability was determined at 85% agreement between two raters.
Results The NMCAT criteria relating to the recording of the patientsÕhealth status, use of objective information and logical presentation were met to a high level. The patientsÕresponse to treatment or nursing interventions including medications requires attention. The recording of events immediately after they have occurred was limited. The structure of the sentences and language used, restricted the read-ability of the documentation. The widespread use of local abbreviations, often connected together to form the text, was problematic.
Conclusions The present study provides new audit solutions based on time-sampling approaches and focused evidence-based criteria. The use of language support software and writing coaches to improve the presentation of nursing doc-umentation is recommended.
Implications for Nursing Management The NMCAT is a time-efficient tool avail-able to managers for monitoring the quality of nursing documentation, either at a unit level or across health facilities to demonstrate compliance with quality standards.
Keywords: audit, communication, documentation, evidenced-based policy, innovation
Accepted for publication: 26 June 2010
the patient can be made explicit through nursing notes (Karlsen 2007) and can be examined through research (McCormack 2003). From the perspective of other health professionals, the utility of nursing documenta-tion is often diminished by the over abundance of
Ôroutine notesÕ as noted by general practitioners
(Tornvall & Wilhelmsson 2008). Communication, whether written or oral, has been identified as con-tributing to approximately 50% of all adverse events
for patients (Middletonet al.2005). With the looming
introduction of electronic health care records, nurses are well aware of the need to improve their written com-munication of the care they deliver. Indeed, one author suggests that the assessment of the current state of nursing documentation is an important initial step in the conversion to electronic documentation (Dykes 2006).
In addition, one Australian study (Considine et al.
2006) demonstrated that the introduction of standards has successfully led to an improvement in nursing doc-umentation. This present study aims to develop and test a short audit tool to evaluate the implementation of documentation standards and for continuous monitor-ing of nursesÕwritten documentation of their care.
This study examined the development and testing of the Nursing and Midwifery Content Audit Tool (NMCAT) specifically designed to reflect the standards of quality documentation derived from a systematic review of the literature undertaken by the authors (Jefferies et al. 2010). In addition, initial pre-imple-mentation data on nursing docupre-imple-mentation, using the NMCAT tool, are presented.
Developing the standards for quality nursing
documentation
A Health Care Record has been defined asÔa documented
account of a personÕs health, illness or treatment in a
hard copy or electronic formÕ(NSW Health 2008, p. 3).
A definition for nursing and midwifery documenta-tion was developed as part of the process of standard development and is used in this study:
ÔNursing and midwifery documentation is a
pro-cess in which the patientÕs experience from
admission to discharge is recorded in a manner which enables all clinical staff involved in the patientÕs care to detect changes in the patientÕs condition and the patientÕs response to treatment and care deliveryÕ.
This definition emphasized the role of nursing docu-mentation in keeping all members of the health care
team informed of the patientÕs condition, their care and
their response to that care (Gebruet al. 2007) and was
the basis of the Minimum Standards on Nursing Doc-umentation.
Two of the authors initially undertook a systematic review of existing literature to design the seven stan-dards of quality nursing documentation. This entailed a search of published papers on CINAHL 1982 to April Week 3 2008, and MEDLINE 1996 to April 2008 and limited to the English language, using the following terms: attitude, audit, care, culture, documentation, guideline, health, in service, legal, liability, medical, nurses, nursing, organizational, patient, personnel, planning, practice, quality, records, research and
training (Jefferies et al. 2010). Some 71 articles were
identified and quality scoring and thematic analysis was undertaken. Using a meta-synthesis approach, seven key themes emerged from the process and formed the standards. The seven minimum standards were that nursing documentation should: be patient centred, must contain the actual work of nurses including education and psychosocial support, be written to reflect the objective clinical judgement of the nurse, be presented in a logical and sequential manner, be written contem-poraneously (or immediately after events occur), record variances in care within and beyond the health care record and fulfill legal requirements (see Table 1).
The standards were broad in nature, and no attempt was made to define the content of nursing notes. Many diverse formats exist such as nursing diagnoses, nursing intervention classification and nursing outcome classi-fication systems (von Krogh & Naden 2008), a systems approach (Andersonet al.2009), and activities of daily
living (Rajkovic et al. 2009), and this issue of format
has been addressed within the varying clinical units and was not considered within these standards. Engagement of clinicians and consumers was a critical part of the process of standard development.
Quality Improvement Program (EQuIP) (ACHS 2009) which is conducted by independent assessors.
This approach is consistent with the process defined
by Andersonet al.(2009) where a Best Practice Council
was formed and followed theÔSt. LukeÕs Evidence Based
Practice ModelÕ to collect and appraise the evidence,
integrate the evidence with clinical expertise, patient preferences and values and evaluate the practice change
(Andersonet al.2009, p. 85). However, Andersonet al.
(2009) raised concerns about nurses conducting regular audits which were so time consuming that there was little time left for implementing strategies to address deficiencies.
Tools to measure the quality of nursing notes
Audit tools have often been used as part of the general health service accreditation process. However, a review of the literature did highlight that several tools had been developed by nurses for this purpose. The Phaneuf Nursing Audit is one of the earliest tools to focus on reporting and recording (Phaneuf 1976, Manfredi 1986). The Phaeuf is a 50-item instrument that measures pro-fessional nursing. Documentation has five items within the tool and is rated as yes, no, uncertain or does not apply (Manfredi 1986). Manfredi (1986) demonstrated that the Phaneuf tool was a comprehensive, valid and
reliable tool with some limitations. In 1997, Corben
1997, critiqued ManfrediÕs work and concluded that
Phaneuf was the only existing tool, but was unsuitable for the British health system and had varying levels of validity and reliability in the subscales. Corben developed an-other audit tool known as the Buckinghamshire nursing record audit tool. This tool was derived from the criteria within the UKCC Standards on Records and Record Keeping (1992) and included sections on the utilization of the nursing process, questions on individualized care and patient involvement, teaching and health promotion and communication with other disciplines. This audit required examination of a complete set of documen-tation from admission to discharge and relevant charts. A practitioner and facilitator are recommended to undertake the audit thus supporting an educational experience. Corben set a 60% or lower level of achieve-ment as an unsafe result. In conclusion, Corben (1997) noted that this audit tool was the only one available for British documentation.
