A Systematic Review on the Effectiveness of Nurse-led Interventions to Promote Healthy Lifestyles of Clients in Primary Healthcare
Damayanti S, MR
Nursing Program, Faculty of Medicine Udayana University [email protected]
Background:
Health promotion provision is regarded as an integral component of the health professional’s role, particularly for nurses working in a primary healthcare. However, the prevailing evidence leaves in question the effectiveness of health promotion interventions through which nurses promote healthy lifestyles to clients in primary healthcare.
Objective:
To specifically identify the effectiveness of nurse-led interventions for promoting healthy lifestyles amongst clients in primary healthcare, and this shown by several changes in behavioural indicators and clinical outcomes.
Methods:
A computerized literature search was carried out to find studies that fulfil the inclusion criteria. The search period was 1st of January 1995 through recent date. The search was restricted to studies undertaken in human and reported in English. The identified original publications were assessed based on the relevance of the titles and the inclusion criteria. Duplication publications were eliminated. The relevant publications were then assessed independently for their methodological rigor by three reviewers. The standardised assessment and review instrument and the standardised data extraction tool for experimental studies from the Joanna Briggs Institute were employed.
Results:
The most relevant ten publications passed the critical appraisal step. All studies involving randomised controlled trials with a mixed methodological quality. The participants in the studies represented diverse groups of the population. The studies’ interventions varied widely, from single-focus interventions to those applied across several health behaviours (multiple risk factors); and interventions to address coronary heart disease risk factors.
Conclusions:
There is some encouraging evidence that nurse-led interventions are effective in promoting healthy lifestyles amongst the primary healthcare clients. The interventions that appear to be most successful include led nutritional education programs, exercise on prescription, health checks, and nurse-led health promotion consultation. A more focused clinical question and systematic literature search is recommended for further relevant secondary studies. Findings from this review might be useful to inform the development of appropriate health promotion programs targeting primary healthcare clients.
Keywords:
INTRODUCTION
Background
In recent years, a number of studies have been conducted to investigate the link between
non-communicable diseases (NCDs) and their determinants. The mortality and morbidity
related to NCDs are caused by the cumulative effect of metabolic risk factors i.e. overweight
and obesity, high-blood pressure, raised-blood sugar and high-lipid level (1). These metabolic
risk co-morbidities are predisposed by some preventable behavioural risk factors or
NCD-related lifestyles, such as smoking/tobacco use, unhealthy diet, physical inactivity and alcohol
misuse (1, 2). Encouraging people to adopt healthy lifestyles through health promotion (HP)
is one of the interventions endorsed by the World Health Organisation to tackle the
determinants of NCD-related lifestyles (1).
The Ottawa Charter (3, p.1) defines HP as ‘...the process of enabling people to increase
control over, and to improve, their health’. The HP activity is underpinned by a social view of
health; and this means that only by addressing the cultural, environmental, biological,
political and economic factors influencing population’s health can we improve their health
status (1, 4, 5). There are several HP approaches currently in place, focused either on
individuals, groups, communities or whole populations. Naidoo and Wills (6), for instance,
classify the HP strategy into several categories; where each of the approaches represents
different ways of working, namely medical preventive, educational, behaviour change,
empowerment and social-change. Talbot and Verrinder (4) offer another framework to depict
the relationships amongst the available HP strategies, labelled as ‘a continuum of HP
strategy’. This framework shows that interventions which focus on a population’
socio-environmental aspects are placed at one end of the continuum, whilst the individual-focused
interventions occupy the opposite end (4). The socio-environmental approach can be
conducted by creating healthy public policies and supportive environments, and
strengthening community actions (4). The behavioural approach is undertaken by providing
health education or information to improve individuals’ HP skills (4, 7). The
individual-focused interventions also can be delivered through a medical approach by means of
screening, individual’s risk-factor assessment, immunisation and surveillance (4).
HP supported by the structural approach of primary healthcare (PHC) and the Ottawa
Charter (4), is about empowering clients to integrate healthy habits into their lives and to live
component of the health professionals’ role working in PHC context, particularly nurses. Nurses are appropriately positioned to promote healthy-lifestyles (8), as nurses interact with
many people at key points in their lives (9). Indeed, Kendall (10) argues that, nurses remain
the primary advocates and HP providers to clients in PHC settings.
As a first tier of health provision, PHC provides an essential context for HP because of its
unique characteristics. PHC offers a ‘universal access’, because at some point of their lives,
people will come into contact with PHC services. Then, being trusted and regarded as
credible person by the general population, health practitioners working in PHC may have a
greater opportunity to influence people’s knowledge, attitudes and beliefs on health (6). Other
characteristics that may put the PHC centre as an appropriate site to promote people’s healthy
behaviours are its affordable and acceptable services (4). PHC centres also offer better access
because they are located within community settings, and facilitate better communications
between service users and providers as they meet on more equal terms (6). Moreover,
adequate provision of PHC level services will often imply that more specialised
hospital-based services are unnecessary (6), leading to a more cost-effective healthcare practice.
To date, there are quite a lot of primary and secondary studies have been conducted to
investigate the effectiveness of HP interventions within PHC practice led by a large range of
healthcare practitioners addressed to various types of clientele (11-18). The initial literature
search also identified some studies with diverse findings and approaches have been carried
out to assess the effectiveness of nurse-led HP interventions in different settings (19-24).
