Abstrak
Antara tahun 1985-1995 (10 tahun) telah dilakukan penelitian terhadap 30 anak dengan nefritis lupus yang dikumpulkan dari 7 pusat Nefrologi Anak di Indonesia. (Jmur rata-rata penderita ialah I
I,7 tahun (berkisar antara 8 satnpai
I8
tahun) dengan perbandingan anak perempuan terhadap taki-laki 5 berbandtngl.
Gejala klinis yang terbanyak diremukan adalah panas tinggi 8loÀ, ruam muka 66,6ok dan artritis atau artralgia 44,4%. Sembilan penderita (30%) nenunjukkan gambaran klinik sindrom nefrotik,I7
(56,6%ù glomerulonefritis, 2 (6,5%o) proteinuria dan hematuria, 2 (6,5%0) proteinuria saja. Biopsi ginial dilalatkan pada II penderita
dengan hasil nefropati membranosa padaI
kasus, glomerulonefritis proliferatiffokal
pada 1, glomerulonefritis mesangial pada 2 dan kelainan minimal pada 2 kasus. Jenis terapi yang diberikan adalah prednison oral pada kasus ringan, kombinasi prednison dan siklofosfamid atau azalioprin pada penderila dengan glonrerulonefrilis atan sindrom nefrotik. Kadang-kadang diberikan bolus metilprednisolon dan pada beberapa kasus terapi puls siklofos.famid. Selann pengamatdn, 9dari 30 penderita meninggal
dunia. Semuanya menunjukkan gambaran klinik glomerulonef itis. Dua dari 9 penderila sindrom nefrotik mendapat pengobatan dialisis.Abptract
Thirty systemic lupus erythematosus (SLE) children with renal involvement treated benveen 1985-1995
from
7 Pediatric Nephrologt Centers throughout Indonesia were reviewed. The ntean age of onset of lhese palients was I I,7 years (range be^ueen 8 to 18 years) with a preponderance of female to male ratio 5 1oL
The presenting clinical features were high grade fever 81%, malar rash 66,60Âand arthritis or joint pain 44,4%. Nine (30%o) patients had nephrotic syndrome,
l7
(56,6%) (chronic) glomerulonephrttis, 2 (6,6%0) proteinuria and hematuria and 2 (6,6%) isolaled proteinuria. Renal biopsy done in II patients revealed
membranous nephropathy ittl,
dilfuse proliferative glomentlonephritis (GN) in 5, focal proliferative GN in I , mesangial proliferalive GN in 2 and minimal changein
2
cases. The treatmen! regimen given to these patients was oral prednisonein
mild cases, combination
of prednison and cyclosphosphamide or azathioprine in palients with glomerulonephritis and nephrolic syndrome, with occational methylprednisolone bolus andin
some patients pulse cyclophosphamide. Nine of the 30 patients diedof
whomall
had clinical presentationof
glomentlonephritis. Two patients wilh nephrolic syndrome was on dialysis trea!ment.Keywords: systemic lupus erythemalosus, lupus nephritis, lerminal renal failure Vol 9, No 4, October
-
December 2000Lupus
nephritis among
children
in
Indonesia
Husein Alatas
Systemic
Lupus
Erythematosus
(SLE)
is an
immune
complex mediated disorder
affecting multiple
organsof the body. When
the
immune complexes
arelocalized
in
the
capillary wall of
the
glomeruli, lupus
nephritis
develops.Renal manifestations
are presentin
nearly
two
thirds
of
children
with
SLE.
Renal
involvement
is
a
major
cause
of
morbidity
in
SLE.r Although
with
moderntherapy renal failure
is
becoming less frequent, in
many
series
of
patients
renal failure
eventually
developed.2
In
this
paper
the clinical manifestation,
histologic picture
andoutcome
of
lupus nephritis
wasDivision of Neohrologt, Department of Child Health, Faculty of Medicine, University of Indonesia, Jakarta, Indonesia
Lupus
nephritis
265presented. Since
the number
of
cases amongchildren
is
relatively rare compared
with
that in the
adult
population, the
data
was compiled from 7
pediatric
nephrology centers
throughout Indonesia
between1985
to
1995.MATERIALS
AND METHOD
The
patients
was
collected retrospectively
from
7pediatic nephology centers
by distibuting
questionnaire,namely from
Jakarta,
Medan,
Palembang,
Bandung,Yogyakarta,
Surabaya
and Manado. The
number
of
casesfrom
each center was presentedin table
l.
