1
INTEGRATION OF HIV INTO THE NATIONAL SOCIAL
HEALTH INSURANCE PROGRAM - Policy Note
12
Key summary points:
• Indonesia has the opportunity to strengthen its national HIV response by integrating key HIV-related services in the national social health insurance program Jaminan Kesehatan Nasional.
• The type of services to be included in the Basic Benefits Package and resulting costs and public health benefits need careful consideration by decision-makers.
• This policy note explains the options and medium-term cost implications.
• Provision of HIV services within the basic benefits package of JKN would require a medical cost charge ranging from IDR 558 per month to IDR 371, or IDR 7,956 to IDR 4,452 per year (equivalent to USD 0.5 to 0.3) depending on the comprehensiveness of the package. The proposed options are ranging from comprehensive coverage from HIV counselling and testing, diagnosis and treatment of sexually transmitted diseases, diagnostic tests for pre-antiretroviral (ARV) and ARV treatment, management of their side effects, and prevention of mother-to-child transmission of HIV, and basic coverage which only provide screening test and treatment for OI.
• The note summarizes the current coverage/funding mechanisms for HIV-related services, JKN member numbers and key target populations, detailed premium costs for HIV services up to 2019, and possible provider payment mechanisms for HIV services.
Introduction
The universal health coverage (UHC) approach offers great opportunities to reform and refocus national HIV responses and address some of their shortcomings. General taxation and health insurance schemes for UHC can improve financial sustainability of HIV programs and promote standardisation of a package of essential HIV services. Also, the UHC principles,which calls for the delivery of a comprehensive package of health services that respond to the burden of disease, can support the integration and quality of HIV services, improve equity in HIV service access, build coherence across different health areas, help address the social and economic determinants of HIV, strengthen health and community systems, and contribute to human
1This policy note is based on the study report on integration of HIV services into JKN by the World Bank and the Centre for Health Research University of Indonesia as its technical partner. The study is part of the World Bank’s technical support to the Government of Indonesia to strengthen policy development on the assessment of financial and programmatic sustainability of HIV programs.
2About this Policy Brief:
2
rights. However, the integration of programs previously managed vertically, such as HIV, into a national health insurance program requires careful consideration of
a) which HIV services are essential to address the country’s existing HIV disease burden and prevent a future increased HIV disease burden,
b) which populations need to be targeted with these services, and an estimated number of key affected populations who would need these services
c) which of these essential HIV services to include in the basic benefit package (BBP) of the UHC scheme
d) the implications of including such HIV services in primary care delivery in terms of access of HIV services key affected populations , and
e) the resulting costs and impact on the BBP premiums for integrating HIV into the UHC financing mechanisms.
Background
Indonesia is a country of 254.5 million population in 2014 and is a lower middle income country with a GNI per capita of US$3,630 in 2014. The country has rebounded strongly from the Asian financial crisis in 1997 and experienced robust economic growth for the past decade with the
country’s GDP almost doubled from US$ 580 billion in 2001 to US$ 1.1 trillion in 2012, making
Indonesia the 15th largest economy in the world and achieving upper-middle-income status in 2018. Sustained economic growth over the past 15 years helped to pull many people out of poverty and resulted in a more than 50% reduction of poverty rates from 24% during the crisis to 11% in 2014. Yet, inequality is increasing and access to basic health and social services varies significantly across regions.
Over the past decades, the country has achieve significant progress on key health outcomes. Life expectancy has increased from 68 in 2002 to 71 in 2012. Under-five mortality has declined from 48 per 1,000 live births in 2002 to 31 in 2012 and infant mortality rate fell from 68 per 1,000 live births in 1991 to 32 in 2013. Indonesia is projected to meet the child-health related MDG, but is off track for reducing maternal mortality rate. The HIV epidemic is growing, and pockets of the country continue to face challenges with regard to communicable diseases such as malaria and TB. Large disparities between geographic regions and wealth quintiles in health outcomes remains a major challenge.
3
this context, HIV services remain important components of health service delivery to address overall disease burden and rapidly changing health challenges in Indonesia.
