Abstract
Objective: measure carotid intima-medial thickness (CImt), its variability, risk factors, their correlation, in type 2 diabetic (Dm), pre-diabetic (PDm) and non-diabetic (NDm) acute strokes.
Methods: twenty four Dm and a matched population of 14 patients each of PDm and NDm strokes were studied. each group was compared as whole and by gender and stroke segregation. study parameters were right and left CImts (CImtr, CImtL), insulin resistance (Ir), age, bmI and lipids, correlations between CImts and CImts with risk markers.
Results: CImtr was higher in Dm and PDm compared to NDm, but CImtLs did not differ. CImts were similar in genders and stroke types of each group. the Ir was significantly high only in Dm. Age and bmI correlations were predominantly positive and lipids variable except in PDm. Age and Ir had better impacts on CImts in Dm while bmI was poor. Females and infarcts had a more congruous CImt increment in Dm and PDm but male and haemorrhage in NDm.
Conclusion: With similar levels of risk markers, their impacts on the CImts are highly variable at various levels of glycaemia. CImts were similar in the genders and stroke types of each group, irrespective of the glycemic status. the pre-diabetes group had distinct features.
*Nrs medical College, Kolkata, West bengal; **VIms, Kolkata, West bengal, ***bs medical College bankura, ****srichitra Institute ms, trivandrum
received: 14.02.2011; Accepted: 24.08.2011
Introduction
s
troke in diabetes, has a two to four fold increase in its relative risk compared to non diabetics.1,2 this is evident across multiple racial and geographic groups.3 there is relative increase in ischemic stroke; hemorrhagic stroke is probably not increased.4 Atheroma develops faster in diabetes; thickening of the intima is an early change.5 Carotid intima-media thickness (CImt), determined non-invasively by high resolution ultrasound (UsG) imaging, has been widely used as a surrogate for atherosclerosis.6 type 2 diabetes mellitus (t2Dm) patients often have higher CImt values than the general population.7 Whether this elevated CImt predicts future vascular events independent of conventional vascular risk factors is not clear.8 Incident CImt aswell as its rate of change depends on many factors.9
Increased CImt in t2Dm is associated with known risk factors like increasing duration, age, male gender, altered lipids, increased body mass index (bmI), and markers of inflammation.10-12 Adverse lipid ratios, smoking, insulin resistance and homocystienemia have also been positively correlated with CImt.9-11 In non diabetics, established risk factors like age, sex, bmI and dyslipidemias are associated with increased CImt in a graded manner.2
studies are many in relation to coronary vascular disease, but studies that assess the incident CImt in acute stroke in t2Dm vis-à-vis other conventional vascular risk markers and compare with prediabetic and non-diabetic strokes are few.1,6,7,12,13 this study was planned to assess (1) status of the incident CImts and conventional risk markers in type 2 diabetic (Dm), prediabetic (PDm) and non diabetic (NDm) acute strokes (both infarct and haemorrhage), (2) the relation of the two (right and left) side CImts and their correlations with the incident risk markers.
Methods
Consecutive patients of stroke in known t2Dm patients (HbA1c > 6.5) were initially enrolled from the in-patient department of NRS Medical College, who satisfied the inclusion and exclusion criteria between June 2009 and January 2010.14 An age, bmI, gender ratio and matched patients NDm (HbA1c < 5.7) and PDm (impaired fasting glucose and or impaired glucose tolerance with HbA1c between 5.7 and 6.5) stroke types were selected of from same inpatient department, between February 2010 and August 2010 for comparing relevant parameters and act as controls.14 stroke was established according to the World Health Organisation definition—“a focal neurological impairment of sudden onset, and lasting more than 24 hours (or leading to death), and of presumed vascular origin”-- from the history, clinical signs and Ct scan of brain (establishing vascular event).
