World Health House Indraprastha Estate, Mahatma Gandhi Marg, New Delhi-110002, India
in the South-East Asia Region
© World Health Organizaion 2016
All rights reserved.
Requests for publicaions, or for permission to reproduce or translate WHO publicaions – wheth -er for sale or for noncomm-ercial distribuion – can be obtained from Publishing and Sales, World Health Organizaion, Regional Oice for South- East Asia, Indraprastha Estate, Mahatma Gandhi Marg, New Delhi 110 002, India (fax: +91 11 23370197; e-mail: [email protected]).
The designaions employed and the presentaion of the material in this publicaion do not imply the expression of any opinion whatsoever on the part of the World Health Organizaion concern -ing the legal status of any country, territory, city or area or of its authoriies, or concern-ing the delimitaion of its froniers or boundaries. Doted lines on maps represent approximate border lines for which there may not yet be full agreement.
The menion of speciic companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organizaion in preference to others of a similar nature that are not menioned. Errors and omissions excepted, the names of proprietary products are disinguished by iniial capital leters.
All reasonable precauions have been taken by the World Health Organizaion to verify the infor -maion contained in this publicaion. However, the published material is being distributed with -out warranty of any kind, either expressed or implied. The responsibility for the interpretaion and use of the material lies with the reader. In no event shall the World Health Organizaion be liable for damages arising from its use.
Maps disclaimer
The boundaries and names shown and the designaions used on the maps contained in this docu -ment do not imply the expression of any opinion whatsoever on the part of the World Health Organizaion concerning the legal status of any country, territory, city or area or of its authoriies, or concerning the delimitaion of its froniers or boundaries. Doted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
Printed in India
Tuberculosis control in the South-East Asia Region: annual report 2016.
1. Tuberculosis – prevenion and control – staisics and numerical data 2. Tuberculosis, Mulidrug-Resistant 3. HIV 4. Health Resources 5. Data Collecion.
Contents
Abbreviaions ... v
Foreword ...ix
1. Global and Regional burden of Tuberculosis ... 1
TB burden ... 2
Drug-resistant TB ...4
Co-epidemics of TB and HIV ... 5
TB inancing ... 6
2. Global and Regional progress in Tuberculosis care and management ...8
TB care and control ...9
Drug-resistant TB ... 10
Co-epidemic of TB and HIV... 11
New diagnosics rollout ...13
New drugs rollout ...13
Research and development ...13
3. Regional challenges ... 15
Over reliance on donor funding ... 16
4. The End-TB Strategy ... 20
5. Regional Strategic Plan – Overview ... 25
Vision and goal ... 26
Objecives ... 26
Regional targets and milestones ... 26
Strategic direcions and intervenions ...28
6. WHO support in the Region ...32
Transiioning to the End TB Strategy ...33
Diagnosic capacity-building ...34
Expansion of DR-TB services ...35
Rouine surveillance ...38
Operaional research ...39
Resource mobilizaion ...40
7. Major SEA Regional partnerships ...41
Axshya project supported by The Global Fund ...42
EXPAND-TB project ...43
Global TB Drug Facility (GDF) ...45
Paediatric TB project ...47
TB REACH project ...47
UNITAID support in SEAR countries ...49
United States Agency for Internaional Development (USAID) in SEAR countries ... 51
8. Country proiles ...57
Bangladesh ...59
Bhutan ...77
Democraic People’s Republic of Korea ...90
India ...103
Indonesia ...118
Maldives ...134
Myanmar ...146
Nepal ...157
Sri Lanka ...170
Thailand ...182
Abbreviaions
ACSM advocacy, communicaion and social mobilizaion AFB acid-fast bacilli
AIDS acquired immunodeiciency syndrome ART aniretroviral therapy
ARV aniretrovirals
CBO community-based organizaions CCM country coordinaion mechanism
CDC Centers for Disease Control, Atlanta, USA CHW community health worker
CSMBS Civil Servant Medical Beneit Scheme (Thailand) CN concept note(s)
CPT co-trimoxazole prevenive therapy CV community volunteer
DOT directly observed therapy
DOTS the internaionally recommended strategy for TB control and the foundaion of the Stop TB Strategy introduced in 2006
rGLC regional Green Light Commitee GLI Global Laboratory Iniiaive HBC high-burden (TB) country HRD human resource development HRH human resources for health HSS health system strengthening IC infecion control
IPT isoniazid prevenive therapy IQC internal quality control
ISTC Internaional Standards for TB Care IC infecion control
JICA Japan Internaional Cooperaion Agency KNCH Royal Dutch Foundaion
LED light-emiing diode microscopes LTBI latent TB infecion
MCH maternal and child health MDG Millennium Development Goals MDR-TB TB mulidrug-resistant tuberculosis
M&E monitoring and evaluaion NFM New Funding Model MSH Management Sciences for Health
NGO nongovernmental organizaion NRL naional reference laboratory NSP naional strategic plan NSP new smear posiive
NTP naional TB control programme OTC over-the-counter (sale of medicines) PAL pracical approach to lung health PHC primary health care
PMDT programmaic management of drug-resistant tuberculosis PMTCT prevenion of mother to child transmission
PPM public-private mix PTB pulmonary TB
PWID people who inject drugs
PR principal recipient (under Global Fund grants) QA quality assurance
RNTCP Revised Naional TB Control Programme (of India) RR-TB rifampicin-resistant TB
SCC short coerce chemotherapy SDG Sustainable Development Goals SEA South-East Asia
SEAR South-East Asia Region (of WHO) SLD Second-line ani-TB drugs SOPs standard operaing procedures
SR subrecipient (under Global Fund grants) SSF single stream funding (GF)
SSS Social Security Scheme (Thailand)
TA technical assistance
TB Tuberculosis
The Union Internaional Union against Tuberculosis and Lung Disease TWG-TB Technical Working Group on TB
USAID United States Agency for Internaional Development UCS Universal Coverage Scheme (Thailand)
Foreword
The start of 2016 heralds the beginning of a new era in global health and development. The United Naions has adopted the Sustainable Development Goals (SDGs), providing a new development framework for 2016−2030, replacing the 2000−2015 Millennium Development Goal (MDG) framework. Under Goal 3 of the SDGs speciically pertaining to health, target 3.3 states - By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepaiis, waterborne diseases and other communicable diseases. The year 2016 also marks the beginning of implementaion of the WHO End TB strategy based on the principles and targets enshrined in the World Health Assembly resoluion WHA67.1. The three pillars of the End TB strategy include integrated, paient-centred care and prevenion; bold policies and supporive systems; and intensiied research and innovaion. Thus there is a reinvigorated emphasis on ending the global TB epidemic, and 2016 will be the year to lay the foundaion for TB control globally as well as in the South-East Asia (SEA) Region.
The Regional Strategic Plan towards Ending TB in the SEAR 2016–2020 describes
the future direcions and focus of the work towards TB eliminaion aiming to support Member States in the reducion in tuberculosis mortality and incidence in line with the global targets as set in World Health Assembly resoluion WHA67.1, guiding the countries in addressing the persising and emerging epidemiological and demographic challenges and advancing universal health coverage and robust health systems. The plan builds on and expands the exising updated Regional Strategic Plan for TB Care and Control 2012–2015 and focuses on the implementaion of the End TB Strategy in the coming 5 years within the overall scope of the 20-year strategy covering the period 2015 to 2035.
Ending the TB epidemic is not mere biomedical but a developmental challenge. The global, regional, naional and local level response to ending the TB epidemic must therefore be a part of an inclusive response designed to meet the overall development goals. The progress towards ending the TB epidemic will depend as much on achieving overall health improvement as it will on opimizing current strategies, developing new tools and technologies to diagnose, treat and prevent TB, and reaching them to all who need them.
I urge all Member States to work at all levels along with partners for renewed commitment towards ending the TB epidemic. Addiional resources would need to be mobilized. Ending the TB epidemic will require an expansion of the scope and reach of intervenions for TB prevenion, care and control: the insituion of systems and policies to promote an enabling environment, shared responsibiliies with universal coverage; and an aggressive pursuit of research and innovaion to promote development and use of new tools for TB care and prevenion.
Tuberculosis (TB) is contagious and airborne. It ranks alongside HIV/AIDS as a leading cause of death worldwide.
