LEARNING TASK
Tjokorda Gde Agung Senapathi
SELF ASSESMENT:
1. Explain briefly with narration about the scope of “Emergency Medicine” 2. Explain with narration about the “basic principals of Emergency Medicine” 3. Elaborate briefly about the details in “Triad Emergency Medicine”
4. Explain with narration about Emergency Medical Services 5. Explain briefly about the disaster medical services
6. Explain it briefly about the incident command system of the organization of disaster.
All of the person in SGD must write it personally!.
Day 1
Day 2
SEIZURE
IGN BudiarsaLEARNING TASK
1. As a general practitioner who works in public health centre, you were visited by a 40 years old man, who brought his brother 35 years old with seizure all over his body and bubbles in his mouth.
(a) As a doctor what would you do?
(b) After the first aid the seizure has stopped but the patient is still unconscious. What do you do next?
After a while the patient has seizure again, even before gaining consciousness. (c) What caused the patient to seizure again?
(d) If u were working in the emergency room at the hospital, what would your action be?
2. When would you suggest a surgical intervention to an epileptic patient?
SELF ASSESSMENT
Day 3
COMA AND DECREASE OF CONCIOUSNESS
IA Sri Wijayanti
SCENARIO
A 47-year-old man arrives at the emergency room in a coma. His wife reports that he developed shaking movements and abnormal breathing sounds in the middle of the night. His shaking and the sounds woke her, but she was unable to wake him. He has been somewhat forgetful over the prior 3 months, but has seemed well otherwise. Examination in the emergencyroom reveals an unresponsive man who exhibits generalized convulsions every 10 min. He is afebrile and incontinent of urine.
SELF ASSESSMENT
1. What other history taking, other symptoms that we should explore to diagnosis this case?
2. What other examination that we should do to diagnosis this case? 3. What could be the possible diagnosis?
Day 4
ACUTE PSYCHIARTIC EPISODE Cokorda Bagus Jayalesmana
LEARNING TASK
1. A 20-year-old male with a known history of schizophrenia is admitted to the ward compulsorily following deterioration of his mental state. One day while out on unescorted community leave, he returns to the ward agitated and distressed, and discloses that he had consumed cannabis. He becomes irritable and starts shouting abuse at the nurses when they request a urine sample for a drug screen. The nurse attempts to ‘talk him down’ but this fails.
a) What are the risks to the patient as above?
b) What are the available option to the patient so he can make informed choices? c) What is the diagnosis of the patient above?
d) What is the treatment plan for the patient above? e) What is the follow up plan for the patient above? f) How do you assess the patient above for referral?
2. A 52-year-old female is admitted to a medical ward with an acute exacerbation of Crohn’s disease, requiring high-dose steroids and intensive emergency treatment. After a few days, however, she accuses the nurses on the ward of stealing her money and believes that one of the male nurses assaulted her during the night. However, once her steroids are stopped, she starts to settle and no longer voices any bizarre ideations.
a) What is the diagnosis of the patient above? b) What is the treatment plan for the patient above? c) What is the prognosis of the patient above?
SELF ASSESSMENT
1. Be able to identify emergency psychiatry
2. Being able to do a short interview to explore data and plan the necessary investigations for Acute Psychiatric cases.
3. Able to make advance planning for dealing with Acute Psychiatric cases.
4. Understand etio-pathogenesis, patho-physiological and psychodynamic occurrence of Acute Psychiatric cases.
Day 5
ACUTE RESPIRATORY DISTRESS SYNDROME AND FAILURE Putu Andrika
ACUTE RESPIRATORY DISTRESS SYNDROME AND FAILURE
CASE 1 :
A patient was brought to emergency unit by their family with complaint for sudden breathing difficulties and decrease in consciousness. Five days before the patient suffered from high temperature until shivering together with purulent cough and breathing difficulties. During physical examination it was found T. 100/70, N. 120/m, RR. 30 times/m temp.39 oC.
in the lung it was found ronki diffuse, wheezing. On the thorax photo it was found homogen covering on the two lung areas and consolidation in the center – right side part. During examination of blood gas analyses it was found PaO2, 45 mmHg while PaCO2 65 mmHg.