Other researchers also have investigated the effectiveness of nurse-led HP interventions
compared with those initiated by other health practitioners (25).
These preliminary findings demonstrate that sufficient numbers of studies in HP within
PHC context have been carried out. The studies varied considerably in terms of their target
populations, interventions, and outcomes. However, the prevailing evidence leaves in
question the effectiveness of HP interventions through which nurses promote healthy
lifestyles to clients in PHC. Therefore, this review was carried out to specifically and
systematically search, collate and synthesise studies investigating this phenomenon. Findings
from this review might be useful to inform the development of appropriate HP programs
targeting PHC clients. As nurses are considered to be the frontline staff with pivotal roles in
Review Question/Objectives
The review question was: What is the effectiveness of nurse-led interventions to promote
healthy lifestyles of clients in PHC?
The objective of this review was to specifically identify the effectiveness of nurse-led
interventions for promoting healthy lifestyles amongst clients in PHC, and this shown by
changes in the following behavioural indicators and clinical outcomes:
1. Healthy eating habit, including overweight and obesity indicators
2. Physical activity levels
3. Smoking behaviour
4. Alcohol misuse
5. Morbidity and mortality prevalence caused by lifestyle-related diseases
METHODS
Inclusion Criteria
Types of studies
This review considered studies targeting PHC clients (individuals or groups) who received
nurse-led HP interventions. The studies were conducted either within institutions (e.g.
primary cares, schools, workplaces, etc.) or in community settings (e.g. clients’ homes).
Types of interventions
This review included any nurse-led interventions undertaken to promote healthy lifestyles for
clients in PHC, either single or multiple focus interventions. The included interventions were
those that focused on preventing or delaying onset of diseases by changing from unhealthy
lifestyles to encouraging clients to adopt the healthy ones. Interventions led by other
healthcare practitioners with nurses as the supplementary practitioner or nurse-led HP
conducted outside the PHC context were excluded.
Types of outcomes
This review considered the following primary outcomes:
Changes toward healthier dietary pattern e.g. sufficient intake of fruit and vegetables/fibre, decreased intake of fat and/or sodium
Changes in physical activity pattern e.g. increased physical activity levels
Changes in alcohol intake e.g. a reduction in the amount of daily intake
Clinical outcomes related to morbidity caused by unhealthy lifestyles such as overweight or obesity, high-blood pressure, raised blood sugar and lipid. The longer-term related
morbidity or mortality includes cerebro-vascular diseases, diabetes, cancer and chronic
respiratory diseases.
Types of studies
This review considered any related meta-analysis or systematic reviews of RCTs and
RCTs that evaluate the effectiveness of nurse-led interventions to promote healthy lifestyles
amongst clients in PHC.
Search Strategy
A computerized literature search was carried out to find studies that fulfil the inclusion
criteria. The following databases were searched in April 2013: PubMed, CINAHL and
Scopus. Several keywords were used in combination in the search, namely, health promotion
(Medical Subject Headings ‘MeSH’), nurses (MeSH), primary health care (MeSH). The
search period was 1st of January 1995 through recent date (April 2013). The literature search
was also restricted to studies undertaken in human and was filtered to include only research
reported in English because the reviewer was constrained by time, resource and facilities for
translating the non-English publications. To confirm the search strategy, an experienced
librarian was consulted. The reference database EndNote was used to catalogue the articles
that were identified.
Study Selection
First, the identified original publications were assessed based on the relevance of the
titles. Then, the author read the relevant abstracts using the inclusion criteria previously
mentioned. Screening and eliminating for duplication publications was subsequently
conducted. Having finished these steps, the author read the relevant publications in their
entirety. The relevant publications were then assessed independently for their methodological
rigor by three reviewers.
Assessment of Methodological Quality
The reviewers critically appraised the studies’ methodological validity prior to inclusion
in the review using the standardised Assessment and Review Instrument from the Joanna
that arose amongst the reviewers were resolved through a discussion until consensus was
reached.
Data Extraction
The data from studies which passed the methodological quality assessment process were
extracted from papers using the standardised data extraction tool. This review used the JBI
data extraction form for experimental studies. This tool includes specific details about the
interventions, populations, study methods and outcomes of significance to the review
question and specific objectives.
Data Synthesis
Where applicable, a meta-analysis or statistical pooling to measure the combined effect
(average effect size or single-effect estimate) of the interventions from the chosen literature
would be conducted using the Meta-Analysis of Statistics Assessment and Review Instrument
(JBI-MAStARI). However, due to lack of homogeneity across the included studies it was not
possible to statistically pooling the data. Therefore, the results were reported in a narrative
form to conclude the overall findings on current available approaches concerning nurse-led
interventions to promote healthy lifestyles amongst clients in PHC.
RESULT
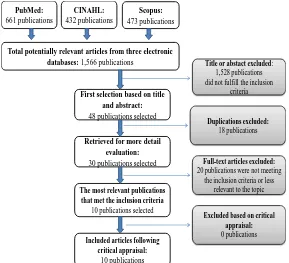
The following figure outlines the processes undertaken to select the publications.
