Regular Article
Risk stratification in patients with unstable angina
and/or non-ST-elevation myocardial infarction by
Troponin T and plasminogen-activator-inhibitor-1
(PAI-1)
Andreja Sinkovic*, Vojko Pogacar
Department for Medical Intensive Care, Teaching Hospital Maribor, Ljubljanska 5, 2000, Maribor, Slovenia
Received 22 February 2004; received in revised form 23 June 2004; accepted 23 June 2004 Available online 12 August 2004
Abstract
Background: Increased Troponin T (TnT) and PAI-1 levels are markers of poor outcome in acute coronary syndromes (ACS). In order to stratify the risk for 30-day combined endpoint of mortality and/or reinfarction in unstable angina and/or non-ST-elevation myocardial infarction (UA/NSTEMI), TnT and PAI-1 levels were simulta-neously assessed.Methods: The TnT and PAI-1 levels of 113 patients with UA/NSTEM were estimated within the first 48 h. Initial therapy was medical. Percutaneous coronary interventions were performed in case of recurrent ischemia and/or hemodynamic and/or rhythmic instability. Results: Statistically significant differ-ences in mean admission PAI-1 (4.2F3.4 vs. 2.8F2.4 U/ml, pb0.05), mean peak
PAI-1 levels within the first 48 h (4.98F3.1 vs. 3.4F2.5 U/ml, pb0.05), and no
significant difference in any TnT level were observed between patients with and without 30-day mortality and/or reinfarction. The risk for 30-day mortality and/or reinfarction significantly increased in patients with admission PAI-1 levelsN4.0 U/ml
(OR=4.44, 95%CI=1.47–13.4), peak PAI-1 levelsN4.0 U/ml (OR=5.78, 95%CI=1.838–
18.20) and with simultaneously increased peak PAI-1N3.5 U/ml and TnTN0.1Ag/l
within the first 48 h (OR=4.9, 95%CI=1.569–15.385). Conclusions: Simultaneous assessment of TnT and PAI-1 would provide complementary prognostic information and enable clinicians to stratify risk more effectively among patients with UA/ NSTEMI.
D2004 Elsevier Ltd. All rights reserved.
0049-3848/$ - see front matterD2004 Elsevier Ltd. All rights reserved. doi:10.1016/j.thromres.2004.06.040
* Corresponding author. Tel.: +386 2 3211656; fax: +386 2 3312393.
E-mail address:[email protected] (A. Sinkovic).
KEYWORDS
Unstable angina; Myocardial infarction; Mortality;
Reinfarction; Troponin T; PAI-1
Introduction
Acute coronary syndromes (ACS), either with or without persistent ST-segment elevation on ECG, share the same athero-thrombotic mechanism and involve different processes including thrombosis, fibrinolysis, hemostasis and inflammation [1].
In ACS without persistent ST-segment elevation on ECG, unstable angina (UA) and non-ST-eleva-tion myocardial infarcnon-ST-eleva-tion (NSTEMI) are consid-ered together as a clinical entity [2,3]. In UA/ NSTEMI, Troponin T (TnT) is the most important biochemical marker of ischemic necrosis and of prognosis including mortality, reinfarction and the need for percutaneous coronary interventions (PCI). Prognostic role of increased TnT levels in UA/NSTEMI is more accurate when clinical risk factors, such as increased age, character of chest pain, changes in ECG during pain, hemodynamic compromise and arrhythmias, are considered as well [3—5].
Increased plasminogen-activator-inhibitor-1 (PAI-1) activity is a marker of impaired fibrinolysis. It significantly stratifies the risk of adverse outcome in ST-elevation ACS due to its resistance to fibrino-lytic agents and progression of coronary athero-thrombosis by decreasing endogenous fibrinolytic plasma activity. It promotes pathogenesis of vulner-able plaques and inflammation and participates in the genesis of acute coronary events[6—11].
Utilizing simultaneous assessment of TnT and PAI-1 levels in patients with UA/NSTEMI has not yet been defined. Our aim was to investigate the predictive role of simultaneous assessments of TnT and PAI-1 levels for the 30-day combined endpoint of all-cause mortality and/or reinfarction in patients with UA/NSTEMI.
Patients and methods
Of the 134 patients, consecutively admitted to the Department of Medical Intensive Care over 24 months due to UA/NSTEMI, 113 were studied prospectively after the patients’ informed consent was obtained. The study was approved by the National Ethical Commission.
