Carotid-Cavernous Fistula :A Case Report
I Komang Oka Krishna1, I Wayan Niryana2, Putu Patriawan3
1Departement of General Surgery, School of Medicine, University of Udayana, Bali
2
Department of Neurosurgery, Neurovascular Division, School of Medicine, University of Udayana, Bali 3
Departement of Radiology, Interventional Radiology Division, School of Medicine, University of Udayana, Bali
Abstract
Introduction. We present a case of direct carotid-cavernous fistula (CCF). Direct carotid-cavernous fistula are high-flow shunts with a direct connection between the internal carotid artery and the cavernous sinus. The goals of treatment are to eliminate the fistula and preserve carotid artery patency
Presentation of Case: A 19-year-old female presented with left eye discomfort, increasingly edema of tarsal conjunctiva, pulsatile tinnitus and progressive visual loss on the left eye.She had a recent history of moderate head injury and maxillofacial fracture. Examination showed proptosis, chemosis and orbital bruit. Digital subtraction angiography confirmed CCF, which was managed endovascularly. The patient recovered after treatment with visual loss on her left eye.
Discussion. CCF has a variety of presenting clinical signs, imaging manifestations, and treatment options available. Early diagnosis and prompt treatment to prevent loss of visual function in patients with CCF.
Conclusion. CCF is a rare and dangerous neurological disorder that should be promptly diagnosed and treated.
Keyword :carotid-cavernous fistula, endovascular treatment, visual loss
Corresponding author:
I Komang Oka Krishna
Address :Departement of Surgery, General Sanglah Hospital JalanDiponegoro Denpasar Bali ( 80114 )
Ph0361 227911 Mobile : 081338158989
Introduction fistulas usually are of the high flow t they are called direct carotid-cavernous with miniplate. In the interval of one pulsatile tinnitus and progressive vis
fistula (CCF) are high-flow shunts with a direct connec avernous sinus. CCF is a rare sight and lifethreatening s. spontaneous), velocity of blood flow (high vs. low flo s. external carotid vs. both). Some fistulas are charac us segment of the internal carotid artery and the cavern
w type. Most often caused by a single, traumatic tear i ernous sinus fistulas. Other CCFs are dural. Many of ous malformations that develop spontaneously, often
tension, connective tissue disease, and during or after consist of a communication between the cavernous internal carotid artery, the external carotid artery, or bo
l blood flow. The goals of treatment are to eliminate
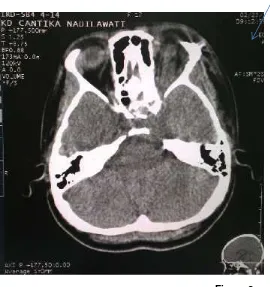
Figure 2
Head CT scan showing dilated left superior ophthalmic vein.
Figure 3
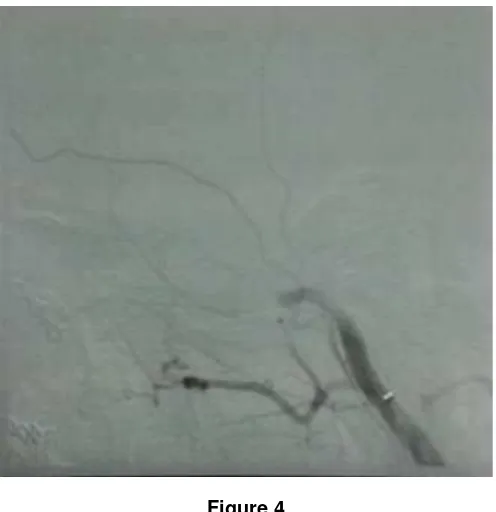
Figure 4
Post ballooning embolization showing complete obliteration of the CCF
Figure 5
This figure shows the status of the patient three month after ballooning embolization with great improvement
Discussion
The complexity of carotid cavernous fistulas (CCF) is a result of their location within the unique anatomical structure of the body where an artery crosses a venous structure. Through the superior and inferior ophthalmic veins the cavernous sinus receives venous blood that is drained via the sphenoparietal sinus, superior petrosal sinus, basilar plexus and pterygoid plexus. When passing through the foramen lacerum the internal carotid enters into the cavernous sinus and in the posterior wall it is divided into three segments: 1) posterior ascending segment, 2) horizontal segment, the largest segment of the intracavernous carotid, 3) superior ascendant segment.1,2
arteriovenousfistula between the meningeal branches in the dura and the cavernous sinus. A clinically useful classification is the anatomical-angiographic classification by Barrow et al. and is based on the communication between the carotid artery, its branches and the cavernous sinus in which fistulas are divided in four types.2,3
Up to 76% of CCFs are traumatic caused by severe injuries such as vehicle accidents or penetrating traumas. CCFs are seen in 0.2-0.3 % of craniofacial trauma2,3,4Direct fistulas are the most common and are caused by trauma in 70 to 90% of the time, mainly basilar skull fracture. They occur more often in young adult men because of their higher involvement in accidents .They can also be iatrogenic (rhinoseptoplasties, endoscopic sinonasal surgeries, transsphenoidalhypophysectomy) or spontaneous by aneurysm rupture in the cavernous portion of the carotid or congenital malformation that break spontaneously due to vascular disease linked to collagen (e.g. Ehlers-Danlos syndrome, atheromatous disease or hypertension). Spontaneous fistulas have a higher incidence in post-menopausal women, with no predominance in a particular When compared to dural fistula, the size of direct lacerations direct fistula is proportionally greater and determines the difference of the endovascular treatment between them3,4.