PubMed: 661 publications CINAHL: 432 publications Scopus: 473 publications
Total potentially relevant articles from three electronic databases: 1,566 publications
First selection based on title and abstract:
48 publications selected
Title or abstact excluded: 1,528 publications did not fulfill the inclusion
criteria
The most relevant publications that met the inclusion criteria
10 publications selected
Full-text articles excluded: 20 publications were not meeting
the inclusion criteria or less relevant to the topic Duplications excluded:
18 publications Retrieved for more detail
evaluation:
30 publications selected
Excluded based on critical appraisal: 0 publications
Included articles following critical appraisal:
[image:10.595.154.443.473.736.2]10 publications
The initial search from three databases mentioned above resulted in 1,566 publications.
Forty eight publications were relevant based on the title and abstract. After excluding for
duplications, 30 publications were retrieved for more detail evaluation. This review was
restricted to include only ten publications that met the inclusion criteria, whilst also best
representing the existing literature pertinent to the chosen topic. The most relevant ten
publications were selected for critical appraisal. There was no publication excluded following
the critical appraisal.
Study Type and Quality
The included publications were all studies involving RCTs with a mixed methodological
quality. Eight studies employed a-two-arm study design (21, 26-32), one adopted a-three-arm
RCT (33) and one trial included four intervention arms (34). The size of samples in seven
studies were determined based on sample-size calculations or reported study power (21,
26-28, 30, 32, 33); but three publications did not clearly address this issue (29, 31, 34). To assign
the participants into a treatment group, most of the studies (80%) employed a true
randomisation e.g. using computer-generated randomisations (21, 26, 32) or consecutive
envelopes (30) or other randomisation techniques (28). In two studies, however, the
randomisation technique was not sufficiently described (29) and was limited by the
clinician’s preference and knowledge (34). The allocation concealment was explicitly
indicated only in one study (26), whilst the rest of the studies provided unclear explanation or
simply did not mention this matter. Almost all of the studies (90%) randomised the
participants at individuals level, except the one conducted by Lock et al. (27) which adopted
a cluster randomisation at practice level. Then, unlike the majority of studies which were
unable to mask the interventions from either participants or those assessed the outcomes (21,
29-32, 34); Lock et al. (27) were able to blind both of their participants and outcome
assessors. In some studies, the researchers managed to mask the outcomes assessors only (26)
or employed independent assessors who were blinded to treatment allocations (28, 33).
Intention to treat (ITT) analysis were carried out in eight publications (21, 26, 27, 29, 31-34).
One publication did not apply the ITT (30) and another one did not provide information
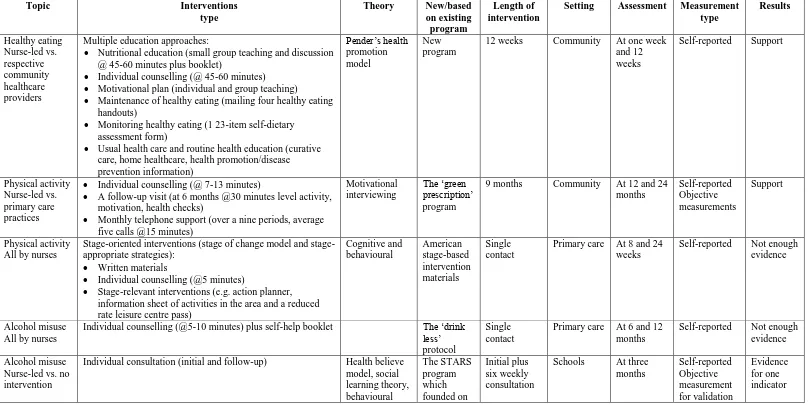
Table 1. The features of the selected publications
Topic Interventions
type
Theory New/based
on existing program
Length of intervention
Setting Assessment Measurement
type Results Healthy eating Nurse-led vs. respective community healthcare providers
Multiple education approaches:
Nutritional education (small group teaching and discussion @ 45-60 minutes plus booklet)
Individual counselling (@ 45-60 minutes)
Motivational plan (individual and group teaching)
Maintenance of healthy eating (mailing four healthy eating handouts)
Monitoring healthy eating (1 23-item self-dietary assessment form)
Usual health care and routine health education (curative care, home healthcare, health promotion/disease prevention information) Pender’s health promotion model New program
12 weeks Community At one week
and 12 weeks
Self-reported Support
Physical activity Nurse-led vs. primary care practices
Individual counselling (@ 7-13 minutes)
A follow-up visit (at 6 months @30 minutes level activity, motivation, health checks)
Monthly telephone support (over a nine periods, average five calls @15 minutes)
Motivational interviewing
The ‘green prescription’ program
9 months Community At 12 and 24
months Self-reported Objective measurements Support Physical activity All by nurses
Stage-oriented interventions (stage of change model and stage-appropriate strategies):
Written materials
Individual counselling (@5 minutes)
Stage-relevant interventions (e.g. action planner, information sheet of activities in the area and a reduced rate leisure centre pass)
Cognitive and behavioural American stage-based intervention materials Single contact
Primary care At 8 and 24 weeks
Self-reported Not enough evidence
Alcohol misuse All by nurses
Individual counselling (@5-10 minutes) plus self-help booklet The ‘drink
less’ protocol
Single contact
Primary care At 6 and 12 months
Self-reported Not enough evidence
Alcohol misuse Nurse-led vs. no intervention
Individual consultation (initial and follow-up) Health believe
model, social learning theory, behavioural The STARS program which founded on Initial plus six weekly consultation
Schools At three
self-control theory the motivational stages prevention model that posits a continuum of stages in alcohol-use habit acquisition and change Multiple focus
All by nurses
Health checks: medical history, lifestyle questionnaire, and structured dietary assessments (initial health checks @45-60 minutes; follow-up visits @10-20 minutes)