Non-Diabetic Acute Stroke
Uday Sankar Ghosh
*, Partha Chattopadhyay
*, Samar Banerjee
**, Madan Karmakar
***,
Suchit Majumder
****Table 1 : Comparative analysis of the clinico-biochemical parameters of diabetic, prediabetic and non diabetic strokes Stroke Type Age(yrs) Sex- Male
(%)
BMI (kg/m2) Infarct %
Dm n=25 60.3±10.34 68% 25.1±3.9 60
PDm n=14 61.4±8.5 64.3 26.1±3.8 64.3
NDm n=14 60.1±8.7 51.78 25.8±2.2 57.1
Dm vs PDm p=0.75 p=0.82 p=0.34 p=0.8
Dm vs NDm p=0.97 p=0.51 p=0.52 p=0.87
PDm vs NDm
p=0.72 p=0.71 p=0.66 p=0.71
stroke type tC(mg/dl) tG(mg/dl) HD(mg/dl) LD(mg/dl) Dm n=25 176.8±26.4 154.4±52.7 39.1±7.3 130.2±25.9 PDm n=14 17.2±41.8 137.9±43.8 38.2±6.3 113.9±45.7 NDm n=14 187.6±42.6 164.5±69 45.8±11.8 120.1±39.9
Dm vs PDm p=0.62 p=0.34 p=0.72 p=0.17
Dm vs NDm p=0.35 p=0.62 p=0.04* p=0.35 PDm vs
NDm
p=0.33 p=0.25 p=0.05* p=0.71
stroke type Ir n-HC(mg/dl) Ctr(mm) CtL(mm) Dm n=25 3.29±2.2 137.8±28.6 0.88±0.16 0.96±0.24 PDm n=14 1.69±1.2 133±41.3 0.88±0.17 0.87±0.15 NDm n=14 1.04±0.7 141.9±46.3 0.76±0.07 0.83±0.1 Dm vs PDm p=0.017* p=0.68 p=0.99 p=0.24 Dm vs NDm p=0.0007* p=0.74 p=0.016* p=0.07 PDm vs
NDm
p=0.09 p=0.61 p=0.04* p=0.42
Dm- diabetic stroke, PDm prediabetic stroke, NDm- non diabetic stroke, yrs- years, bmI- body mass index, tC- total cholesterol, tG- triglyceride, HD- HDL cholesterol, LD- LDL cholesterol, Ir- insulin resistance level, n-HC- non HDL cholesterol, Ctr- carotid intimo-medial thickness of the right side, CtL- carotid intimo-medial thickness of the left side, vs- versus, p- p value of t test, n- number of patients, * = significant p value.
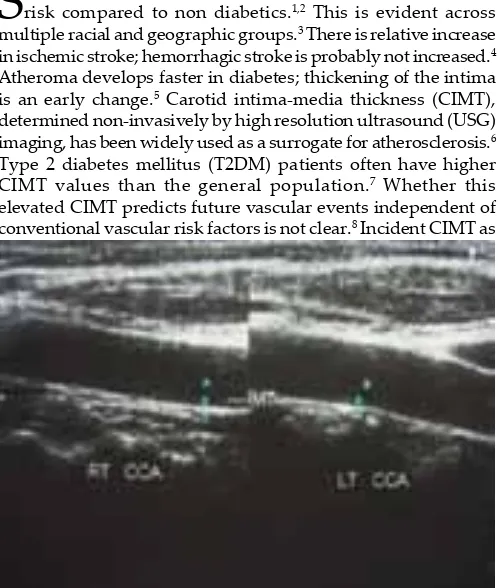
Fig. 2 : Carotid doppler at the level of carotid bulb
Fig. 3 : Carotid intima-media thickness measurement at the level of carotid bulb (IMT-BULB)
Fig. 4 : Carotid intima-media thickness measurement at the level of common carotid artery (IMT-CCA) and internal carotid artery
(IMT-ICA)
Parameters studied included – age, gender, bmI, serum cholesterol (tC), serum triglyceride (tG), LDL-cholesterol (LD) and non HDL-cholesterol (n-HC), HDL-cholesterol (HD), Insulin resistance level (Ir) and CImt of the right (CImtr) and left (CImtL) carotids (Figures 1, 2, 3, 4). Initially the status of the parameters were compared between the three major (Dm, PDm, NDm) groups (table 1). then, each major group was segregated by stroke types (infarct and haemorrhage) and by gender (tables 2 and 3), and again compared. the CImtr and CIMTL correlation status and mean difference is depicted in table 4 and the correlation of the risk factors with the CImts in tables 5 and 6.
Patients who survived for three days post hospitalisation were studied as performing the CImt measurements were not possible before that duration as well as a repeat Ct scan to establish infarct in certain cases. exclusion criteria included previous documented vascular event, renal failure, known secondary or severe hypertension, subarachnoid haemorrhage, intra cranial arteriovenous malformations, valvular heart disease, AV block, atrial fibrillation and patients on drugs that might modify the CImts (statins, aspirin, ACe inhibitors and Angiotensin receptor blockers).12,13,15 serum for biochemical analysis were collected after 6-8 hours of fasting (without insulin) after the last feed and stored if required, as longer fasting and/or delay in therapeutic interventions was not permitted by the ethical committee.
