Heart fatty acid
–
binding protein in combination with the
80-lead body surface potential map improves early detection of acute
myocardial infarction in patients who are cardiac troponin T
–
negative
at presentation
☆
,
☆☆
Michael J. Daly, MB, MRCP,
aConor J. McCann, MD, MRCP,
aColum G. Owens, MD, MRCP,
aMark T. Harbinson, MD, FRCP,
bJennifer A. Adgey, MD, FRCP, FACC
a,⁎
a
The Heart Centre, Royal Victoria Hospital, Belfast, Northern Ireland, UK
b
Centre for Vision and Vascular Sciences, Queen's University, Belfast, Northern Ireland, UK
Received 1 December 2010
Abstract Of patients who present with ischemic-type chest pain and a negative cardiac troponin T (cTnT) at first
medical contact, there are patients at a very early stage of infarction. The aim of this research was to assess heart fatty acid–binding protein (H-FABP), a novel marker of myocyte necrosis, in combination with the
80-lead body surface potential map (BSPM) in the early diagnosis of acute myocardial infarction (AMI).
Methods:In this prospective study, consecutive patients presenting with acute ischemic-type chest
pain between 2003 and 2006 were enrolled. At first medical contact, blood was sampled for cTnT and H-FABP; in addition, a 12-lead electrocardiogram (ECG) and BSPM were recorded. A second cTnT was sampled 12 hours or more after presentation. Peak cTnT 0.03μg/L or higher diagnosed
AMI. Elevated H-FABP was 5 ng/mL or higher. A cardiologist blinded to both the clinical details and 12-lead ECG interpreted the BSPM.
Results:Enrolled were 407 patients (age 62 ± 13 years; 70% men). Of these 407, 180 had cTnT less
than 0.03μg/L at presentation. Acute myocardial infarction occurred in 52 (29%) of 180 patients. Of
these 180 patients, 27 had ST-segment elevation (STE) on ECG, 104 had STE on BSPM (sensitivity, 88%; specificity, 55%), and 95 (53%) had H-FABP elevation. The proportion with elevated H-FABP was higher in the AMI group compared with non-AMI group (Pb.001). Body surface potential map STE was significantly associated with H-FABP elevation (Pb.001). Of those with initial cTnT less than 0.03μg/L, the c-statistic for the receiver operating characteristic curve distinguishing AMI from
non-AMI using H-FABP alone was 0.644 (95% confidence interval [CI], 0.521-0.771), using BSPM alone was 0.716 (95% CI, 0.638-0.793), and using the combination of BSPM and H-FABP was 0.812 (95% CI, 0.747-0.876;Pb.001).
Conclusion:In patients with acute ischemic-type chest pain who have a normal cTnT at presentation,
the combination of H-FABP and BSPM at first assessment identifies those with early AMI (c-statistic, 0.812;Pb.001), thus allowing earlier triage to reperfusion therapy and secondary prevention. © 2011 Elsevier Inc. All rights reserved.
Introduction
In patients presenting with ischemic-type chest pain, early diagnosis of acute myocardial infarction (AMI) ensures prompt triage to urgent revascularization. Current guidelines require a positive serum level of cardiac troponin for AMI diagnosis.1 However, because of its large molecular size, cardiac troponin Journal of Electrocardiology 44 (2011) 432–438
www.jecgonline.com
☆
Financial support: Dr. Michael J. Daly is supported by The Heart Trust Fund (Royal Victoria Hospital), 9B Castle Street, Comber, Newtownards Northern Ireland BT23 5DY.
☆☆
Relationship with Industry/Conflict of Interest: None.
⁎Corresponding author. The Heart Centre, Royal Victoria Hospital, Grosvenor Road, Belfast, Northern Ireland BT12 6BA, UK.
E-mail address:jennifer.adgey@belfasttrust.hscni.net
0022-0736/$–see front matter © 2011 Elsevier Inc. All rights reserved.