Thediagnosis
of
SLE
was made using The
American
Rheumatism
Association
(ARA)
1982
revised266
AlatasAll
were
18years o
f age
or younger. Renal
disease(Lupus Nephritis) in
thesepatients was confirmed
by
the
presenceof
one
or more
of
the following sign
:proteinuria,
hematuria,
acute
glomerulonephritis,
nephrotic
sSmdrome,renal failure.
The resultsof
renalbiopsy
evaluated
by
light and
immunofluorecent
microscopy, were classified
according
to
the WHO
criteria:aMedJ Indones
The dominant clinical feature
at
the time
of
initial
presentationis shown in table 2.
It
could be
seen thatthe presenting clinical
featureswere high
gradefever
in
22
cases(81%), malar rash
in 18 (66,6%)
andarthritis
or arthralgiain
12 cases(4,4%).
Hypertension was detectedin
l0
cases (33,3o/o).Table2. Clinical manifestation on admission
-
ClassI
-
Class 2-
Class 3-
Class 4-
Class 5normal
glomeruli
mesangial
alteration
(mesangiopathy)focal proliferative glomerulonephritis
diffu
seproliferative glomerulonephritis
membranous
glomerulonephritis
Fever Malar rash Arthritis / arthalgia Alopecia
Stomatitis Hyperpigmentation Pallor
22
l8
t27 4 4
7
81,5
66,6 44,4
25,9 13,2 t3,2 25,7 Table L Number ofcases reported from 7 pediatric nephrology
centers
City Medan Palembang Jakarta Bandung Yogyakarta Surabaya Manado Total
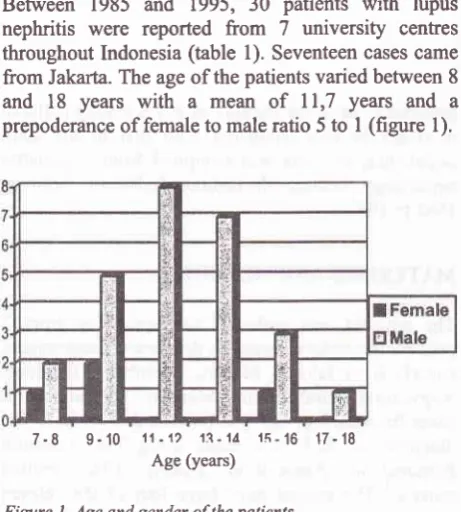
RESTJLT
Between 1985
and
1995,
30
patients
with lupus
nephritis were reported
from
7 university
centresthroughout Indonesia (table
l). Seventeen
cases camefrom
Jakarla. The ageof
the patientsvaried
between 8and
18
years
with
a
mean
of
ll,7
years and
a prepoderanceof
female to maleratio
5to
I
(figure
l).
[image:2.595.86.317.459.715.2]7-8 9-10
11-1)
17-1À
l5-'16
17-18 Age (years)Figure
l.
Age and gender ofthe patientsHypertension
Table
3
showed
the
result
of
hematological
andimrpunological pattem
of
the patients.
Anemia
wasfound in
80%of
the cases,but hemolytic
anemiaonly
l2Yo;
leucopenia
in 25%o
and thrombocytopenia
in
20%. Erytfuocyte sedimentation
rate wasfound
in all
cases(100%),
low C3
90olo,low C4
60yo,antinuclear
antibody (ANA)
80%,double
strandedDNA
75% andLE cell
in40%..Table
3.