CImt was measured by high resolution UsG machine (made by m/s HP make, marketed by Agilent, model Image point HX) of carotid arteries with the patient in supine position and the neck being slightly extended and rotated towards the opposite
side, with 5 -10 mHz linear array transducer.6 All measurements were performed by manual planometry by asingle operator, who was blinded about the glycemic status of the subjects.
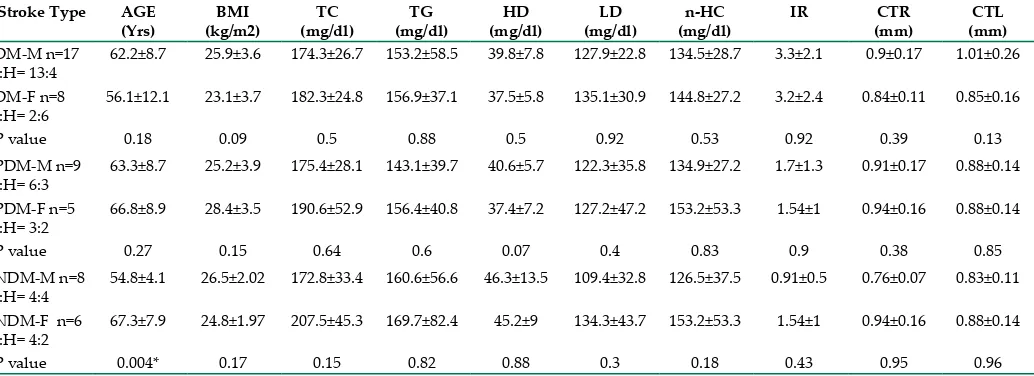
Table 3 : Intra group comparative analysis of the clinico-biochemical parameters of males and females of the diabetic, prediabetic and non diabetic strokes
Stroke Type AGE (Yrs)
BMI (kg/m2)
TC (mg/dl)
TG (mg/dl)
HD (mg/dl)
LD (mg/dl)
n-HC (mg/dl)
IR CTR
(mm)
CTL (mm) Dm-m n=17
I:H= 13:4
62.2±8.7 25.9±3.6 174.3±26.7 153.2±58.5 39.8±7.8 127.9±22.8 134.5±28.7 3.3±2.1 0.9±0.17 1.01±0.26
Dm-F n=8 I:H= 2:6
56.1±12.1 23.1±3.7 182.3±24.8 156.9±37.1 37.5±5.8 135.1±30.9 144.8±27.2 3.2±2.4 0.84±0.11 0.85±0.16
P value 0.18 0.09 0.5 0.88 0.5 0.92 0.53 0.92 0.39 0.13
PDm-m n=9 I:H= 6:3
63.3±8.7 25.2±3.9 175.4±28.1 143.1±39.7 40.6±5.7 122.3±35.8 134.9±27.2 1.7±1.3 0.91±0.17 0.88±0.14
PDm-F n=5 I:H= 3:2
66.8±8.9 28.4±3.5 190.6±52.9 156.4±40.8 37.4±7.2 127.2±47.2 153.2±53.3 1.54±1 0.94±0.16 0.88±0.14
P value 0.27 0.15 0.64 0.6 0.07 0.4 0.83 0.9 0.38 0.85
NDm-m n=8 I:H= 4:4
54.8±4.1 26.5±2.02 172.8±33.4 160.6±56.6 46.3±13.5 109.4±32.8 126.5±37.5 0.91±0.5 0.76±0.07 0.83±0.11
NDm-F n=6 I:H= 4:2
67.3±7.9 24.8±1.97 207.5±45.3 169.7±82.4 45.2±9 134.3±43.7 153.2±53.3 1.54±1 0.94±0.16 0.88±0.14
P value 0.004* 0.17 0.15 0.82 0.88 0.3 0.18 0.43 0.95 0.96
Dm- diabetic stroke, PDm prediabetic stroke, NDm- non diabetic stroke, yrs- years,m- male, F- female, I- infarct, H- haemorrhage, bmI- body mass index, tC- total cholesterol, tG- triglyceride, HD- HDL cholesterol, LD- LDL cholesterol, Ir- insulin resistance level, n-HC- non HDL cholesterol, Ctr- carotid intimo-medial thickness of the right side, CtL- carotid intimo-medial thickness of the left side, p- p value of t test, n- number of patients, * = significant p value
the measurements were done in the posterior (far) wall at three places (i.e. common carotid artery: 20 to 60 mm proximally from the flow divider; carotid bulb: 0 to 20 mm distally from the flow divider; and carotid artery bifurcation: 0 to 20 mm proximally from the flow divider) at zones free of plaques.16 these three measurements were averaged on either side (left and right carotid) and the mean values were taken separately for either side.16,6 the images were digitally captured during the systole of a single heartbeat (eCG r wave gated) and measurements were performed offline for each area.16
serum lipids (tC, tG, LD and HD - directly measured and n-HC calculated) and blood glucose were measured by auto analyzer and serum insulin by eLIsA (monobind Corporation). Insulin resistance was assessed by using the previously validated homeostasis model assessment for insulin resistance, calculated
from the fasting insulin and glucose concentrations according to the formula: HOmA-Ir = [(insulin × glucose)/22.5].17 HbA1c was estimated by Boronate affinity chromatography (Bio-Rad micromat-2). statistical analysis was done by student’s t test and Pearson’s correlation co-efficient (SPSS Version 14.0). A p value of ≤ 0.05 was considered significant.