Previously developed standard health checks Initial health check Annual follow-up health checks General practices At three years Self-reported Objective measurements Support Multi focus Nurse-led vs. usual care
Individual consultation (@20 minutes) Standard
protocol
Single contact
General practices
At three and 12 months Self-reported Objective measurement for validation Support Coronary Heart Disease risk All by nurses
Individual counselling based on self-monitoring results (initial session @20 minutes)
Motivational interviewing and the stage-based concept Existing standard plus self-monitoring A 3-month protocol, including the initial and follow-up counselling General practices
At one year Self-reported Objective measurements Not enough evidence Coronary Heart Disease risk Nurse-led vs. conventional PC (primary physician)
Individual consultation (monthly for six months: initial consultation @60 minutes and follow-up session @30 minutes) Behavioural self-management, transtheoretical stages of change model New protocol
6 months At 6 months Objective
measurements Not enough evidence Coronary Heart Disease risk
Nurse-Individual counselling (initial face-to-face @60 minutes). Then monthly follow-up face-to-face @60 minutes in high level group and telephone consultation in low level group
Cognitive behavioural
New protocol
12 months General
practices
Participants
The participants in the studies represented diverse groups of the population, from young
people (31, 32) to older people (21, 26, 28, 30, 34). Three studies recruited participants from
a wide range of age groups (27, 29, 33). The interventions were mainly delivered within
primary care settings (80%) (21, 26, 27, 29, 30, 32-34) or in combination with clients’ houses
(28), and one study was at schools (31). In most studies (80%), the treatment and control
groups were comparable at entry (21, 26-30, 32, 34). In two studies (31, 33), a significant
difference was found in one aspect of the participants’ baseline characteristics; but there was
no sufficient information to determine whether or not this factor influenced the studies’
outcomes.
Interventions
The studies’ interventions varied widely, from single-focus interventions applied to target
healthy eating (28), physical activity (26, 34), and alcohol misuse (27, 31); to those applied
across several health behaviours (multiple risk factors) (29, 32); and interventions to address
CHD risk factors (21, 30, 33). The interventions ranged from a relatively simple regime that
was predominantly delivered through individual counselling or consultation with various
intensity (five to 60 minutes per each session) and diverse methods of delivery (mostly
face-to-face or in combination with telephone sessions) (27, 30-33); to more complex ones by
combining individual counselling with other interventions, e.g. small-group teaching and
discussion sessions plus usual healthcare and health education (28), health checks (26),
stage-relevant interventions (action planner and referral to leisure centres) (34), or self-monitoring
programmes (21). Only one study employed health checks as the main intervention (29).
Seven studies employed interventions that were built on the existing programmes (21, 26, 27,
29, 31, 32, 34). In three other studies, new programmes were developed base on the
standardised theories in HP, namely, Pender’s HP theory (28), behavioural self-management
and trans-theoretical stages of change model (30), and cognitive behavioural approach (33).
The interventions ranged from a single-contact intervention (27, 29, 32, 34) to those requiring
multiple contacts with clients (26, 28, 31). For studies with multiple contacts, the period of
time needed to deliver a full course of the intervention ranged from less than two months (31)
or three months (21, 28); to a longer period such as six months (30), nine months (26), and 12
months (33). A common component of all programmes was that the interventions were
treatment to their controls’ subjects, Werch, Carlson, Pappas and DiClemente (31) gave no intervention for those assigned to the control group.
Outcomes
Studies reported diverse outcomes depending on their focus interventions, including those
related to specific or multiple health behaviours and outcomes related to CHD morbidity.
Assessment methods greatly varied from relying on a self-reported survey (self-administered
or administered by the assessors) to a more objective and comprehensive measurement and
verification technique. The chosen follow-up periods were also various across the studies; the
shorter one was 12 weeks post-intervention (28) and the longest one was a three year
follow-up (29). In order to sufficiently delineate the findings and to compare studies addressing
similar outcomes, each publication will be classified into three groups that can be
demonstrated as follows:
Evidence of the effectiveness of interventions to address specific health behaviours
Healthy eating
One publication evaluating intervention for promoting healthy eating amongst the aged (≥
60 years) and their family members was identified (28). A-three month Pender’s based
nutritional-education program using multiple strategies was employed to measure its impact
on the respondents’ eating habits (food selection, preparation, and consumption). The
findings showed significantly higher scores on all indicators in intervention group at week
one and 12 weeks post-intervention. Three other studies included in this review that primarily
focused on comprehensive healthy lifestyles (29, 32) and the effect of nurse-led intervention
on CHD risk factors (33) also evaluated their participants’ dietary patterns.