SELF ASSESSMENT
1. Discuss about that case assessment 2. Other recommended examination 3. What is the procedure
4. How is the pathophysiology of ARDS 5. Explain etiopathogenesis of ARF
6. Distinguish between ARF Hypoxemia and Hyperkapnea 7. Objective of ventilator installation
RESOURCES
Polly E. Parson, MD. Acute Respiratory Distress Syndrome in Michael E. Hanley, Carolyn H. Welsh, Lange Current Diagnosis & Treatment in Pulmonary Medicine 2003, 161 – 166.
ARDS IN PEDIATRIC Dyah Kanyawati
A 5 years old boy came to the hospital with chief complain short of breath since 5 days before admitted to the hospital. Short of breath became more severe every day and now the patient came with sianotic in the lips. The patient also had high fever, cough and cold since 5 days before admitted to the hospital.
Blood pressure : 80/65 mmHg
Pulse : 120 x/minute
RR : 40 x/minute
Temp : 38ºC
Thorax : subcostal retraction, rales +/+
Learning Task
1. What is the possible diagnosis?
2. What modality (laboratory, imaging) should be done in this patient? 3. Blood gas analysis : PCO2 45, PO2 60, PF ratio <300
A mother of 3 years old child complained about difficult breathing with her child after eating peanuts. There is no fiver. ENT condition with normal limited.
Task:
1. What are other helpful informations you should get from his mother for complete management of this case?
2. Considering the onset of manifestation: please describe other clues you should find during physical examination on this child!
3. Do you need laboratory investigation? 4. What are your suggestions for the mother? 5. What are your planning for manage this case? Self assessment:
1. What causes acute upper airway obstruction?
2. Describe the etiopathogenesis of foreign body airway obstruction. 3. Describe the risk factor of foreign body airway obstruction. 4. Describe symptom and sign of foreign body airway obstruction. 5. Describe the imaging studies of acute upper airway obstruction.
RADIOLOGY Srie Laksminingsih
LEARNING TASK
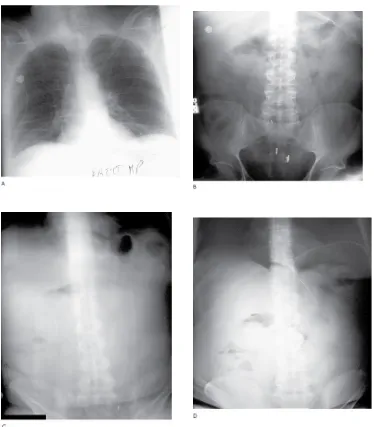
1. A 78-year-old previously healthy man presented with two days of cough productive of thick purulent sputum, fever and dyspnea on exertion. On examination, he was an elderly man who appeared acutely ill. Vital signs—blood pressure 96/60 mm Hg, pulse 116 beats/ min, respiratory rate 24 breaths/min, temperature 103.5°F rectal. Lung examination revealed scattered ronchi, which were greater on the right than the left. Blood tests and a chest radiograph were obtained and intravenous antibiotics were administered. What do the chest radiographs show (Figure 1)?
2. A 34-year-old woman presented to the ED with dyspnea that began three hours earlier. The ambulance call report clearly captures the essence of the patient’s clinical presentation Her chief complaint was: “I can’t breathe.” She had dull substernal chest pain. The ambulance crew noted that she was “hysterical and hyperventilating” and that she was taking birth control pills. During the previous month, she had had episodes of shortness of breath and dull chest pain. She appeared ill, and the presumptive diagnosis was “rule-out myocardial infarction.”
On examination, her lungs were clear to auscultation and her heart was rapid and regular without murmur, pericardial friction rub, or gallop. Her abdomen was not tender and there was no lower extremity edema or tenderness. She was overweight.