T (cTnT) does not peak until 6 to 12 hours after symptom onset.2In addition, the 12-lead electrocardiogram (ECG) has only 50% sensitivity for AMI diagnosis.3,4 However, body surface potential mapping (BSPM) using 80-lead ECG has been shown to be more sensitive for detection of ST-segment elevation myocardial infarction (STEMI) than 12-lead ECG (67%-76% vs 45%-60%, respectively),5,6 particularly in the high right anterior, posterior, and right ventricular territories.5,7 Heart-type fatty acid–binding protein (H-FABP), a small cytoplasmic molecule, has been suggested as an early biomarker for evolving AMI, as it has high diagnostic sensitivity in the first few hours after symptom onset.8 Several studies in various clinical settings have reported favorable diagnostic results.9-14 In addition, H-FABP has been shown to predict long-term mortality in patients with acute coronary syndrome15 and identifies those troponin-negative patients who are at high risk for death.15-18
Thus, we hypothesized that the combination of H-FABP and BSPM assessment at presentation would improve the early diagnosis of AMI in patients with ischemic-type chest pain who are cTnT negative.
Methods
Study population
Over a 3-year period (2003-2006), we recruited prospec-tively all patients (n = 664) admitted to the coronary care unit who fulfilled the following criteria:
1. Typical ischemic-type chest discomfort occurring at rest and of greater than or equal to 20 minutes of duration
2. Twelve-lead ECG and BSPM at first medical contact (BSPM recorded within 15 minutes of 12-lead ECG) 3. Blood sampled for H-FABP (Hycult Biotech, Uden,
The Netherlands) and creatinine (estimated glomerular filtration rate) at first medical contact
4. Blood sampled for cTnT (Roche Diagnostics, Rotkreuz, Switzerland) initially and at 12 hours or more post symptom onset
Patients were excluded from analysis if they had been transferred from another ward or hospital for tertiary care (n = 118); had improper timing or collection of initial blood sample (n = 20); had received fibrinolytic therapy or anticoagulant before the 12-lead ECG, BSPM, or initial blood sample (n = 59); had ECG confounders, that is, left bundle-branch block (n = 14), right bundle-branch block (n = 6), left ventricular hypertrophy (n = 9), digitalis therapy (n = 2), or ventricular pacing (n = 7); or had greater than 15 minutes between recording of initial 12-lead ECG and BSPM (n = 22) (Fig. 1). Demographic data and established risk factors for coronary artery disease were also collected.
Twelve-lead ECG analysis
A 12-lead ECG was recorded at first medical contact (25 mm/s and 10 mm/mV). ST-segment alteration was measured at the J point for ST-segment elevation (STE) and 80 milliseconds after the J point for ST-segment depression (STD) using the preceding TP segment as a baseline19by 2 cardiologists who were blinded to all other clinical data. ST-segment elevation myocardial infarctionwas defined using the Minnesota criteria 9-220 as greater than or equal to 0.1
Fig. 1. Overview of methodology to obtain study population.
mV STE in 1 or more of leads I, II, III, aVL, aVF, V5, V6or greater than or equal to 0.2 mV STE in 1 or more of leads V1 to V4.ST-segment depression(STD) was defined as greater than or equal to 0.05 mV in any lead, and T wave inversion (TWI) was greater than or equal to 0.1 mV but was not assessed in leads III or V1.
BSPM analysis
The BSPM was recorded with a flexible plastic anterior and posterior electrode harness and a portable recording unit (Heartscape Technologies, Inc, Bangor, N. Ireland). The anterior harness contains 64 electrodes, including 3 proximal bipolar limb leads (Mason-Likar position) and a posterior harness with 16 electrodes. This lead configuration enables the recording of 77 unipolar ECG signals with respect to the Wilson central terminal. During the interpretation process, the electro-des are defined to represent anterior, lateral, inferior, high right anterior, right ventricular, and posterior epicardial regions.5,6
Harness application takes 3 to 4 minutes.7Body surface potential mapping was recorded over 5 to 10 seconds at a sampling rate of 1 kHz and a bandwidth of 0.05 to 100 Hz7 and transferred into digital format for core laboratory analysis. The 80-lead BSPMs were uploaded and displayed on an IBM compatible computer running PRIME analysis software (Heartscape Technologies, Inc., Bangor, N.