Patients were included, if they had had chest pain at rest within the last 48 h (Braunwald classes IIIA, IIIB and IIIC), changes in standard ECG without persistent ST-segment elevations (ST-segment depression z0,1 mV and/or T wave inversion z0,1 mV and/or pathological Q wave suspective of previous MI) and/or increased TnT level on admis-sion [2—5]. PAI-1 levels were estimated in addition
to admission TnT. Neither TnT, nor PAI-1 levels were estimated in 21 excluded patients.
On admission, standard ECG was recorded, continuous monitoring of rhythm initiated and a peripheral i.v. catheter inserted. TnT was esti-mated by the immunochemical method (Boeh-ringer-Mannheim, Germany, normal levels up to 0.1 Ag/l) from blood samples drawn on admission 8—12 h later and in case of recurrent chest pain to confirm reinfarctions. [12]. PAI-1 activity was estimated by the chromogenic method (Berichrom PAI by Dade Behring, Marburg, Germany, normal range 0.3—3.5 U/ml) from blood samples on admission and every 12 h within the first 48 h of hospitalization[13]. Creatine kinase MB isoenzyme (CK-MB mass) was estimated by the immunomethod (Boehringer-Mannheim, normal levels up to 5Ag/l) at recurrence of chest pain to confirm reinfarction. Standard ECG was recorded 12 h after admission and afterwards every 24 h of hospitalization and at recurrence of chest pain.
Treatment consisted of daily oral acetylsalycylic acid (ASA; 100—300 mg tablet), i.v. infusion of standard heparin or s.c. injection of the recom-mended dose of low molecular weight heparin for at least 5 days. Heparin therapy was prolonged at the discretion of the attending physician [3—5]. If necessary, the patients were treated with nitro-glycerin, clopidogrel, beta blockers, ACE inhibitors, statins, diuretics, calcium-channel blockers, dobu-tamin, etc.[3—5].
NSTEMI was confirmed by an increase in TnT levelN0.1Ag/l either on admission and/or 8—12 h later.
Arterial hypertension was defined, when with chronic antihypertensive therapy normal arterial blood pressure was achieved, or when during hospitalization systolic blood pressure was N160
mm Hg and/or diastolic N100 mm Hg on several
occasions without chest pain and without prior antihypertensive treatment.
For at least 2 days, the patients were contin-uously monitored for arrhythmias and conduction disturbances. Noninvasive systemic arterial blood pressure was measured hourly and clinical exami-nation was carried out twice daily during the first few days. Later on, the patients were examined at least once daily and noninvasive systemic arterial blood pressure was measured at least once daily.
interven-tion (PCI) or surgical revascularizainterven-tion [3—5]. PCI was associated with inevitable clopidogrel ther-apy-loading dose 300 mg, followed by 75 mg daily [14].
In patients without recurrent chest pain, hemodynamic and/or rhythmic instability within the first 48—72 h, coronary angiography was performed within the next few days or weeks and subsequent PCI or surgical revascularization, if indicated [3—5].
The primary end-point was 30-day combined endpoint of all-cause mortality and/or reinfarction rate. Complications within 30 days were reinfarc-tions, mortality, heart failure, bleedings, conduc-tion disturbances and arrhythmias.
Atrial arrhythmias were atrial tachycardias, atrial fibrillation and/or flutter. Ventricular arrhythmias, tachycardias and fibrillation were classified according to Lown’s classification [15]. Conduction disturbances were bundle branch blocks or atrioventricular blocks I, II, III, sinoatrial block or asystole. Reinfarction or a new MI was defined as recurrent chest pain, accompanied by new changes in ECG, recurrent rise in TnT and/or rise and fall in CK-MB mass, when TnT was already high (2.3). Heart failure was diagnosed when classes II, III and IV were identified, according to the NYHA and Killip—Kimball classi-fication [16].
Statistical analysis
Statistical analysis was performed by IBM PC, SPSS for Windows. The values were expressed as meansFstandard deviations, or percentages where necessary. Differences between the two groups were tested by the chi-squared test and two-sided Student’st-test. Thepvalueb0.05 was statistically
significant. Odds ratios and 95% confidence
inter-vals (CI) were calculated to test the relative importance of variables[17].