Blood tests, EKG, and chest radiographs were obtained. The EKG revealed sinus tachycardia and nonspecific T-wave flattening.
The chest radiographs were interpreted as being “normal” (Figure 3). A bolus and infusion of heparin was administered by intravenous catheter. Should you order a chest radiograph in this patient?
What are you looking for?
(There are three significant radiographic findings.)
3. A 51-year-old man presented to the ED with progressive abdominal pain of one day's duration. He had not eaten all day and had vomited twice. There was no associated diarrhea or melena. He had a history of alcoholic hepatitis, COPD, and surgical repair of a colonic-bladder fistula 10 years earlier. He had mild constipation and abdominal discomfort for the past few months.
On examination, the patient was in moderate distress due to abdominal pain. Vital signs: blood pressure 130/70 mm Hg; pulse 118 beats/min; respirations 24 breaths/min; temperature 100.8º F (rectal). His abdomen was distended but soft, with mild diffuse tenderness and no rebound tenderness. His stool
was negative for occult blood. He was anicteric.
nasogastric tube was inserted. Because of concern that he might have a perforated peptic ulcer, 300 mL of air was insufflated via a nasogastric tube and the upright abdominal radiograph was repeated (Figure 4D). The air noted under the left hemidiaphragm was interpreted as being in the patient’s distended stomach.
Two hours later, an abdominal CT was performed that revealed the correct diagnosis.
The diagnosis was evident on the initial radiographs (Figure 4). What do they show?
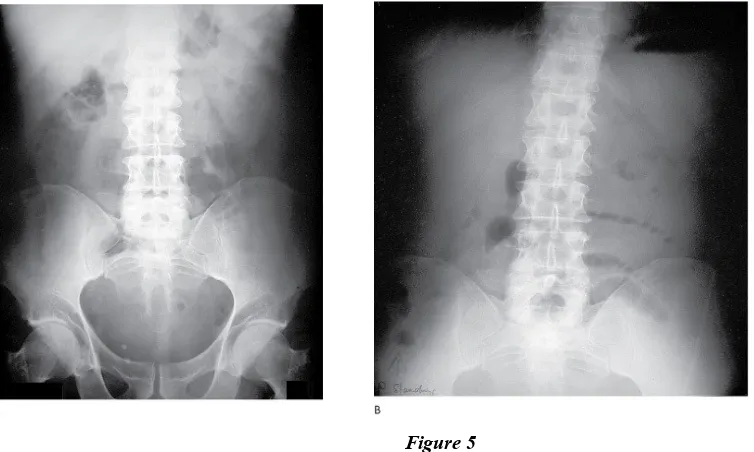
4. A 50-year-old man complained of periumbilical and left lower quadrant abdominal pain that began earlier in the day. The pain was intermittent, “crampy” in character, and accompanied by anorexia and vomiting. He had a normal bowel movement the previous day. He had not experienced similar pain in the past. There was no history of prior abdominal surgery. On examination, the patient was afebrile and in moderate distress due to his abdominal pain. Bowel sounds were present, and the abdomen was mildly distended with periumbilical tenderness, but no rebound tenderness. Abdominal radiographs
(Figure 5) and chest radiographs were obtained.
Figure 5
The abdominal radiographs were interpreted as showing a “nonspecific bowel gas pattern.”
Do you agree with this interpretation? Explain
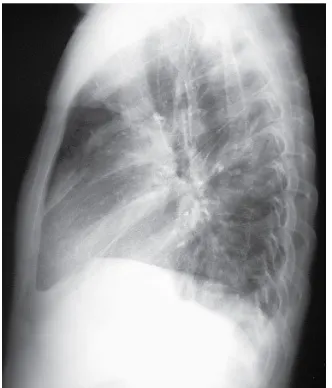
5. A 36-year-old man presented to the ED complaining of a cough. He had been drinking heavily that night and did not have a place to stay.