Physical activity
Two RCTs focused on physical activity outcomes (26, 34). Whilst Lawton, Rose, Elley,
Dowell, Fenton and Moyes (26) specifically recruited physically-inactive women aged 40-74;
Naylor, Simmonds, Riddoch, Velleman and Turton (34) included all clients attending health
checks aged averagely 42.4. Lawton, Rose, Elley, Dowell, Fenton and Moyes (26) employed
a nine-month exercise on prescription intervention built on the existing ‘green-prescription’
program which underpinned by motivational interviewing principles. Using both
self-reported and objective measurements, the researchers measured the intervention’s primary
and Turton (34) only utilised self-reported scales to compare the effectiveness of four
variations of a single-contact staged-based intervention on participants’ stage of exercise
behaviour, exercise level, weekly physical-activity energy, and self-efficacy. Lawton, Rose,
Elley, Dowell, Fenton and Moyes (26) assessed their outcomes at 12 and 24 months
post-intervention and found that the post-intervention significantly increased physical activity and some
variables of quality of life (QoL) over two years, even there were no statistically significant
improvements in the other secondary outcomes. Naylor, Simmonds, Riddoch, Velleman and
Turton (34) did short-term evaluations at week eight and 24 post-intervention and revealed
that the stage-based interventions were not superior to other interventions. All groups
increased in their motivational readiness to exercise, without significant improvements on
physical activity levels or self-efficacy levels (34). Unequal group size at the entry and
alteration on its random assignment should be taken into consideration when interpreting
findings from this study (34). A common element of both studies (26, 34) was that the
intervention was principally delivered through a relatively brief individual counselling.
Physical activity patterns were also measured as the component of broader measurements in
other included publications (21, 29, 32).
Smoking
There was no study included in this review that specifically investigated smoking
behaviour as the primary outcome. However, it has been measured as an integral component
of studies conducted to assess the overall healthy behaviour (29, 32) and CHD risk factor
assessment (21, 30).
Alcohol misuse
Two included publications reported intervention measuring alcohol-related outcomes (27,
31). While Lock et al. (27) set a wide age interval for their included participants (aged ≥ 16
years), younger participants (aged 12.2 years ± 1.16) were recruited by Werch, Carlson,
Pappas and DiClemente (31) at schools. Although each study employed a nurse-led brief
alcohol consultation targeting individual clients based on a previously developed program,
the nature of the interventions and measurements were different. Employing a pragmatic
cluster sampling to deliver a 5-10 minute ‘drink-less’ protocol, Lock et al. (27) used a more
comprehensive assessment and standardised instruments and followed up the outcomes at six
and 12 months after the program. However, this study demonstrated no evidence that
nurse-led screening and a brief alcohol program was superior to standard intervention; but a
Pappas and DiClemente (31) only measured the outcomes up to three months after a-two
phase consultation program that was underpinned by multiple HP theories i.e. health-belief
model, social learning theory, and behavioural self-control theory. They found that there was
no significant difference between intervention and control groups, except on heavy alcohol
use (31). Alcohol behaviour related outcomes were also examined in three other studies
included in this review (29, 32, 33).
Evidence of the effectiveness of interventions applied across multiple health behaviours
There were two studies that evaluated the impact of interventions across several health
behaviours (29, 32). OXCHECK study was conducted to assess the long-term effect of a
nurse-led standardised health-check program amongst clients aged 35-64 years by measuring
self-reported outcomes and objective indicators (29). The OXCHECK study found that over a
period of three years, there were sustained positive changes in dietary pattern and cholesterol
concentrations and blood pressure (29). Walker et al. (32) recruited teenagers aged 14 or 15
employing a 20-minute HP consultation and evaluated the outcomes at three and 12 months
post-intervention. Self-reported assessments were carried out with additional objective
measurements to validate the results. Unfortunately, Walker’s et al. (32) study reported its
baseline data for intervention and control groups in a combined-single table, thus it is
difficult to highlight any differences upon the entry. Furthermore, the 12 months follow-up
results were not given in this publication (32). Except for improvements in motivation or
stage of change for diet and exercise, Walker’s et al. (32) intervention did not result in any
significant differences on other indicators. In addition, attention should have been given to
interpreting the results because there were a considerable number of non-responders
especially at 12 months in this study (32).
Evidence of the effectiveness of interventions to address CHD risk factors
Three studies investigating the effectiveness of intervention to manage CHD risk factors
were included in this review (21, 30, 33). Unlike two other studies that recruited men and
women clients aged over 50 years old with CHD risk factors, Woollard, Burke, Beilin,
Verheijden and Bulsara (33) determined a wider age interval by including hypertension
clients aged between 20 to 75 years old. In Tiessen, Smit, Broer, Gronier and van der Meer’s
study, the experimental group received a-three month additional self-monitoring program into
their existing cardiovascular risk management which underpinned by motivational
Coronary Risk Evaluation (SCORE) formula (21). Tonstad, Alm and Sandvik (30)
administered a monthly nurse-led consultation for six months period based on behavioural
self-management and trans-theoretical stage of change theories. Here, the researchers
identified the intervention effects at baseline and six months post-intervention and then
calculated the estimated 10-year incidence of CHD using the Framingham risk model (30).
Woollard, Burke, Beilin, Verheijden and Bulsara (33) evaluated the effectiveness of three
different interventions and followed-up the effects at 12 and 18 months after intervention by
assessing physical measurements, biochemical indicators, and dietary intake. Overall,
findings from the three studies revealed that there was not enough evidence to conclude that
nurse-led interventions were more effective than CHD standard cares (21, 30, 33). However,
a lesser increase in waist circumference and reduced triglyceride concentrations was
discovered in Tonstad, Alm and Sandvik’s study (30).
DISCUSSION
Due to heterogeneities across the included primary studies’ target participants, objectives,
interventions, measurements and findings; it has not been possible to report any particular
area in greater detail. However, this report offers a general overview of the available evidence
pertaining to the effectiveness of nurse-led HP interventions in the PHC context. Several
interesting findings highlighted from this review will be discussed as follows.