Result of hematological and immunological examinationLaboratory finding
33,3
l0
I
4 t7
I
24
I
30
% Anemia (Hb <
l0
g%Hemolyic anemia Leucopenia Thrombocytopenia ESR
Low C3 Low C4
ANA(+)
Ds DNA (+)
80
t2
25 20
100
90 60 80 75 LE cells (+)
Yol 9, No 4, October
-
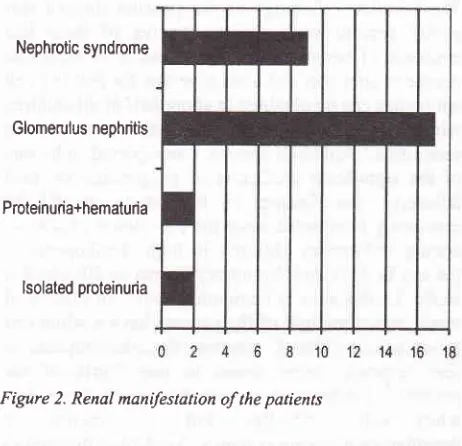
December 2000Nephrotic syndrome
Glomerulus nephritis
Proteinuria+hematuria
[image:3.595.77.308.86.309.2]lsolated proteinuria
Figure 2. Renal mandestation of the patients
Renal
biopsy
was doneonly in
I
I
patients dueto lack
of
parental permission. Diffi.rseproliferative
glomcrulo-nephritis was the most frequenthistologic abnormality
in
the biopsy
specimens,namely
in 5
cases.One had
membranous nephropathy,
I
focal
proliferative
glomerulonephritis,
I
with
mesangialalteration
and 2with minimal
lesion (rable 4).Table 4. Result ofrenal biopsy in I
I
casesHistopathology Class I minimal lesion
Class 2 mesangial alteration
Class 3 focal proliferative glomerulonephritis
Class 4 diffuse proliferative glomerulonephritis
Class 5 membranous nephropathy
2
2
I
5 I TotalAll
patients were
treatedwith
prednisone.
In
patientswith
clinical
presentation
of
acute
or
chronic
glomerulonephritis
or
nephrotic syndrome
or
renalbiopsy
flrnding
of
diffi.rse proliferative
lesion,combination
of
oral
prednisone and cyclophosphamideor
azathioprine
was given. Some patients
received coursesof
intravenous methylprednisolone
bolus
(30mg/kgBWday
in 3
onsecutive days, every other day).Three
patients received
pulse
cyclophosphamidecourses
monthly (500-750 mg/m2)
in
combination
with MESNA for
6 monthsfollowed
by a
threemonth
intervals.
Beside a moderate degreeof
leucopenia and nausea, no other side effects was detected.Lupus
nephitis
267Table
5.
Correlation of clinical presentation and outcomeof
the patientClinical
N
Normal
Renalfailure
DeaÉrpresentation
Rslal
--filrction Moderate
I
Terminal ProteinuriaProteinuria +
hematuria
Glomerulo-nephritis Nephrotic
syndrome
2 2
)
7
2(D)
Table
5 showedthe outcome
of
the patients relatedto
the clinical
presentation.
The
total
number
of
deathduring the study period was
9
out
of
30
patients(30%).
No
death was reportedin
thegroup of
patientswith
the
clinical
presentation
of
only
proteinuria
and/or
hematuria.The renal
firnction of
these patients was alwayswithin normal limits
during the
follow
upperiod, while
in
II
out
of
20
cases
with
clinical
presentation
of
acute
or
chronic
glomerulonephritis
and 3out
of
6 caseswith
nephrotic
syndrome showed moderateto severe
impairment
of
the renalfirnction.
Nine
out
of
20 patients
with
acuteglomerulonephritis
died. In
patients
with nephrotic
syndrome
2
was
ondyalisis
treatment.Table 6 showed the
correlation of
the numberof
death and thehistological
presentation. Threeout
of5
caseswith
class
IV
lupus nephritis
died.
Two
due
to
terminal renal
failure
and one
dueto
nonrenal cause.
One
case
with
class
I
died due
to
nonrenal
cause(shock
ofunknown
cause)and
I case
ofclass 3
died
due toterminal renal failure.
Table
6. Correlation
of
renal biopsy and outcomeof the
patientsHistopathology
N Death
Cause of death(N)
Ren"t-fN"*e"al
Classl
2
I
-
IClass
2
2
-Class3
I
I
I
-Class4
5
3
2
|Class 5
I
-l6 30
ll
[image:3.595.330.570.86.262.2] [image:3.595.327.569.472.731.2]268
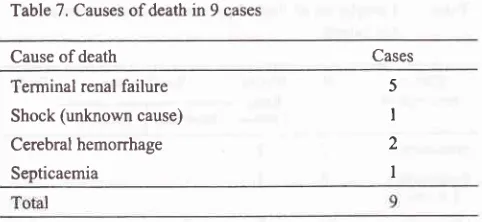
AlatasTable 7. Causes ofdeath in 9 cases
Cause of death Cases
Terminal renal failure Shock (unknown cause) Cerebral hemorrhage Septicaemia
5
I
2
I
In
Table
7
it
could be
seenthat the
causeof
deathwere mostly
dueto terminal renal failure namely
5of
9
cases.One patient
died
due
to
shock
of
unknown
cause,2
dueto
cerebral hemorrhageand
I
becauseof
septicaemia.