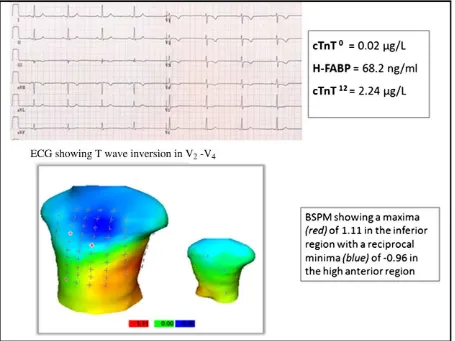
Ireland).5 All 80 leads were manually checked; and those of unacceptable quality, that is, where noise or movement artifact disallowed recognition of QRST variables, were marked and substituted using linear grid interpolation. Any BSPM with greater than 6 leads requiring interpolation were disregarded, and these patients were excluded from analysis.6 Printouts were obtained from the processed BSPM of the 80-lead ECG and a color-contour map displaying the amount of STE at the J point (ST0 isopotential map) (Fig. 2). The result of the PRIME diagnostic algorithm was noted. Using the 80-lead BSPM and color-contour map, a single cardiologist familiar with BSPM interpretation and blinded to the clinical details, 12-lead ECG, and PRIME diagnostic algorithm result coded the BSPM as AMI or non-AMI. The STE measured from the ST0 point was defined by the following thresholds: anterior greater than or equal to 0.2 mV elevation, lateral/inferior/high right anterior/right ven-tricular greater than or equal to 0.1 mV elevation, and posterior greater than or equal to 0.05 mV elevation.6
Diagnosis
Acute myocardial infarction diagnosis was made when peak cTnT was 0.03 μg/L or higher. Heart-type fatty acid–binding protein elevation was defined as 5 ng/mL or higher.21,22
Fig. 2. Patient with cTnT less than 0.03μg/L at presentation, anterior TWI on 12-lead ECG, and H-FABP elevation. Body surface potential mapping performed within 15 minutes of 12-lead ECG shows inferior territory STE. Peak cTnT of 2.24μg/L confirms AMI diagnosis.
Statistical analysis
Data are presented as mean ± SD. Group comparisons were tested using the unpairedt test and χ2 test. Sensitivity and specificity of the various diagnostic methods were calculated by comparing the prediction of AMI against peak cTnT 0.03 μg/L or higher. Overall, performance of the various diagnostic methods by receiver operating characteristic curve analysis was assessed, with area under the curve (c-statistic) greater than 0.75 taken as a good performance. Statistical analysis was performed using SPSS version 17.0 for Windows (SPSS Inc, Chicago, IL).Pb.05 was taken as statistically significant. The Northern Ireland Research Ethics Committee granted ethical approval for this research before commencement. All patients gave informed consent at the time of enrollment.
Results
Baseline characteristics
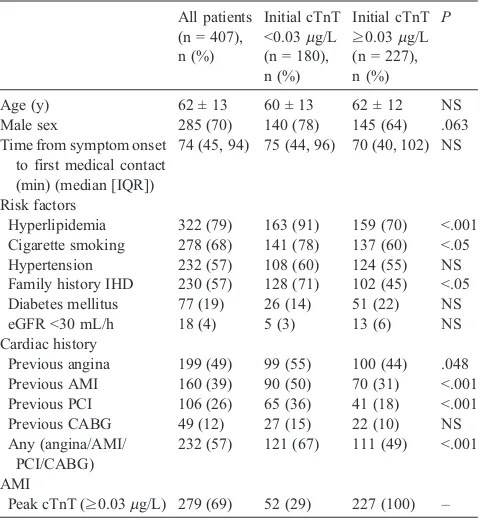
Four hundred seven patients with ischemic-type chest pain at rest (70% men; mean ± SD age, 62 ± 13 years) were included in this study. Of these, 180 (44%) had initial cTnT less than 0.03 μg/L. Demographic characteristics are summarized inTable 1. Hyperlipidemia (Pb.001), cigarette smoking (P b .05), and family history of ischemic heart disease (Pb.05) differed significantly between groups, that is, were more prevalent in those with initial cTnT less than 0.03μg/L compared with those with initial cTnT 0.03μg/L or higher. Furthermore, history of angina (Pb.05), AMI, or percutaneous coronary intervention (PCI) (P b .001) was
more frequently encountered in those with initial cTnT less than 0.03μg/L.