In relation to the studies’ methodology, it was found that nearly all studies (90%)
employed an individual-level randomisation. Only in one study the researchers randomised
their subjects in practice level using a cluster randomisation. This is arguably necessary given
two facts. Firstly, it was impractical to randomize individuals separately within each primary
care and secondly the response to treatment of one individual may affect that of other
individuals in the same cluster (35, 36). However, given the mixed results yielded from the
primary studies and the lack of details on the randomisation method provided by some
publications, it is difficult to draw a firm conclusion as to whether it is the individual or the
cluster randomisation that was more suitable for conducting a HP RCT within the PHC
context. The decision to choose the randomisation technique should be made by considering
at least three factors i.e. the type of intervention being tested in the PHC, the level of
intervention delivery, and the risk of contamination (36).Another methodological issue in the
included studies was the difficulty to maintain the allocation concealment from the allocators.
Only one study sufficiently maintained the treatment allocations until recruitment was
Ineffective masking or blinding the interventions from studies’ participants (clinicians,
clients, and assessors) was also discovered to be a prominent problem in the majority of the
studies. Ideally, a RCT should be double blinded to the study’s participants (e.g. nurses and
clients); yet this is often difficult to achieve effectively, or may even not be feasible to do.
Alternatively, a blinded third party can be employed to assess the outcome (35, 38). Then,
when almost all of the studies analysed their data based on the ITT principle to avoid the
introduction of bias as a consequence of potentially selectively dropping clients from
previously randomised or balanced groups (35, 38); one study employed an on-treat analysis
by considering only those that participated in a full course of the intervention. This could lead
to biased treatment comparisons (35). In addition to the studies’ methodological issues
mentioned above, there was also lack of information on the validity and reliability of the
instruments used to assess the outcomes, as well as inadequate details presented in several
publications. Therefore, it is challenging for the readers to clearly interpret the studies’
findings.
The studies’ participants and contexts represented diverse groups of population and
settings within the PHC practice. This is almost similar to some earlier published reviews
which investigated the effectiveness of HP interventions within the PHC context (13, 39-41).
These findings support the notion that as a first tier of health provision, PHC offers a
universal access for all people, provides affordable and acceptable services (4), and gives
better access for its users as PHC centres are located within community settings (6). This
versatility, indeed, has placed PHC in a pivotal position to manage NCD-related lifestyles
(11).
In terms of the type of HP interventions, this review was unable to locate any studies
which employed nurse-led HP interventions at the group, community or population level.
This finding differs from those reported in the previous publications (13, 39-41). Across all
the included studies in this review, behavioural change approaches targeting individuals’
clients stood as the most frequently cited intervention. Behavioural HP strategies are
predominantly delivered through the provision of counselling or consultation and health
information to improve individuals’ HP skills (4, 7). This either results in changes to existing
unhealthy lifestyles or promotes more positive behaviour. Most studies specified the theory
underlying the interventions’ designs, which mostly stemmed from the educational, social
psychological, expectancy value, socio cognitive and decision-making theories. The key
the interventions were underpinned by the stage models of behaviour change, in particular the
trans-theoretical model. This model suggests that interventions designed to take into account
an individual’s current stage of change ‘readiness’ will be more effective and efficient than
‘one size fits all’ interventions (43).
The studies’ interventions were typically built on multiple theories of HP and required the
clinicians to employ multiple HP strategies. This is reasonable because HP itself is a holistic
concept and its integration into practice require us to take into account the role of the wider
social determinants of health (44). HP is underpinned by a social view of health, which
means that only by addressing the cultural, environmental, biological, political and economic
determinants of health can we improve the population’s health status (4). The social
determinants of health strongly relate to an individuals’ lifestyle choices and behavioural risk
factors, and these will subsequently manifest into their measurable health outcomes (4).
Unfortunately, the contribution of these aspects on HP has received very little attention in the
reviewed primary studies. This finding is identical with those found in Jepson, Harris, Platt
and Tannahill’s review (39).
The other interesting finding of this review was that in 70% of the included publications,
the outcomes were evaluated by not only relying on self-reported measurements, but also by
employing more objective and comprehensive measurement and verification techniques.
Coincidently, this same 70% of the studies also provided sufficient follow-up periods (≥ 6
months) to assess the long-term effect of the interventions; three with unequivocal evidence,
two with mixed effects, and the rest of the studies showing insufficient evidence. This is
dissimilar with Jepson, Harris, Platt and Tannahill’s review which concluded that the
majority of their included publications provided evidence in short-term effects rather than the
longer-term ones (39). Achieving a long-term, sustained effect arguably has become one of
the most significant challenges to bring about a change in people’s health behaviours.
The evidence of nurse-led HP interventions generated from the included studies varied
from outcomes which concluded that nurse-led HP interventions were effective, to those
revealing insufficient evidence to support the conclusion. Interventions that primarily
constituted of an individual counselling or consultation appeared to be the most effective
strategy to change specific health behaviours. Where two studies provided unequivocal
evidence, two showed mixed results and one publication concluded that there was not enough
evidence to support the interventions. Interventions that were most effective in changing
multiple health behaviours included those with individual counselling and health checks
conclude that nurse-led interventions were more effective compared to standard treatments.