TB burden
Globally, 9.6 million people fell ill with TB in 2014, including 1.2 million people living with HIV. In the same year 1.5 million people died from TB, including 0.4 million among people who were HIV-posiive. TB is one of the top ive killers of women among adult women aged 20–59 years. 480 000 women died from TB in 2014, including 140 000 deaths among women who were HIV-posiive. 890 000 men died from TB and 5.4 million fell ill with the disease. An esimated 1 million children became ill with TB and 140 000 children died of TB in 2014.
The SEA Region of WHO is home to 26% of the world’s populaion; however the Region accounts for 41% of the global burden in terms of TB incidence. In 2014, there were an esimated 5.4 million prevalence and 4 million incidence of TB, and about 460 000 people died due to TB in SEAR. India and Indonesia have among the largest numbers of cases (23% and 10% of the global total respecively). An esimated 340 000 children in the Region developed TB in 2014.
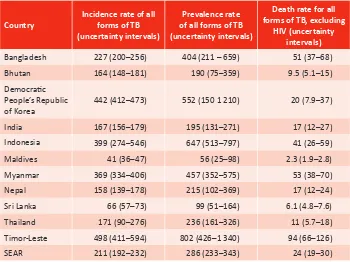
Table 1.1: Esimates of TB burden in SEAR countries in terms of incidence, prevalence and mortality, 2014
Country
Incidence rate of all forms of TB (uncertainty intervals)
Prevalence rate of all forms of TB (uncertainty intervals)
Death rate for all forms of TB, excluding
HIV (uncertainty intervals)
Bangladesh 227 (200–256) 404 (211 – 659) 51 (37–68) Bhutan 164 (148–181) 190 (75–359) 9.5 (5.1–15) Democraic
People’s Republic
of Korea 442 (412–473) 552 (150 1 210) 20 (7.9–37)
India 167 (156–179) 195 (131–271) 17 (12–27)
Indonesia 399 (274–546) 647 (513–797) 41 (26–59)
Maldives 41 (36–47) 56 (25–98) 2.3 (1.9–2.8)
Myanmar 369 (334–406) 457 (352–575) 53 (38–70)
Nepal 158 (139–178) 215 (102–369) 17 (12–24)
Sri Lanka 66 (57–73) 99 (51–164) 6.1 (4.8–7.6)
Thailand 171 (90–276) 236 (161–326) 11 (5.7–18)
Timor-Leste 498 (411–594) 802 (426–1 340) 94 (66–126)
SEAR 211 (192–232) 286 (233–343) 24 (19–30)
The trends of TB burden in SEA Region in terms of esimated disease
incidence, prevalence and mortality are shown in Graph 1.1, Graph 1.2 and Graph 1.3 respecively
Graph 1.1: Esimated TB incidence rates (green) and esimated incidence rates of HIV-posiive TB (red) in SEAR. Shaded areas represent uncertainty bands
200
100
0
1990 1995 2000 2005 2010 2015
Source: World Health Organizaion. Global tuberculosis report 2015. Geneva: WHO, 2015.
Graph 1.2: Esimated TB prevalence in SEAR (1990–2015). Shaded areas represent uncertainty bands. The horizontal dashed lines represent the Stop TB Partnership target of a 50% reducion
in the prevalence rate by 2015 compared with 1990
400 600
200
0
1990 1995 2000 2005 2010 2015
Graph 1.3: Esimated TB mortality rates in SEAR (1990–2015). Esimated TB mortality excludes TB deaths among HIV-posiive people. Shaded areas represent uncertainty bands. The horizontal dashed lines represent the Stop TB Partnership target of a 50% reducion in the
mortality rate by 2015 compared with 1990
40 60
20
0
1990 1995 2000 2005 2010 2015
Source: World Health Organizaion. Global tuberculosis report 2015. Geneva: WHO, 2015.
Drug-resistant TB
An esimated 480 000 people developed mulidrug-resistant TB (MDR-TB) and an esimated 190 000 deaths from MDR-TB occurred globally in 2014. If all TB cases noiied in 2014 had been tested for drug resistance, an esimated 300 000 would have been found to have MDR-TB.
The SEA region has relaively low levels (2.2, range: 1.9–2.6%) of mulidrug-resistant (MDR) among newly detected cases. The esimated levels of MDR-TB among retreatment cases is 16% (range 14–18%). However, given the large number of TB cases in the SEA Region, this translates to a total of 99 000 esimated MDR-TB cases among noiied pulmonary TB cases accouning for approximately 30% of the world’s MDR-TB cases among noiied pulmonary TB cases in 2014. Six of the 30 high MDR-TB-burden countries are in the SEA Region: Bangladesh, Democraic People’s Republic of Korea, India, Indonesia, Myanmar
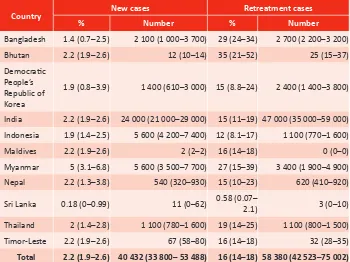
Table 1.2: Esimates of proporion of MDR-TB among new and retreatment cases in SEAR countries, 2014
Country New cases Retreatment cases
% Number % Number
Bangladesh 1.4 (0.7–2.5) 2 100 (1 000–3 700) 29 (24–34) 2 700 (2 200–3 200) Bhutan 2.2 (1.9–2.6) 12 (10–14) 35 (21–52) 25 (15–37) Democraic
People’s Republic of Korea
1.9 (0.8–3.9) 1 400 (610–3 000) 15 (8.8–24) 2 400 (1 400–3 800)
India 2.2 (1.9–2.6) 24 000 (21 000–29 000) 15 (11–19) 47 000 (35 000–59 000) Indonesia 1.9 (1.4–2.5) 5 600 (4 200–7 400) 12 (8.1–17) 1 100 (770–1 600) Maldives 2.2 (1.9–2.6) 2 (2–2) 16 (14–18) 0 (0–0) Myanmar 5 (3.1–6.8) 5 600 (3 500–7 700) 27 (15–39) 3 400 (1 900–4 900) Nepal 2.2 (1.3–3.8) 540 (320–930) 15 (10–23) 620 (410–920)
Sri Lanka 0.18 (0–0.99) 11 (0–62) 0.58 (0.07–2.1) 3 (0–10)
Thailand 2 (1.4–2.8) 1 100 (780–1 600) 19 (14–25) 1 100 (800–1 500)
Timor-Leste 2.2 (1.9–2.6) 67 (58–80) 16 (14–18) 32 (28–35) Total 2.2 (1.9–2.6) 40 432 (33 800– 53 488) 16 (14–18) 58 380 (42 523–75 002) Source: World Health Organizaion. Global tuberculosis report 2015. Geneva: WHO, 2015.
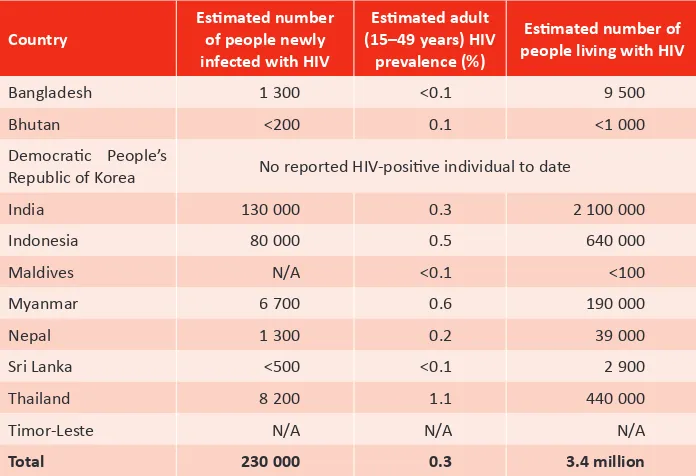
Co-epidemics of TB and HIV
In 2014, an esimated 1.2 million (12%) of the 9.6 million people who developed TB worldwide were HIV posiive. In SEAR, an esimated 210 000 cases (5.2%) of the 4 million incident cases were HIV posiive. This corresponds to 11 per 100 000 and 5% of all esimated TB incident cases.