Results
A total of 29 consecutive patients of stroke in known t2Dm were collected; 4 could not complete the total investigations - the study was done with 25 patients of t2Dm. In the NDm subgroup the total number at inclusion was 14 and 17 were found to be PDm (3 could not complete the study). the Dm strokes had 40% smokers and the other 2 groups had 37.5% each - all were males without any significant inter group difference in prevalence. m:F= 13:2
Dm-H n=10 m:F= 4:6
62±12.3 24.4±4.1 181.5±29.4 180.4±57.9 39.1±5.7 131.1±24.7 142.4±28.9 3.4±2.4 0.81±0.14 0.95±0.32
P value 0.52 0.52 0.49 0.045* 0.99 0.89 0.52 0.83 0.06 0.89
PDm-I n=9 m:F=6:3
58.3±6.5 25.2±3.4 160.4±28.9 127.7±42 38.7±5.7 106.4±43 121.8±27 1.8±1.2 0.84±0.17 0.86±0.16
PDm-H n=5 m:F= 3:2
66.8±8.9 28.4±3.5 190.6±52.9 156.4±40.8 37.4±7.2 127.2±47.2 153.2±53.3 1.54±1 0.94±0.16 0.88±0.14
P value 0.08 0.15 0.23 0.3 0.74 0.5 0.2 0.8 0.4 0.9
NDm-I n=8 m:F= 4:4
60.8±9.4 25.5±1.9 194.8±27.3 192.5±71 45.9±8.9 126.6±38.1 148.9±33.9 0.8±0.4 0.76±0.07 0.83±0.1
NDm-H n=6 m:F= 4:2
59.3±7.4 26.2±2.4 178.2±55.5 127.2±44.2 45.7±15 111.3±40.4 132.5±57.5 1.4±0.8 0.77±0.08 0.83±0.11
P value 0.8 0.6 0.5 0.09 0.97 0.5 0.54 0.13 0.9 0.88
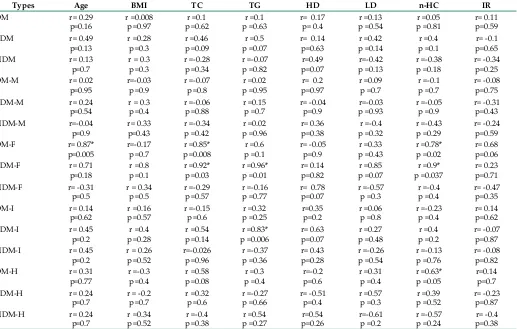
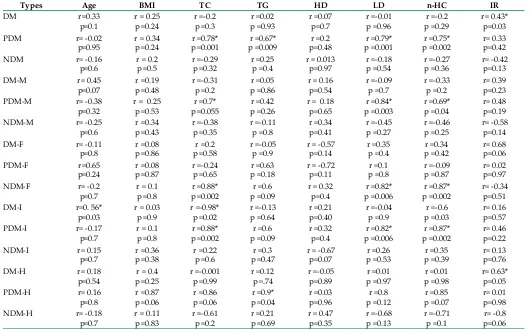
Table 5 : CIMTR correlations of the risk factors Dm- diabetic stroke, PDm prediabetic stroke, NDm- non diabetic stroke, CImtr- CImt of the right side, yrs- years,m- male, F- female, I- infarct, H- haemorrhage, bmI- body mass index, tC- total cholesterol, tG- triglyceride, HD- HDL cholesterol, LD- LDL cholesterol, Ir- insulin resistance level, n-HC- non HDL cholesterol, CIMT- carotid intimo-medial thickness, r= correlation coefficient, p= p value of the correlation, * = significant p value
Table 4 : Status of the right and left CIMTs : Level of
correlation and difference in their mean values of each stroke type and their sub groups
Stroke Type p -values Stroke Type p -values
Dm r= - 0.03
Dm- diabetic stroke, PDm prediabetic stroke, NDm- non diabetic stroke,m- male, F- female, I- infarct, H- haemorrhage, CImts- carotid intimo-medial thickness of the right and left sides, p(t)- p value of t test, r= correlation coefficient, p= p value of the correlation, * = significant p value
table1 : the age, bmI, and sex ratio were matched and the incident lipid parameters differed little among the groups; only HD was significantly higher in NDM. The mean CIMTR values were significantly higher in both DM and PDM compared to NDM; however, DM and PDM did not differ. There was no difference between the three groups for CIMTL. The IR status was significantly higher in DM compared to both PDM and NDM, but NDM and PDM did not differ.
