E
DITORIAL
Stress and Schizophrenia: The Importance of Cognition
Schizophrenia is increasingly viewed as a neurodevelop-mental process caused by an interaction between genetic factors and environmental stressors (for a review, see Parnas 1999). In this interactive model, environmental stressors may precipitate psychotic periods in vulnerable individuals (the “Vulnerability/Stress model of schizo-phrenic episodes,” Nuechterlein and Dawson 1984). How-ever, when considering this model, one should take into account that a situation is stressful only if the individual
interprets this situation as being threatening or stressful
(Mason 1968). Cognitive interpretation of an environmen-tal stimulation is thus one of the major factors explaining the important inter- and intrasubject variability in response to stress, and it might be at the origin of the increased vulnerability of schizophrenic patients to environmental stressors.
Interpretation of a situation as being stressful or not is under the control of cognitive processing, and the ability of the individual to discriminate between threatening and nonthreatening information (a cognitive process called selective attention). When assessing cognitive function in schizophrenic patients, researchers have for many years relied almost exclusively on tasks measuring the extent of cognitive impairments in schizophrenic patients. This methodology only permits assessment of whether schizo-phrenic patients are more impaired than normal control subjects in terms of overall cognitive processing. How-ever, measuring the extent of a cognitive impairment does not provide any information as to the nature of the cognitive deficit. Cognition is made up of a variety of information processing components (vigilance, selective attention, working memory, consolidation, long-term memory of an episodic or semantic form), and it is only by measuring the exact nature of a “cognitive impairment” that one can determine its cerebral origin and set up appropriate therapeutic interventions. The same rationale applies to the study of the relationship between stress and schizophrenia. Indeed, and because a situation has to be interpreted as stressful to generate a physiologic reaction, it becomes important to know the exact nature of the cognitive impairment in schizophrenic patients if one wants to disentangle the cause(s) of the increased reactiv-ity to stress observed in this population.
The report by Dr. Walder and collaborators (Walder et al 2000) in this issue is a perfect example of such an approach. Using various cognitive tests chosen for their specificity and sensitivity to various components of cognitive processing, the authors report that, in a population of patients with psychotic disorders, basal cortisol levels are inversely correlated with
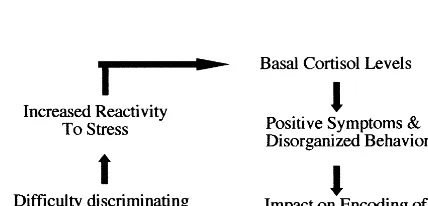
performance on cognitive tasks assessing hippocampal and frontal lobe functions. More importantly, they report that there is no significant correlation between basal cortisol levels and performance on a task measuring vigilance and attention, thus showing that the cortisol-related memory problems in schizophrenic patients are not due to basic attentional problems. This finding is a good example of the richness of data obtained when one is measuring the nature rather than the extent of a cognitive impairment. Indeed, if a memory scale like the Mini-Mental State Examination (MMSE) had been used in this study to assess cognitive function in schizophrenic patients, there would have been no way of knowing whether the observed memory deficits in the patient population were due to basic attentional problems or to pure memory impairments (for a report on the limits of the MMSE in psychiatric populations, see Anthony et al 1982). On a second set of analysis, the authors report that in the patient population higher cortisol levels were correlated with higher ratings of positive symptoms and disorganized behaviors, although not with negative symptoms. Since positive symptoms were also correlated with performance of patients on hippocampal-dependent memory tasks, this second-order relationship suggests that impaired hip-pocampal-dependent memory performance in schizo-phrenic patients might be related to the close relationship existing between high cortisol levels and increased ratings of positive symptoms. Positive symptoms and/or disorga-nized behaviors in schizophrenic patients might act by impairing successful encoding of information into long-term memory store, leading to memory impairments. Encoding of information into long-term memory is depen-dent upon working memory process, which serves to maintain and manipulate incoming information for a short period of time. If schizophrenic patients are impaired at the level of encoding of information, this might affect their capacity to discriminate between relevant (threat) and irrelevant (nonthreat) information and further increase their reactivity to stress. This increased reactivity to stress in patients with disorganized behaviors and/or positive symptoms might in turn increase circulating levels of stress hormones and lead to the observed relationship between increased basal cortisol levels and psychotic symptoms (for a schematic representation of this closed-loop relationship, see Figure 1).