Results
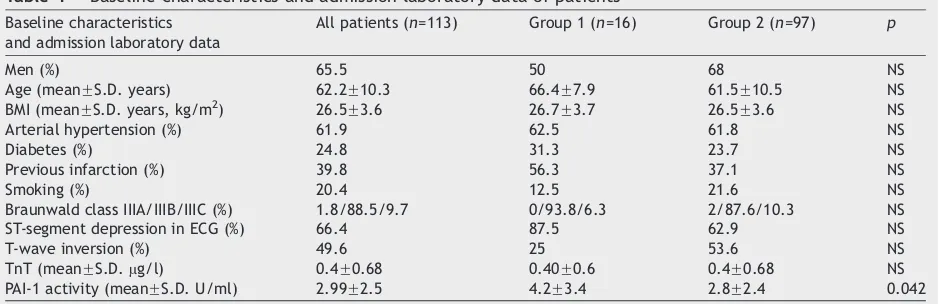
Baseline characteristics and admission laboratory data of patients are listed in Table 1. Complica-tions of patients within 30 days are summarized in Table 2.
Primary endpoint 30-day combined endpoint of all-cause mortality and/or reinfarction rate was 14.2% (16/113). Thirty-day survival without rein-farction was observed in 97 patients. Between the group with mortality and/or reinfarction (Group 1) and the group of 97 survivors without reinfarction (Group 2) within 30 days, we observed nonsignifi-cant and signifinonsignifi-cant differences (Tables 1 and 3). We observed significant differences in mean admis-sion PAI-1 levels (Table 1) and peak PAI-1 levels (4.98F3.1 vs. 3.4F2.5, p=0.022).
We did not observe any significant difference between the Group 1 and Group 2 in neither mean TnT level 8—12 h after admission (1.1F1.4 vs. 0.83F1.3 Ag/l; p=NS) nor mean peak TnT level within 48 h (1.4F1.4 vs. 0.9F1.3 Ag/l;
p=NS).
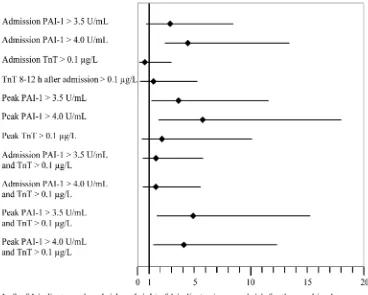
When the patients were stratified into subgroups according to different TnT levels, elevated TnT levels were not associated with significant 30-day combined endpoint of mortality and/or reinfarction (Table 4). When stratifying patients into subgroups, according to different PAI-1 levels and according to simultaneous increase of PAI-1 and TnT, we observed that admission and peak PAI-1 levelsN4.0
4.0 U/ml as well as simultaneous increase of peak PAI-1 and peak TnT were associated with significant 30-day combined all-cause mortality and/or
rein-Table 1 Baseline characteristics and admission laboratory data of patients
Baseline characteristics and admission laboratory data
All patients (n=113) Group 1 (n=16) Group 2 (n=97) p
Men (%) 65.5 50 68 NS
Age (meanFS.D. years) 62.2F10.3 66.4F7.9 61.5F10.5 NS BMI (meanFS.D. years, kg/m2) 26.5F3.6 26.7F3.7 26.5F3.6 NS Arterial hypertension (%) 61.9 62.5 61.8 NS
Diabetes (%) 24.8 31.3 23.7 NS
Previous infarction (%) 39.8 56.3 37.1 NS
Smoking (%) 20.4 12.5 21.6 NS
Braunwald class IIIA/IIIB/IIIC (%) 1.8/88.5/9.7 0/93.8/6.3 2/87.6/10.3 NS ST-segment depression in ECG (%) 66.4 87.5 62.9 NS
T-wave inversion (%) 49.6 25 53.6 NS
TnT (meanFS.D.Ag/l) 0.4F0.68 0.40F0.6 0.4F0.68 NS PAI-1 activity (meanFS.D. U/ml) 2.99F2.5 4.2F3.4 2.8F2.4 0.042
farction rate of our patients (Table 5). Further analysis demonstrated that the risk of combined 30-day mortality and/or reinfarction rate of patients with UA/NSTEMI significantly increased with PAI-1N4.0 U/ml and with the simultaneous increase of
PAI-1N3.5 U/ml and TnTN0.1Ag/l within the first
48 h of hospitalization (Fig. 1).
Discussion
According to the results of several registries, including ENACT, Euroheart Survey, GRACE and NRMI, the incidence and prevalence of UA/NSTEMI
have increased over the last few years, while the number of patients with STEMI is declining. There-fore, accurate early diagnosis, treatment and risk stratification in patients with UA/NSTEMI are gain-ing importance[18—21].