table 2 : In intra group analysis of the parameters between infarct and haemorrhage none of the parameters differed except tG which was higher in Dm haemorrhage. In case of infarcts of all groups both the CImts were higher in Dm compared to NDM only, though the only the right side was highly significant (p=0.009) the left only expressed a higher trend (p=0.06). In case of haemorrhage none of the CIMT values differed for either side (p value ranged from 0.067 to 0.73).
p=0.95 p =0.24 p =0.001 p =0.009 p=0.48 p =0.001 p =0.002 p=0.42 Dm- diabetic stroke, PDm prediabetic stroke, NDm- non diabetic stroke, yrs- years CImtL- CImt of the right side,m- male, F- female, I- infarct, H- haemorrhage, bmI- body mass index, tC- total cholesterol, tG- triglyceride, HD- HDL cholesterol, LD- LDL cholesterol, Ir- insulin resistance level,
n-HC- non HDL cholesterol, CIMT- carotid intimo-medial thickness, r= correlation coefficient, p= p value of the correlation, * = significant p value
varieties of stroke (CImtr p value was = 0.84, 0.21, 0.53 and CImtL p value was = 0.92, 0.79 and 0.72 respectively for Dm Vs NDm, Dm Vs PDm and PDm Vs NDm).
table 4 : the mean values of the right and left CImt did not differ amongst the 3 groups as well as their stroke types and gender types. However there was significant variation in their correlations. the right – left correlation was worst in Dm and best in NDM. It was significantly positive in cases of DM infarcts, PDm infarcts and females, and NDm males and haemorrhage. table 5 and 6 : Age had predominantly positive correlation for the right side, being significant only in DM females; it was more variable for the left side and significantly positive in DM infarcts only. bmI correlated positively in nearly all groups of both the sides but was weakest in Dm for the right side and best in PDM haemorrhage for the left side, but none were significant. the Ir correlations were predominantly negative for the right side and none were significant; it was predominantly positive for the left side being significant only in DM and DM haemorrhage subgroup.
Correlations of total cholesterol were variable and predominantly negative for both the CIMT, being significantly positive in females of Dm, total PDm and PDm infarcts for CImtr, and total PDm, infarcts of Dm and PDm for CImtL.
triglyceridelevels predominantly had a positive correlation for
both CImts, especially in females and infarcts of PDm for the right side, and PDm and its haemorrhage subgroup for the left.
LDLhad a variable correlation with both side CImts but it was
significantly positive in total PDM, PDM males and infarct and NDm females for the left side only. the HDL cholesterol had a predominantly positive correlation with both the sides but was never significant. For n-HC the relations were predominantly variable for both CIMTs though it was significantly positive in the females of Dm and PDm and haemorrhage subgroup of Dm on the right side and PDm group and its male and infarct subgroups, as well as Dm infarcts and NDm females for the left side.