AMI diagnosis
Of those with initial cTnT less than 0.03μg/L, 52 (29%) of 180 patients had AMI diagnosis, that is, peak cTnT 0.03μg/L or higher at greater than or equal to 12 hours postsymptoms. Univariate analysis of the various diagnostic methods studied is summarized in Table 2. Using the 12-lead ECG, STEMI using Minnesota 9-2 criteria occurred in 27 patients and had a sensitivity of 38%, specificity of 95%, positive predictive value of 74%, and negative predictive value of 79% for AMI diagnosis. ST-segment depression in 2 or more contiguous leads occurred in 54 patients and had a sensitivity of 58%, specificity of 81%, positive predictive value of 56%, and negative predictive value of 83%. T wave inversion in 2 or more contiguous leads occurred in 28 patients and had a sensitivity of 27%, specificity of 89%, positive predictive value of 50%, and negative predictive value of 75%; and the combination of both STD and TWI in 2 or more contiguous leads had a sensitivity of 33%, specificity of 98%, positive predictive value of 85%, and negative predictive value of 78% for AMI diagnosis. In addition, STEMI (Minnesota 9-2 criteria) with STD greater than or equal to 0.05 mV and TWI greater than or equal to 0.1 mV in 2 or more contiguous leads occurred in 18 patients and had a sensitivity of 29%, specificity of 98%, positive predictive value of 83%, and negative predictive value of 77% for AMI diagnosis.
Using BSPM, STE was detected in 100 patients using the PRIME diagnostic algorithm, having a sensitivity of 85%, specificity of 56%, positive predictive value of 44%, and negative predictive value of 90% for AMI diagnosis. On physician's analysis of BSPM, STE was detected in 104 patients, resulting in a sensitivity of 88%, specificity of 55%, positive predictive value of 44%, and negative predictive value of 92% for AMI diagnosis.
Heart-type fatty acid–binding protein elevation occurred in
95 patients. In those with AMI, a significant proportion had H-FABP elevation (81%;Pb.001), that is, sensitivity of 81%, specificity of 59%, positive predictive value of 44%, and negative predictive value of 88% for the diagnosis. Further-more, H-FABP elevation was significantly associated with the detection of STE on BSPM (Pb.001). In this study, 15 (14%) of 109 of those with no Minnesota STE, STD, or TWI on initial 12-lead ECG had AMI. Of these 15 patients, all had either BSPM STE or H-FABP elevation, with 12 (80%) having both.
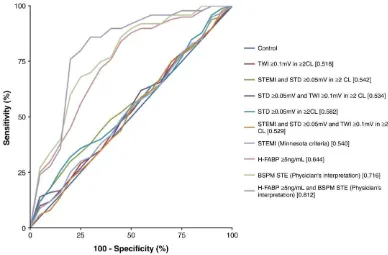
Receiver operating characteristic curve analysis
Receiver operating characteristic curves were constructed to assess the ability of H-FABP elevation, BSPM STE, and various 12-lead ECG abnormalities to predict AMI in those with initial cTnT less than 0.03μg/L (Fig. 3). Heart-type fatty acid–binding protein elevation had c-statistic 0.644 (95%
confidence interval [CI], 0.521-0.771; P = .045) for AMI diagnosis. Using BSPM, the c-statistic for AMI diagnosis using only physician's diagnosis of STE on BSPM was 0.716 (95% CI, 0.638-0.793; P = .034); and using only PRIME algorithm, diagnosis of STE was 0.708 (95% CI, 0.628-0.784; Table 1
Hyperlipidemia 322 (79) 163 (91) 159 (70) b.001 Cigarette smoking 278 (68) 141 (78) 137 (60) b.05 Hypertension 232 (57) 108 (60) 124 (55) NS Family history IHD 230 (57) 128 (71) 102 (45) b.05 Diabetes mellitus 77 (19) 26 (14) 51 (22) NS eGFRb30 mL/h 18 (4) 5 (3) 13 (6) NS Cardiac history
Previous angina 199 (49) 99 (55) 100 (44) .048 Previous AMI 160 (39) 90 (50) 70 (31) b.001 Previous PCI 106 (26) 65 (36) 41 (18) b.001 Previous CABG 49 (12) 27 (15) 22 (10) NS
Results expressed as n (%), mean ± SD, and median (interquartile range). NS indicates nonsignificant; IQR, interquartile range; IHD, ischemic heart disease; eGFR, estimated glomerular filtration rate; CABG, coronary artery bypass grafting.
P = .037). Using the 12-lead ECG, STEMI defined by Minnesota 9-2 criteria had c-statistic of 0.540 (95% CI, 0.460-0.611;P= .088); STD in 2 or more contiguous leads, 0.582 (95% CI, 0.510-0.651;P= .073); TWI in 2 or more contiguous leads, 0.518 (95% CI, 0.447-0.592; P = .096); and the
combination of both STD and TWI in 2 or more contiguous leads, 0.534 (95% CI, 0.468-0.606;P= .090).