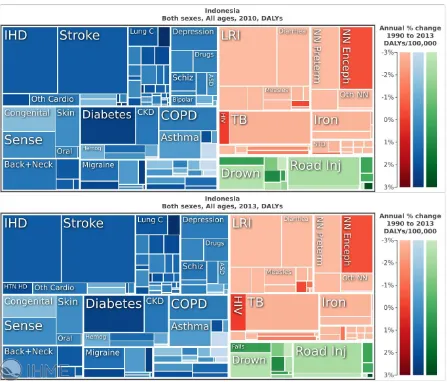
Figure 1: Leading causes of disability-adjusted life years (DALYs) and percent change from 2010 to 2013 for Indonesia
Source: Institute for Health Metrics and Evaluation (IHME), 2015
HIV epidemic in Indonesia
The HIV epidemic in Indonesia is on the rise: adult (15-49) HIV incidence increased from 0.02 in 2000 to 0.06 in 2014 and adult HIV prevalence was estimated at 0.41 % in 2014. Indonesia confronts two very distinct HIV epidemics: a concentrated epidemic among injecting drug users, sex workers, and men-having-sex-with-men outside of Papua, and a low-level generalized epidemic with transmission among vulnerable groups and the general population in the
4
among KAPs in non-Papua regions, the HIV prevalence among adults in Papua was estimated at 2.3 % in 2013, the second highest level of prevalence in the world outside of Africa. In contrast to global trends, the HIV epidemic in Indonesia is growing steadily. Indonesia is one of the few countries that reported an increase in new HIV cases in the 2014 UNAIDS report. The country was also listed as one of the 30 countries (28 low and middle income countries) that contribute 90% of new cases globally.
Figure 2. HIV prevalence estimates by province, 2012
Source: Ministry of Health, 2014
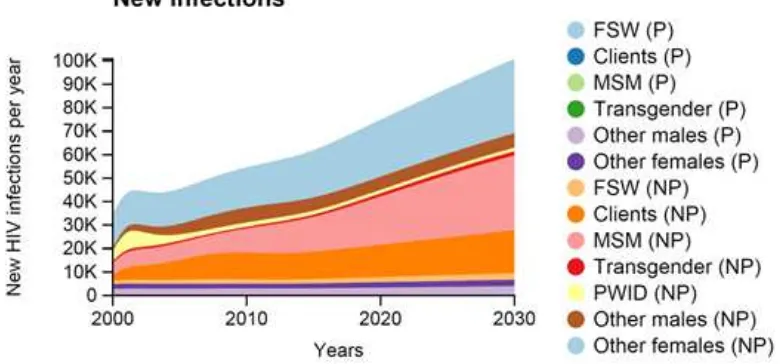
According to the HIV projections using Optima model (Figure 3), the estimated number of new HIV infections has steadily increased over the 10 years since 2000 and it is projected to reach 90,000 new infections by 2030. Much of the increase in new reductions is projected among MSM in non-Papua.
Figure 3: Annual New Infections projected by Optima, 2000-2030
5
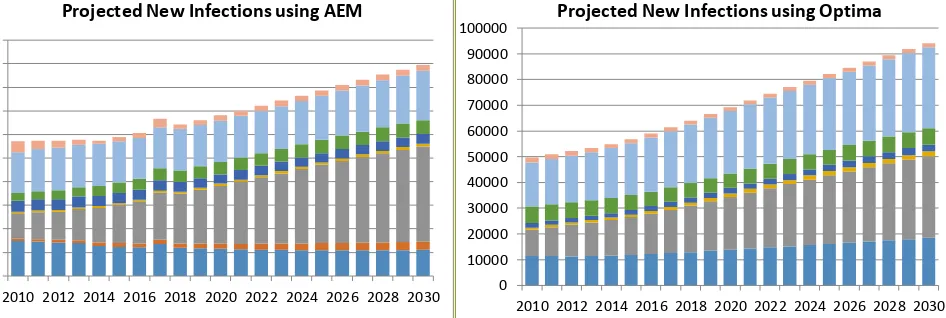
The epidemiological projections from two HIV models (Asian Epidemic Model and Optima) confirmed similar growing epidemic trend with a growing share of new infections MSM. Without increasing intervention effectiveness and program coverages among KAPs, the number of annual new HIV infections is projected to grow significantly from 2000 to 2030.
Figure 4: Projected Number of Annual New Infections, 2010-2030, using AEM and Optima models
National HIV Response
Indonesia’s response to HIV has been supported by domestic political commitment from 2006.