Table 1.3: Esimated HIV prevalence among adult populaions and the number of people living with HIV infecion in SEAR countries, 2013
Country
Esimated number
of people newly infected with HIV
Esimated adult (15–49 years) HIV
prevalence (%)
Esimated number of
people living with HIV
Bangladesh 1 300 <0.1 9 500
Bhutan <200 0.1 <1 000
Democraic People’s
Republic of Korea No reported HIV-posiive individual to date
India 130 000 0.3 2 100 000
Indonesia 80 000 0.5 640 000
Maldives N/A <0.1 <100
Myanmar 6 700 0.6 190 000
Nepal 1 300 0.2 39 000
Sri Lanka <500 <0.1 2 900
Thailand 8 200 1.1 440 000
Timor-Leste N/A N/A N/A
Total 230 000 0.3 3.4 million
Source: World Health Organizaion, Regional Oice for South-East Asia. Health sector response to HIV in the South-East Asia Region 2013. New Delhi: WHO-SEARO, 2013.
TB inancing
Table 1.4: General government expenditure on health as a percentage of total government expenditure, and out-of-pocket expenditure on health as a percentage of total expenditure
on health, 2013
Country
General government expenditure on health as a percentage of total government
expenditure
Out-of-pocket expenditure on health as a percentage of total
expenditure on health
Bangladesh 8–11 >45
Bhutan <8 16–29
Democraic People’s
Republic of Korea Data not available Data not available
India <8 >45
Indonesia <8 >45
Maldives 12–14 30–44
Myanmar <8 >45
Nepal 12–14 >45
Sri Lanka 8–11 >45
Thailand >15 <15
Timor-Leste <8 16–29
Cut of points used: (<8; 8–11; 12–14; >15) (<15; 15;16–29; 30–44; >45)
2
The MDG target of haling and reversing TB incidence by 2015 was achieved globally in all six WHO Regions. The TB mortality rate in 2015 was 47% lower than in 1990: the target of a 50% reducion was almost met. The target was achieved in four WHO Regions including SEAR. Globally, the TB prevalence rate in 2015 was 42% lower than in 1990. The target of a 50% reducion was met in three WHO regions including SEAR. Overall, all three 2015 MDG targets for TB were met in the Region of the Americas, SEAR and WPR.
Between 2000 and 2014, 43 million lives were saved through efecive diagnosis and treatment.
TB care and control
In 2014, 6 million newly diagnosed cases were noiied to naional TB
programmes. This is about 63% of the 9.6 million people esimated to have fallen sick with the disease. In SEAR, TB noiicaions were about 2.6 million in 2014 whereas in 2013, they were about 2.3 million. This was mostly due to a 29% increase in noiicaions in India, which followed the introducion of a policy of mandatory noiicaion in May 2012, creaion of a naional web-based reporing system in June 2012 and intensiied eforts to engage the private health sector.
Globally, the treatment success rate for people newly diagnosed with TB was 86% for the 2013 cohort. In SEAR, TB treatment success rate has coninued to be more than 88% since 2009.
Graph 2.1: Case noiicaion and esimated TB incidence rates in SEAR (1990–2014). [Trends in case noiicaion rates (new and relapse cases, all forms) (black) and esimated TB incidence
rates (green). Shaded areas represent uncertainty bands]
200
Drug-resistant TB
Globally 123 000 people were diagnosed with MDR-TB in 2014, about one fourth of the total 480 000 new cases of MDR-TB that occurred in 2014. A total of 111 000 people started MDR-TB treatment in 2014, an increase of 14% compared with 2013. 43 countries reported cure rates for MDR-TB paients of ≥75%. Nevertheless, globally, data show an average cure rate of only 50% for treated MDR-TB paients. Extensively drug-resistant TB (XDR-TB) has been reported by 105 countries by 2015. An esimated 9.7% of people with MDR-TB have XDR-TB.
In SEAR, 33 264 cases were conirmed as Rifampicin resistant or mulidrug-resistant TB and 28 536 cases were started on MDR-TB treatment in 2014, which represented only 34% and 29 % respecively out of the esimated 99 000 MDR-TB cases among noiied TB cases.
Globally only 50% of MDR-TB paients were successfully treated and 49% in SEAR in 2014 (2012 cohort).
Extensively drug-resistant TB had been reported by six countries in SEAR.
Table 2.1: Treatment outcomes expressed as percentage among cases registered by type of cases in 2013 and 2012 (later for RR/MDR-TB) and in Member States of the SEA Region
Country
Bangladesh 93 86 75 72 25
Bhutan 91 60 na 100 Na
Indonesia 88 64 49 54 64
Maldives 84 75 na 50 100
Country
Thailand 81 66 67 No data No data
Timor-Leste 84 91 No data 75 No data
SEAR 88 67 74 49 37
Source: World Health Organizaion. Global tuberculosis report 2015. Geneva: WHO, 2015.
Treatment outcomes of MDR-TB paients iniiated on treatment in yearly cohort since 2007 is provided in Graph 2.2
Graph 2.2: Treatment outcomes for paients diagnosed with MDR-TB in SEAR (2007–2012) cohorts. [The total number of cases with outcome data is shown beside each bar]
2007
Source: World Health Organizaion. Global tuberculosis report 2015. Geneva: WHO, 2015.
Co-epidemic of TB and HIV
an increase of about 60% compared with 2013. Over half of these people (59%) were in South Africa. Thirteen of the 41 high TB/HIV burden countries reported provision of IPT in 2014 and coverage among people living with HIV who were newly enrolled in care was 41%.
In SEAR, 45% of noiied TB paients had a documented HIV test result in 2014. Out of the TB paients known to be living with HIV, 85 % were on ART in the Region. SEAR maintained 85% CPT enrolment of all noiied HIV posiive TB paients from 2003. IPT uptake is sill low with only 3049 cases reported in 2014. The achievement of Member States in strengthening TB/HIV collaboraive aciviies are provided in Table 2.2
Table 2.2: Achievements in TB/HIV collaboraive aciviies in Member States of the SEA Region, 2014
Country
Bangladesh 0.36 <1 45 100 100
Bhutan 12 65 7 100 0
Indonesia 25 5 2355 26 41
Maldives 0.09 99 0 0 0
Myanmar 36 40 6 412 36 73
Nepal 5.4 9 369 No data 74
Sri Lanka 0.26 78 21 86 86
Thailand 22 71 6831 69 64
Timor-Leste 4.9 54 24 100 100
SEAR 11 45 60 235 85 85
New diagnosics rollout
Globally, the use of the rapid test Xpert® MTB/RIF has expanded substanially since 2010, when WHO irst recommended its use. In all, 4.8 million test cartridges were procured in 2014 by 116 low- and middle-income countries at concessional prices, up from 550 000 in 2011. By 2015, 69% of countries recommended using Xpert® MTB/RIF as the iniial diagnosic test for people at risk of drug-resistant TB, and 60% recommended it as the iniial diagnosic test for people living with HIV.
GeneXpert has also been introduced and being rolled out in SEAR countries.
New drugs rollout
In 2013 and 2014, WHO issued interim guidance on the use of bedaquiline and delamanid. By the end of 2014, 43 countries reported having used bedaquiline as part of treatment for MDR-TB.
Indonesia is among the irst countries in the Region and among four countries across the globe to systemaically pilot bedaquiline introducion with WHO support. The process started in November 2013, and in June 2014, the irst workshop of bedaquiline introducion was held followed by pharmacovigilance assessment and site selecion. In October 2014, endorsement of technical guidelines and pharmacovigilance plan was done by the technical working group. In April 2015, a pharmacovigilance training workshop was held followed later by integraion of bedaquiline Pv system in e-TB Manager sotware. Later, a Cohort Event Monitoring (CEM) Pv training was also held. The enrolment of paients started in September 2015, and by November 2015, seven paients were on treatment with a regimen inclusive of bedaquiline.
Research and development
TB care and control in the SEA Region has taken great strides in recent years with the expansion of programmes towards universal coverage, introducion of new tools and diagnosics, partnership building and resource mobilizaion. However addiional concerted eforts are required to ensure the necessary progress towards the target of the eliminaion of TB by 2035. Analyses of constraints to regional TB control bring forward major persising barriers. These include:
Over reliance on donor funding
In most countries of the Region, insuicient domesic resources have been allocated for TB control programmes and for most countries, the funding is being supplemented considerable by internaional bilateral and mulilateral funding agencies. Naional governments meet an average of 40% of current budgets for NTPs and variaion between countries is considerable.
For achieving the ambiious goals of the End TB strategy, it is expected that addiional intervenions may be needed speciically for introducion and roll-out of new tools, diagnosics and drugs that have not been included in the inancing
reported for 2015.