Another aspect of chart auditing raised by Wong is timing of the audit. Wong (2009) noted that most chart audits are done retrospectively which does not allow the auditors to check on the care that is given and Wong recommends that the chart audit be done 1 day after the
care is given. WongÕs (2009) audit tool covered vital
signs, admission forms, discharge planning, system
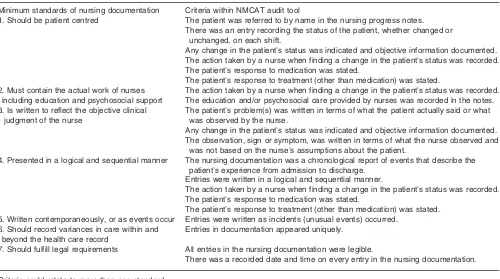
Table 1
Relationship between standards and criteria used in the Nursing and Midwifery Content Audit Tool (NMCAT)
Minimum standards of nursing documentation Criteria within NMCAT audit tool
1. Should be patient centred The patient was referred to by name in the nursing progress notes. There was an entry recording the status of the patient, whether changed or
unchanged, on each shift.
Any change in the patientÕs status was indicated and objective information documented. The action taken by a nurse when finding a change in the patientÕs status was recorded. The patientÕs response to medication was stated.
The patientÕs response to treatment (other than medication) was stated. 2. Must contain the actual work of nurses
including education and psychosocial support
The action taken by a nurse when finding a change in the patientÕs status was recorded. The education and/or psychosocial care provided by nurses was recorded in the notes. 3. Is written to reflect the objective clinical
judgment of the nurse
The patientÕs problem(s) was written in terms of what the patient actually said or what was observed by the nurse.
Any change in the patientÕs status was indicated and objective information documented. The observation, sign or symptom, was written in terms of what the nurse observed and
was not based on the nurseÕs assumptions about the patient.
4. Presented in a logical and sequential manner The nursing documentation was a chronological report of events that describe the patientÕs experience from admission to discharge.
Entries were written in a logical and sequential manner.
The action taken by a nurse when finding a change in the patientÕs status was recorded. The patientÕs response to medication was stated.
The patientÕs response to treatment (other than medication) was stated. 5. Written contemporaneously, or as events occur Entries were written as incidents (unusual events) occurred.
6. Should record variances in care within and beyond the health care record
Entries in documentation appeared uniquely.
7. Should fulfill legal requirements All entries in the nursing documentation were legible.
There was a recorded date and time on every entry in the nursing documentation.
assess charting, progress charting, intravenous fluids and labelling, fluid balance and other risk management charts such as fall prevention, deep venous thrombosis prophylaxis and skin assessment. The audit was con-ducted by a nurse educator. The NMCAT is a concur-rent audit, and records are accessed on the ward unit while actively in use.
Another aspect is the use of technology to conduct the audit. In one study in the emergency department, an automated audit system was introduced to scan through documentation and notify nurses of areas omitted
(Wainwright et al. 2008). The Nurse Documentation
Improvement Tool (END-IT) used peer mentoring to
enhance the Ôaccountability in documentationÕ
(Wain-wrightet al.2008, p. 16).
Another approach has been to review the text of many records and glean the essence of the process of nursing notes as undertaken by Karlsen (2007) within a Norwegian psychiatric hospital. Karlsen found evidence of private nursing plans (written in a way that has limited transference of information), hidden nursing plans (recordings of where the patient is and what he/ she is doing) and local diagnostic systems using local language. This process of reading and understanding the text is valuable. The authors have included an opportunity to collect verbatim nursing notes from nurses and midwives within the NMCAT.
Likert-scale approaches have also been used to determine improvements in the quality of nursing
doc-umentation (Muller-Staub et al. 2007). These authors
used a 29-item four-point likert scale tool known as the Quality of Nursing Diagnosis, Interventions and Out-comes (Q-DIO) to detect changes in the quality of documentation after an education intervention. Using a pre-post test design, Muller-Staub et al. (2007) identi-fied improvements after educational interventions. The criteria within the NMCAT did not lend themselves to a likert-scale approach, although we acknowledge the usefulness of a continuous data set of this kind.
Design aspects
Audit tools should provide data in a timely manner, therefore allowing clinicians and managers to imple-ment changes in response to the findings (Anderson
et al.2009). The tool proposed here needed to be short and focused on the standards developed. The audit needed to be conducted within 5–10 minutes in most cases. The ideal was the nurse managers or nursing peers could undertake an audit of 20 records every 3–6 months (within 1–2 hours), generate the findings to share with staff and put in place strategies to address
areas of concern and then reaudit at a later time. Tools to measure nursing documentation often focus on legal aspects and not much more, while this audit tool also focuses on content.
Several key aspects included in the NMCAT were: a time sampling approach, examination of the content as well as the legal requirements of documentation and capture of the text or actual language used by nurses to demonstrate the areas of strength and weakness. The NMCAT criteria were designed to relate to the standards for quality nursing documentation (Jefferieset al.2010). The final criteria included in the NMCAT tool are presented in Table 1 and in Appendix I. As can be seen from Table 1, the NMCAT criteria could have been re-lated to more than one standard. Therefore, the aim of the present study was to develop and test the NMCAT in a large metropolitan health service. To pilot test the utility of the tool and reporting mechanism to Directors of Nursing & Midwifery was the focus, although details of the inter-rater reliability were also examined. This study also provided initial pre-implementation data for the introduction of the Minimum Standards on Nursing Documentation project implementation.