Domestic and international funding has been secured to support a growing national response, and mobilization of domestic resources has increased, albeit slowly and fluctuated, over the
same period of time. In 2014 the Government started the “Strategic Use of ARV (SUFA)
program” to gradually scale up ART to all PLHIV regardless of how advanced their HIV infection. It is expected that treating more HIV infected people will help reduce new infections. At the same
time, the Government has initiated the “comprehensive continuum of care” (Layanan Komprehensif Berkesinambungan - LKB) in several sites, and which will be rolled out to more districts.
Under the SUFA, HIV treatment has expanded and the country has made substantial progress in scaling up ART coverage but there is still a substantial gap in ART coverage. In order to address the ART coverage gap, MOH has developed a roadmap with clear strategies and and
implementation plan for (i) expanding HIV diagnostics, (ii) promoting effective enrolment and retention in HIV care, and (iii) building on the LKB.
Financing for National HIV Response in Indonesia 0
2010 2012 2014 2016 2018 2020 2022 2024 2026 2028 2030
Projected New Infections using AEM
Clients MSW MSM TG FSW Other male Other female PWID 0
2010 2012 2014 2016 2018 2020 2022 2024 2026 2028 2030
Projected New Infections using Optima
6
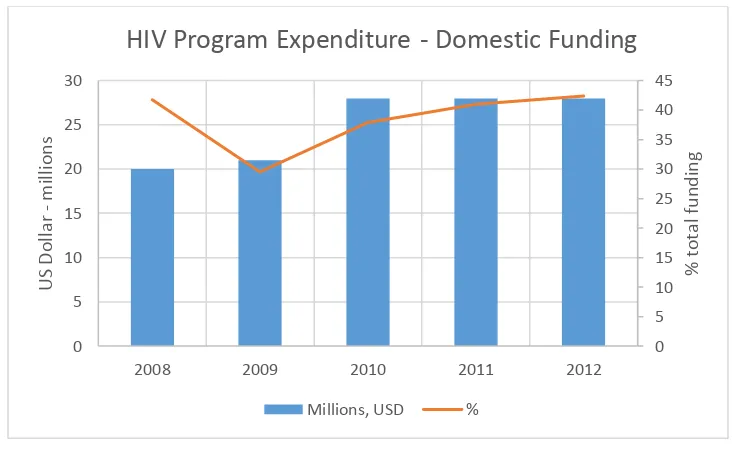
The HIV response in Indonesia has significantly scaled up in the last decade with annual spending increasing more than threefold between US$25 million in 2003 and US$87 million in 2012. Domestic and international funding has been secured to support a growing national response, and mobilization of domestic resources has increased, albeit slowly and fluctuated, over the same period of time. Despite increased domestic funding from USD 15 million (27% of total) in 2006 to USD 28 million (42% of total) in 2012, the HIV response continues to rely on external funding.
Figure 5. HIV program expenditure by sources of funds
Source: NASA 2008 - 2012
Roughly 36% is spent HIV treatment, care and support, and NASA data shows a shift from spending on prevention to spending on treatment and care which reflects the higher number of PLHIV receiving ART.
A role of external funding for health in Indonesia is very limited. On average, roughly 1% of
Indonesia’s total health expenditure over the past several years has come from external sources.
However, this is not the case for HIV, TB, malaria and immunization, where external donors play a major role in financing overall program expenditures. . Externally financed spending for HIV in Indonesia is dominated by three donors – the GFATM, AusAID, and USAID – who together accounted for more than 90% of total international spending in 2011/12 or 58% of total HIV expenditures or US$50.2 million. In 2012, the Global Fund alone funded 28.6% of total national HIV response cost (or ~0.4% of public expenditure on health) in the country.
The share of HIV spending from domestic sources increased from about a quarter of total spending in 2006/07 to about two-fifth in 2011/12. The Central Government was the main contributor (especially the Ministry of Health which finances most of the drug procurement), but sub-national entities – provinces, districts, and municipalities – assumed a more important role
0
HIV Program Expenditure - Domestic Funding
7
in HIV financing in recent years, providing up to one third (2009/10) of the domestic resources for the HIV response. As private spending plays a negligible role in Indonesia the remainder of expenditures
Key Challenges for Indonesia's HIV Response and HIV Financing
Indonesia experiences a concentrated HIV epidemic in different key affcted populations nationwide, but also a low-level generalized epidemic in Papua. How should HIV spending be allocated to take account of this diversity in the epidemiological landscape and to ensure maximal benefit?