Chest pain, changes in standard ECG and increased TnT level are most important for early recognition and prognosis in UA/NSTEMI patients [3—5,22]. Classification of UA by Braunwald incor-porated clinical circumstances as well as severity of chest pain. Prognosis is worse with chest pain within 14 days of an acute MI or in primary UA
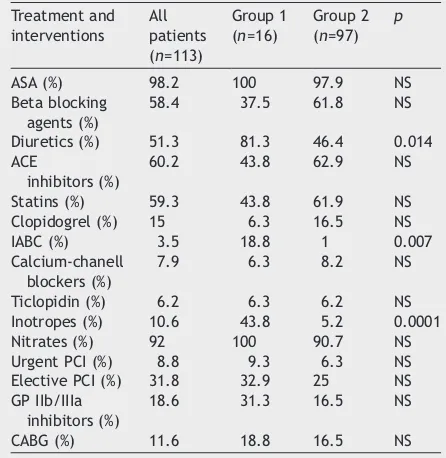
Table 3 Treatment and interventions within 30 days
Treatment and
Diuretics (%) 51.3 81.3 46.4 0.014 ACE
inhibitors (%)
60.2 43.8 62.9 NS
Statins (%) 59.3 43.8 61.9 NS Clopidogrel (%) 15 6.3 16.5 NS IABC (%) 3.5 18.8 1 0.007 Calcium-chanell
blockers (%)
7.9 6.3 8.2 NS
Ticlopidin (%) 6.2 6.3 6.2 NS Inotropes (%) 10.6 43.8 5.2 0.0001 Nitrates (%) 92 100 90.7 NS Urgent PCI (%) 8.8 9.3 6.3 NS Elective PCI (%) 31.8 32.9 25 NS GP IIb/IIIa
inhibitors (%)
18.6 31.3 16.5 NS
CABG (%) 11.6 18.8 16.5 NS Group 1: Patients with mortality and/or reinfarctions. Group 2: Survivors without reinfarctions. PCI: Percutaneous coronary interventions.GP IIb/IIIa inhibitors: Glycoprotein IIb/IIIa inhibitors. CABG: Coronary artery bypass graftin-g.IABC: Intra-aortic balloon counterpulsation.
Table 4 Stratification of patients according to Tropo-nin T levels
Troponin T 8—12 h after admission
N0.1 76.1 81.3 75.3 NS
Group 1: Patients with mortality and/or reinfarctions. Group 2: Survivors without reinfarctions.
Table 2 Complications within 30 days
Complications All patients (n=113) Heart failure Killip II (%) 47.8
Pulmonary edema (%) 15 Cardiogenic shock (%) 13.3 Ventricular arrhythmias (%) 28.3 Ventricular fibrillation (%) 4.4 Atrial arrythmias (%) 17.7 Conduction disturbances (%) 18.6 In-hospital mortality (%) 9.7 30-day Mortality (%) 10.6 30-day Reinfarctions (%) 9.7 30-day Mortality and/or
reinfarctions (%)
14.2
Table 5 Risk stratification, according to increased PAI-1 activity and simultaneous increase of PAI-1 and TnT level
Admission PAI-1N3.5
U/ml
8 (50%) 25 (25.5%) NS
Admission PAI-1N4.0
U/ml
8 (50%) 18 (18.4%) 0.014
Peak PAI-1N3.5 U/ml 11 (68%) 37 (37.7%) 0.04
Peak PAI-1N4.0 U/ml 11 (68%) 27 (27.5%) 0.0043
Admission PAI-1N3.5
U/ml+TnTN0.1Ag/l
4 (25%) 16 (16.5%) NS
Admission PAI-1N4
U/ml+TnTN0.1Ag/l
without extracardiac causes. 88.5% of our patients had primary UA (Braunwald class IIIB) and 9.7% were within 14 days of an acute MI (Braunwald class IIIC) [4,22]. Considering changes in standard ECG, ST-segment depression, carrying worse prog-nosis, was present in 66.4% of our patients [4]. Increased TnT level, the most sensitive and specific biochemical marker of ischemic necrosis and prognosis, was present in 77.9% of our patients, indicating the presence of NSTEMI in majority of patients. When considering chest pain, ECG changes and TnT levels, our patients were of high-risk profile for subsequent events such as mortality and reinfarctions. Indeed, 30-day com-bined all-cause mortality and/or reinfarction rate was as high as 14.2%.