Methods
A mixed methods design was used in this study including a concurrent health record audit examining the criteria for nursing documentation (derived from the standards) and use of text from notes as examples of the criteria reflecting the qualitative aspects of the study.
Sample and setting
A total of 200 records from 10 metropolitan hospitals formed the data. Twenty records were randomly selected using random number tables from wards identified from hospitals participating in the present study. Data were pooled to develop benchmarks for the health service, while individual hospitals received reports on their 20 records examined, with a copy of the NMCAT and explanatory notes (Appendix I). The inter-rater reliability testing examined the agreement or disagreement between two raters.
NMCAT tool
demonstrating where areas of strengths and weakness occur. The survey tool was developed within Survey
Monkey, an internet-based data entry and reporting
system. The response categories ranged from absent, present, always present and not rated. Explanatory notes for each of the response categories for the criteria are presented in Appendix I.
The NMCAT uses a time sampling approach and allows for capture of records covering five major time periods: admission to 24 hours, between 25 and 48 hours after admission, 49 and 72 hours after admission, 73 and 96 hours after admission, prior to discharge and other cases of extended periods. The auditor was required to locate three nursing entries (or a 24-hours time period). The large sample size ensured a distribution across the usual time periods for inpatients.
Procedure
The Director of Nursing and Midwifery Services (DON&MS) from each hospital participating in the study was requested to nominate a ward for the docu-mentation audit. One of the authors collected the data and was generally well supported by staff within the unit. Data entry was done directly into the dedicated Survey Monkey URL where access to the internet was available. In most cases, these data were placed on a hard copy form of the survey and later entered into Survey Monkey URL. Although the records were examined by one data col-lector, inter-rater reliability testing was also undertaken. Data were analysed within the health service nursing research centre and results were then sent directly to the ward areas and the DON&MS. Aggregated data from all services were presented in a summary report with recommendations to the Area DON&MS and all DON&MS and this provided the benchmarks for pre-implementation of the standards.
Ethical approval was sought and obtained from two Health and Research Ethics Committees covering all the hospitals participating in the study.
Results
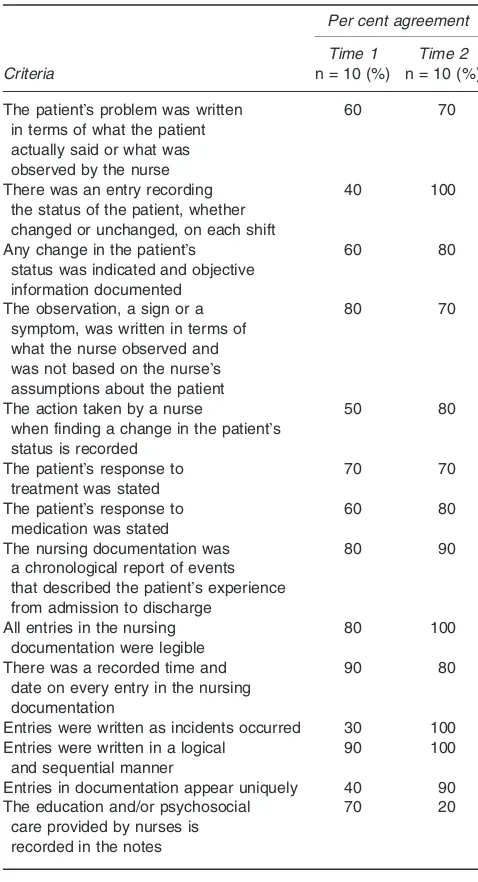
Inter-rater reliability was confirmed on Time 2 with most criteria achieving at least 70% agreement between the raters (see Table 2). The last criterion relating to psychosocial care and education was further defined to reflect education that would be expected to be received relating to the condition. Nonetheless, the overall agreement was 81% or 85% excluding the education criterion. Modifications to the criteria were undertaken after Time 1 reliability results were received.
These changes included adding more specific wording and removing response categories that did not reflect the experience e.g. it was not felt that having a present and always present category for education was reasonable so these categories were collapsed into present only.
The time sampling approach was appropriate as can be seen from the distribution of records across the expected length of stay of patients within the health facilities (see Table 3). The mean time for completion of an audit was 6.64 minutes (4.25 minutes SD).