With robust economic growth, Indonesia is expected to achieve upper-middle-income status in 2018. The country is expected to increase domestic financing for key programs, including HIV, which are currently largely financed by external partners, and to spend their resources most efficient and sustainable manner as Indonesia will be less eligible for grant support by the Global Fund.
While treatment is financed domestically in large part, Indonesia remains donor dependent with regard to prevention spending. How could the "breathing space" until 2018 be used to invest strategically to install or expand critical strategies and programme elements and to accelerate their roll-out? What should be done to prepare Indonesia's HIV response to be domestically funded in the future?
Programmes for KAPs that are critical to curb further growth of the HIV epidemic are largely delivered by NGOs. What are the possible opportunities for financing and mechanisms for sustaining the programmes for KAPs? Is integration of HIV into the national health insurance program an option for Indonesia to ensure sustainability of HIV response in Indonesia?
Analysis Objectives
The epidemic growth coupled with the expansion of access to ARV will increase financial requirements for HIV programs. To meet these and achieve sustainability, a clear
strategy/transition plan needs to be developed. In support of efficient, effective and sustainable HIV response in Indonesia, two analytical studies were conducted as part of the overall World Bank technical support to the Government of Indonesia: (i) an HIV allocative efficiency analysis and (ii) a financial and programmatic sustainability assessment. The HIV allocative efficiency analysis using Optima3 was conducted to inform the Government with optimal allocations of
3 Optima is a mathematical model of HIV transmission and disease progression, which is integrated with an
8
available HIV resources (with decreasing contribution from Global Fund grant) to achieve maximum HIV and health impact. The results from this study are described in details in a
separate policy note. An assessment of the financial and programmatic sustainability of national HIV program was carried out by the World Bank with its technical partner, the Centre for Health Research University of Indonesia building on the results from the allocative efficiency analysis and costing studies conducted earlier. . The main objective of this analytical work is to provide policy options for integrating HIV programs into the existing National Social Health Insurance (JKN). A central objective was to assess which HIV services might be included in JKN’s basic benefit package and which HIV services were best financed through public health financing means. Results from the two analytical studies will feed into the technical support to improve overall efficiency, financial and programmatic sustainability of the national HIV programs.
Approach
To achieve the approach, consultations were conducted with various stakeholders, including HIV program managers at the national and sub national level, health service providers, and civil society organizations representing key affected population groups. Future costs were projected based on the estimated epidemic trajectories. Cost analysis in this study assessed the baseline cost of current program coverage and calculated the cost of including additional HIV services into the existing benefit package using an actuarial model. Various data sources were used for the cost calculations including a rapid survey of HIV services unit costs, utilization and claims data from the JKN program, NASA data and epidemic projection data from MOH4.
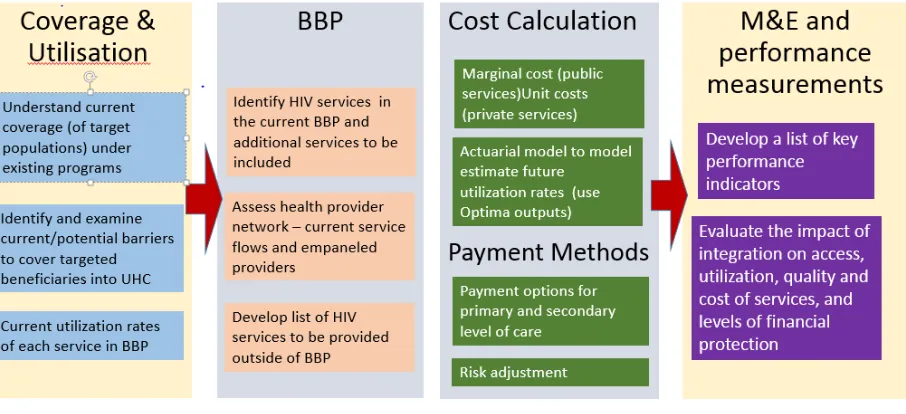
Figure 3. HIV Integration into UHC – Analytical Steps
4 The epidemic projection data was as the results from the joint exercise of Asian Epidemic Model (AEM) and
9
For such an analysis, the Optima model has several potential areas to contribute; The first one is to provide input to development of the actuarial model especially on the course of HIV infection in one individual and in the community, and on the epidemic trajectories. The second is during the priority setting discussion for health insurance basic benefit package, the results of allocative efficiency analysis which assesses cost-effectiveness of HIV services or programs can be used as one of considerations for the decision making.5
Results : Coverage
Availability of HIV services has improved significantly at least in the past five years.