Heart failure, arrhythmias and recurrent chest pain are well-known risk factors for subsequent mortality or new MI in patients with UA/NSTEMI. When they occurred within first 48 h in spite of medical therapy, urgent PCI or surgical revascula-rization were performed [3—5]. However, neither urgent PCI nor CABG within 30 days were associated with 30-day combined endpoint of mortality and/or reinfarction rate (Table 4).
Some clinical studies observed that in UA/ NSTEMI, risk stratification by multiple biomarkers was more precise and earlier than by a single marker, detecting multiple pathological processes of coronary athero-thrombosis including inflamma-tion, myocardial damage or dysfunction[23].
Increased PAI-1 activity is a marker of impaired fibrinolysis, associated with severity, progression and complications of atherosclerosis such as rup-ture, erosion or inflammation with subsequent thrombosis [6—9]. Many clinical and experimental studies suggest that thrombosis and inflammation are closely linked, as markers of thrombosis are often associated with inflammation and vice versa [10,24]. PAI-1 is an acute phase reactant in inflammation, where it stabilizes the chemoattrac-tant form of Interleukin-8 [25]. The proinflamma-tory status associated with overexpression of TNF, IL-6 and PAI-1, found in insulin resistant people, provides a potential link between insulin resistance and endothelial dysfunction, the early stage of atherosclerosis in obese and type 2 diabetes [26,27]. Our observations suggest that when PAI-1 assessment within the first 48 h was added to risk stratification provided by clinical picture, ECG
changes and TnT estimation, prediction of 30-day combined endpoint of mortality and/or reinfarction was more accurate and earlier. The conclusion is that simultaneously assessed TnT and PAI-1 could provide complementary prognostic information and allow clinicians to stratify risk more effectively among patients with UA/NSTEMI.
There are several limitations of this small pilot study. The population studied is relatively small in size to allow any definite conclusions at present to introduce our observations into everyday clinical practice. Our observations should be validated in a larger and better defined population, especially regarding prior drug treatment, prior PCI or surgical revascularization, etc.
Acknowledgments
The work was supported by the grant from Sloven-ian Ministry of Education, Science and Sports (L3-2159, 3411-00-232159). The authors wish to thank Prof. Joze Nemec from the University of Maribor for help with the statistical analysis and Marijana Gajsek-Marchetti for help with the manuscript.
References
[1] Schaeffer AI, Ali NM, Levine GN. Hemostasis, thrombosis, fibrinolysis, and cardiovascular disease. In: Braunwald E, Zipes DP, Libby P, editors. Heart disease. A textbook of cardiovascular medicine, 6th ed. Philadelphia, PA7
Saun-ders; 2001. p. 2099 — 132.
[2] Alpert JS, Thygesen K. The joint European Society of Cardiology/American College of Cardiology Committee. Myocardial infarction redefined—a consensus document of the joint European Society of Cardiology/American College of Cardiology Committee for Redefinition of Myocardial Infarction.Eur Heart J2000;21:1502 — 13.
[3] Bertrand M, Simoons ML, Fox KAA, Wallentin L, Hamm CW, McFadden E, et al. Management of acute coronary syn-dromes in patients presenting without persistent ST-seg-ment elevation.Eur Heart J2002;23:1809 — 40.
[4] Braunwald E. Application of current guidelines to the management of unstable angina and non-ST-elevation myocardial infarction. Circulation 2003;102(Suppl 1): 28 — 37.
[5] Cannon C, Braunwald E. Unstable angina. In: Braunwald E, Zipes DP, Libby P, editors. Heart disease. A textbook of cardiovascular medicine; 6th ed. Philadelphia, PA7
Saun-ders, 2001. p. 1232 — 71.
[6] Sinkovic A. Pre-treatment plasminogen activator inhibitor-1 (PAI-1) levels and the outcome of thrombolysis with streptokinase in patients with acute myocardial infarction.
Am Heart J 1998;136:406 — 11.
[7] Collet JP, Montalescot G, Vicaut E, Ankri A, Walylo F, Lesty C, et al. Acute release of plasminogen activator inhibitor-1 in ST-segment elevation myocardial infarction predicts mortality.Circulation2003;108:391 — 4.
[8] Sobel BE. Increased plasminogen activator inhibitor-1 and vasculopaty. A reconcilable paradox.Circulation1999;99: 2496 — 8.