Table 2
The patientÕs problem was written in terms of what the patient actually said or what was observed by the nurse
60 70
There was an entry recording the status of the patient, whether changed or unchanged, on each shift
40 100
Any change in the patientÕs status was indicated and objective information documented
60 80
The observation, a sign or a symptom, was written in terms of what the nurse observed and was not based on the nurseÕs assumptions about the patient
80 70
The action taken by a nurse
when finding a change in the patientÕs status is recorded
50 80
The patientÕs response to treatment was stated
70 70
The patientÕs response to medication was stated
60 80
The nursing documentation was a chronological report of events that described the patientÕs experience from admission to discharge
80 90
All entries in the nursing documentation were legible
80 100
There was a recorded time and date on every entry in the nursing documentation
90 80
Entries were written as incidents occurred 30 100 Entries were written in a logical
and sequential manner
90 100
Entries in documentation appear uniquely 40 90 The education and/or psychosocial
care provided by nurses is recorded in the notes
70 20
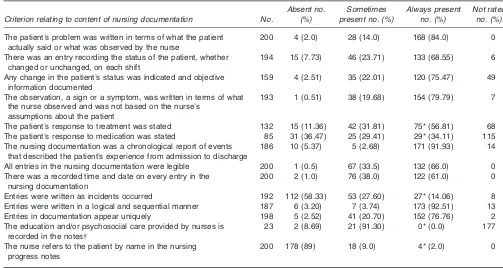
Achieving standards and meeting criteria relating
to the content of nursing notes
Recording the patientÕs status whether changed or
un-changed at every shift was found in most records (92% present or always present) (see Table 4). Similarly, the use of objective information when reporting changes was apparent (what the patient said or objective signs). Patient responses to treatment was found in most records, although the patient responses to medication was not as extensive (63.5% present and always pres-ent). The record did represent a chronological record of
the patientÕs hospital stay, although the presence of
contemporaneously reporting (or the recording of events immediately after they occur) was not wide-spread in the records (41.66% present and always
present). Documentation by variance was demonstrated with most records reflecting abnormal rather than normal vital signs or other observations. The criterion requiring that the patientÕs name be used is a new cri-terion for staff in hospitals participating in the present study and was accordingly infrequently recorded (11%). The purpose of this criterion is to personalize the records for the patient and nurse and allow the subject of the documentation to be the patient rather than a list of nursing tasks disconnected from the patient which was frequently found.
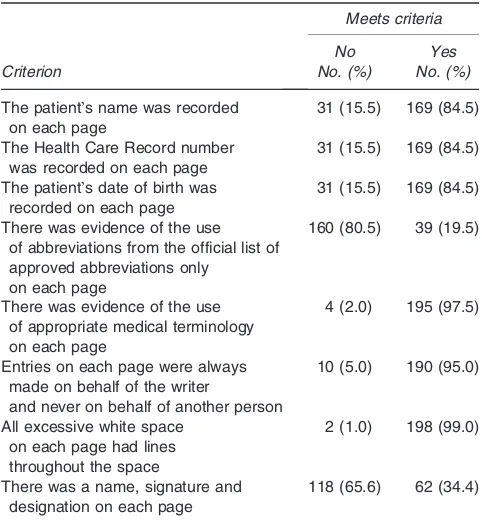
Legal requirements of nursing documentation
The achievement of legal requirements has been the focus of nursing audits in hospitals participating in the present study in the past. Most of these criteria were met to a high level (85% or more) (see Table 5). However, the use of varying abbreviations (81%), many of which were not on the official list for the organization, was a substantial problem.
As the NMCAT also captured text from the record the following examples are presented to highlight when the various criteria within the NMCAT were met or not met and further demonstrate both the Standards and the NMCAT criteria in use.
Table 4
Nursing and Midwifery Content Audit Tool (NMCAT) criteria and achievement of criteria prior to implementation (n= 200)
Criterion relating to content of nursing documentation No.
Absent no. (%)
Sometimes present no. (%)
Always present no. (%)
Not rated no. (%)
The patientÕs problem was written in terms of what the patient actually said or what was observed by the nurse
200 4 (2.0) 28 (14.0) 168 (84.0) 0
There was an entry recording the status of the patient, whether changed or unchanged, on each shift
194 15 (7.73) 46 (23.71) 133 (68.55) 6
Any change in the patientÕs status was indicated and objective information documented
159 4 (2.51) 35 (22.01) 120 (75.47) 49
The observation, a sign or a symptom, was written in terms of what the nurse observed and was not based on the nurseÕs
assumptions about the patient
193 1 (0.51) 38 (19.68) 154 (79.79) 7
The patientÕs response to treatment was stated 132 15 (11.36) 42 (31.81) 75* (56.81) 68 The patientÕs response to medication was stated 85 31 (36.47) 25 (29.41) 29* (34.11) 115 The nursing documentation was a chronological report of events
that described the patientÕs experience from admission to discharge
186 10 (5.37) 5 (2.68) 171 (91.93) 14
All entries in the nursing documentation were legible 200 1 (0.5) 67 (33.5) 132 (66.0) 0 There was a recorded time and date on every entry in the
nursing documentation
200 2 (1.0) 76 (38.0) 122 (61.0) 0
Entries were written as incidents occurred 192 112 (58.33) 53 (27.60) 27* (14.06) 8 Entries were written in a logical and sequential manner 187 6 (3.20) 7 (3.74) 173 (92.51) 13 Entries in documentation appear uniquely 198 5 (2.52) 41 (20.70) 152 (76.76) 2 The education and/or psychosocial care provided by nurses is
recorded in the notes
23 2 (8.69) 21 (91.30) 0* (0.0) 177
The nurse refers to the patient by name in the nursing progress notes
200 178 (89) 18 (9.0) 4* (2.0) 0
*Corben (1997) set a 60% or lower level of achievement as an unsafe result. Criteria were flagged that did not achieve 60% for always present. Note that most criteria did reach 60% or more for present and always present categories.
This criteria has been rewritten to include a statement relating to condition see version 3 of NMCAT (Appendix I).
Table 3
Time period covered in the audit
Time No. (%)
Between 0 and 24 hours of admission 56 (28.0) Between 25 and 48 hours of admission 43 (21.5) Between 49 and 72 hours of admission 44 (22.0) Between 73 and 96 hours of admission 40 (20.0)
Prior to discharge 4 (2.0)
Other 13 (6.5)
Text that reflected a collection of abbreviations, focusing mostly on nursing tasks with little connection to the patient was common:
Independent in ADLs. Mobilizing around ward. Regular IVABX given as charted. Obs monitored and stable. v/b husband. No voiced complaints.
Observed to be resting for short periods, easily rousable. IVF continues via portacath IV A/biotics given Afebrile.