DISCUSSION
Systemic
lupus
erythematosus(SLE) is
an uncotrunonchildhood illness
characterized
by
the formation
of
autoantibodies and
immune
complexeswhich
mediateinflammatory
responses.Lupus nephritis
(LN)
is
oneof
the most
severe
forms
of
organ involvement in
SLE.5-6
In
this
study
in
aperiod
of
l0
yearsonly
30patients was reported
from
7
pediatric
nephrology
centres
of which
l7
patients was registeredin
Jakarta.Accurate figures
on the incidenceof
SLE
in
childhood
are
difficult
to
obtain,
but
estimates
in
the
United
States
are
about
0,6
children
in
100.000.t
Othe.
countries
much lower
rates,
possibly
reflecting
rs.8
Overall
incidence
of renal
diseasein
LEis7SY,.e
The
averageage
of
the
patients
was
I1,7 years old
(range
8-18
years)
with
a
female
to
male ratio
5:1,which is
in
accordancewith the
literature. The
onsetof
SLE in
childhood
is
observedmostly
between the agesof
ll
and
15years,
although the
diseasemay
piesent earlier
in
life.r0
Girls
get lupus
five
timesmore
frequently
than
boys, although
this
striking
female
preponderanceis not
seenuntil
after
puberty, suggesting therole
of
endocrine factors
in
theclinical
expression
of
the disease. I IThe
clinical
manifestation at the
time
of
diagnosisin
this study
is
mostly fever, malar rash and
arthritis.
These
sign
and
symptoms
are
most
commonly
encountered
in
theliterature.
A
collaborative
studyby
the French Society
of
Pediatric Nephrologyr2
reportedthat fever, rash and arthritis was the major
clinical
features
in
62 children
with
SLE namely
75yo,72yo
and 64Yo consecutively.
Med J Indones
The laboratory findings
of
the
patients showed
thateighty percent
were
anemic,
twelve
of
them
hadevidence
of hemolyic
anemia.
Anemia
of
moderate degreeis
common
and apositive test
for
anti red cell
antibodies can be obtained
in
abouthalfofall
children
with
lupus. However
severehemolytic
anemia arenot
seen often.2Although
anemiawas reported
to
be
oneof
the significant predictors
of
progression
to
renalfailure,13
the finding
in
this
study
should
becausiously interpreted
sincethe
prevalenceof
anemiaamong Indonesian children
is
high. Leukopenia
is presentin
25%o andthrombocytopenia
in
20%oin
this
study.
Leukopenia
is
commonly found
in
childhood
lupus,
sometimehalf
of
thepatients
have awhite
cell
count below 5000/ul,
whereas thrombocytopenia
isless common,
being found
in one fourth
of
thepatients.' Leukopenia presumably result
from
antiwhite cell
antibodies,
but the
origins
of
thrombocytopenia
arecomplex. Antibodies
directed todsDNA
are
comnonly
considered
to
be specific for
active SLE. Hypocomplementemia
is
evident
in
morethan three
fourth
of
children
with
lupus and
in
agreater proportion
of
those
with
evident
nephritis.Hypocomplementemia
was found along
with
raisedanti-ds
DNA. In this
study the
percentageof
positive
ANA, dsDNA is
found
in 80%
and75oÂof
the cases,while low
C3
andC4 in
90o and 60%o consecutively showing that the disease arestill
active.The
renalmanifestation
in this
study
aremostly
acuteglomerulonephritis
and
nephrotic syndrome. Mild
presentation
like
isolated
proteinuria and
hematuriawas
only found
in
13%
of
the patients. The mode
of
clinical
presentationof
renal disease ismostly
relatedto
the
histological grade
of
renal biopsy.
Of
thepatients
who
presentedwith nephrotic
syndrome,
all
but
one had
proliferative
glomerulonephritis
(class 3and
4)
where
as
of
those
who
presented with
proteinuria
had classI
and2histologic
feature.raThe natural history and overall
prognosis
of lupus
nephritis
in
childhood as were
in
adult
cases
areclosely
correlated
with
the nature
of
the patbological
renat
lesions.'t
The prognosis
areworst
in
caseswith
diffuse proliferative
glomerulonephritis
lesion
(class4).r6 Repeated
biopsies
showed thatminimal
lesionof
focal
and segmentalglomerulonephritis may
progressto
more
severe
lesion such as diffirse
proliferative
lesion
if not
properly treated.