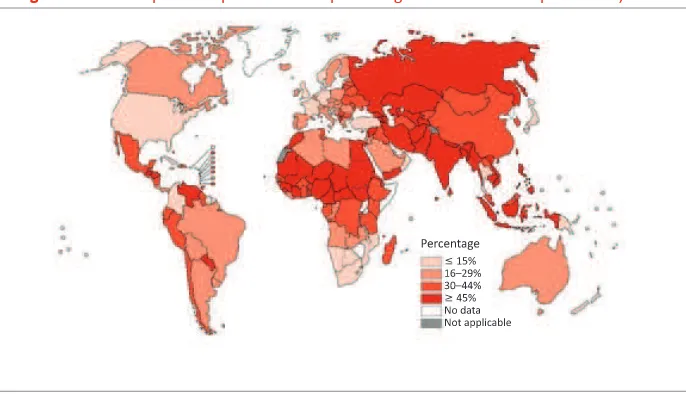
Health inancing data from naional health accounts provide insights into the current status of progress towards universal health coverage (UHC). Two suggested benchmarks required to achieve UHC are that health spending reaches at least 6% of gross domesic product (GDP) and that out-of-pocket expenditures account for less than 15% of total health spending. Most countries, including all of the 22 HBCs (previous HBCs list) and all low-income countries, have not yet reached these benchmarks. Among SEAR Member States, Thailand is closest to
doing so.
Figure 3.1: Out-of-pocket expenditure as a percentage of total health expenditures, 2013
Source: World Health Organizaion. Global tuberculosis report 2015. Geneva: WHO, 2015.
Low noiicaion rate of TB cases: More than 35% of the esimated incident cases in the region are not noiied. These include cases that are either not being detected at all or being detected in sectors that do not noify the case to the naional programme. There are also issues with the following.
§ Delayed diagnosis and treatment of persons with TB, including children;
§ Unregulated and growing private sector; many public and private health providers remain unlinked with naional tuberculosis control eforts and there is insuicient involvement of big hospitals (public and private), lung clinics and other specialized faciliies seeing people with respiratory symptoms;
§ Insuicient progress in scaling up programmaic management of DR-TB (PMDT);
§ Insuicient progress in scaling up TB-HIV collaboraive aciviies;
Persising weaknesses in the health systems
§ Weak health systems:
w Limited access to quality health services;1
w Overstretched and weak performance of health services, not only related to services for people with TB, but limiing access to high-quality tuberculosis care;
w Poor governance and weak accountability mechanisms;
w Shortages of well-trained, moivated and supported health workers and unfair distribuion of them within and across countries; and lack of knowledge or capability in many key areas such as quality assurance;
§ Insuicient data collecion, quality and use of data at all levels;
§ Limited linkages required across social sectors to address poverty, undernutriion and risk factors that adversely inluence people’s vulnerability to tuberculosis, and the health outcomes of people with tuberculosis;
§ Limited programme management capacity with limited involvement of NTPs in decision-making related to the health sector reform processes while NTPs are afected by changes made.
Insuicient management of comorbidiies
§ Risk factors and comorbidiies of tuberculosis such as diabetes, tobacco smoking, silicosis, alcohol and drug misuse, and undernutriion are oten ignored and not addressed adequately, which hampers tuberculosis control, especially in low- and middle-income countries.
Insuicient regulatory systems and mechanisms
§ Absence of universal health coverage and access to free treatment aggravates the economic burden on the poor. This hardship is compounded by a lack of social protecion mechanisms to address associated income loss and nonmedical costs.
1 Tracking universal health coverage: irst global monitoring report. World Health Organizaion. World
§ Weak regulatory mechanisms essenial to ensure efecive infecion control, raional use of tuberculosis diagnosics and medicines,
mandatory disease noiicaion, funcioning vital registraion systems, and protecion of the legal rights of people with tuberculosis.
Absence of long-term strategies to address the underlying social
determinants
Source: World Health Organizaion. The end TB strategy. htp://www.who.int/tb/strategy/en/ - accessed 15 February 2015.
In May 2014, the World Health Assembly in its resoluion WHA67.1 adopted the global strategy and targets for tuberculosis prevenion, care and control ater 2015 based on a bold vision of a world without tuberculosis and targets of ending the global tuberculosis epidemic, eliminaion of associated catastrophic costs for tuberculosis-afected households. The three pillars of the strategy include – integrated, paient-centred care and prevenion; bold policies and supporive systems; and intensiied research and innovaion. The strategy is based on principles of government stewardship and accountability, with monitoring and evaluaion; strong coaliion with civil society organizaions and community; protecion and promoion of human rights, ethics, and equity; and adaptaion of the strategy and targets at the country level, with global collaboraion.
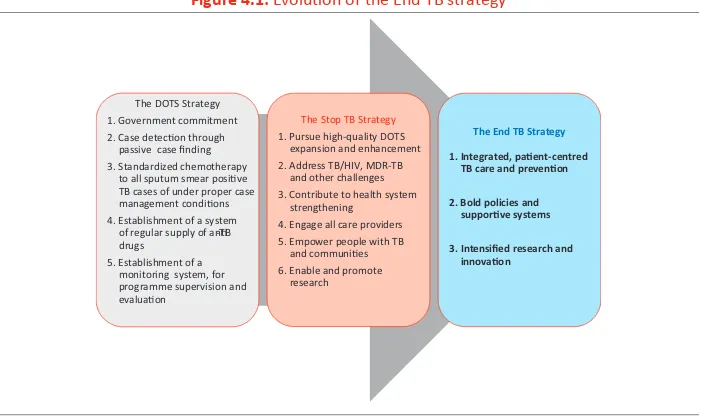
Figure 4.1: Evoluion of the End TB strategy
The DOTS Strategy
1. Government commitment 2. Case detecon through
passive case finding 3. Standardized chemotherapy
to all sputum smear posive TB cases of under proper case management condions
4. Establishment of a system of regular supply of an-TB drugs
5. Establishment of a monitoring system, for programme supervision and evaluaon
The Stop TB Strategy
1. Pursue high-quality DOTS expansion and enhancement
2. Address TB/HIV, MDR-TB and other challenges
3. Contribute to health system strengthening
4. Engage all care providers 5. Empower people with TB
and communies
6. Enable and promote research
The End TB Strategy
1. Integrated, paent-centred TB care and prevenon
2. Bold policies and supporve systems
3. Intensified research and innovaon
Graph 4.1: The eforts required to reach the intended targets
Opmize use of current & new tools emerging from pipeline,
pursue UHC and social protecon, substanal investments in research
-10%/year by 2025
-17%/year
Current global trend: -1.5%/year
Introduce new tools: a vaccine, new drugs and shorter regimens for treatment of acve TB and latent infecon, a point-of-care test
-5%/year
Source: World Health Organizaion. The end TB strategy. Geneva: WHO, 2015. htp://www.who.int/tb/ End_TB_brochure.pdf?ua=1 – accessed 15 February 2015.
The SEA Region as whole is on track to meet the MDG targets that were to be accomplished by 2015:
§ halving the TB mortality rate – achieved
§ halving the 1990 level of TB prevalence – on track to meet the target by
the end of 2015
§ haling and reversing TB incidence – achieved
This has been possible because of the high TB treatment success rate of more than 88% since 2009 and an increasing case noiicaion: 2.58 million cases of TB noiied in 2014. Table 4.1 provides an overview of country-wise progress in achievement of MDGs in the Region
However, addiional eforts and updaing of strategies is required with renewed vigour to atain the End TB strategy goals. Acion needed by Member States is as follows.
1. Reairm commitment to eliminate TB as a public health problem by
adaping the End TB strategy;
2. Revise and implement the naional tuberculosis strategic plans in line
3. Secure adequate inancing for implemening and monitoring all tuberculosis speciic, health sector-related and mulisectoral acions proposed in the End TB Strategy, taking into consideraion variaions in the epidemiological, socioeconomic and health system contexts; 4. Engage a wide range of stakeholders in the implementaion of the
strategy, including local, naional, regional and internaional partners, as well as stakeholders from within and beyond the health sector.