Discussion
the common non-invasive markers of sub-clinical and clinical atherosclerosis include AbPI (ankle brachial pressure index), CIMT, and AoIMT (aortic intimo medial thickness), flow mediated brachial artery dilatation and the number and volume
of carotid plaques.18 A CImt of less than 0.55 mm and AoImt
of less than 3 mm have been found to be excellent markers of the absence of macrovascular abnormalities, especially coronary
artery disease. 18 Higher CImt is more commonly associated with
diabetic strokes, irrespective of the gender and stroke type.19
the status in patients of pre-diabetes is not very conclusive.20
In general, due to anatomic reasons, the left side is known to suffer more shear stress and so it is more likely to have a higher
CImt than the right.21,8 CImts at all arterial sites may predict
future vascular events to almost the same level.15 However, each
In our study, CIMTs of all varieties of stroke were significantly
higher than non –stroke historical controls.7,15 In the three groups
of patients, incidents CImts were higher in Dm strokes, though predominantly on one side. Predominance of CImtr in Dm was probably related to the stroke side circulation (more patients in our study population had a stroke in the right side circulation,
especially in Dm).8 the right and left CImt correlation was most
variable in Dm - possibly signifying a more altered vascular anatomical remodelling in Dm. Insulin resistance was the only
risk marker that was significantly increased in DM and also expressed better correlation with the incident CIMTs though
more on one side (left); the relation was least congruous in
non-diabetic strokes. 23, 11 the age of the patient also had a
better correlation with the CIMT status in diabetics (left side)
than the others.24 the Ir level and age of the patient probably
plays some role in CImt status modulation in Dm, while it of
lesser significance in PDM and NDM. 11 the incident lipids were similar in the three groups; however they correlated best with
the CImt status only in PDm.20 bmI had a positive relation with
the CImts in all, but it was worst in Dm (the right side); its role
in Dm may be questionable.9,10
In intra group analysis of Dm strokes, though females were non-smokers and hemorrhagic stroke is supposed to have a
different mechanism, they had similar CIMTs and IR status as
males and infarcts. the CImt increments were more uniform
and better related to the IR status in the females while it was age
in males; more so, for the left side.25,24 the bmI may have some
impact in infarcts only.11 Females are probably more predisposed
to have a higher CImt once they are in the post menopausal
state where the usual protection related to female gender is lost.9
there was a poor relation of the CImts in hemorrhage (though
females predominated) but it was better in infarcts indicating a
more uniform vascular remodelling in them; however, the CImt
versus IR correlations were better in hemorrhagic stroke (left
side). the correlation of age was positive in both stroke types but
it was better in cases of infarct (left side).9 the lipid correlations of the CIMTs were highly variable but were better in females and in
case of hemorrhagic stroke.23 though the mean age, CImts, bmI,
lipids and IR status varied little between the stroke types and the genders, there was significant variability in their individual
relation with the CImt status as well as the congruity of the two side CImts, being more congruous in females and infarct.
In intra group analysis of NDm strokes, the mean study parameters did not vary between the genders as well as the
stroke types. Females were non-smokers and of a significantly
higher mean age, but they had similar CImts as males. Ir status correlations were poor in the genders and stroke types except in haemorrhage for CImtL. the uniformity of the right-left
CIMTs were significant in males and haemorrhage than infarct
and females, this was in absolute contrast to both Dm and PDm
strokes.15,16 In contrast to Dm and PDm, incident Ir status and
age had little relation with CIMTs.8,9 the lipid correlations of
CImts were worst compared to both Dm and PDm.8,9 the bmI
correlations were better than both DM and PDM. The CIMTs in
non-diabetics are probably more associated with the tensile wall stress than altered intimo-endothelial vascular physiology; Ir,
age and lipids play little role, BMI may be more important.26,21 In intra group analysis of PDm strokes, there was no
difference in the mean study parameters between the genders
and stroke types. the right and left side CImt correlation was
significantly positive in females. Like the DM strokes, females
and haemorrhage had a similar CImt as males and infarct respectively. similar to the Dm strokes, females and infarcts
had a more uniform two side CImt status. the Ir and age had
better relations with CIMTs in females compared to DM. Relation
of Ir status with the CImts were variable in the stroke types,
being better for the left side in both. Impact of age was variable in infarct but better in haemorrhage. The CIMT correlations and the IR with CIMT relations in the males were better than in DM,
and the impact of age less pronounced except in females. the
correlations of lipid status with the CIMTs were significantly better in females and infarct than in DM; BMI also had a better
association than in Dm but for the right side only.1,19
At the time of stroke the CImts were higher in Dm and PDm
than NDm but were predominantly one sided (not uniform).8,21
the stroke side circulation CImt was most altered in diabetics,
while the incident risk markers often had a better correlation
with the non-stroke side.8,15,16 the CImt status and risk factor
association in pre-diabetics is distinctly different from both
diabetics and non-diabetics.20 In major groups, especially
NDm, the mean CImt values were slightly higher on the left
side, probably reflecting the physiologic variation.21 Vascular remodelling, as evidenced by the CImt status, was more
uniform in non-diabetic strokes than in Dm or PDm.27,21 the
significantly raised IR status is probably an important contributor
for the increased CImt status and or its variability in t2Dm.8
Though the mean CIMTs differed little between the genders and
stroke types of all the stroke groups, the right – left CImt level variability was an important feature and most marked in Dm and PDm (except in females and infarcts). the Ir correlations of the CImts were best in Dm, followed by PDm and worst in NDm; age correlations were similar while bmI associations
were reverse.10
Dyslipidemia was a common association of strokes of all glycemic statuses, however the lipid correlations of the CImts varied immensely; it had a consistent relation only in PDm.