[9] Okada S, Woddcock-Mitchell J, Mitchell J, Sakamoto T, Marutsuke K, Sobel B, et al. Induction of plasminogen activator inhibitor type 1 and type 1 collagen expression in rat cardiac microvascular endothelial cells by interleukin-1 and its dependence on oxygen-centered free radicals.
Circulation1998;97:2175 — 82.
[10] Ross R. Atherosclerosis—an inflammatory disease.N Engl J Med1999;340:115 — 6.
[11] Sobel BE, Woodcock-Mitchell J, Schneider DJ, Holt RE, Marutsuka K, Gold H. Increased plasminogen activator inhibitor type 1 in coronary artery atherectomy specimens from type 2 diabetic compared with nondiabetic patients: a potential factor predisposing to thrombosis and its persis-tence.Circulation1998;97:2213 — 21.
[12] Zimmerman J, Fromm R, Meyer D, Boudreaux A, Wun CC, Smalling R, et al. Diagnostic marker cooperative study for the diagnosis of myocardial infarction.Circulation 1999;
99:1671 — 7.
[13] Hamsten A, Wiman B, de Faire U, Blomback M. Increased plasma levels of a rapid inhibitor of tissue plasminogen activator in young survivors of myocardial infarction.N Engl J Med1985;313:1557 — 63.
[14] CURE investigators M. Effects of pre-treatment with clopidogrel and aspirin followed by long term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study.Lancet2002;358:527 — 33.
[15] Lown B, Graboys TB. Sudden death. An ancient problem newly perceived.Cardiovasc Med1977;2:219 — 29. [16] Killip T, Kimball JT. Treatment of myocardial infarction in a
coronary care unit. A two years experience with 250 patients.Am J Cardiol1967;20:457 — 64.
[17] Jekel JF, Elmore JG, Katz DL, editors. Epidemiology, biostatistics and preventive medicine; 1st ed. Philadelphia, PA7Saunders, 1996.
[18] Fox KAA, Cokkinos DV, Deckers J, Keil U, Maggioni A, Steg G on behalf of the ENACT. The ENACT study: a pan-European survey of acute coronary syndromes. Eur Heart J 2000;
21:1440 — 9.
[19] Hasdai D, Behar S, Wallentin L, Danchin N, Gitt AK, Boersma E, et al. Prospective survey of the characteristics, treat-ments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin. The Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS).Eur Heart J2002;23:1190 — 201.
[20] Fox KAA, Goodman SG, Klein W, Brieger D, Steg PO, Dabbous O, et al., for the GRACE investigators. Management of acute coronary syndromes. Variations in practice and outcome. Findings from the Global Registry of Acute Coronary Events (GRACE).Eur Heart J2002;23:1177 — 89.
[21] Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid DA, Shoultz DA, et al. EveryNfor the investigators in the National Registry of Myocardial Infarction 1, 2 and 3. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the U.S. from 1990 through 1999. The National Registry of Myocardial Infarc-tion 1, 2 and 3.J Am Coll Cardiol2000;36:2056 — 63. [22] Braunwald E. Unstable angina—a classification.Circulation
1989;80:410 — 4.
[23] Sabatine MS, Morrow DA, de Lemos JA, Gibson CM, Murphy SA, Rifai N, et al. Multimarker approach to risk stratification in non-ST-elevation acute coronary syn-dromes. Simultaneous assessment of Troponin. C-reactive protein, and B-type natriuretic peptide.Circulation2002;
[24] De Maat MPM, Bladbjerg EM, Drivsholm T, Borch-Johnsen K, Moller L, Jaspersen J. Inflammation, thrombosis and atherosclerosis: results of the Glostrup study. J Thromb Haemost2003;1:950 — 7.
[25] Marshall LJ, Ramdin LSP, Charlton P, Shute JK. Plasminogen activator inhibitor-1 supports IL-8-mediated neutrophil transendothelial migration by inhibition of the constitutive shedding of endothelial IL-8/heparan sulfat/syndecan-1 complexes.J Immunol2003;171:2057 — 65.
[26] Bastelica D, Mavri A, Verdier M, Barthet B, Juhan-Vague I, Alessi MC. Relationships between fibrinolytic and inflam-matory parameters in human adipose tissue: strong con-tribution of TNFa receptors to PAI-1 levels. J Thromb
Haemost2003;88:481 — 7.