Acions planned by WHO Regional and Country oices to support Member States:
5. Advocate from the highest level poliical commitment and increased
funding from naional and internaional sources to support TB eliminaion eforts in the Region;
6. Provide guidance to Member States on how to adapt and operaionalize
the End TB Strategy, including development of a Regional Strategic Plan for intervenions in the period 2016–2020 towards TB eliminaion; 7. Assist Member States with implementaion of the strategy, and evaluate
the impact in terms of progress towards set milestones and targets; 8. Promote equitable access to new tools and medical products for the
prevenion, diagnosis and treatment of tuberculosis and
lo
Country Year (excluding HIV) rate
(esimates) (esimates)
HIV) all forms number (thousands)
(including HIV) rate
relapse number (thousands)
Bangladesh 1990 80 (53–106) 504 (228–8879 240 (200–310) 226 (183–289) 48 673
2014 51 (37–68) 404 (211–659) 360 (320 – 410) 227 (200–256) 191 166
Bhutan 1990 277 (191–326) 1760 (827–3040) 4.2 (3.8–4.5) 770 (707–841) 1 154
2014 9.5 (5.1–15) 190 (75–359) 1.3 (1.1–1.4) 164 (148–181) 1 066
Democraic People’s Republic of Korea
1990 110 (105–224) 480 (130–1050) 78 (59–100) 384 (292–515) No data
2014 20 (7.9–37) 552 (150–1 210) 110 (100–120) 442 (412–473) 13 045
India 1990 38 (25–54) 465 (415–518) 1 900 (1 700–2 100) 217 (200–242) 1 519 182
2014 17 (12–27) 195 (131–271) 2 200 (2 000–2 300) 167 (156–179) 1 609 547
Indonesia 1990 70 (47–89) 443 (211–760) 370 (320–440) 206 (177–249) 74 470
2014 41 (26–59) 647 (513–797) 1 000 000 (700–1 400) 399 (274 546) 322 806
Maldives 1990 29 (27–31) 285 (140–480) 0.32 (0.250–0.400) 146 (116–187) 152
2014 2.3 (1.9–2.8) 56 (25–98) 0.15 (0.13–0.17) 41 (36–47) 131
Myanmar 1990 154 (106–193) 894 (414–1550) 170 (140–200) 395 (341–473) 12 416
2014 53 (38–70) 457 (352–575) 200 (180–220) 369 (334–406) 138 352
Nepal 1990 52 (32–70) 348 (162–602) 30 (24–38) 164 (133–210) 10 142
2014 17 (12–24) 215 (102–369) 44 (39–50) 158 (139–178) 35 277
Sri Lanka 1990 7.6 (4.5–12) 111 (57–184) 11 (9.4–15) 66 (54–84) 6 666
2014 6.1 (4.8–7.6) 99 (51–164) 13 (12–15) 65 (57–73) 9 305
Thailand 1990 19 (6.3–40) 211 (110–346) 78 (70–87) 138 (123–154) 46 510
2014 11 (5.7–18) 236 (161–326) 120 (61–190) 171 (90–276) 67 722
Timor-Leste 2002 89 (48–145) 809 (381–1390) 4.5 (3.6–5.4) 498 (406–601) 2 760
Vision and goal
The vision for TB control in the SEA Region is to have a Region free of TB with zero
death, disease and sufering due to TB. All Member States can adopt this vision in naional strategies and plans.
The goal for TB control in the SEA is to End the TB epidemic in the Region by 2035, by adoping and adaping the vision, milestones and targets as outlined in
the WHA67.1 resoluion.
Objecives
The overall objecives of the plan are to:
§ advance universal access to high-quality care for all people with TB as part of robust health systems
§ reduce the human sufering and socioeconomic burden associated with TB
§ protect vulnerable populaions from TB, TB/HIV, and drug-resistant TB
§ roll out new tools and enable their imely and efecive use
§ protect and promote human rights in TB prevenion, care and control.
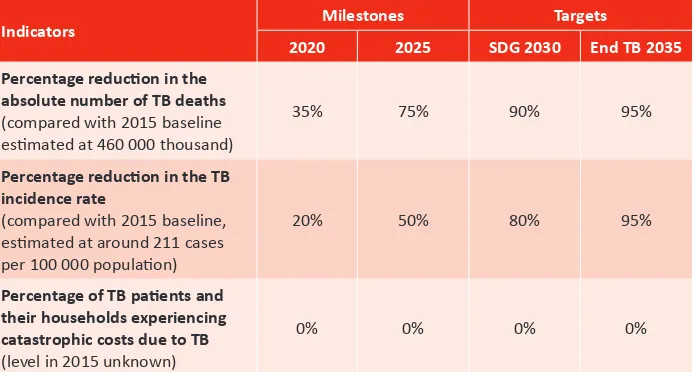
Regional targets and milestones
With the goal of ending TB in the SEA Region by 2035, this Regional Strategic Plan provides guidance for the irst 5 years, 2016–2020 towards this date. Ending the regional TB epidemic is deined as reducing the regional burden of TB disease to ≤10 cases per 100 000 populaion. For comparison, regionally there was an esimated 183 (175–192) cases per 100 000 populaion in 2013.
The Regional Strategic Plan to End TB 2016–2020 includes three high-level, overarching indicators, and corresponding regional targets and milestones as detailed in Table 4 below. The long-term regional targets for 2030 reducions in TB cases and deaths correspond to the end date of the United Naions’ post-2015 Sustainable Development Goal framework, within which targets have been set for 2030.2 The SDG framework includes the End Strategy’s 2030 targets for reducions
2 The SDGs provide a new development framework for 2016−2030, replacing the 2000−2015 Millennium
in TB cases and deaths as part of a health-related subgoal. The corresponding regional milestones are for 2020 – the period covered by this strategic plan (Table 5.1).
Table 5.1: The Regional Strategy to End TB – three high-level regional indicators and associated targets and milestones
Indicators Milestones Targets
2020 2025 SDG 2030 End TB 2035
Percentage reducion in the
absolute number of TB deaths (compared with 2015 baseline esimated at 460 000 thousand)
35% 75% 90% 95%
Percentage reducion in the TB
incidence rate
(compared with 2015 baseline, esimated at around 211 cases per 100 000 populaion)
20% 50% 80% 95%
Percentage of TB paients and
their households experiencing catastrophic costs due to TB (level in 2015 unknown)
0% 0% 0% 0%
Source: World Health Organizaion, Regional Oice for South-East Asia. Ending TB in South-East Asia – Regional Strategic Plan 2016–2020. New Delhi: WHO-SEARO, 2015.
The third high-level indicator, the percentage of TB paients and their
households experiencing catastrophic costs as a result of TB, is chosen because of its direct link to progress towards universal health coverage and universal social protecion. UHC is deined as “all people who need health services (promoion, prevenion, treatment, rehabilitaion and palliaion) receive them, without undue inancial hardship. It has two interrelated components: the full spectrum of good-quality essenial health services according to need, and protecion from inancial hardship, including possible impoverishment, due to out-of-pocket payments for
health services.”3 Social protecion includes replacement of income when this is
Graph 5.1: Projected regional trajectory of TB incidence and TB death 2015–2035 in the South-East Asia Region. Doted line represening the current trend; coninuous line represening
needed decline to reach targets
Source: Ending TB in South-East Asia – Regional Strategic Plan 2016–2020. WHO-SEARO.