Targeting lipids as an intervention tool might be effective only
in pre-diabetics; targeting all the atherosclerosis risk factors
together is probably the option in the others.28,21 In most
subgroups of the patients, non-HDL cholesterol had a negative correlation (except in PDm) while HDL cholesterol (except in Dm females and haemorrhage) had a positive relation with the
CImts; this in contrast to conventional thoughts.23
male diabetics and pre-diabetics are more prone to have higher CImt values than their non-diabetic counterparts
irrespective of the stroke type.25 In females, along with the
conventional risk factors, the post menopausal state is probably an important contributor for CImt alterations. though t2Dm is not known to increase the risk of intracerebral parenchymal haemorrhage and CImt is regarded as a non-invasive marker of ischemic stroke in diabetics, the CImts were similar in both
infarcts and hemorrhagic strokes.26,4
CImt estimated by 2D UsG does not measure medial and intimal thickness separately and therefore cannot distinguish between medial remodelling as a result of an adapted response to tensile (hypertensive) stress, and intimal thickening which is
primarily indicative of atherosclerosis.29-31 estimation of plaque
number or volume by the 3D USG is probably a better indicator
of the atherosclerosis burden than the CImt at plaque free
zones.32,6 However, diffuse CIMT increments are known to be
predictive for plaque formation.6,17 Genetic or other acquired and
less measured factors might be more important in this regard.3,10
circulation status might be helpful.
References
1. Air eL, Kissela bm. Diabetes, the metabolic syndrome, and Ischemic stroke. epidemiology and possible mechanism. Diabetes Care 2007;30:3131-3140.
2. Raggi P, Bellasi A. Imaging to Assess Effect of Medical Therapy in
Patients With Diabetes mellitus. Br J Diabetes Vasc Dis 2007;7:157-164.
3. maple-brown L, Cunningham J, Celermajer Ds, O’Dea K. Increased carotid intima-media thickness in remote and urban Indigenous Australians: impact of diabetes and components of the metabolic syndrome. Clin Endocrinol (Oxf) 2007;66:419-25.
4. Karapanayiotides t, Piechowski-Jozwiak b, van melle G, bogousslavsky J, Devuyst G. stroke patterns, etiology, and prognosis in patients with diabetes mellitus. Neurology 2004;62:1558-62.
5. Lo J, Dolan se, Kanter Jr, Hempill LC, Conelly Jm, Lees rs, et
al. Effects of Obesity, Body Composition, and Adiponectin on
Carotid Intima-media thickness in Healthy Women. J Clin Endo Met 2006;91:1677-1682.
6. mukherjee sC, basu AK, bandyopadhyay r, Pal sK, bandyopadhyay
D, Mandal SK et al. Correlation of Lipid Profile and Carotid Artery
Plaque as Detected by Ultrasound in Ischemic stroke Patients- A Hospital –based study. J Indian Med Assoc 2006;104:325-6. 7. mohan V, ravikumar r, shanthi rani s, Deepa r. Intima-media
thickness of the carotid artery in south Indian diabetic and nondiabetic subjects: the Chennai Urban Population study (CUPs).
Diabetologia 2000;43:494–99.
8. Onbas O, Kantarci m, Okur A, bayraktutan U, edis A, Ceviz N. Carotid intima-media thickness; is it correlated with stroke side.
Acta Neurol Scand 2005;111:169-171.
9. bots mL, Hoes AW, Koudstaal PJ, Hofman A, Grobbee De. Common Carotid Intima-media thickness and risk of stroke and myocardial
Infarction: The Rotterdam Study. Circulation 1997;96:1432-1437.
10. Guvener N, tutuncu Nb, Oto A, erbas t. major determinants of the carotid intima-media thickness in type 2 diabetic patients: age and body mass index. Endocr J 2000;47:525-33.
11. bonora e, tessari r, miccolo r, Zenera m, targer G, Padovani r et al. Intima-media thickness of the carotid artery in nondiabetic and NIDDm patients. relationship with insulin resistance. Diabetes Care
1997;20:66-73.