The combination of H-FABP elevation and all 12-lead ECG abnormalities and BSPM criteria in AMI diagnosis is summarized inTable 2. The physician's diagnosis of STE on
Fig. 3. Receiver operating characteristics for diagnostic modalities listed inTable 2. Table 2
Univariate analysis of initial 12-lead ECG, BSPM, and H-FABP in the 180 patients with initial cTnT less than 0.03μg/L
Patients with cTnTb0.03μg/L
With and without AMI
(n = 180; 52 with AMI, 128 without AMI)
With AMI (n = 52)
c-Statistic
n (%) Sensitivity Specificity PPV NPV n
12-lead ECG
STEMI (Minnesota 9-2 criteria) 27 (15) 38% 95% 74% 79% 20 0.540
STD≥0.05 mV in≥2 CL 54 (30) 58% 81% 56% 83% 30 0.582
TWI≥0.1 mV in≥2 CL 28 (16) 27% 89% 50% 75% 14 0.518
STEMI (Minnesota 9-2 criteria) and STD≥0.05 mV in≥2 CL
20 (11) 35% 98% 90% 79% 18 0.542
STD≥0.05 mV and TWI≥0.1 mV in≥2CL 20 (11) 33% 98% 85% 78% 17 0.534 STEMI (Minnesota 9-2 criteria) and
STD≥0.05 mV and TWI≥0.1 mV in≥2 CL
18 (10) 29% 98% 83% 77% 15 0.529
BSPM STE
PRIME diagnostic algorithm 100 (56) 85% 56% 44% 90% 44 0.708
Physician's interpretation 104 (58) 88% 55% 44% 92% 46 0.716
H-FABP elevation (≥5 ng/mL) 95 (53) 81% 59% 44% 88% 42 0.644
H-FABP elevation (≥5 ng/mL) and
STEMI (Minnesota 9-2 criteria) 22 (12) 35% 97% 82% 78% 18 0.538
STD≥0.05 mV in≥2 CL 54 (30) 46% 77% 44% 78% 24 0.578
TWI≥0.1 mV in≥2 CL 26 (14) 15% 86% 31% 71% 8 0.480
STEMI (Minnesota 9-2 criteria) and STD≥0.05 mV in≥2 CL
19 (11) 29% 97% 79% 77% 15 0.522
STD≥0.05 mV and TWI≥0.1 mV in≥2 CL 13 (7) 12% 95% 46% 72% 6 0.488 STEMI (Minnesota 9-2 criteria) and STD≥0.05 mV
and TWI≥0.1 mV in≥2 CL
17 (9) 27% 98% 82% 77% 14 0.521
BSPM STE using PRIME diagnostic algorithm 89 (49) 73% 60% 43% 85% 38 0.807 BSPM STE using physician's interpretation 88 (49) 77% 63% 45% 87% 40 0.812
CL indicates contiguous leads; NPV, negative predictive value; PPV, positive predictive value.
BSPM in combination with H-FABP elevation has c-statistic 0.812 (95% CI, 0.747-0.876), which is significantly better than that obtained through combination of H-FABP and any 12-lead ECG criteria for AMI diagnosis in those with initial cTnT less than 0.03μg/L (Pb.001). Importantly, there is a trend toward a significant difference between the c-statistic for H-FABP alone and BSPM alone (P= .053) and a highly significant difference between the c-statistic for the combi-nations of BSPM STE and FABP elevation and both H-FABP alone (Pb.001) and BSPM STE alone (Pb.001).
Discussion
The major findings of this study on the early diagnosis of AMI in patients with chest pain, who have cTnT less than 0.03μg/L at presentation, using H-FABP and BSPM at first medical contact can be summarized as follows: (1) H-FABP greater than or equal to 5 ng/mL has a sensitivity of 81% and specificity of 59% for AMI diagnosis (c-statistic, 0.644); (2) STE occurred in 58% patients using BSPM, compared with 15% patients using the 12-lead ECG, resulting in sensitivity of 88% and specificity of 55% for AMI diagnosis (c-statistic, 0.716); and (3) the combination of H-FABP elevation and BSPM STE improved AMI diagnosis (c-statistic, 0.812).