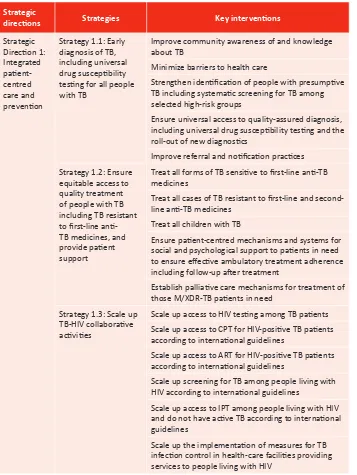
Strategic direcions and intervenions
The strategic direcions, areas of intervenions and aciviies to reach the overall goal, vision, objecives and targets to End TB are grouped under the following 3 strategic direcions:
1. Integrated paient-centred care and prevenion
2. Bold policies and supporive systems
3. Intensiied research and innovaion.
Implementaion of strategies and intervenions under the three strategic direcions requires the combined eforts as well as close coordinaion and
Table 5.2: Strategic direcions, strategies and key intervenions of the Regional Strategic Plan to End TB in SEAR, 2016–220
Strategic
direcions Strategies Key intervenions
Strategic
Strategy 1.1: Early diagnosis of TB, including universal drug suscepibility tesing for all people with TB
Improve community awareness of and knowledge about TB
Minimize barriers to health care
Strengthen ideniicaion of people with presumpive TB including systemaic screening for TB among selected high-risk groups
Ensure universal access to quality-assured diagnosis, including universal drug suscepibility tesing and the roll-out of new diagnosics
Improve referral and noiicaion pracices Strategy 1.2: Ensure
equitable access to quality treatment of people with TB including TB resistant to irst-line ani-TB medicines, and provide paient support
Treat all forms of TB sensiive to irst-line ani-TB medicines
Treat all cases of TB resistant to irst-line and second-line ani-TB medicines
Treat all children with TB
Ensure paient-centred mechanisms and systems for social and psychological support to paients in need to ensure efecive ambulatory treatment adherence including follow-up ater treatment
Establish palliaive care mechanisms for treatment of those M/XDR-TB paients in need
Strategy 1.3: Scale up TB-HIV collaboraive aciviies
Scale up access to HIV tesing among TB paients Scale up access to CPT for HIV-posiive TB paients according to internaional guidelines
Scale up access to ART for HIV-posiive TB paients according to internaional guidelines
Scale up screening for TB among people living with HIV according to internaional guidelines
Scale up access to IPT among people living with HIV and do not have acive TB according to internaional guidelines
Strategic
direcions Strategies Key intervenions
Strategy 1.4:Ensure screening for and management of comorbidiies
Ensure integrated management at primary health-care level of TB comorbidiies and noncommunicable diseases of documented risk such as diabetes Rouinely assess elderly people atending health services and other insituions
Strategy 1.5:Ensure prevenive treatment of people at high risk; and vaccinaion against TB
Expand prevenive treatment of people with high risk of tuberculosis, especially children below 5 years of age in close contact with adults afected with TB Ensure that WHO recommendaions on BCG immunizaion are implemented through the EPI Strategic for TB prevenion care and control
Update naional strategic plans for TB prevenion, care and control
Mobilize adequate resources for the implementaion of the naional strategic plan
Strengthen programme management capacity at all levels Strengthen human resource development
Scale up implement comprehensive infecion control measures in health-care faciliies
Strengthen management of ani-TB medicines Strengthen the TB surveillance systems including new standards and benchmarks
Improve TB prevenion, care and control in the peniteniary services and other non-MOH health services
Strategy 2.3: Improved regulatory frameworks including universal health coverage policy
Move with urgency to universal health coverage including equitable and full access to TB speciic tests and treatment, minimizing geographical and inancial barriers to services
Enforce mandatory noiicaion of tuberculosis cases Ensure recording of tuberculosis deaths within vital registraion systems
Strategic
direcions Strategies Key intervenions
Strategy 2.4: Engage communiies, civil society organizaions and all public and private-care providers
Engage civil society organizaions such as NGOs and CBOs in community-based TB prevenion, care and control services
Scale up public-private and public-public mix approaches and promote the Internaional Standards for Tuberculosis Care
Strategy 2.5: Address social protecion, poverty alleviaion and acions on other determinants of tuberculosis
Expand coverage of social protecion schemes to cover needs associated with tuberculosis beyond free diagnosis and treatment
Address poverty and related risk factors through “health–in–all policies” approaches impact and promote innovaion
Create a research-enabling environment
Establish mechanisms for collaboraion in planning and implementaion of research aciviies between all stakeholders
WHO supports global health promoion by providing leadership on maters criical to health and engaging in partnerships where joint acion is needed; shaping the research agenda and simulaing the generaion, translaion and disseminaion of valuable knowledge; seing norms and standards and promoing and
monitoring their implementaion; ariculaing ethical and evidence-based policy opions; providing technical support, catalysing change, and building sustainable insituional capacity; and monitoring the health situaion and assessing health
trends.
All 11 Member States in the Region coninue to receive technical assistance through the WHO Regional Oice for South-East Asia and respecive WHO country oices, in coordinaion and collaboraion with internaional technical partners, namely the Centers for Disease Control and prevenion (CDC), USA; the Royal Foundaion for Tuberculosis in the Netherlands (KNCV); U.S. Agency for Internaional Development (USAID); USAID supported Challenge TB project, Foundaion for Innovaive New Diagnosics (FIND); PATH; the Insitute of Tropical Medicine in Antwerp, Belgium; and The Union. There are ive WHO Collaboraing Centres in the Region, namely All India Insitute of Medical Sciences (AIIMS), Delhi, India; Naional TB Insitute (NTI), Bangalore, India; Naional Insitute of Research in Tuberculosis (NIRT), Chennai, India; Naional Insitute of TB and Respiratory Diseases (NITRD), Delhi, India; and the SAARC TB and HIV/ AIDS Centre in Kathmandu, Nepal. Technical missions were undertaken to all 11 Member States during 2015 to provide support to naional programmes in various areas. These areas include laboratory assessments and laboratory capacity-building; strengthening laboratory quality control and assurance; culture and drug-sensiivity tesing; introducion of rapid molecular tests; development and implementaion of guidelines and/or naional strategies for TB; human resource development for TB control; MDR-TB, TB-HIV, childhood TB, infecion control, PPM; improvement of drug procurement and supply management, data management and use; and impact assessments.
Transiioning to the End TB Strategy
plan are discussed in an earlier secion. The updated plan adopts key principles and strategies, pillars and components (integrated, paient-centred care and prevenion, bold policies and supporive systems, intensiied research and innovaion) of the global “End TB Strategy: 2016–2035”. The updated Regional Strategic Plan aims to support member countries for reducion in TB mortality and incidence in line with the global goals in resoluion WHA67.1, to guide countries in addressing the persising and emerging epidemiological and demographic challenges, and to advance universal health coverage and robust health systems.
The WHO Regional Oice and Country Oices are providing support to countries to develop or revise Naional Strategic Plans (NSP) covering the post-2015 period in alignment with the End TB Strategy. This year, the support was provided to Nepal and Thailand to develop a costed naional strategic plan for TB control. All other countries were supported in implementaion of the exising
plans.
WHO headquarters and organized an End TB summit for 30 high-burden countries in Cape Town, South Africa. The Regional oice through country oices coordinated suicient representaion of naional programme representaives to the summit from the Regional high-burden countries.
Diagnosic capacity-building
Technical assistance, on laboratory issues such as upgrading and capacity building of naional reference laboratories, quality assurance, ceriicaion and, introducion and roll-out of newer diagnosics is coordinated by WHO through the Supra Naional Reference Laboratory (SNRL) network. Such laboratories are based at the Insitute of Medical and Veterinary Science (Australia), Insitute of Tropical Medicine (Belgium), Central Reference Laboratory, Gauing (Germany), Naional Insitute of Research in Tuberculosis (India), Naional Tuberculosis Insitute (India), Bureau of TB (Thailand) and Department of Health, SAR (Hong Kong). All 11 countries have formally established linkages with SNRLs. Addiionally, India receives support from the newly established SNRL-Naional Centre of Excellence (SNRL-CE) at the Naional Insitute of TB and Respiratory Diseases in New Delhi, which belongs to the NRL network and has similar terms of reference to that of an SNRL but with an in-country focus.
with SNRL) and four countries developed capacity for quality-assured second-line DST.
The WHO Regional Oice has been collaboraing with the Global Laboratory Iniiaive (GLI), the Foundaion for Innovaive New Diagnosics (FIND) and GDF to ensure access to quality-assured new diagnosic technologies in various countries under the EXPAND-TB (Expanding Access to New Diagnosics for TB) Project inancially supported by UNITAID. The project has been acive in Bangladesh, India, Indonesia and Myanmar.
In 2015, an addiional technical support mission was undertaken for
Bangladesh, Myanmar and Timor-Leste. A proposal to support diagnosic capacity expansion in Bhutan is under consideraion. In 2015, representaives of the NTP of Democraic People’s Republic of Korea were supported for training in Culture and DST at the SRL Hong Kong.