Interestingly, although the implementation of stage-based interventions has gained its
popularity in HP research; the findings across the three evidence groups in this review
(specific, multiple, CHD morbidity) suggested that there was little evidence to support the
effectiveness of interventions underpinned by this theory. This result is congruent with a
previously reported systematic review of the effectiveness of stage-based HP interventions
addressing individual’s behavioural changes (41). Finally, since one study typically assessed
multiple outcomes, it is recommended for the reader to carefully interpret the results of the
individual publication. Likewise, ‘no significant differences’ mentioned in several studies
should not be directly inferred that nurse-led interventions were not effective in improving
PHC clients’ health behaviours. The reason for this is because in some studies, the
researchers employed nurse-led interventions in both treatment and control groups by
modifying the interventions’ elements, which resulted in positive changes across all the
groups. Thus, it may suggest that nurse-led interventions did have potential to promote
healthy behaviours amongst the PHC’ clients.
CONCLUSION
The aim of this study was to identify the effectiveness of nurse-led interventions to
promote healthy lifestyles amongst clients in the PHC context. It can be concluded that there
is some encouraging evidence that nurse-led interventions are effective in promoting healthy
lifestyles amongst the PHC clients. The interventions that appear to be most successful
include nurse-led nutritional education programs, exercise on prescription, health checks, and
nurse-led health promotion consultation. The limited number of databases being employed
for the literature search, the exclusion of non-English language and unpublished materials,
and the topic’s broad focus can be seen as the limitations of this review. A more focused
clinical question and systematic literature search is recommended for further relevant
secondary studies in order to capture more comprehensive evidence.
For those interested in investigating this topic through primary research, applying
interventions that acknowledge the interplay between people’s health and the wider social
determinants of health is advisable. Likewise, further research should be focused on
identifying the long-term effectiveness of nurse-led HP interventions by employing
standardised assessment methods. Essentially, further studies should be planned,
pp.167-8) ‘...a well designed, methodologically sound RCT evaluating an intervention
provides strong evidence of a cause-effect relation if one exists; it is therefore powerful in
changing practice to improve patient outcome, this being the ultimate goal of research on
therapeutic effectiveness’.
Findings of this review may also offer implications for the enhancement of nursing
practice and education by highlighting the need to develop approaches to foster nurses and
nursing students’ capacity to undertake their HP roles. The policy makers may also benefit
from the results by gaining a deeper understanding of the nurses’ contributions in HP practice
particularly within PHC context; then putting in place the most appropriate HP strategy to
effectively and efficiently foster the population’s health status. All of these implications are
relevant, given the international commitment to emphasis on the important role of PHC to
safeguard the health of the general population. As nurses are generally considered to be the
frontline workforce of PHC, they may affect a significant percentage of clients with their
effective HP activities, ultimately leading to a more cost-effective healthcare provision.
DECLARATION OF INTEREST
No conflicts of interest noted.
ACKNOWLEDGEMENTS
The reviewer would like to acknowledge Dr. Rick Wiechula from the University of Adelaide
for his valuable supervision and assistance from the beginning of this project.
REFERENCE
1. World Health Organisation. Global status report on noncommunicable diseases 2010. Geneva: World
Health Organisation, 2011.
2. World Health Organisation. Noncommunicable disease: country profiles 2011. Geneva: World Health Organisation, 2011.
3. World Health Organisation. Milestones in health promotion: statements from global conferences. Geneva: World Health Organisation, 2009.
4. Talbot L, Verrinder G. Health promotion in context: primary health care and the new public health movement. In: Talbot L, Verrinder G, editors. Promoting health: a primary health care approach. 4th ed. Chatswood NSW: Elsevier Australia; 2010. p. 1-34.
5. World Health Organisation. 2008-2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. Geneva: World Health Organisation, 2009.
7. Egger G, Spark R, Donovan R. Towards better health. In: Egger G, Spark R, Donovan R, editors. Health promotion strategies and methods. 2nd ed. North Ryde NSW: McGraw-Hill Australia Pty Ltd; 2005. p. 1-25.
8. Kemppainen V, Tossavainen K, Turunen H. Nurses' roles in health promotion practice: an integrative review. Health Promotion International. 2012;27(4):1-12.
9. Kelley K, Abraham C. Health promotion for people aged over 65 years in hospitals: nurses' perceptions about their role. Journal of Clinical Nursing. 2007;16(3):569-79.
10. Kendall S. How has primary health care progressed? Some observations since Alma Ata. Primary Health Care Research & Development. 2008;9(03):169-71.
11. Harris M, Lloyd J. The role of Australian primary health care in the prevention of chronic disease. Australian National Preventive Health Agency Australian Government. 2012.
12. Harris M. The role of primary health care in preventing the onset of chronic disease, with a particular focus on the lifestyle risk factors of obesity, tobacco and alcohol. Canberra: National Preventative Health Taskforce. 2008.
13. Taggart J, Williams A, Dennis S, Newall A, Shortus T, Zwar N, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam Pract. 2012;13(1):49. Epub 2012/06/05.
14. Noordman J, van der Weijden T, van Dulmen S. Communication-related behavior change techniques used in face-to-face lifestyle interventions in primary care: a systematic review of the literature. Patient education and counseling. 2012;89(2):227-44. Epub 2012/08/11.
15. Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. 2011;171(13):1173-80. Epub 2011/07/13.