Direct CCFs have a different hemodynamic change compared to the dural fistulas. After the establishment of the arteriovenous fistula the blood pressure and flow are transmitted to the cavernous sinus. This causes reverse flow and venous dilation of the veins that drain into the sinus, as well as an increased flow in their usual draining veins. When they reverse their venous flow the ophthalmic veins cause engorgement and orbital congestion that prevents drainage of the aqueous humor and increases intraocular pressure and secondary glaucoma. The elevated intraocular pressure may compromise retina perfusion and result in decreased visual acuity, a surgical emergency. Eye oedema resulting from the impairment of venous drainage may lead to mechanical limitations of the extraocular muscles which may already have their function compromised by compression on the cranial nerves3,5,6
The intercavernous sinuses can transmit the same hemodynamic changes, to the other side resulting in a similar clinical picture. The result of blood flow reversal and increased venous pressure in the ophthalmic veins can result in exophthalmos, ophthalmic fremitus, chemosis, proptosis, and diplopia. Loss of vision occurs in about 90% of direct CCFs and 20 to 30% of indirect CCFs.Glaucoma and retinal perforation are symptoms of direct CCF and may appear days or weeks after the TBI. Ischemia involving cranial nerves III, IV, V and VI may be premature and evident due to mass effect on the cavernous sinus. This is different from the indirect CCF that has slow evolution and usually manifests with ocular hyperaemia and tortuous arterializations of the conjunctiva, without proptosis. After angiography 20 to 50% of indirect fistulas close spontaneously7
The patient’s history and the clinical examination often point to the diagnosis: a direct CCF is suspected in every patient with a painful red eye, chemosis , exophthalmia and orbital bruit, especially after a previous head trauma.2,3,4The gold standard complementary diagnostic method is the selective digital arteriography of the carotid artery. This exam shows the size and estimates the damage of the fistula. The tests that have a complementary role in diagnosis are magnetic resonance, computed tomography angiography and Transcranial Doppler7,8.
The differential diagnosis should include posterior scleritis, endocrine exophthalmia, idiopathic inflammation of the orbit, retrobulbar bleeding, cavernous sinus thrombosis, malignancyof the orbit and arteriovenous malformations of the orbit/cavernous sinus.8,9,10To ensure proper diagnosis we emphasize the importance of multidisciplinary examination of the eye function and periorbital condition.
Treatment of a direct CCF is mandatory for immediate orbital symptom relief and to prevent the development of intracranial venous hypertension. Most direct CCFs can be treated electively,urgent treatment is necessary only in patients with progressive visual loss, corneal exposure, severe proptosis with pain and high intraocular pressure, intolerable bruit, epistaxis, sphenoid sinus aneurysm, severe retro-orbital pain, cortical venous drainage or coma 1,2,4,11 Carotid Cavernous Fistula treatment has become more effective, safer and less invasive with the advent of new neuroimaging techniques When the fistula is small and asymptomatic, further treatment is not indicated.4
device to the venous site of the fistula, where the balloon is then inflated and detached in situ. A complete obliteration can be achieved in 80-90% of all direct CCFs. The carotid artery blood flow can be preserved in up to 75% of patients 4,11,12The size of the cavernous sinus and of the fistula may affect the success rate of the procedure. When the size of the fistula is too large or incompatible with the size of the balloon, the use of electrodetachable coils decreases the size of the hole allowing for the occlusion of the remaining fistula.13. Radiological examination of the skull is necessary after embolization to control the location of the balloon. In select cases, open surgery, radiosurgery, or conservative management are also treatment options. Symptom resolution with low rates of recurrence can be expected in most cases after appropriate therapy.1,2
Liang found significant differences between the time of the first symptoms and embolization by comparing groups with and without complications3. Collaborating that with early detection and immediate intervention it is possible to accomplish full visual recovery with proper treatment8,11,12. Intravenous treatment has been recommended for indirect CCF. This is a safer treatment with less arterial thrombotic events, lower rate of treatment failure and easier implementation. The most common complications observed in the treatment of CCF by embolization are the migration of the balloon, formation of a false aneurysm, on the internal carotid (which usually recedes spontaneously), perforation of the superior ophthalmic vein, orbital haemorrhage and injury of the abducens and trochlear nerves. Post treatment recurrences and deaths have been reported10.