Expansion of DR-TB services
To provide coordinated and quality support for the implementaion and expansion of programmaic management of drug-resistant TB (PMDT), the Regional Green Light Commitee (rGLC) was established in 2012 with its secretariat housed in the WHO Regional Oice. The rGLC acts as an advisory body performing in accordance with the memorandum of understanding between the GF and WHO. Its main objecive is to provide decentralized monitoring and guidance on new policies and strategies for PMDT intervenions in countries of the Region for rapid scale-up of DR-TB services. The rGLC in SEAR is sscale-upporing the implementaion of the Regional Response Plan for MDR-TB, ensuring that country PMDT plans relect programmaic recommendaions on the response to DR-TB, including recording and reporing of the standard indicators selected for the SEA Region. The rGLC through its secretariat coordinates monitoring missions to countries to assess the progress in implementaion of services, and undertakes peer review of monitoring missions’ reports. As a follow-up to these monitoring missions, the rGLC supports the organizaion of high-quality technical assistance and resource mobilizaion for countries in accordance with the PMDT expansion plan.
intensify case screening by prioriizing groups at risk of drug resistance and develop algorithms for increased use of WHO-approved rapid diagnosics; enhanced technical support for laboratory expansion through the SRLs; paient-centred care with increased involvement of paient groups and community members; strengthened infecion control; and drug resistance surveys to esimate the burden of resistance to irst-line TB drugs. The rGLC is also working towards idenifying regional and naional centres of excellence in MDR-TB management at the regional level to provide decentralized and sustained technical support for PMDT.
With the assistance of the rGLC, monitoring missions were conducted in Bhutan, Democraic People’s Republic of Korea, Indonesia, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste to assess implementaion status and idenify any botlenecks to expansion. Technical support to update PMDT guidelines and PMDT expansion plans were provided to Bhutan and Sri Lanka.
through various approaches including capacity-building in the sector to ensure quality MDR-TB care; HR planning in alignment with PMDT expansion plan; and operaional feasibility of universal insurance coverage for DR-TB.
Strengthening TB/HIV collaboraion
Considerable scale-up of collaboraive TB/HIV aciviies has been reported in a majority of the countries in the Region. However, coverage needs to be expanded and the collaboraion between TB and HIV control programmes needs further strengthening in all Member States to ensure universal HIV counselling and tesing for all TB paients, the availability of co-trimoxazole prevenive therapy and ART for all eligible TB paients coinfected with HIV as well as INH prevenive therapy, and airborne infecion control in health-care faciliies. Mobilizaion of HIV groups and afected communiies to advocate for the provision of TB prevenion, treatment and care services to all people living with HIV is crucial for the successful implementaion of the listed intervenions. It is equally important to have epidemiological assessment of TB/HIV coinfecion in countries to target aciviies and adequate resource mobilizaion.
In 2015, assistance was provided for development of TB/HIV seroprevalence survey protocol in Bangladesh. As part of resource mobilizaion aciviies,
Indonesia also developed a joint TB/HIV concept note for funding support through the GF.
Capacity-building and informaion exchange
Training and exchange of informaion at the global and regional levels, as well as in-country capacity-building have been the key areas of work for the WHO Regional Oice and country oice during the past few years. WHO in the Region supported the facilitaion of several naional level trainings and workshops in all countries through Regional and country oices and where needed, with support from the HQ. Country staf also facilitate workshops and trainings organized by the NTP and partners. Some of the key Regional meeings and trainings held during the year include:
§ 6th meeing of the SEA Regional Advisory Commitee on MDR-TB (rGLC),
§ Regional and country oice staf paricipated in STAG meeing along with workshop on END TB strategy, Geneva, 15-20 June 2015
§ Regional representaion was also made on the Global Drug-resistant TB Iniiaive (GDI) and Global Laboratory Iniiaive (GLI) combined meeing as well as the GDI core group meeings
§ NTP Managers’ meeing held in Sri Lanka, 26-30 October 2015
§ 7th Meeing of the SEA Regional Advisory Commitee on MDR-TB (rGLC) in
Myanmar, 10-12 August 2015
§ Childhood TB and PPM workshop, Nepal, November 2015
§ Regional and country oice staf along with NTP representaives also paricipated in the irst END TB summit for 30 high-burden countries, Child-TB subgroup and PPM subgroup meeings, South Africa, 2-6 December 2015
Drug supply and management
All eleven countries in the Region use the Global TB Drug Facility (GDF) services and products for access to the low-cost and quality-assured ixed dosage combinaion drugs as well as second-line drugs (in part or completely). No stock-outs were reported from any country at the point of treatment delivery.
The rGLC secretariat coninued to support the GDF by reviewing the applicaions for second-line drugs to check appropriateness of drugs used and the regimen, and quaniicaion in accordance with planned expansion of MDR-TB services. This ensured imely supply of quality-assured drugs in adequate amounts.
Rouine surveillance
Technical support was provided to several countries for strengthening rouine surveillance systems. Eforts are being made to strengthen naional TB
surveillance systems, focussing on quality of data, with emphasis on completeness of case reporing, accurate compilaion and implemening of new reporing framework.
infecion surveys, mortality surveys, in-depth analysis of several years’ programme data to determine trends, revision of burden esimates.
In 2015 support to prevalence survey and analysis of results was provided to various countries. Thailand received support in disseminaion of the results of the prevalence survey completed on 2014; Indonesia was supported in the review of results inalized earlier; Bangladesh and Democraic People’s Republic of Korea received support in iniiaion and implementaion of the TB prevalence survey. Preparaions for a prevalence survey in Nepal are under way and a ield visit for observaion was organized this year for the NTP.
Assistance to India and Indonesia was provided this year in implementaion of the Naional DRS ater development of DRS protocol in 2014. Protocol for DRS developed by Sri Lanka NTP is currently under review.
WHO also provided technical support to several countries for strengthening rouine surveillance systems. Eforts are being made to strengthen naional TB surveillance systems, focusing on quality of data, with main emphasis on completeness of case reporing, accurate compilaion and reporing of data, and implementaion of the new reporing framework.
Operaional research
Achievement of targets envisaged in the End TB strategy in 2035, require intensiied, programme based research not only to develop new tools and drugs but also their adapion and roll-out in country context. These novel tools, as well as any innovaion, must be linked with relevant epidemiological, health system, and operaional research to ensure their adopion and implementaion to scale. Programme-based operaional research speciically aimed at developing intervenions that result in improved policy-making, beter design and
implementaion of health systems, as well as more eicient methods of service delivery is necessary to opimize TB control and determine the best ways of implemening and monitoring intervenions.
operaional research on use of ambulatory care of MDR-TB treatment. Technical assistance is on-going to India and Indonesia to scale up implementaion of PPM
approach.
Resource mobilizaion
Member States were also assisted in resource mobilizaion from development partners and donor agencies during the past year. Indonesia, Sri Lanka and Timor-Leste were supported to develop a Concept Note for the Global Fund support under the New Funding Model (NFM). Indonesia developed a joint TB/HIV Concept Note.
All countries (except Maldives) receive support for management of GF grants and funding. Maldives also intends to apply for funding under the NFM in 2016.
In addiion to the GF, the Region also receives support from USAID in the form of the Challenge TB project currently acive in Bangladesh, India and Indonesia and the CAP-TB project in Myanmar. Commodity grants are available from the GDF and UNITAID. Other donors also have country-speciic agreements.
Axshya project supported by The Global Fund
Supported by the Global Fund and implemented by The Union in 300 districts across 21 States of India through eight civil society organizaion partners, Project Axshya coninued its innovaive intervenions to intensify outreach to those with the greatest diiculty in accessing TB diagnosis and treatment. During January to December 2014, Axshya has facilitated ideniicaion and tesing of over 300 000 TB symptomaics, including sputum collecion and transportaion of nearly 250 000 cases, resuling in diagnosis and treatment iniiaion of over 25 000 paients.
The various intervenions undertaken by the project during this period include:
§ Early diagnosis and treatment iniiaion through Axshya SAMVAD
(Sensiizaion and Advocacy in Marginalized and Vulnerable areas of
District). During January-December 2014, over 3.8 million households in
vulnerable areas have been reached resuling in tesing of nearly 140 000 TB symptomaics, and over 10 000 paients being diagnosed and put on treatment.
§ Sputum collecion and transportaion services - Over 245 000 TB symptomaics beneited from the sputum collecion and transportaion
services during this period.
§ The project has trained and engaged 2500 Rural Health-Care Providers (RHCPs) and AYUSH providers who have ideniied nearly 51 000 TB symptomaics resuling in diagnosis of over 4200 TB paients. Nearly 25% of the trained RHCP and AYUSH are also serving as DOT providers.