Reporting change in status using objective informa-tion and contemporaneous (as events occurred) recording:
0215 hours obs attended & stable. Nil C/0 chest
pain. 0445 Monitor alarmed HRfl 39 bpm. Pt asleep,
snoring loudly. Pt woken up to attend to obs pt denies
feeling symptoms of same States he was Ôout cold &
sound asleepÕBP now 122/75 HR 66.
The following transcript identifies the patientÕs response to treatment and prn medication and educa-tion is noted:
3/07/09 2250 Patient becoming › confused &
aggressive contacted RMO stat dose of Haloperidol
1.0 mg IMI admin await effect…
2400 (patients name) unsettled at handover. At
moment in bed with O2 prongs reapplied 2L/minutes
obs as charted. Note previous dose of Haloperidol given await effect.
0300 N/R dozing for short periods when awake takes off nasal prongs- same continuously reapplied.
A/Prof XXX requested to put 5 mL betadine around and into SPCin situsite and then replace SPC to size 18 and keep it clamped with a valve. Procedure completed without any problems. Patient felt comfortable.
Educated patient on the reason for keeping IDC-leg bag which needs replacement weekly.
Discussion
A metasynthesis of the literature relating to documen-tation (Jefferies et al. 2010) highlighted key areas for improvement in nursing documentation and shaped seven Minimum Standards on Nursing Documentation and the criteria for a nursing documentation audit tool (SSWAHS 2009). The NMCAT is a short, practical tool that focuses on the content of nursing documen-tation rather than being restricted to only the legal aspects of nursing documentation.
Several aspects of the design were derived from other
tools or other researcherÕs views. Anderson et al.
(2009) proposed that a short tool was needed and the NMCAT requires 6–7 minutes to complete. Time sampling proved to be a useful and practical approach that allowed for this shortened time for completing the audit. Although contemporary approaches such as using an internet survey tool which allows staff to in-put data and receive reports was included, the auditor had difficulty getting access to the internet to input data at the ward level. This aspect may be in question at this point, but the authors believe this will be re-solved with widespread wireless access for nurses at the ward level. Corben (1997) reviewed the entire record of the patient in her work and this approach does have merit if not some difficulties with the time required to
complete the audit. Although Muller-Staub et al.
(2007) examined diagnoses, interventions and out-comes using continuous data, the NMCAT has in-cluded essentially categorical data which explores nursing interventions and their effectiveness, or patient outcomes.
The problems with retrospective chart audits were outlined by Wong (2009) with the proposal that audits should be conducted 1 day after the care is given. The NMCAT, in most cases, was completed using the last 24-hours period recorded and would represent a description of the care delivered within 1 day of the audit. The ability to question staff about the content is an advantage in this approach and would be very effective when audits are conducted by ward nursing staff rather than an external auditor.
Table 5
Criteria relating to legal requirements
Criterion
Meets criteria No
No. (%)
Yes No. (%)
The patientÕs name was recorded on each page
31 (15.5) 169 (84.5)
The Health Care Record number was recorded on each page
31 (15.5) 169 (84.5)
The patientÕs date of birth was recorded on each page
31 (15.5) 169 (84.5)
There was evidence of the use of abbreviations from the official list of approved abbreviations only
on each page
160 (80.5) 39 (19.5)
There was evidence of the use of appropriate medical terminology on each page
4 (2.0) 195 (97.5)
Entries on each page were always made on behalf of the writer
and never on behalf of another person
10 (5.0) 190 (95.0)
All excessive white space on each page had lines throughout the space
2 (1.0) 198 (99.0)
There was a name, signature and designation on each page
The general impression of the text was that nursing documentation was a connected series of short state-ments often involving abbreviations that may or may not be acceptable across the service. Many local abbreviations were in use, which in some cases, were unknown to the auditor and may potentially be mis-understood by casual health staff.
It was evident that there was little sentence structure and the presentation would have been difficult for a consumer or the general public to read and understand. Health care records are reviewed by legal services and consumers. Consumers often request to read health care records, which is supported, if undertaken in the pres-ence of a medical officer.
Karkkainen et al.(2005) suggest that the quality of
nursing documentation reflects the nursesÕview of their documentation. For example, if nurses did not believe that documentation had a useful clinical purpose, nur-ses did not give a full picture of the care given to patients. However, if nurses saw their documentation as an important aid to communication and a guide to care, their documentation gave a fuller picture of the care
given to the patient (Karkkainen et al.2005). Another
aspect of nursing documentation that has come to the
researchersÕ attention anecdotally through discussions
with Directors of Nursing has been the influx of over-seas trained nurses who speak English as a second lan-guage. These nurses may be assisted to give fuller descriptions of patient care if they are able to access descriptions of care through prompts or predictive text. These prompts could potentially be available with the introduction of the electronic medical record. The idea of structuring descriptions of care into codes on the electronic medical record, rather than using free text boxes, to ensure the quality of nursing documentation, has been argued by Moss (2007). This author suggests that these codes would be more easily analysed by all health care professionals than any narrative descrip-tions of care given in free text (Moss 2007).
The content reflected in the text reviewed in this study often described a series of nursing tasks that were unrelated to any identified patient problem or sign or symptom. This has been previously reported by other
authors (Brooks 1998, Pearson 2003, Karkkainenet al.
2005). There was little use of the patientÕs actual name with the patient being frequently referred to in the abbreviated form of ÔptÕ. The authors believed that not
using a patientÕs name was a mechanism that distanced
the nurse from the patient. Using the patientÕs name
required the nurse to personalize their account of the
patientÕs care and encourages nurses to involve the
patient in the nursing documentation. For example, an
objective account of a patientsÕ problem is obtained
using the patientÕs own words to describe the problem: Mr Smith complained of a headache and said that it was Ôblurring his visionÕ. Nurses have traditionally used the word patient (pt) in nursing notes as the patientÕs name appeared at the top of all pages (addressograph label), however, this results in a focus often upon the tasks of nurses disconnected from any patient problem (Jefferies
et al. 2010). These authors are trialing a ward-based writing coach strategy to explore the possibilities of improving written accounts of patient care through coaching.