After successful occlusion of the CCF, the orbital symptoms gradually disappear, and in the presence of elevated ocular pressure, resolution to normal intraocular pressure within 72 hours can be expected. In some cases intraocular pressure normalization needs several months. The orbital congestion resolves usually after several weeks, reconstitution of cranial nerve function may lag several weeks (19). Diploplia almost always improves but in some cases, operative shortening of the lateral rectus muscle may be necessary8,10When the CCF is left untreated, vision is eventually lost in 89% of patients. In 1981, before the use of intra-arterial procedures, reported progressive visual loss in 28% of patients, even with carotid artery surgery.14More recently, visual acuity was preserved or improved in 94% of cases after treatment with detachable balloons in patients with preoperative visual loss. There are only some case reports of reversal of blindness after endovascular treatment.10,11
Conclusion
CCF is a rare and dangerous neurological disorder that should be promptly diagnosed and treated. Although rare, CCF is a serious complication that should be considered in the differential diagnosis of ocular proptosis and visual loss associated with maxillofacial trauma. Cerebral angiography is the gold standard imaging modality used in the diagnosis and classification of CCF. Although historically difficult to treat, these lesions are now routinely managed with low rates of morbidity and mortality. Endovascular intervention with a goal of complete fistula occlusion while preserving normal blood flow through the internal carotid artery has emerged as the treatment of choice. In select cases, open surgery, radiosurgery, or conservative management are also treatment options. Symptom resolution with low rates of recurrence can be expected in most cases after appropriate therapy.
References
1. Ellis JA, Goldstein H, Connoly ES, Meyers PM. Carotid-cavernous fistulas.Neurosurg
Focus,2012, 32(5)
2. Miller NR. Dural Carotid-Cavernous Fistulas: Epidemiology, Clinical Presentation, and
Management.Neurosurgclin N Am.2012,23 :179-192
3. Liang W, Xiaofeng Y, Weiguo L, Wusi Q, Gang S, Xuesheng Z. Traumatic carotid cavernous fistula accompanying basilar skull fracture: a study on the incidence of traumatic carotid cavernous fistula in the patients with basilar skull fracture and the prognostic analysis about traumatic carotid cavernous fistula. J Trauma. 2007, 63 (5): 1014-1020.
4. Naesens R, Mestdagh C, Breemersch M, Defreyne L. Direct carotid-cavernous fistula: a case report and review of the literature. Bulletin de la SocieteBelgedOphtalmologie 2006:43–54.5. 5. Martin S, TeoM, Bhattacharya JAlakandy L.Carotico-cavernous fistula: An educational case
International Journal of Surgery Case Reports, 2013 (4): 858– 860
6. Guimares AC, de Carvalho GM, Chone CT, Pfeilsticker LN. Carotid cavernous fistula: A rare complication of maxillofacial trauma. Head Neck Oncol, 2014 10;6(3):23.
7. Cheng JW, Wei RL, Cai JP, Zhu H, Li Y. Imaging diagnosis of carotid-cavernousfistula. Zhonghua
Yan KeZaZhi 2007;43:36–94
8. Charlin RE, Pacheco PB, Villarroel FW, Urbina FA. Carotid cavernous fistula: the importance of its opportune diagnosis and treatment to prevent blindness. Rev Med Chil. 2004, 132(10):1221-1226.
9. Karaman E, Isildak H, Haciyev Y, Kaytaz A, Enver O. Carotid-cavernous fistula after functional endoscopic sinus surgery. J Craniofac Surg. 2009, 20(2):556-558.
10. Yang ZJ, Li HW, Wu LG, Zheng JN, Zhang JD, Shi XW, Chu GR. Prognostic analysis and complications of traumatic carotid cavernous fistulas after treatment with detachable balloon and/or coil embolization. Chin J Traumatol. 2004, 7(5):286-288.
11. Tjoumakaris SI, Jabbour PM, Rosenwasser RH. Neuroendovascular management of carotid cavernous fistulae. NeurosurgClin N Am 2009;20:447–52.
12. Lo D, Vallee JN, Bitar A, Guillevin R, Lejean L, Van Effenterre R, Chiras J. Endovascular management of carotid-cavernous fistula combined with ipsilateral internal carotid artery occlusion due to gunshot: contra-lateral arterial approach. ActaNeurochir. 2004, 146:403-406 13. Sawlani V, Phadke R, Kumar S, Gujral RB. Gugliemi detachable coils in the treatment of
carotid-cavernous fistula. Clinradiol. 2004, 59:86-90