§ The project has so far ideniied 6100 such villages under Axshya Villages
(TB-Free Village) reaching out to over 930 000 people through more than
65 000 community meeings. To empower the afected community, the project has facilitated creation of over 250 TB forums at the district level.
§ To ensure early diagnosis and treatment of TB among the high-risk PLHIV, over 240 TIs, DLNs and CSCs have been sensiized on TB care and control.
§ The project has sensiized nearly 3500 NGOs on RNTCP schemes of which 705 have submited applicaions and 82 schemes have been successfully
§ A toll-free TB helpline has been iniiated in the States of Punjab, Karnataka and Maharashtra.
§ The project is providing services for regular prevenive maintenance and addressing breakdown for over 5 000 BMs in nine States.
§ Through Axshya, The Union is providing technical support to RNTCP in the areas of ACSM, PPM and M&E at the naional level and nine ideniied States (Bihar, Jharkhand, Chhaisgarh, Punjab, Karnataka, Madhya Pradesh, Maharashtra, Utarakhand and Utar Pradesh) for ACSM.
§ To address the high loss to follow up among drug-resistant TB (DR-TB) paients, Axshya has iniiated a pilot ofering counselling services to facilitate treatment adherence of DR-TB paients (MDR and XDR-TB) across 30 districts in the country.
§ The Union through Axshya coninues capacity-building on key themaic areas including TB epidemiology, operaional research (OR), clinical management of DR-TB, and leadership and management. Over 125 personnel working with RNTCP have been trained in these courses during January–December 2014.
§ The Naional Partnership for TB Care and Control, supported through Project Axshya, has networked with Civil Society Organizaions across the country that are interested in TB control. The strength of the partnership has increased signiicantly in the last two years, and 180 partners have joined the partnership.
EXPAND-TB project
(in partnership with BMGF, FIND, GF, UNITAID and WHO)
Bangladesh
India
FIND in India is supporing use & policy development on newer TB diagnosics via demonstraion & evaluaion studies, building naional capacity of newer rapid TB diagnosics and acceleraing access to new TB diagnosics. FIND has supported the Central TB Division in establishing 40 Liquid Culture & DST, 46 Line Probe Assay and 38 GeneXpert sites in the country under projects supported by UNITAID, GFATM and BMGF. While the UNITAID funded EXPAND-TB project provisioned equipment, test kits and consumables; GFATM complemented this scale-up by supporing infrastructure up-gradaion, lab capacity enhancement, addiional lab HR and on-site trainings.
Till end of 3rd quarter 2015, 42 LPA, 35 LC and 38 Xpert sites had been
established and supported by FIND and a total of 742,264 TB tests had been conducted in these faciliie and 78,709 MDR-TB cases detected at these sites.
In early 2011, FIND established the Internaional Centre for Excellence in Laboratory Training (ICELT) at the Naional TB Insitute in Bangalore with support from GLI, WHO, and UNITAID. This centre has played a pivotal role in scaling up of laboratory capacity in India. ICELT provides hands-on training courses on newer TB diagnosics, and on biosafety and infecion control measures. ICELT also trains master trainers to build experise required for scale-up and sustainability. FIND has supported training of close to 2500 laboratory personnel through the ICELT facility and on-site trainings
Indonesia
In Indonesia FIND has helped establish two Liquid Culture & DST and two Line Probe Assay (LPA) laboratories by providing equipment, consumables and
essenial supplies through EXPAND-TB project. 797 MDR-TB cases were diagnosed between 2013 and 2014 in the country.
Myanmar
Global TB Drug Facility (GDF)
GDF, housed in the Stop TB Partnership, has been an important partner in the Region supporing supply of low-cost quality-assured irst- and second-line drugs as well as providing technical support in strengthening the supply chain management systems within countries.
Highlights of the GDF support in the Region for 2015 include:
§ Stop TB/UNOPS has approved the applicaion from the Government of Democraic People’s Republic of Korea for the excepional support for a 1-year adult and paediatric grant for the Jagang province where there is no support from the Global Fund, acknowledging the extenuaing circumstances faced by the Ministry of Public Health of Democraic People’s Republic of Korea.
§ The quaniicaion exercise further to the monitoring mission conducted in Bhutan highlighted an early warning risk of stock-out for SLDs. Appropriate measures have since been taken and needed medicines have been made immediately available from the GDF Strategic Rotaing Stockpile or diferent orders.
§ The quaniicaion exercise further to the monitoring mission conducted in Sri Lanka highlighted an early warning risk of stock-out for FLDs. Appropriate measures have since been taken and the best cost-efecive price quotes proposed according to the programme’s requirement.
§ Monitoring missions for review of the commodiies supply chain and providing technical support for strengthening systems have also been undertaken in Bangladesh, Myanmar and Timor-Leste.
§ There is ongoing support for the procurement of medicines and diagnosics commodiies in the Region.
Graph 7.1: Overview of procurement support per product line: products (FLDs, SLDs and diagnosics) already delivered in each year and product expected to be delivered (orders already conirmed/placed with suppliers with shipments in pipeline and orders in drat status)
USD 120 000 000
USD 100 000 000
USD 80 000 000
Graph 7.2: Overview of procurement support per country: breakdown per country/year
USD 120 000 000
USD 100 000 000
USD 80 000 000
Democratic Republic of Timor-Leste Maldives
Democratic People’s Republic of Korea Indonesia
Paediatric TB project
FIND, in consultaion with the Revised Naional TB Control Programme of India (RNTCP) and with funding support from USAID and CDC, has been implemening a novel iniiaive from February 2014 aimed at the diagnosis of TB in children in Delhi, Kolkata, Chennai and Hyderabad. Under the project, Xpert MTB/Rif was ofered as an upfront diagnosic test for paediatric TB diagnosis for the irst ime in Indiain both pulmonary and extrapulmonary samples. The project has been focusing on Public-Private Mix (PPM) aciviies targeing paediatric populaions in key ciies, in order to build the paediatric diagnosic capacity in both the public and private sector; for this purpose, one high throughput Xpert lab was established in each of the four ciies at RNTCP sites. Upfront Xpert-based diagnosis was ofered to all children showing symptoms of pulmonary and extra-pulmonary TB from linked faciliies free of cost through a hub-and-spoke model. Rapid specimen transportaion and a reporing mechanism using email and SMS was also established for same-day transportaion and reporing.
TB REACH project
Project Highlight: India
Asha Kalp
India’s tribal and indigenous people oten have poor access to TB care services because they live in isolated and insular communiies; the Saharia tribes of Madhya Pradesh province are no excepion.
Asha Kalp used community health workers to act as an extension of the India NTP in Saharia communiies. These health workers verbally screened the tribes people for symptoms of TB, and specimens are collected in the community and transported to the nearest laboratory for tesing. TB paients are then started on treatment in the community.
Between July and December 2014, over 25 000 individuals were screened, resuling in the detecion of more than 450 smear-posiive TB paients. These aciviies resulted in a +89.4% increase in TB treatment compared with the previous year.
This remote and tribal populaion has an extremely high TB burden. The rate of smear-posiive TB alone in this community (1767 smear-smear-posiive TB cases per 100 000 populaion) is over 8 imes that of India’s naional all forms TB noiicaion (-211 all forms TB cases per 100 000). The scale-up and replicaion of impacful community intervenions, which alleviate the barriers in accessing care, will be essenial to achieve the ambiious post-2015 targets.
Project Highlight:Indonesia
Yayasan Menara Agung Pengharapan Internasional
South Nias Regency is one of the most underdeveloped areas in Indonesia. Due to the lack of human resources and the high transportaion costs among more than 100 remote islands, many TB paients are not able to access care.
Indigenous community volunteers were recruited and trained to screen for symptoms of TB as part of a comprehensive maternal child health and nutriion programme. Individuals presumed of having TB were then referred to a health facility to smear microscopy. Volunteers facilitated transportaion to ensure tesing. When a TB paient was detected, the volun -teers helped to iniiate and follow up treatment on the remote islands. In addiion to these community-based aciviies, laboratory technicians were trained and monitored to improve the quality of diagnosic services ofered through government health faciliies.
Over 50 000 people were screened for symptoms of TB in 112 villages in just 3 quarters. These aciviies resulted in the detecion of over 225 posiive TB paients, including 44 smear-posiive paients among children (an impressive feat given the paucibacillary presentaion of disease in children). These acive case-inding aciviies resulted in 86% increase in TB noiica -ions compared with the previous year.