The nursing documentation audited presented an objective account of the patientÕs experience of their condition and the care they received during their admission. The legal aspects of nursing documentation were particularly strong, demonstrating that clinicians had a good understanding of the importance of ensuring that the patient was identified by their name (label), health care record number and date of birth on every page, and that no entry was made on behalf of another person.
Areas identified for improvement (based on CorbenÕs 60% rule applied to always present category) included: need for a statement in the shift report that identifies the patientÕs status, notation of the patientÕs response to all
treatment including medications, using the patientÕs
name in the script and documenting the education and psychosocial care provided where appropriate. There was limited evidence of nurses recording events when they happened, with the end of shift reporting tradition
remaining prominent. As Jefferies et al. (2010) notes:
ÔDocumenting events as they occur guarantees that
important information about the patientÕs condition
and care is not forgotten if subsequent events take placeÕ (p. 120) Ôit can be difficult to reconstruct events at a later timeÕ(p. 122).
The inclusion of psychosocial care and education is particularly problematic and has been referred to by other authors (Brooks 1998). Psychosocial care is often difficult to put into written language for nurses (Jefferies
et al. 2010) and therefore often results in a limited scope of nursing interventions being reported. Similarly, education delivered to the patient or family is often extensive and details of the education content delivered provides evidence of the role of nurse in patient care. This may result from the situation where the nurse delivers education and support while undertaking a
task. This results in only the task of Ôattending the
woundÕ being reported upon even although much
Neither the NMCAT nor the Minimum Standards on Nursing Documentation prescribed the exact words or language or scope of content to be used in nursing documentation, rather these standards only provide general direction; defining patient problem, nursing interventions and outcomes of care. Various content approaches exist throughout the service – systems approach in critical care, activities of daily living in rehabilitation and aged care and others prefer a prob-lem-based or nursing diagnosis approach. The devel-opment team of the Minimum Standards believed that only broad guidance should be given to professional nurses rather than a prescriptive text (Jefferies et al.
2010). Finally, health care documentation is not only the responsibility of nurses, but rather an important quality issue for all health care professionals including allied health professionals and medical practitioners.
In conclusion, the NMCAT is a short audit tool that uses time sampling methods to capture 24-hours periods of nursing documentation around 1 day after the care is delivered. It has demonstrated face validity and inter-rater reliability (85%) and has been used here prior to implementation of Minimum Standards on Nursing Documentation. The tool is directly related to the Stan-dards. The structure of the nursing scripts examined highlights the need for either language support software or additional training in writing prior to undertaking the transition to electronic format. There is a need for clini-cians, managers and educators to promote the inclusion of education and psychosocial support, provided to the patient, within nursing documentation.
The NMCAT is a useful, reliable and valid tool that clinicians, managers and educators can use to monitor aspects of nursing documentation.
References
Anderson J.J., Mokracek M. & Lindy C.N. (2009) A nursing quality program driven by evidence-based practice. Nursing Clinics of North America44, 83–91.
Australian Council on Healthcare Standards (ACHS) (2009)The Australian Council on Healthcare Standards National Report on Health Services Accreditation Performance 2007–2008. ACHS, Ultimo.
Brooks J.T. (1998) An analysis of nursing documentation as a reflection of actual nurse work.Medsurg Nursing7, 189–198. Considine J., Potter R. & Jenkins J. (2006) Can written nursing practice standards improve documentation of initial assessment of ED patients?Australasian Emergency Nursing Journal9, 11–18. Corben V. (1997) The Buckinghamshire nursing record tool: a unique approach to documentation.Journal of Nursing Man-agement5, 289–293.
Dykes P. (2006) A systematic approach to baseline assessment of nursing documentation and enterprise-wide prioritisation of electronic conversion. Studies in Health Technology and Informatics122, 683–687.
Gebru K., Ahsberg E. & Willman A. (2007) Nursing and medical documentation on patientsÕ cultural background. Journal of Clinical Nursing16, 2056–2065.
Gropper E.I. (1988) Does your charting reflect your worth? Geriatric Nursing9, 99–101.
Jefferies D., Johnson M. & Griffiths R. (2010) A metastudy of the essentials of quality nursing documentation. International Journal of Nursing Practice16, 112–124.
Karkkainen O., Bondas T. & Eriksson K. (2005) Documentation of individual patient care: a qualitative metasynthesis.Nursing Ethics12, 123–132.
Karlsen R. (2007) Improving the nursing documentation: pro-fessional consciousness-raising in a Northern-Norwegian psy-chiatric hospital. Journal of Psychiatric and Mental Health Nursing14, 573–577.
von Krogh G. & Naden D. (2008) Implementation of a docu-mentation model comprising nursing terminologies – theoreti-cal and methodologitheoreti-cal issues.Journal of Nursing Management 16, 275–283.
Manfredi C. (1986) Reliability and validity of the Phaneuf Nursing Audit.Western Journal of Nursing Research8, 168–180. McCormack B. (2003) The meaning of practice development:
evidence from the field.Collegian10, 13–16.
Middleton S., Chapman B., Griffiths R. & Chester R. (2005) Reviewing recommendations of root cause analyses.Australian Health Review31, 288–295.