On arrival in the ED, he was ill-kempt and lethargic, but arousable. His vital signs were normal: blood pressure 120/80 mm Hg, pulse 88 beats/min, respiratory rate 18 breaths/min, and temperature 98.8°F. Hisoxygen saturation was 97% on room air and finger stick blood glucose was 110 mg/dL. There was a laceration on his forehead that had been sutured two weeks ago, but no evident acute trauma. Because he had a cough that was productive of blood-tinged sputum, he was triaged to a respiratory isolation room. He stated that he had never had tuberculosis (TB), but a PPD tuberculin skin test had been positive in the past.
similar symptoms several months earlier and had been prescribed medications that he was no longer taking. On examination, heart sounds were normal, and lungs were clear to auscultation.
For the past two months, he had been staying in a nearby homeless shelter or occasionally with a friend or on the street. He had had an HIV test in the past but did not know the result.
Chest radiographs were obtained (Figure 6).
Figure 6
What do they show?
BLEEDING DISORDERS Epistaxis
Dr.Sari Wulan,SpTHT-KL(K)
Learning task
1. Female, 22 yo, pregnant 20 week gestation, comes to fast track because of bleeding of the nose.
a. What kind of information that we need more? b. Describe the pathophisiology, why is this happened?
c. What kind of complication that can be occurred in this patient? How to avoid it?
2. A boy, 6 yo, company by the parents complaining about habitual bleeding of the nose a. What question we sould asked in order to recover the caused?
b. Explained the pathophisiology in this boy! c. How to avoid bleeding int the future?
Vaginal Bleeding
Dr.dr Wayan Megadhana, SpOG(K)
Learning Task
1. A 25 years old G3 woman presents to the maternity unit with vaginal bleeding. Fetal heart rate is 140 per minute and her blood pressure is 110/60 and her HR is 85/minute. Fundal height is 28 cm. she has been given nothing. What are the possible diagnosis?
Day 7
Shock
dr. IGAG. Utara Hartawan, SpAn MARS
Learning Task
1. A 24 year woman arrives in ER with dyspneau and skin rash on her chest and abdominal, the woman unconsious and her lip was thiked and numbness, history of allergic was denied. On Physical examination are BP 100/90 Pulse 100x/menit RR 37x/mnt temp 37, wheezing +/ + on right and left pulmo, rhonki -/- angioodema was found.
a. Diagnose the patient b. The different diagnose are
c. can describe the algorithm of management d. Describe the Hypersensitivity Reaction
2. A 67 year man unconcious felt down from 5 meters of tree, there are stab wound in posteror of head. The backbone are fuly pain and can’t move legs. On Physical examination are BP 80/50 pulse 88RR 20 temp 37. Paraparese found in lower extremitas
a. what is the diagnose
b. what the supporting examination do you need? c. describe the management this patient
3. Male 56 years admitted to the ICU for 1 week initially treated patients with symptoms of urinary tract infections . Patients sudden loss of consciousness followed by shortness followed decreased urine output .
On Physical examination are BP 90/50 pulse 120 RR 30 temp 40 a. Diagnose for ths patient
b. Decribe the management
4. 22 year old male presents following a motorcycle crash. He complains of the inability to move or feel his legs. His blood pressure is 80/50 mm Hg, heart rate is 100, respiratory rate is 20. GCS is 15. Temp 37 Oxygen is 99%on 2L nasal prongs. Chest X-ray, pelvic X-ray, FAST are normal. Extremities are normal.
a. What the diagnose
b. Describe the emergency problem of the patient c. How the management
5. 22-year-old man sustains a shotgun wound to the left shoulder. His blood pressure is initially 80/40. After two liters of Ringer's lactate solution his blood pressure
increases to 122/84. His pulse rate is now 100 beats per minute and his respiratory rate is 28 breaths per minute. His breath sounds are decreased in the left hemithorax,
Shock in Pediatric
dr.Nyoman Budihartawan,MSc,SpA
Learning Task Case 1
A 5 years old boy with body weight 20 kg, came with chief complain cold in palms and soles since 24 hours before admitted to the hospital. History of fever occurred 5 days before admitted to the hospital, but 1 day before admitted, the fever being decreased. The patient had been urinated 10 hours before admitted to the hospital.