On the
other
handimprovement
of
renal
lesions
may be
observed
andcellular
proliferation
of difhrse
proliferative
glo-merulonephritis may resolve
with
adequate treatment. [image:4.595.76.317.94.205.2]Yol 9, No 4, October
-
December 2000prompt
treafrnent
in
lupus nephritis
in
children. Five
of I
I
biopsy
finding in this
study showed histologic
featureof
diffirse
proliferative
lesion. The severity
of
clinical
presentation
and high proportion
of class 4
renal
histology
finding
could
maybe explain
therelatively
high
mortality in
this study namely 9 out
of
30
cases(30%).
Recent
publication
showed
that
themortality
rateof
SLE
in
children
wasonly
15% inl0
years and 23%n
l5
years period.lTThe
causeof death
in
this study are mostly
due to
terminal renal failure (5
of
9 cases). One dueto
shockofunknown cause,2
dueto
cerebralhemonhage
andI
due
to
septicaemia.
In
a compilation
of
100 casesfrom
several centres showed that44 cases died
due torenal
failure,
and
36
cases dueto
septicaemia, and 4cases
died
caused
by
central
nervous
systeminvolvement.2
The
importance
of
extrarenalinvolvement
as a causeof
deathin
children
with
lupusis
evident
in
these series,particularly
central
nervoussystem and pulmonary
hemorrhage.
However,
themain
nonrenal causeof
death isinfection.
In mild
cases renal involvementin
children
with
SLE
is often
well
controlled
with
corticosteroid alone.
In
children
with
severe
lupus
nephritis,
intravenousmethylprednisolone
may
provide
dramatic
anti
inflarnatory effects as was also
experience
in
our
cases.
However,
intavenous
methylprednisolone
isnot
satisfactory
for
long
term
control
of lupus
nephritis since
this
regimen
has been associatedwith
significant
complication,
including
pancreatitis, hypertension,electrolyte abnorm
alities
and death. I 8' I eFor
cases
with
corticosteroid unresponsive
lupusnephritis,
combination
with
cytotoxic drugs
arenecessary.
After
the
use
of
cyclophosphamide
theprognosis
for children with continuing
active
diseaseimproved
significantly.20
Others
reported
that
combination
of
prednison and
azathioprine
to
be
a sati sfactory alternative.2 IFor
lupus nephritis
with
histological lesion
of
diftrrseproliferative glomerulonephritis
the useof
intermittent
intravenous cyclophosphamide has been reportedwith
dramatically improved
outcome.22In
comparisonwith
daily oral
therapy,
the
immunosuppressiveeffects
of
this
regimen
appea-rt-o
be
greater and
its
toxicity
appearsto
be
less.22'23In
this
report three
patientsreceived pulse
cyclophosphamide.Beside
a
moderate degreeof
leucopenia and nausea,no
other side effects was detected.Luptæ
nephritis
269
Hemorrhagic
cystitis occurs
in
l5o/o
of
patientsreceiving cyclophosphamide.
MESI\IA
inactivates
the cyclophosphamide metabolites responsiblefor bladder
irritation."
We
have used
MESNA
in our
cases togetherwith
adequatehydration
andno
hemorrhagiccystitis
wasfound
among them.Cyclosporine has been proposed as
a usefirl
therapyfor
children
with
corticosteroid-resistant
lupus nephritis.2sHowever, more
studiesof
cyclosporinè is
still necessary
before fiuther
recommendation
of
its
usein
lupusnephritis
in
children.
Acknowledgements
rile
would like to thank Drs.
Rusdidjas, Bachnrn D,
Sudjatrniko S.,
SekarwanaN.,
Damanik
M., Noor
S.'
Umboh
A., for
their confibution
to
send data
of
patients to be analizedin this
report.REFERENCES
L
Fish AJ, Blau ED, Westberg NG, et al. Systemic lupus erythematosus within the first two decadesof
life. Am J Med 1977:62:99-117.2.