Moss J. (2007) An analysis of narrative nursing documentation in an other otherwise structured intensive care clinical informa-tion system.AMIA Annual Symposium proceedings543–547. Muller-Staub M., Needham I., Odenbreit M., Lavin M.A. & van
Achterberg T. (2007) Improved quality of nursing documen-tation: results of a nursing diagnoses, interventions, and out-comes implementation study.International Journal of Nursing Terminologies and Classifications18, 5–17.
NSW Health (2008)Principles for Creation, Management Storage and Disposal of Health Care Records, NSW Health, Sydney. Pearson A. (2003) The role of documentation in making nursing
work visible.International Journal of Nursing Practice9, 271– 271.
Phaneuf M. (1976)The Nursing Audit: Self-regulation in Nursing Practice, 2nd edn. Appleton-Century-Crofts, New York. Rajkovic U., Sustersic O. & Rajkovic V. (2009) E-documentation
as a process management tool for nursing care in hospitals. Studies in Health Technology and Informatics146, 291–296. Sydney South West Area Health Service (2009) Minimum
Stan-dards on Nursing Documentation. SSWAHS, Sydney. Tornvall E. & Wilhelmsson S. (2008) Nursing documentation for
communicating and evaluating care.Journal of Clinical Nurs-ing17, 2116–2124.
Wainwright G.A., Stehly C.D. & Wittman-Price R.A. (2008) Emergency nurse documentation improvement tool.Journal of Trauma Nursing15, 16–18.
Appendix I Nursing and Midwifery Content Audit Tool (NMCAT)
1. Ward / Unit Area: ...
2. Time period covered by this record audit:
Admission to =<24 hours
Between >24 hours to <=48 hours after admission
Between >48 hours to <=72 hours after admission
Between >72 hours to <96 hours after admission
Other cases extended periods (describe the situation): ...
...
...
...
...
SECTION B: Nursing Documentation Content
Examine the written text, within the time period selected (only 3 shifts are examined am, pm and night) for this record audit, for any evidence of each of the following criteria and code according to the notes below. Explanatory notes follow.
Absent – Criteria not present in any of the written text
Present – Criteria occasionally present (present on notes from one shift, but not notes from another shift)
Always Present – Criteria always present (present in notes from all shifts) Not Rated – Question not applicable to this record
t o N s y a w l A t n e s e r P t n e s b A
d e t a R t n e s e r P
3. The patient’s problem(s) is written in terms .... ... ... ... of what the patient actually said or what was
observed by the nurse
4. There is an entry recording the status of the ... ... ... ... patient, whether changed or unchanged, on
each shift
5. Any change in the patient’s status is supported ... ... ... by documented objective information
6. Any observation, sign or symptom, is written .. ... ... ... in terms of what the nurse observed and is
not based on the nurse’s assumptions about the patient
7. The action taken by a nurse when finding a .... ... ... ... change in the patient’s status is recorded
8. The patient’s response to treatment (other ... ... ... ... than medication) is stated
9. The patient’s response to medication is ... ... ... ... stated
10. The nursing documentation is a chronological . ... ... ...
... ... report of events that describe the patient’s
experience from admission to discharge
12. There was a recorded and date on every ... ... ... ... nursing entry in the patient’s note
13. Entries were written as incidents occurred ... ... ... ...
14. Entries were written in a logical and ... ... ... ... sequential manner
15. Entries in documentation appear uniquely ... ... ... ...
16. The education and / or psychosocial care ... ... ... provided by nurses is recorded in the notes
17. The patient is referred to by name in the ... ... ... ... nursing entries of the patient’s notes
Final explanatory notes relating to the criteria and additional information collected within the NMCAT,
Absent Present Always Present Not Rated
3 Notes are not written in the patient’s words nor what was observed by the nurse (e.g., comments such as appears, seems, etc).Notes that are mostly using subjective language rate as absent.
Some, but not all, notes are objectively written in the patient’s words or what was observed by the nurse (e.g., patient is, patient states).
All notes are objectively written in the patient’s words or what was observed by the nurse (e.g., patient is, patient states). a description of the patient’s status.
Some entries within the shift period contains a statement regarding the patient’s condition. (e.g. the patient’s condition is deteriorating and he stated that he was ‘having difficulty breathing’). (e.g. Mrs Smith was comfortable today and refused all analgesia).
Each entry within the shift period contains a statement regarding the patient’s condition (e.g. the patient’s condition is deteriorating and he stated that he was ‘having difficulty breathing’). (e.g. Mrs Smith was comfortable today and refused all analgesia). The emphasis is on the status of the patient
No status would be required due to the context-(this would
Some entries contain evidence of a change in the patient’s condition, and some, but not all,
Each entry contains evidence of a change in the patient’s condition plus a description of the
There is no evidence of a change in the patient’s condition. That is: existing include a description
of the patient’s status, nor any observable signs or symptoms.
relevant notes include a description of observable and recorded signs and symptoms (e.g., coughing up blood, tachycardia of 160bpm) and whether this is an improvement or deterioration. The emphasis is on objective information.
observable and recorded signs and symptoms (e.g., coughing up blood, tachycardia of 160bpm) and whether this is an improvement or deterioration. The emphasis is on objective information supporting change in status.
problems continue or no problems continue
6 Notes are not written
Some, but not all, notes are objectively written in terms of observable behaviour (e.g., Mr Tablis was found clutching at his chest and stated “I can’t breathe”).
All notes are objectively written in terms of observable behaviour (e.g., Mr Tablis was found clutching at his chest and stated “I can’t breathe”).
7 There is evidence of deterioration in the patient’s condition, but the notes do not include a description of actions taken by the nurse.
There is evidence of deterioration in the patient’s condition, and some, but not all, relevant notes include a description of actions taken by the nurse (e.g., contacted the medical officer, sat Mrs Faith in the upright position).