Physical examination
Patient with decreased of consiousness, pulse 140 x/minute regular smooth pulsation, capillary refill time > 2 seconds.
Complete blood count
WBC: 2.000/uL, Hb: 15 g/dL, HCT: 45%, Plt: 20.000/uL
Self Assesment
1. Discuss about the assessment 2. Discuss about the therapy 3. Discuss about the monitoring
Learning Source
Day 8
Cardiac Arrest and +
Cardiopulmonary Resuscitaton
dr. IGN. Mahaalit Aribawa, SpAn KAR
Learning Task
1. A 24 year woman arrives in ER with dyspneau and skin rash on her chest and abdominal, the woman unconsious and her lip was thiked and numbness, history of allergic was denied. On Physical examination are BP 100/90 Pulse 100x/menit RR 37x/mnt temp 37, wheezing +/ + on right and left pulmo, rhonki -/- angioodema was found.
1. Diagnose the patient 2. The different diagnose are
3. can describe the algorithm of management 4. Describe the Hypersensitivity Reaction
2. A 67 year man unconcious felt down from 5 meters of tree, there are stab wound in posteror of head. The backbone are fuly pain and can’t move legs. On Physical examination are BP 80/50 pulse 88RR 20 temp 37. Paraparese found in lower extremitas
1. what is the diagnose
2. what the supporting examination do you need? 3. describe the management this patient
3. Male 56 years admitted to the ICU for 1 week initially treated patients with symptoms of urinary tract infections . Patients sudden loss of consciousness followed by shortness followed decreased urine output .
On Physical examination are BP 90/50 pulse 120 RR 30 temp 40 a. Diagnose for ths patient
b. Decribe the management
4. 22 year old male presents following a motorcycle crash. He complains of the inability to move or feel his legs. His blood pressure is 80/50 mm Hg, heart rate is 100, respiratory rate is 20. GCS is 15. Temp 37 Oxygen is 99%on 2L nasal prongs. Chest X-ray, pelvic X-ray, FAST are normal. Extremities are normal.
a. What the diagnose
b. Describe the emergency problem of the patient c. How the management
5. 22-year-old man sustains a shotgun wound to the left shoulder. His blood pressure is initially 80/40. After two liters of Ringer's lactate solution his blood pressure increases
to 122/84. His pulse rate is now 100 beats per minute and his respiratory rate is 28 breaths per minute. His breath sounds are decreased in the left hemithorax,
Day 9
Emergency Toxicology and Poisoning
dr. I Ketut Agus Somia, SpPD KPTI
LEARNING TASK Case 1
Female 25 years, came to the ER carried by his family in a state of unconsciousness. After approximately 22 hours ago attend the party. Previous patients with mild drunk and sleepy, then complained of blurred vision and blind
Learning task 1
1. Describe the symptoms and clinical signs in these cases?
2. What are the other anamnesis and the other physical examination that needed 3. What the laboratory examination is needed to confirm the diagnosis
4. What the differential diagnosis above case 5. What the diagnosis above case
6. How to manage the above case
Case 2
Male 20 years, student, came to the ER Sanglah, was brought by his parents in a state of unconsciousness. On physical examination found coma, blood pressure 80/60 mm Hg, pulse 48 beats per minute, frequency of breathing 12 times per minute. The pupils: miosis. Abdominal examination: decreased bowel sounds. At the forearm found needle track marks. Learning task 2
7. Describe the symptoms and clinical signs in these cases?
8. What are the other anamnesis and the other physical examination that needed 9. What the laboratory examination is needed to confirm the diagnosis
10. What the differential diagnosis above case 11. What the diagnosis above case
12. How to manage the above case
Case 3
Male, 20 years old, a builder, came to the ER escorted by his friend, the pain after accidentally ingesting drinking colored floor cleaning liquid is clear and odorless. On physical examination lip until pharing area look red and swollen.