Cameron JS. Nephritisof systemic
lupus egrthematosus. In: Edelmann CM Jr, editor. Pediatric Kidney Disease, 2d ed. Boston: Little Brown Co;1992. p. l+07-65.3,
Tan EM, Cohen AS, Fries JF, etal.
The 1982 rcvisedcriteria
for
the classification
of
systemic
lupus erythematosus. Arthritis rheum 1982;35 :127l-7.
4.
Churg J, Sobin LA. Classification and atlas of glomerular disease. Tokyo: Igaku Shoin; 19E2.5.
Gisnel. Lupus nephritis: Prognostic factors and probabilityof
maintaining life-supporting renal functionl0
years after the diagrosis. Am J Kidney Dis 1992;19:473-9.6.
Appel GB, Cohen DJ, Pirani CL, et al. Long term follow up ofpatients with lupus nephritis. A study based on the classification of the wHo. Am J Med lggT;g3:877-g5.7.
Fessel
WJ.
Systemic
lupus
erythematosusin
the community. Arch Intern Med 1974;134:1027-31.8.
Lehman
TJA,
Mouradian
TA.
Systemic
lupus erythematosus.In:
Holliday
MA,
Banat
TM, editors.
Pediatric Nephrology,3d
ed.
Baltimore:Williams
&
Wilkins 1994:849-70.9.
Fish AJ, Renal manifestationof
systemic disorders. In: Poslethwaite RI, editor. Clinical Pediatric Nephrology 2ded. London: Butterworth Heinemann Ltd" 1994:23547.
10.
LehmanTJA,
Mc
Cardy
DK,
BemsteinBH,
et
al.Systemic lupus erythematosus
in the
first decadeof life.
Pediatrics I 989;83:235-9.I
l.
Emery
H.
Clinical
aspects
of
systemic lupus
er1Æhematosus
in
childhood. PediatrClin
North
Am 1986;33: I 177-90.270
AIatasMc
KurdyDK
Lehman TJA, BemsteinB,
et al. Lupusnephritis
:
Prognostic factorsin
children. Pediatics 1992;89:240-6.Morris MC,
Cameron JS, ChantlerC, et al.
Systemiclupus erythematosus
with nephritis. Arch Dis
Childh l98l;56:779-83.Austin
HA
III,
Muenz LR, JoyceKM,
et al. Prognostic factors in lupus nephritis. Contribution of renal-histologic data. Am J Med 1983;75:382-91.Austin
HA III, Muenz
LR"
JoyceKM, et
al.
Diffrrseproliferative lupus nephritis
:
Identificationof
specificpathological features
affecting
outcome.Kidney Int
1984;25:689-95.
Platt
JL, Burke
BA,
Fish
AJ, et al.
Systemic lupus erythematosusin
the
first
two
decadesof
life. Am
JKidney Dis 1982;2(Suppl l):212-21.
Barron
KS,
Person DA,Brewer
EJ,
et
al.
Pulse methylprednisolone therapy in diffrrse proliferative lupus nephritis. J Pediatr 1982;l0l
: 137-141.Kimberly RP. Systemic lupus erythematosus treatment -corticosteroids and anti inflammatory drugs. Rheum Dis
ClinNorth Am 1988; 14:203-21.
Med J Indones
Mc
Curdey DK, Lehman TJA, Bemstein B, et al. Lupus nephritis : prognostic factors in children. Pediatrics 1992; 89:240-6.Cameron
JS. Lupus nephritis
in
childhood
and adolescence. Pediat Nephrol 1994;8:23049.Martinelli R, Pereira LJ, Santos ES, et al. Clinical effects
of
intermittent intravenous cyclophosphamidein
severe S.L.E. Nephron 1996;7 4:313-7.Lehman
TJA,
Mouradian
JA.
Systemic
lupuserythematosus, in: Barratt TM, Avner ED, Harmon WE, Eds. Pediatric Nephrology, 4ù ed. Baltimore
:
Lipincott Williams&
Wilkins 1999:793-810.Firm GP,
SidanRNB. Protecting the
bladdercyclophosphamide
with
MESNA.
N
Engl
J1986;3 l4:61-5.
25. Feufien
G,
Guerin
S, Noel LH, et al.
Effects
of
Cyclosporine
in
severe systemic lupus erythematosus. JPediatr 1987; I I l:1063-8.
13.
14.
15.
t6.
t7.
18.
t9.
20.
21.
22.