The appropriate triage of patients with suspected AMI depends on the availability of results from sensitive diagnostic tests. The 12-lead ECG is the cornerstone in the initial evaluation of patients with chest pain and is especially crucial in the diagnosis of STEMI. In patients with STE on initial 12-lead ECG, the diagnosis of AMI is easily and rapidly established. However, 40% or more of patients with a final diagnosis of AMI have a nondiagnostic 12-lead ECG on admission23; and therefore, the initial 12-lead ECG has poor sensitivity for AMI diagnosis when STE is not present.20,24-27 It is also severely limited in its detection of right-sided, high right anterior, lateral, and posterior myocardial infarctions.24 Furthermore, in 60% to 70% of patients admitted to hospital with chest pain, the suspicion of AMI will ultimately be dismissed because of lack of diagnostic ECG changes and negative biochemical tests.23As a consequence, patients with STEMI that are not identified on the initial 12-lead ECG have been shown to have a poor prognosis,28 in part, because of delayed invasive strategies.24
In an effort to improve AMI diagnosis at presentation, McCann et al12 have shown initial H-FABP in unselected patients with ischemic-type chest pain to have c-statistic of 0.740 (Pb.001) for AMI diagnosis, improving to 0.770 (Pb
.001) when restricted to those admitted less than 4 hours from symptom onset. In addition, Haltern et al29have shown H-FABP greater than 7.3 ng/mL to have a sensitivity of 71% and specificity of 65% for AMI diagnosis (c-statistic, 0.710), with improved sensitivity in 49 consecutive patients admitted less than 4 hours from onset of ischemic-type chest pain (sensitivity, 86%; c-statistic, 0.760). In our study of unselected patients with ischemic-type chest pain who have cTnT less than 0.03 μg/L at presentation, H-FABP greater than or equal to 5 ng/mL had sensitivity of 81%, specificity of 59%, positive predictive value of 44%,
negative predictive value of 88%, and c-statistic of 0.644 (P = .045) for AMI diagnosis (Table 2 and Fig. 3). In assessing the prognostic role of H-FABP, Viswanathan et al18have shown an initial titer greater than 6.48μg/L to have clear prognostic value in those with cTnI less than 0.05 μg/L at presentation, that is, adjusted hazard ratio 3.12 (P= .03) for death or myocardial infarction at 1 year.
High-sensitivity cardiac troponin assays are now currently available, which detect cardiac troponin in excess of the 99th percentile, assuring impressive sensitivity and specificity for AMI.30,31 A recent comparison of highly sensitive cTnT (TnThs) and H-FABP in the early identification of AMI in patients with acute coronary syndrome conducted by Kurz et al30 found no significant difference in the diagnostic ability of either biomarker at presentation, that is, c-statistic 0.817 vs 0.808, respectively (P = .991). In contrast to our study, all patients in the study of Kurz et al30with baseline ECG STEMI (n = 263) were excluded. Kurz et al conclude that TnThs has a performance comparable with that of H-FABP at presentation. Ilva et al31 studied 293 patients with acute chest pain, 187 (63.8%) of whom had an initial TnIhs less than 0.03 μg/L. Although the diagnostic performance of TnIhs was again comparable with H-FABP, death or recurrent AMI at 6 months occurred in 21.4% of those with initial TnIhs less than 0.03 μg/L and H-FABP greater than 10.4 μg/L, in comparison with only 6.9% of those with normal levels of both biomarkers at presentation.30
Regarding early ECG diagnosis of AMI, Owens et al5 have shown BSPM to have a sensitivity of 76%, specificity of 92%, and c-statistic of 0.84 for AMI diagnosis in consecutive patients presenting with acute ischemic-type chest pain at rest (n = 755). Furthermore, the improvement in sensitivity over the 12-lead ECG (sensitivity, 68%) was shown to be mainly due to detection of STE in the high right anterior, posterior, and right ventricular territories in this study.5In the Optimal Cardiovascular Diagnostic Evaluation Enabling Faster Treat-ment of Myocardial Infarction (OCCULT-MI) trial, BSPM was shown once again to provide an incremental 27.5% increase in STEMI detection vs the 12-lead ECG.24 In our study of 52 patients with AMI and cTnT less than 0.03μg/L initially, 20 (38%) of 52 had STEMI on 12-lead ECG; and 46 (88%) of 52 patients had STE on BSPM (Table 2). This improvement in STE detection is due to STE occurring in leads beyond the territory of the 12-lead ECG. However, the recording of the BSPM 15 minutes or less after the 12-lead ECG in our patients potentially favored the BSPM as a diagnostic modality. In addition, 12-lead ECG diagnosis of AMI in those with factors confounding the interpretation of the ST-segment, for example, left bundle-branch block, right bundle-branch block, left ventricular hypertrophy, and digitalis therapy, remains a challenge. As these patients were excluded from analysis in our study, we cannot indicate whether H-FABP would improve AMI diagnosis in them.