Learning task 3
13. Describe the symptoms and clinical signs in these cases?
15. What the laboratory examination is needed to confirm the diagnosis 16. What the differential diagnosis above case
17. What the diagnosis above case 18. How to manage the above case
Case 4
Male 30 years old come to the ER, in between by his girlfriend, complained of fatigue and vomiting - vomiting after drinking Baygon (insecticide), approximately 6 hours ago. Patients also complain of frequent urination and defecation. On physical examination found the pulse of 48 beats per minute, miosis, lacrimation, salivation.
Learning task 4
19. Describe the symptoms and clinical signs in these cases?
20. What are the other anamnesis and the other physical examination that needed 21. What the laboratory examination is needed to confirm the diagnosis
22. What the differential diagnosis above case 23. What the diagnosis above case
24. How to manage the above case
REFERENCES
Eddleston M. Buckley NA, Eyer P, AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008 Feb 16; 371(9612): 597–607.
Lupa M, Magne J, Guarisco JL, Amedee R. Update on the Diagnosis and Treatment of Caustic Ingestion. The Ochsner Journal. Volume 9, Number 2, Summer 2009.
Boyer EW. Management of Opioid Analgesic Overdose. N Engl J Med 2012; 367:146-155
Day 10
Hypertension In Pregnancy
dr. I Gede Mega Putra, SpOG(K)
Learning Task
CASE :
A 35 years-old G1P0 woman present for her prenatal visit at 34 weeks gestation. Her BP is 165/110. she has no history of hypertension.
1. What steps do you perform as part of your initial investigation? 2. What is your differential diagnosis and working diagnosis?
3. What are the reason do you explain for the differential diagnosis and the working diagnosis?
4. What is the etiology of this disease?
5. What is the worst complication of the disease? 6. What are the caregivers must be able to do?
7. What is the plan for management and treatment of his case ?
Day 11
SHOULDER DYSTOCIA
Endang SriwidayantiLearning Task
CASE :
In the labor ward, you as a intern help a pregnant woman in second stage of labor. Following and easy application, after two time maternal pushing, there is moderately good descent during the first pull but this slows down as the head is half out.
a. What are potential causes for this and what is your plan of action at this point?. b. If shoulder dystocia is confirmed,
c. What is your management?
d. What are the complication if its occur? e. What will you do if the complication occur? f. What are the risk factor? And explain why?
Day 12
DERMATO - EMERGEMENCIES
Nyoman Suryawati Learning Task
Case 1
A 25 years old male come to emergency unit sanglah hospital with blistering skin rash. He had fever, cough and malaise 5 days before and get medication such us amoxicillin, parasetamol, and mucopect tablets from general practitioner. Two days later, he developed erythematous lesions over his extremities, face and trunk. Patient with weak condition, BP 120/80 mmHg, temp 40°C, RR 20x/minutes. From eye examination there is redness on conjungtiva, from mouth and genetalia examination we find multiple erosion with hemmoragic crust. From his extremities, face and trunk we find multiple purpuric lesion and some part of rash with bullous and erotion that involve 45% BSA
LEARNING TASK
1. According this case, what is the most likely diagnosis?
2. What other information do you need to support the diagnosis? 3. What other examination you should do to this patient?
4. What monitoring should you do to this patient? 5. How do you manage this patient?
6. What is the complication of this condition?
SELF ASSESSMENT
1. Describe the principle clinical features of SJS, TEN 2. Describe the pathogenesis of SJS, TEN
3. Explain more detail the basic principle of management of SJS, TEN 4. Describe the prognosis and complication of SJS, TEN.