16. Orrow G, Kinmonth A-L, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ: British Medical Journal. 2012;344:e1389.
17. Kaczorowski J, Chambers LW, Dolovich L, Paterson JM, Karwalajtys T, Gierman T, et al. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP). BMJ. 2011;342:d442. Epub 2011/02/09.
18. Sakane N, Sato J, Tsushita K, Tsujii S, Kotani K, Tsuzaki K, et al. Prevention of type 2 diabetes in a primary healthcare setting: three-year results of lifestyle intervention in Japanese subjects with impaired glucose tolerance. BMC Public Health. 2011;11(1):40. Epub 2011/01/18.
19. Ross HM, Laws R, Reckless J, Lean M. Evaluation of the Counterweight Programme for obesity management in primary care: a starting point for continuous improvement. The British Journal of General Practice. 2008;58(553):548-54.
20. Tappenden P, Campbell F, Rawdin A, Wong R, Kalita N. The clinical effectiveness and cost-effectiveness of home-based, nurse-led health promotion for older people: a systematic review. Health Technology Assessment. 2012;16(20).
21. Tiessen AH, Smit AJ, Broer J, Groenier KH, van der Meer K. Randomized controlled trial on cardiovascular risk management by practice nurses supported by self-monitoring in primary care. BMC Fam Pract. 2012;13:90. Epub 2012/09/06.
23. Lee LL, Kuo YC, Fanaw D, Perng SJ, Juang IF. The effect of an intervention combining self-efficacy theory and pedometers on promoting physical activity among adolescents. J Clin Nurs. 2012;21(7-8):914-22. Epub 2011/11/16.
24. Schadewaldt V, Schultz T. Nurse-led clinics as an effective service for cardiac patients: results from a systematic review. Int J Evid Based Healthc. 2011;9(3):199-214. Epub 2011/09/03.
25. Voogdt-Pruis HR, Beusmans GH, Gorgels AP, Kester AD, Van Ree JW. Effectiveness of nurse-delivered cardiovascular risk management in primary care: a randomised trial. The British Journal of General Practice. 2010;60(570):40-6.
26. Lawton BA, Rose SB, Elley CR, Dowell AC, Fenton A, Moyes SA. Exercise on prescription for women aged 40-74 recruited through primary care: two year randomised controlled trial. BMJ. 2008;337:a2509. Epub 2008/12/17.
27. Lock CA, Kaner E, Heather N, Doughty J, Crawshaw A, McNamee P, et al. Effectiveness of nurse-led brief alcohol intervention: a cluster randomized controlled trial. J Adv Nurs. 2006;54(4):426-39. Epub 2006/05/05.
28. Meethien N, Pothiban L, Ostwald SK, Sucamvang K, Panuthai S. Effectiveness of nutritional education in promoting healthy eating among elders in northeastern Thailand. Pacific Rim International Journal of Nursing Research. 2011;15(3):188-201.
29. OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. Imperial Cancer Research Fund OXCHECK Study Group. BMJ. 1995;310(6987):1099-104. Epub 1995/04/29.
30. Tonstad S, Alm CS, Sandvik E. Effect of nurse counselling on metabolic risk factors in patients with mild hypertension: a randomised controlled trial. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2007;6(2):160-4. Epub 2006/08/18.
31. Werch CE, Carlson JM, Pappas DM, DiClemente CC. Brief nurse consultations for preventing alcohol use among urban school youth. Journal of School Health. 1996;66(9):335-8.
32. Walker Z, Townsend J, Oakley L, Donovan C, Smith H, Hurst Z, et al. Health promotion for adolescents in primary care: randomised controlled trial. BMJ: British Medical Journal (International Edition). 2002;325(7363):524-7.
33. Woollard J, Burke V, Beilin LJ, Verheijden M, Bulsara MK. Effects of a general practice-based intervention on diet, body mass index and blood lipids in patients at cardiovascular risk. Journal of cardiovascular risk. 2003;10(1):31-40. Epub 2003/02/06.
34. Naylor PJ, Simmonds G, Riddoch C, Velleman G, Turton P. Comparison of stage-matched and unmatched interventions to promote exercise behaviour in the primary care setting. Health Educ Res. 1999;14(5):653-66. Epub 1999/10/06.
35. Petrie A, Sabin C. Medical statistics at glance. 3rd ed. Oxford: Wiley-Blackwell; 2009.
36. Elley C, Kerse N, Chondros P. Randomised trials - cluster versus individual randomisation: Primary Care Alliance for Clinical Trials (PACT) network. Australian Family Physician. 2004;33(9):759 -63.
37. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-12.
38. Kendall JM. Designing a research project: randomised controlled trials and their principles. Emergency Medicine Journal. 2003;20(2):164-8.
40. Wilhelmsson S, Lindberg M. Prevention and health promotion and evidence-based fields of nursing - a literature review. Int J Nurs Pract. 2007;13(4):254-65. Epub 2007/07/21.
41. Riemsma R, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt I, et al. A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change in health care settings. Health Technology Assessment. 2002;6(24):1-242.
42. Pender NJ, Murdaugh CL, Parsons MA. Health promotion in nursing practice. 5th ed. Upper Saddle River NJ.: Prentice Hall; 2006.
43. Prochaska JO, DiClemente CC. Trans-theoretical therapy: toward a more integrative model of change. Psychotherapy: Theory, Research and Practice. 1982;19:276-88.