From 2010 to 2013, the number of publicly owned health facilities that provide HIV counselling and testing (HCT) services increased from 385 to 1,391, Needle Syringe Exchange services from 180 to 194, ART services from 195 to 455, and PMTCT services from 29 to 116.
HIV services remain heavily reliant on publicly owned health facilities and these services are mainly provided as vertical interventions rather than as part of an integrated HIV service package.6
The financing of HIV services is fragmented, with one type service often financed by different sources of funding (Annex 1).
Roles and responsibilities are shared across Central and sub-national levels, province and districts, including responsibility for providing funding for HIV services.
Responsibility sharing for one component of service is common, which creates issues in continuity of service. For instance, sub-national levels are responsible for a 55-45% financial share in procuring test kits; but compliance is difficult in the absence of an accountability mechanism.
The extent to which sub-national funding has contributed to the increase of domestic HIV funding is unclear because resource tracking is not systematically done and documented.
Sub-national governments make significant contributions in funding local HIV programs and delivering HIV services. There is anecdotal evidence of significant funding increases in several districts, but in general, local funding for HIV programs remain unreliable.
Overall, the basic benefit package of the JKN program is quite comprehensive for facility-based services. For HIV services it currently covers some HIV essential services, namely some coverage for diagnostic, and treatment and care for opportunistic infection (OI) in both ambulatory and inpatient settings, and sexually transmitted disease management.
5 Criteria for decision making on basic benefit package varies by country/insurance scheme, for instance based on
needs/ necessity, effectiveness, and cost-effectiveness.
10 Instead of a detailed list of services covered (positive list), JKN BBP provides a negative list
of excluded services (Exclusions and Limitations).
The program does not cover services that are financed through general subsidies, donor funds, and the MOH vertical program budget, which means it excludes most of HIV services. Those include HIV prevention services that are provided outside of the facilities through NGOs and community workers such as outreach services.
Currently, harm reduction services for KAPs which are essential for outside of Papua financed under the HIV program budget and are not included in the JKN BBP.
There is an ongoing debate on the inclusion of such services into the BBP as it conflicts with a Government decree that regulates JKN implementation, which excludes substance abuse-related diseases from the BBP.
Results : Proposed Additional HIV Services into Basic Benefit Package
The proposed options for the basic benefit package including HIV services were developed based on three considerations; (i) the disease burden and which are the most essential HIV services need to be included irrespective of the delivery and, funding and payment mechanism for it, (ii) funding source, (iii) who will be managing the funds, and (iv) which service components to include in the BBP.
The cost calculation for these proposed options was based on social health insurance principles which pool risk at the national level, regardless of epidemic situation in parts of the country; for instance the epidemic difference between Papua and outside of Papua.
Option 1 – Comprehensive Clinical HIV Program Coverage
BBP to cover all HIV related services: including counselling, condoms, screening tests (pre-ARV, other basic lab tests), ARV treatment, STI diagnosis and treatment, prevention of mother-to-child transmission (PMTCT) services, and HIV-opportunistic infection services in ambulatory care and inpatient settings. This option does not include outreach activities, public/mass social behavior change activities, and community prevention programs. Within this option, there are 2 financing scenarios:
Financing scenario A: Whole cost of abovementioned services is included (actuarially
calculated) in the premium; and paid by all members. For government-assisted recipients (i.e. the poor) premium contribution will be paid by the Government.
Financing scenario B: Whole cost paid by the Government.
Challenges for Option 1
Integrating existing HIV funding and services which are highly fragmented, for instance financial responsibilities would need to be re-arranged as some services are funded via multiple funding mechanisms;
11 Ensuring adequate incentives for providers to reach out and retain covered target
population especially ARV patients who have a 30% drop out rate currently;
Coordinated planning and budgeting, including synchronized procurement for drugs and supplies for HIV services.