Case 2
A 8 months baby come to dermatology polyclinic sanglah hospital with skin rash all over the body. She had a fever, cough and rhinitis 6 days before. Two days later, she developed erythematous rash around the nose and the rash widespread all over her body with the skin peel easyly. Patient with weak condition, temp 38.5°C, RR 28x/minutes. Skin effloresence from face, trunk, back, and extremities, we find erythematous macule, some part of the lesion with multiple vesicle and desquamation skin.
LEARNING TASK
- What other information do you need to support the diagnosis?
- What other examination you should do to this patient?
- What monitoring should you do to this patient?
- How do you manage this patient?
- What is the complication of this condition?
SELF ASSESSMENT
- Describe the principle clinical features of SSSS.
- Describe the pathogenesis of SSSS
- Explain more detail the basic principle of management of SSSS
Day 13
TRAUMA WHICH POTENTIALLY DISABLING AND LIFE
THREATENING CONDITIONS
Dr.dr. Ketut Suyasa, SpB SpOT(K) Spine dr. IGN Wien Aryana, SpOT
LEARNING TASK
Case 1.
Male , 24 years old, admitted to our hospital after traffic accident, he was riding a motor bike. He suffered crush injury on his right lower leg 4 hours before admitted.
Primary survey : airway and breathing clear, circulation ; BP : 90/60 mmHg, HR : 120 x/minute. Distal part of lesion : pale, cold and non palpable pulsation of dorsalis pedis artery.
1. What is your initial assessment ? 2. How to manage this patient ?
Case 2
Male, 20 years old, came to our hospital after traffic accident, He was getting difficulty of taking his breath and restlessness.
On physical examination :
- A symetrically of thoracic movement
- Breathing sound (-) on the right side and hypersonor on percussion
1. What is your conclusion ? 2. How to manage the patient ?
Case 3
Girl, 13 years old, came to emergency department after traffic accident. She got lower leg pain on the left side
Physical examination ( Left lower leg) - Swelling
- Tense feeling - Painfull
- Stretch pain (+)
3. How to treat the patient ?
Day 14
Phlegmon
drg. Putu Lestari Sudirman
Learning task :
1. Patient female, 28 years old, with complaints of pain in the lower chin, up to the front of the neck feel hard when touched, fever, difficulty swallowing and difficulty
breathing, the patient appears weak. Intra-oral examination is difficult because patients with difficulty opening the mouth, tongue looks lifted and swelling of the gums behind that cover most of the right mandibular M3. Pain in the gums behind the perceived than 4 days ago, the patient just gargling with warm salt water when not withstand the pain.
a. As a doctor what would you do?
b. What examinations will you do for this case? c.What is the diagnosis?
d. What does your planning for management in this case?
2. Patient male, 38 years old, come to RSPTN with dread because of the pain that is felt in mandibulla left with swelling to the left cheek, intra oral condition appears to exist in the dental caries with mobillity o2 M2 residual roots on the left, buccal fold appears
elevated, palpation there is fluctuation exudate. Dental pain is felt starting from 3 days ago but have not had time to check to the dentist, just buy painkillers to reduce the pain.
a. What you should ask to complete the anamnesis? b. What is the diagnosis?
c. What does your planning for management in this case?
3. Patient woman, 38 years old, with complaints mandibulla swollen and hard when touched on the lower jaw side since a few months ago, seemed teeth no complaints. There is no pain and illness but the patient had never examined the situation to the doctor or dentist.
a. What you should ask to complete the anamnesis? b. What is the diagnosis?
c. What does your planning for management in this case?
Self Assassment:
Day 15
Urologic Concern in Critical Care for NonTrauma Case
dr. Gede Wirya Kusuma Duarsa, M.Kes, SpU(K)
Learning Task
Case 1 An Old man that unable to void
A 73 years – old man with multiple medical problems presented with complaints that he could not void and had pain in the lower abdomen. He had a mild dementia, so much of the history was from his wife, who accompanied him to the clinic. She stated that he had neither incontinence, fever, nauses, nor vomiting, and he had any recent acute illnesses. The patient had not had any recent change in medication, doses or frequency of dosing of his pain medication. He had similar problems in the past, but the symptoms had resolved after he underwent a transurethral resection of the prostate (TURP) 2 years ago. His wife also stated that he had been able to void normally up until earlier this morning. Since that time he had complained frequently about the urge to void and being to do so.