The observed relationship between positive symptoms and basal cortisol levels in schizophrenic patients reported by Dr. Walder and collaborators is consistent with the cortical–thalamic– cerebellar– cortical model of schizo-phrenia proposed by Andreasen et al (1999). A growing
© 2000 Society of Biological Psychiatry 0006-3223/00/$20.00
body of clinical and neuroimaging literature now recog-nizes a possible cerebellar correlate in schizophrenia (Jacobsen et al 1997; Levitt et al 1999; Nasrallah et al 1985). Interestingly, there is evidence for a high density of glucocorticoid receptors in the cerebellum (Sanchez et al 2000), and this structure has important projections to the forebrain, limbic system, hypothalamus, and brain stem, as well as multiple projections to the prefrontal cortex (for reviews, see Leiner et al 1995; Schmahmann 1991). Moreover, the functional role of the cerebellum in cogni-tive function is being rethought, and various studies now report the implication of this structure in aspects of cognition involving modulation of thought, learning, and strategic planning (for a review, see Schmahmann 1991). Patients with cerebellar pathology are impaired in tasks of selective attention, showing that these populations have difficulty discriminating between relevant and irrelevant information. Finally, many case studies have recently been published that describe a significant relationship between psychiatric symptoms and cerebellar pathology (Hamilton et al 1983). For example, Jurjus et al (1994) reported the presence of psychotic, positive symptoms in patients suffering from cerebellar degeneration, and Sandyk (1993) reported the case of a 27-year-old man diagnosed with paranoid schizophrenia who developed onset of psychotic symptoms after removal of a cerebellar tumor. Given the presence of glucocorticoid receptors in the cerebellum, this set of data could eventually be used to test whether the relationship observed between basal cortisol levels and positive symptoms in schizophrenic patients is related to a glucocorticoid-induced cerebellar dysfunction. Here again, using neuropsychology as a tool (nature) rather than as a mean (extent) should prove highly valuable for determining the exact origin of this relationship.
Sonia J. Lupien
McGill University Douglas Hospital Research Department 6875 Boulevard LaSalle Montre´al, Que´bec H4H 1R3 Canada
References
Andreasen NC, Nopoulos P, O’Leary KS, Miller DD, Wassink T, Flaum M (1999): Defining the phenotype of schizophrenia: Cognitive dysmetria and its neural mechanisms. Biol
Psychi-atry 46:908 –920.
Anthony JC, LeResche L, Niaz U, von Korff MR, Folstein MF (1982): Limits of the “Mini-Mental State” as a screening test for dementia and delirium among hospital patients. Psychol
Med 12:397– 408.
Hamilton NG, Frick RB, Takahashi T, Hopping MW (1983): Psychiatric symptoms and cerebellar pathology. Am J
Psy-chiatry 140:1322–1326.
Jacobsen LK, Giedd JN, Berquin PC, Krain AL, Hamburger SD, Kumra S, Rapoport JL (1997): Quantitative morphology of the cerebellum and fourth ventricle in childhood-onset schizophrenia. Am J Psychiatry 154:1663–1669.
Jurjus GJ, Weiss KM, Jaskiw GE (1994): Schizophrenia-like psychosis and cerebellar degeneration. Schizophr Res 12: 183–184.
Leiner HC, Leiner AL, Dow RS (1995): The underestimated cerebellum. Hum Brain Mapp 2:244 –254.
Levitt JJ, McCarley RW, Nestor PG, Petrescu C, Donnino R, Hirayasu Y, et al (1999): Quantitative volumetric MRI study of the cerebellum and vermis in schizophrenia: Clinical and cognitive correlates. Am J Psychiatry 156:1105–1107. Mason JW (1968): A review of psychoendocrine research on the
pituitary-adrenal cortical system. Psychosom Med 30:576 – 607.
Nasrallah HA, Jacoby CG, Chapman S, McCalley-Whitters M (1985): Third ventricular enlargement on CT scans in schizo-phrenia: Association with cerebellar atrophy. Biol Psychiatry 20:443– 450.
Nuechterlein KH, Dawson ME (1984): A heuristic vulnerability/ stress model of schizophrenic episodes. Schizophr Bull 10: 300 –312.
Parnas J (1999): From predisposition to psychosis: Progression of symptoms in schizophrenia. Acta Psychiatr Scand Suppl 395:20 –29.
Sanchez MM, Young LJ, Plotsky PM, Insel TR (2000): Distri-bution of corticosteroid receptors in the rhesus brain: Relative absence of glucocorticoid receptors in the hippocampal for-mation. J Neurosci 20:4657– 4668.
Sandyk R (1993): Psychotic behavior associated with cerebellar pathology. Int J Neurosci 71:1–7.
Walder DJ, Walker EF, Lewine RJ (2000): Cognitive function-ing, cortisol release, and symptom severity in patients with schizophrenia. Biol Psychiatry 48:1121–1132.
Figure 1. A closed-loop model of the impact of cognition on reactivity to stress in schizophrenic populations.
1120 BIOL PSYCHIATRY Editorial