In the OCCULT-MI trial, STE on BSPM was associated with increased risk of death or myocardial infarction at 30 days (odds ratio, 3.4) in those without initial 12-lead ECG STEMI.24 In addition, H-FABP elevation is independently established as a poor prognostic indicator.18 In our study,
H-FABP elevation was significantly associated with STE on BSPM, that is, of those with H-FABP elevation, 88 (93%) of 95 patients had STE on BSPM beyond the territory of the 12-lead ECG (P b .001). Furthermore, in those patients with AMI and the absence of Minnesota STE, STD, or TWI on initial 12-lead ECG, 80% had both BSPM STE and H-FABP elevation. As such, early BSPM and H-FABP assessment can identify patients with AMI who might otherwise have delayed diagnosis or be discharged from the emergency department. In addition, as shown in the OCCULT-MI trial, patients with STEMI identified on BSPM only are treated with significantly delayed or conservative invasive strategies; yet they have angiographic and clinical adverse outcomes similar to those of patients with 12-lead ECG STEMI.24
Conclusion
In this study, the combination of H-FABP and BSPM STE improves early diagnosis of AMI in those with chest pain who are cTnT negative at presentation. Both BSPM STE in patients without 12-lead ECG STEMI24and H-FABP elevation18 have independently been shown to be poor prognostic indicators for death or recurrent myocardial infarction. In this study, early BSPM and H-FABP assessment in those with ischemic-type chest pain who are cTnT negative have the potential to identify an important group of high-risk patients at an earlier time point, facilitate more timely revascularization, and reduce mortality.
References
1. Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation 2007;116:2634.
2. Panteghini M, Pagani F, Bonetti G. The sensitivity of cardiac markers: an evidence-based approach. Clin Chem Lab Med 1999;37:1097. 3. Menown IBA, Allen J, Anderson JMcC, Adgey AAJ. ST depression
only on the initial 12-lead ECG: early diagnosis of acute myocardial infarction. Eur Heart J 2001;22:218.
4. O'Neil BJ, Hoekstra J, Pride YB, et al. Incremental Benefit of 80-lead Electrocardiogram Body Surface Mapping Over the 12-lead Electro-cardiogram in the Detection of Acute Coronary Syndromes in Patients Without ST-elevation Myocardial Infarction: Results from the Optimal Cardiovascular Diagnostic Evaluation Enabling Faster Treatment of Myocardial Infarction (OCCULT MI) Trial. Acad Emerg Med 2010;17:932.
5. Owens C, McClelland A, Walsh S, Smith B, Adgey J. Comparison of value of leads from body surface maps to 12-lead electrocardiogram for diagnosis of acute myocardial infarction. Am J Cardiol 2008;102:257. 6. Owens C, Navarro C, McClelland A, et al. Improved detection of acute myocardial infarction using a diagnostic algorithm based on calculated epicardial potentials. Int J Cardiol 2006;111:292.
7. Ornato JP, Menown IB, Peberdy MA, et al. Body surface mapping vs 12-lead electrocardiography to detect ST-elevation myocardial infarc-tion. Am J Emerg Med 2009;27:779.
8. Alhadi HA, Fox KAA. Do we need additional markers of myocyte necrosis: the potential value of heart fatty-acid–binding protein. QJM 2004;97:187.
9. Ecollan P, Collet J-P, Boon G, et al. Pre-hospital detection of acute myocardial infarction with ultra-rapid human fatty acid–binding protein (H-FABP) immunoassay. Int J Cardiol 2007;119:349.
10. Liao J, Chan CP, Cheung YC, et al. Human heart-type fatty acid– binding protein for on-site diagnosis of early acute myocardial infarction. Int J Cardiol 2008;133:420.
11. Mad P, Domanovits H, Fazelnia C, et al. Human heart-type fatty acid– binding protein as a point-of-care test in the early diagnosis of acute myocardial infarction. QJM 2007;100:203.