12. Sahoo R, Krishna MV, Subrahmaniyan DKS, Dutta TK, Elangovan S.
Common carotid intima-media thickness in acute ischemic stroke: A case control study. Neurol India 2009;57:627-30.
13. Kreutzenberg SV, Tiengo A, Avogaro A. Cerebrovascular disease in
diabetes mellitus: the role of carotid intima-media thickness. Nutr
Metab Cardiovasc Dis 2009;19:667-73.
14. ADA: executive summary: standards of medical care in diabetes– 2010. Diabetes Care 2010;33(suppl-1): s4-s10.
15. Lorenz MW, von Keglar S, Steinmetz H, Markus HS, Sitzer M.
Carotid Intima-media thickening Indicates a Higher Vascular risk Across a Wide Age range: Prospective Data From the Carotid Atherosclerosis Progression study (CAPs). Stroke 2006;37:87-92. 16. Homma s, Hirose N, Ishida H, Ishii t, Araki G. Carotid plaque and
Intima-media thickness Assessed by b-mode Ultrasonography in subjects ranging From Young Adults to Centenarians. Stroke
2001;32:830-835.
atherosclerosis in patients scheduled for heart valve surgery. J Am
Coll Cardiol 2002;39:1139-44.
19. brohall G, Oden A, Fagerberg b: Carotid artery intima-media thickness in patients with type 2 diabetes mellitus and impaired glucose tolerance: a systemic review. Diabet Med 2006;23:609-616. 20. Kissela bm, Khoury J, Kliendorfer D, Woo D, schneider A, Akwell
K et.al. epidemiology of Ischemic strokes in Patients with Diabetes: the Greater Cincinnati/ Northern Kentucky stroke study. Diabetes Care 2005;26:355-359.
21. Gnasso A, Irace C; Carallo C, De Franceschi M S, Motti C, Mattioli
PL, et al .InVivo Association between Low Wall shear stress and Plaque in subjects With Asymmetrical Carotid Atherosclerosis.
Stroke 1997;28:993-998.
22. Mackinnon AD, Jerrard-Dunne P, Sitzer M, Buehler A, von Kegler S, Markus HS. Rates and determinants of site-specific progression
of carotid artery intima-media thickness: the carotid atherosclerosis progression study. Stroke 2004;35:2150-4.
23. Folsom Ar, rasmussen mL, Chambless Le, Howard G, Cooper Ls, schmidt mI et al: Prospective associations of fasting insulin, body fat distribution, and diabetes with risk of ischemic stroke: the Atherosclerosis risk in Communities (ArIC) study Investigators.
Diabetes Care 1999;1077-83.
24. Vicenzini e, ricciardi mC, Puccinelli F, Altieri m, Vanacore N, Di Piero V, et al. Common Carotid Artery Intima-media thickness Determinants in a Population study. J Ultrasound Med 2007;26:427-432 .
25. Khealani bA, syed NA, maken s, mapari UU, Hameed b, Ali s, et al. Predictors of ischemic versus hemorrhagic strokes in hypertensive patients. J Coll Physicians Surg Pak 2005;15:22-25.
26. Johnson Hm, Douglas Ps, srinivasan sr, bond mG, tang r, Li s, et al . Predictors of carotid intima-media thickness progression in young adults: the bogalusa Heart study stroke. 2007;38:900-5. 27. Lee eJ, Kim HJ, bae Jm, Kim JC, Han HJ, Park Cs, et al. relevance
of common carotid intima-media thickness and carotid plaque as risk factors for ischemic stroke in patients with type 2 diabetes mellitus. Am J Neuroradiol 2007;28:916-9
28. O’riordan m. CAsHmere: No Imt effect With Atorvastatin
Over 12 Months (Unpublished data): http://www.medscape.com/
viewarticle/577309
29. Johnsen sH, mathiesen eb. Carotid plaque compared with intima-media thickness as a predictor of coronary and cerebrovascular disease. Curr Cardiol Rep 2009;11: 21-7.
30. Allan PL, mowbray PI, Lee AJ, Gerald F, Fowkes r. relationship between Carotid Intima-media thickness and symptomatic and Asymptomatic Peripheral Arterial Disease. the edinburgh Artery study. Stroke 1997;28:348-353
31. matsumoto K, sera Y, Nakamura H, Ueki Y, miyake s: Correlation between common carotid arterial wall thickness and ischemic stroke in patients with type 2 diabetes mellitus. Metabolism 2002;51:244-247. 32. Chlumsky J, Charvat J. echocardiography and carotid sonography
in diabetic patients after cerebrovascular attacks. J Int Med Res
2006;34:689-94.