The patient’s medical history was extensive. Of particular note, he had metastatic squasmous – cell lung cancer and was placed in hospice care 2 weeks before presentation. He had type 2 diabetes, hypertension, glaucoma, and benign prostatic hypertrophy (BPH)
His medication included an extended – release morphine tablet for pain, rosiglitazone for his diabetes, and recently discontinued ramipril and hydrochlorothiazide, which he had taken in the past for his hypertension.
On examination, he was midly tender over the bladder, which was palpably distended. He attempted to void for a urinalysis specimen and was unable to do so. A Foley catheter was placed, and 240 ml of urine was collected. The urinalysis showed a trace of protein, and results were otherwise negative; the pH was 7,3.
Question :
1. What are some cuases of acute urinary retention?
2. What are some typical symptoms of acute urinary tract obstruction?
3. What tests would be helpful in determining the cause of this patient’s urinary retention?
4. What treatments would be useful in relieving the symptoms? 5. What are some complications of untreated acute urinary retention?
Case 2.
Seorang laki-laki umur 60 thn datang ke UGD dengan keluhan bengkak bernanah pada penis dan scrotumnya sejak 2 hari. Riwayat sulit kencing sejak 1 bulan sebelumnya dan pernah 2x dipasang kateter dan dilepas lagi. Riwayat DM dengan terapi tidak teratur selama 10 tahun Jelaskan tentang
b. Pemeriksaan penunjang c. Penanganan kasus di atas
Case 3.
Seorang laki-laki umur 56 thn datang ke UGD dengan keluhan nyeri pinggang kanan dan demam intermitteen selama 3 hari. Riwayat kencing keluar batu berulang. Pasien tampak gelisah dengan T 85/60, N 96x/mnt dan RR 24x/mnt. Jelaskan tentang
a. Differensial diagnose b. Pemeriksaan penunjang c. majemen kasus diatas
Case 4.
Seorang wanita umur 52 tahun datang ke UGD dengan keluhan sesak nafas dan tidak keluar kencing sejak 2 hari. Riwayat sering keluar darah dari vagina sejak 2 bulan. Dari pemeriksaan fisik ditemukan takikardi dan takipnea. Flank kanan dan kiri terasa nyeri ketok. Jelaskan tentang
a. Differensial diagnose b. Pemeriksaan penunjang c. Penanganan kasus diatas
Please answer these questions
1. Sebutkan penyebab Hematuria dan manajemennya 2. Definisi urosepsis dan penatalaksanaannya
Day 16
Urologic Concern in Critical Care for Trauma Case
LEARNING TASK
Explain your initial assessment, further clinical investigation needed and advise for appropriate management according to the scenario presented below ;
a. A male 50 years old involved in a mass fight and afterward he came to emergency department (ED) with a stab wound in his right upper abdomen. He also complained of gross hematuri. His vital sign were stable.
b. A 25 years old male complained of having bloody discharge from his penis after fell down from the stair 3 hours before admitted to hospital. He also feel pain on his groin and lower abdomen area. He found himself very difficult to void.
c. A man was driving a car when suddenly crash to a parking car in front of him. He complained of pain on his lower abdomen, difficulties in voiding and hematuria. Physical examinations found bruise on his lower abdomen with a full bladder. the clinicians at ED was unable to pass the urine catheter.
d. A 12 years old boy was riding a bycycle when suddenly fell down in to a rocky road. we found a dirty open wound on his scrotal skin 4 cm long.
e. Young female came to ED with right flank pain and gross hematuria after traffic accident. initially vital sign were found stable but 30 minute later the blood pressure were 90/60 and pulse rate reached 112x/ mnt. Fluid rescucitation with crystalloid were done with no response.