Option 2 – Basic HIV Services
Two variants are considered for the option that would include only Basic Coverage of HIV related services in the JKN BBP:
Scenario 2a – Current Basic Benefit Package (BBP) coverage which covers treatment for OI plus ARV treatment and screening tests
Scenario 2b – Similar to option 2a but excluding ARV treatment; ARV remains provided through Government’s vertical channeling mechanism. This option would be a slight expansion of the existing BBP
This option would be financed by premium contributions and government subsidy for ARV.
All other HIV-related services would continue to be financed by public (domestic) and external financing, continuing to use the current service provision mechanism.
This option is a potential start for an incremental BBP expansion; over time BBP could be expanded to include more HIV services.
Challenges for Option 2
Changes in funding mechanism, especially for ARV,
A clear and realistic roadmap to add HIV services into BBP over time, would need to be developed.
Actuarial calculation were then performed for both options to serve as inputs for the Government decision making process to integrate HIV services into JKN BBP.
Results : Cost calculation
The cost of adding services into the BBP is an important consideration in the decision making process. The cost to include HIV services into JKN BBP is projected for the next five years using 2014 costs as the baseline. The first step is to summarize the cost of the HIV service package and produce cost estimates per member per month (Cost PMPM)7. The probability of use of HIV services is derived from service utilization and membership data from the JKN carrier (BPJS) (see Annex 2).8
7 The analysis produces Cost per member per month (Cost PMPM) instead of premium per member per month
(Premium PMPM) in which the latter has included loading factor (administration cost)
8 The Government has requested the WB and CHR UI team to project the costs of both Option 2 scenarios as they
12
Comprehensive coverage (option 1) would mean an additional charge per member of
approximately IDR 558 per month or IDR 6,696 (equivalent to USD 0.6) per year9. This includes the HIV-related services of counseling and HIV testing, STI lab test, STI treatment, diagnostic test for pre ARV, ARV treatment, side effect treatment and PMTCT. Current JKN basic premium is IDR 19,225 per month, and additional HIV services would mean an additional of around 3 % to the premium cost.
The additional cost per person for basic options (Option #2) that includes ART is estimated at IDR 467 per month, while for the scenario that maintains ART provision through current channeling mechanism (Model 2B) would add IDR 317 to the current premium. The additional services will increase for 2.4% and 1.6% for coverage model 2A and 2B respectively.
The cost projection for 2015 – 2019 uses the 2014 inflation rate of four percent, and the 2014 utilization rate as the basis (Annex 4). Assumptions were carefully developed through several consultative meetings with the HIV-UHC Working Group (Pokja BPJS – HIV), for instance to identify factors influencing the use of services in the context of the national strategic responses, such as expansion of ARV (SUFA) and the comprehensive continuum of care (LKB).
Cost projections for the comprehensive coverage suggests that the 2019 premium (around IDR 1,200 per member per month) would need to be double the 2014 amount (see Annex 4). Meanwhile for the basic options the costs will increase to IDR 1,000 and IDR 811, for the scenario with ART and without ART, respectively. This higher rate considers the government’s plans to extend the VCT program to include condom provision. Providing condoms along with counseling would be the main driver of the increase in Cost PMPM in 2019. Other service components have much less effect requiring only a slight increase in PMPM over the years.
Results: Provider payment mechanism options
Provider payment systems should be selected to help achieve health policy objectives by encouraging providers to offer necessary health services, ensure quality of care, and reduce inequity, while promoting the effective and efficient use of resources and, where appropriate, cost containment.10
The provider payment method in the JKN scheme is regulated through a ministerial decree in which three payment mechanisms are specified. They are (i) capitation, (ii) non-capitation, and (iii) a diagnostic related group called INA-CBGs (Indonesia Case-based Groups). Capitation payment is a periodic (monthly) scheme for primary care (FKTP) providers, based on the number
9 Current JKN basic premium is IDR 19,225 per month (this is for the government fully subsidized premium, third
class ward bed facility), while for voluntary members the premium ranges from IDR 25,500 to 59,500 pmpm depending on amenity class of care selected, Third class ward to First class ward respectively. In this exercise, the
calculation of cost per member per month used the ‘basic’ premium (similar to the government subsidized premium
program). The same applies for Option 2.
10 Langenbrunner, John C.; Cashin, Cheryl; O’Dougherty, Sheila. 2009. Designing and Implementing Health Care
Provider Payment Systems: How-To Manuals. Washington, DC: World Bank. © World Bank.