12. McCann CJ, Glover BM, Menown IB, et al. Novel biomarkers in early diagnosis of acute myocardial infarction compared with cardiac troponin T. Eur Heart J 2008;29:2843.
13. Ruzgar O, Bilge AK, Bugra Z, et al. The use of human heart-type fatty acid–binding protein as an early diagnostic biochemical marker of myocardial necrosis in patients with acute coronary syndrome, and its comparison with troponin-T and creatine kinase-myocardial band. Heart Vessels 2006;21:309.
14. Valle HA, Riesgo LG, Bel MS, Gonzalo FE, Sanchez MS, Oliva LI. Clinical assessment of heart-type fatty acid binding protein in early diagnosis of acute coronary syndrome. Eur J Emerg Med 2008;15:140. 15. Kilcullen N, Viswanathan K, Das R, et al. EMMACE-2 Investigators. Heart-type fatty acid–binding protein predicts long-term mortality after acute coronary syndrome and identifies high-risk patients across the range of troponin values. J Am Coll Cardiol 2007;50:2061.
16. O’Donoghue M, de Lemos JA, Morrow DA, et al. Prognostic utility of heart-type fatty acid binding protein in patients with acute coronary syndromes. Circulation 2006;114:550.
17. De Lemos JA, O’Donoghue M. The skinny on fatty acid–binding protein. J Am Coll Cardiol 2007;50:2068.
18. Viswanathan K, Kilcullen N, Morrell C, et al. Heart-type fatty acid– binding protein predicts long-term mortality and re-infarction in consecutive patients with suspected acute coronary syndrome who are troponin-negative. J Am Coll Cardiol 2010;55:2590.
19. Cohen M, Hawkins L, Greenberg S, Fuster V. Usefulness of ST-segment changes in≥2 leads on the emergency room electrocardio-gram in either unstable angina pectoris or non–Q-wave myocardial infarction in predicting outcome. Am J Cardiol 1991;67:1368. 20. Menown IBA, Mackenzie G, Adgey AAJ. Optimizing the initial 12-lead
electrocardiographic diagnosis of acute myocardial infarction. Eur Heart J 2000;21:275.
21. Wodzig KW, Pelsers MM, van der Vusse GJ, Roos W, Glatz JF. One-step enzyme-linked immunosorbent assay (ELISA) for plasma fatty acid–binding protein. Ann Clin Biochem 1997;34:263.
22. McCann CJ, Glover BM, Menown IBA, et al. Prognostic value of a multimarker approach for patients presenting to hospital with acute chest pain. Am J Cardiol 2009;103:22.
23. Xu Q, Chan CPY, Cao X, et al. Cardiac multi-marker strategy for effective diagnosis of acute myocardial infarction. Clin Chim Acta 2010;411:1781.
24. Hoekstra JW, O'Neill BJ, Pride YB, et al. Acute detection of ST-elevation myocardial infarction missed on standard 12-lead ECG with a novel 80-lead real-time digital body surface map: primary results from the multicenter OCCULT MI trial. Ann Emerg Med 2009;54:779. 25. Herring N, Paterson DJ. ECG diagnosis of acute ischaemia and
infarction: past, present and future. QJM 2006;99:219.
26. Fesmire FM, Percy RF, Bardoner JB, Wharton DR, Calhoun FB. Usefulness of automated serial 12-lead ECG monitoring during the initial emergency department evaluation of patients with chest pain. Ann Emerg Med 1998;31:3.
27. Welch RD, Zalenski RJ, Frederick PD, et al. Prognostic value of a normal or nonspecific initial electrocardiogram in acute myocardial infarction. JAMA 2001;286:1977.
28. Wang TY, Zhang M, Fu Y, et al. Incidence, distribution, and prognostic impact of occluded culprit arteries among patients with non-ST elevation acute coronary syndrome undergoing diagnostic angiography. Am Heart J 2009;157:716.
29. Haltern G, Peiniger S, Bufe A, Reiss G, Gülker H, Scheffold T. Comparison of usefulness of heart-type fatty acid binding protein versus cardiac troponin T for diagnosis of acute myocardial infarction. Am J Cardiol 2010;105:1.
30. Kurz K, Giannitsis E, Becker M, Hess G, Zdunek D, Katus HA. Comparison of the new high sensitive cardiac troponin T with myoglobin, h-FABP and cTnT for early identification of myocardial necrosis in the acute coronary syndrome. Clin Res Cardiol 2011;100:209.