There is evidence of deterioration in the patient’s condition, and all relevant notes include a description of actions taken by the nurse (e.g., contacted the medical officer, sat Mrs Faith in the upright position).
There is no evidence of deterioration in the patient’s condition.
8 There is evidence of the patient receiving treatment, but notes do not include a description of the patient’s response to the treatment. Treatment could include nebulizer, oxygen therapy, TED stockings, repositioning, personal hygiene, changes to the way which the patient ambulates, and counselling
There is evidence of the patient receiving treatment and some, but not all, relevant notes include a description of the patient’s response to the treatment (e.g., TDS dressings applied to Mr Hamilton’s leg wound and wound edges are now raised and pink and the wound surface area is decreasing).Treatment could include nebulizer, oxygen therapy, TED stockings, repositioning, personal hygiene, changes to the way which the patient ambulates, and counselling
There is evidence of the patient receiving treatment and all relevant notes include a description of the patient’s response to the treatment (e.g., TDS dressings applied to Mr Hamilton’s leg wound and wound edges are now raised and pink and the wound surface area is decreasing). Treatment could include nebulizer, oxygen therapy, TED stockings, repositioning, personal hygiene, changes to the way which the patient ambulates, and counselling
There is no evidence of the patient receiving any treatment.
9 There is evidence of the patient receiving a prn or short-term medication, but notes do not include a description of the patient’s response to
There is evidence of the patient receiving prn or short- term medication and some, but not all, relevant notes include a description of the patient’s response to the
There is evidence of the patient receiving a prn or short-term medication and all relevant notes include a description of the patient’s response to the medication (e.g., BP
There is no evidence of the patient receiving any prn or short-term medication.
the medication. Note: Short-term medication is a medication commenced to reduce a patient’s blood pressure or a medication that is adjusted according to the patient’s response such as warfarin or insulin.
medication (e.g., BP returned to normal limits 120/80 mmHg following 2 days of XXX) either in the current note or in a separate later note. Note:
Short-term medication is a medication commenced to reduce a patient’s blood pressure or a medication that is adjusted according to the patient’s response such as warfarin or insulin.
returned to normal limits 120/80 mmHg following 2 days of XXX) either in the current note or in a separate later note. Note:
Short-term medication is a medication commenced to reduce a patient’s blood pressure or a medication that is adjusted according to the patient’s response such as warfarin or insulin.
10 Notes do not describe a progressive series of events in time order.
Some, but not all, notes describe a progressive series of events in time order.
All notes describe a progressive series of events in time order.
There are not enough notes in the time period.
11 All words are illegible.
Most words are legible.
12 None of the notes include a date or time.
Some, but not all, notes include a date and time.
All notes include a date and time.
13 There is evidence that unusual events (other than normal activities, e.g. going to the toilet) occurred during the
There is evidence that unusual events (other than normal activities, e.g. going to the toilet) occurred during the shift and some, but not all,
There is evidence that unusual events (other than normal activities, e.g. going to the toilet) occurred during the shift and the majority of
There is no evidence that unusual events (other than normal activities, e.g. going to the toilet) occurred during the shift. shift, but notes are
only written at the end of the shift, with no evidence of specific times when events occurred.
relevant notes were written as the incidents occurred, including specific times when incidents occurred.
14 There is evidence of events occurring during the shift, but notations are made out of sequence (e.g., referring to a resolved problem in an unusual sequence, recording of events on dates or at times that have not followed the event appropriately).
There is evidence of events occurring during the shift, and some, but not all, notes describe the pattern of events appropriately and in a logical and sequential order (e.g., procedure, observations for complications, preparation for discharge).
There is evidence of events occurring during the shift, and all notes describe the pattern of events appropriately and in a logical and sequential order (e.g., procedure, observations for complications, preparation for discharge).
There is no evidence that events occurred during the shift.
15 Notes include normal data values (BP, temperature, etc) that is also recorded, signed and dated on other nursing charts
Some, but not all notes, include normal data values (BP, temperature, etc) that is also recorded, signed and dated on other nursing
There is no evidence of duplication or normal data values (BP, temperature, etc), with this data being recorded only on other nursing
Long term patients with no routine daily observations.
(i.e., duplication). charts (i.e., some duplication).
charts (i.e., no duplication). 16 There is no evidence
of written documentation of any education or psychosocial support being delivered, although the patient’s clinical condition would require such care.
There is evidence that education and / or psychosocial support is being received by the patient, and relevant notes document the provision by nurses.
There is no evidence that education or psychosocial support is required.
17 The patient is never referred to by name (e.g., patient rather than Mrs Nguyen).
The patient is sometimes, but not always, referred to by name (e.g., Mrs Nguyen rather than the patient).
The patient is always referred to by name (e.g., Mrs Nguyen rather than the patient).
SECTION C: Transcription of documentation
For every 10th record, please transcribe verbatim the text for the 24 hour period selected for this record audit. Do not record the patient’s name or MRN, using a code number or pseudonym of necessary. Please use the back of this page and additional pages if necessary.
Record No.: ...
Audit Reviewer’s Name: ...
Shift 1: ...
...
...
...
Shift 2: ...
...
...
...
Shift 3: ...
...
...
...
SECTION D: Record Characteristics and Legal Aspects of Documentation 18. Was the following recorded on each page?
A / N o N s e Y a
i r e t i r C
a. Patient’s name
b. Health Care Record number c. Patient’s date of birth
d. Evidence of the use of abbreviations from the official list of
approved abbreviations only
e. Name, signature and designation of the nurse writing the report is
written legibly at the end of each entry
f. Evidence of the use of appropriate medical terminology g. Entries are made on the behalf of the writer and never on behalf
of another person