13
of registered members regardless of type and amount of services given. INA-CBGs payment, based on a case-mix and diagnostic related group, is prospective payment to secondary level providers of both ambulatory and inpatient services at hospitals (FKRTL). Aside from the two bundling schemes to pay providers, non-capitation and non-INA CBGs payment are also allowed. Non-capitation payment is basically a payment claim for each service rendered. This claim comes from the primary level of care for inpatient services (Primary Health Center with beds). Non-INA CBGs payment is payment made to FKRTL for services provided using different payment system (top-up) based on MOH regulation.
Proposed benefit package for HIV consists of both inpatient and outpatient services. For OI inpatient care, which is currently already covered by JKN scheme, providers are paid using INA CBG. The most appropriate payment mechanism for the other HIV care services need to be thought through carefully, as prospective payment might not be the right choice for some services. For example, capitation might not be appropriate for some HIV services as HIV is a rare occurrence, especially in regions with a low level epidemic, and requires chronic and lifelong treatment while the cost tends to be high. Capitation payment also has weak incentives to providers to do outreach and preventive measures. Non capitation could be considered as an option for services such as ambulance service; drugs service on counter-referral program; additional tests of counter-referral program (program rujukan balik); and specialized health screening service.
The proposed payment mechanisms for different types of HIV service can be found in Annex 5.
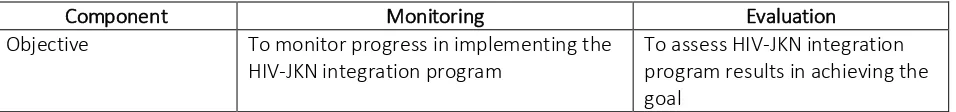
Monitoring and Evaluation of the Implementation of HIV-JKN Integration in Indonesia
The monitoring and evaluation of the JKN implementation of including HIV services into its BBP has the following objectives:
1. Monitor progress in implementing the HIV-JKN integration program.
2. Identify gaps in delivering the agreed service package to targeted beneficiaries.
3. Review the impact of the HIV-JKN integration program on:
a. Access of target beneficiaries to HIV and AIDS services
b. Quality of medical/non-medical services and cost of HIV and AIDS services
c. Level of financial protection for targeted beneficiaries.
Table 1. Monitoring and Evaluation of HIV-JKN Integration Program
Component Monitoring Evaluation
Objective To monitor progress in implementing the
HIV-JKN integration program
14
Focus Inputs, process, and some outputs Identification of program impact
Time Routine and continuous Periodic
Data collection process Routine reports, observation and field-visits
Pre-post test observation
Data Source SIM BPJS Kesehatan, audit, and
spot-check
Baseline survey (existing data) and follow-up surveys Implementing Agency BPJS and External (DJSN and NAC) External (DJSN, NAC,
Universities)
Performance Assessed Program implementation improvement Evaluation of results achieved, premium calculation, etc.
Conclusions and recommendations
1. HIV UHC integration can be done for reasonable costs. Option 2 will results in around 2% increase in premium cost, while Option 1 will increase 3% of the current premium. 2. The integration of HIV services into the national social health insurance scheme requires a
comprehensive approach as it includes changes beyond transitioning funding mechanisms. The integration into JKN will affect service delivery, program management, and the
dynamics among players (organizational arrangement). There should be a concerted effort to ensure that existing regulations support the targeted beneficiaries, KAPs, in enrolling as members of the health insurance program and receiving the program’s benefit (enabling environment). The preparedness of the supply side in the JKN provider network to deliver additional services in the BBP needs to be ensured and needs to be in line with the Government strategy to provide comprehensive HIV service (LKB) and expand access to ARV (SUFA). Institutional arrangements relating to division of roles and responsibilities among the sub national levels and also among other Government agencies at the Central level need to be considered (or accommodated).
3. But, it is complicated and some aspects may never be able to be fully integrated. Although HIV/AIDS services are comparable with those for other chronic conditions, they have specific characteristics such as the sensitivity of services due to social stigmatization of HIV, and the population groups most at risk and HIV key affected populations. This specificity needs to be taken into account in making the final decision on which services to include in the BBP and how the BBP would change overtime. Also, careful decisions are needed on the most appropriate funding channels and provider payment mechanism/s to ensure sustainable and affordable services. Even if not all HIV services are eventually integrated into the JKN, linkages and referrals between services should be strengthened so that, from a client perspective, a seamless service is provided.
15
and responsibilities of each player, also in stating its goals and milestones. The roadmap also needs to be realistic in taking into account the current and projected epidemic situation, and the capacity to deliver service.
5. The highly participatory decision making process, involving various stakeholders including other relevant ministries, sub national governments, providers, and representatives from civil society, should be maintained.
6. HIV-UHC integration is only part of the answer in terms of improving HIV program
sustainability. The integration of HIV services into JKN should be considered as part of the
effort to develop the country’s transition plan from external donor dependency to ensure
16
Annex 1. Financing of HIV Services
Interventions Service Component
Service elements Current Coverage/Funding mechanism
Prevention STI services Diagnostic : STI tests JKN and Public Financing
Drugs JKN and Public Financing
Condom and lubricant Public - Domestic and External
IEC materials Public - Domestic and External
Consultation (Medical and Lab
Tech fee)
JKN and Public Financing
HIV Counseling and
Testing
Diagnostic tests Public financing - Central & Sub National
Condoms Public - Domestic and External
Consultation JKN and Public Financing
Harm Reduction NSP Public - Domestic and External
MMT Public financing
Condoms Public – Domestic and External
Consultation fee Public Financing
PMTCT Diagnostic tests Public financing - Central & Sub National
Condoms Public - Domestic and External
ARV Public - Domestic and External
C-section Public - Domestic and External
IEC materials Public - Domestic and External
Consultation fee JKN and Public Financing
Treatment
and Care
Treatment and Care Screening tests: ARV eligibility Public financing - Central & Sub National
Prophylaxis drugs Public - Domestic and External
ARV Public - Domestic and External
Monitoring tests : CD4 & VL Public - Domestic and External
OI Hospitalization JKN
OI Drugs JKN and Public Financing
Condoms Public - Domestic and External
Consultation (Medical and Lab
Technician fee
17
Annex 2. Key Affected Population size estimates - Targeted beneficiaries
2014 2015 2016 2017 2018 2019 2020
Total Population (all) 252,073,120 255,461,700 265,499,840 275,537,980 285,576,120 295,614,260 305,652,400
JKN Members (Roadmap Target) 15% 39% 60% 83% 90% 100% 100%
JKN Members (Current & Projection) 135,700,000 228,696,523 257,018,508 295,614,260 305,652,400
Key Affected Population (15+)
KAP Total 8,577,964 8,694,356 8,809,579 8,924,000 9,037,279 9,148,556 9,257,543
Total Population (15+) 184,131,232 186,583,955 189,037,263 191,482,978 193,902,756 196,280,239 198,609,853
PLHIV Population
Total KAP PLHIV 272,153 282,353 293,170 304,853 317,522 331,195 345,842
Total PLHIV 649,884 679,736 708,048 735,297 761,786 787,795
18
Annex 3 Summary of the Premium PMPM 2014
Baseline Option 1
19
Annex 4. Cost Projection 2015-2019
Option 1
Option 2
2014 2015 2016 2017 2018 2019
20
Annex 5. Provider Payment Mechanisms
No
Strength Weakness for the Proposed Method
1 Counseling and pre-ARV test (Viral Load and CD4).
Capitation Fee-for-service – Encourage provider
to provide services. – More appropriate to
recurrent HIV service.
May encourage unnecessary service (FFS), and as BPJS only uses prospective
payment, Capitation has to equipped with additional incentive mechanism such as additional performance-based bonus 2 Basic laboratory test for
ARV therapy (test on liver, kidney, and heart function and TB test).
Fee-for-service Encourage provider to provide services.
Multiple (un necessary) tests
3 STI laboratory test. FFS/Out of pocket INA-CBGs INA-CBG code is
available.
Only if the service is included in the service package as it is calculated as a case based group; this doesn’t allow separate payment mechanism.
INA-CBGs INA-CBGs INA-CBG code is
available.
Level of payment doesn’t necessarily reflect actual costs
INA-CBGs INA-CBGs INA-CBG code is
available.
Level of payment doesn’t necessarily reflect actual costs
DRG ‘Creep up’
Multiple un necessary admission 7 Condom provision and
counseling/education service at health facility.
Fee-for-service Encourage provider to provide services.