1
PHYSICAL ACTIVITY AND OSTEOPOROSIS FRACTURE
AMONG OLDER WOMEN IN MALAYSIA
(Ex Post Facto Study of Physical Activity and Osteoporosis Fracture In Malaysian women of 50 years and older in outpatient and orthopedic
department of Malaysian Hospitals, Kuala Lumpur, Malaysia)
THESIS
A Research Project Submitted in Partial Fulfilment of The Requirement of Postgraduate for Sport Science Master Degree Program
by:
RABIAH ABDURRUHMAN OMAR A 121302038
POSTGRADUATE PROGRAM SEBELAS MARET UNIVERSITY
SURAKARTA 2015
STATEMENT OF ORIGINALITY AND PUBLICATION OF CONTENTS THESIS
I stated clearly that:
1. Thesis entitled: “PHYSICAL ACTIVITY AND OSTEOPOROSIS FRACTURE AMONG OLDER WOMEN IN MALAYSIA” this is my own research work and plagiarism free. And there is no scientific papers that have been asked by others to obtain academic degrees and there is no work or opinion ever written or published by another person except in writing is used as a reference in this text and reference source as well as mentioned in the bibliography. If at a later proved there is plagiarism in this paper, then I am willing to accept the corresponding provisions of the law (Decree No. 17 of 2010).
2. Publication of part or all of the contents Thesis on scientific journals or other forums and permission must include supervising team as author and PPs-UNS sebgaia institution. If within at least one semester (six months after enactment of the thesis) I do not do the publication of part or all of this thesis, then Prodi Sport Science PPs-UNS entitled to publish it in a scientific journal published by Prodi-UNS Sport Science PPs. If I do penlanggaran of the provisions of this publication, I am willing to get academic sanctions that apply.
Surakarta, 2015
Rabıah Abdurruhman Omar A 121302038
MOTTO
“We will never know the real answer, before you try” (anonim)
“If you want the respect of others, you must respect yourself first”
(anonim)
"Be a good man, because Allah loves the goodness" (the writer)
v
DEDICATION
This paper is dedicated to:
1. Abd alrahman and Fatima, my parents who have been educated with simplicity, compassion with tolerance and patience above all prayer and boundless sacrifices that he always gave to the author.
2. Ebrahim and Hasna and Fatima and Yousef my husband and my children dear, who always gives warmth and motivation that makes its own spirit to the author.
3. Brother and sister who always gives a special motivation so I have always been motivated to move forward.
4. My friends dear students of Sport Science Graduate Program, Sebelas Maret University that has been put together to share joy and sorrow during lectures and thesis preparation process.
INTRODUCTION
All praise and gratitude writer prayed Almighty God's gift. Because thanks to His mercy and grace, I can finish this thesis entitled “PHYSICAL ACTIVITY AND OSTEOPOROSIS FRACTURE AMONG OLDER WOMEN IN MALAYSIA (Ex Post Facto Study of Physical Activity and Osteoporosis Fracture In Malaysian women of 50 years and older in outpatient and orthopedic department of Malaysian Hospitals, Kuala Lumpur, Malaysia)”.
The authors wish to thank you especially to the supervisor that the Honorable Prof. Dr. Sugiyanto and Prof. Dr. Agus Kristiyanto, M.Pd which has deigned to provide motivation, direction, guidance, knowledge, inputs and corrections to this thesis can be resolved. As well as to the entire to fathers and mothers lecturer Sport Science Program Sebelas Maret University of Surakarta who has given science and knowledge to the author for his education at the Graduate Program, Sebelas Maret University of Surakarta.
On this occasion, the authors also express gratitude to:
1. Prof. Dr. Ravik Karsidi, M.S., as Rector of the University of Sebelas Maret, which has given permission to the author and the opportunity to participate in and complete the Graduate Program at the Sebelas Maret University of Surakarta.
2. Prof. Dr. Ir. Ahmad Yunus, M.S., as Director of the Graduate Program, Sebelas Maret University of Surakarta who has given the author the opportunity to gain knowledge of education in the Graduate Program.
3. Prof. Dr. Sugiyanto, as the first supervisor who has given direction and guidance in the preparation of the thesis.
4. Prof. Dr. Agus Kristiyanto, M.Pd., as Chairman of Sport Science Graduate Program, University of March, as well as a second supervisor who has given direction and guidance in the preparation of the thesis.
5. All those who helped in completing this thesis and the author cannot describe one by one.
Care and support they have given to the author will be given just reward by Allah Almighty and be charitable and glory for all of us.
Surakarta, 2015
Rabıah Abdurruhman Omar
PRONOUNCEMENT
This is to pronounce that the writer himself wrote the thesis entitled "physical activity and osteoporosis fracture among older women in Malaysia".
Then, the thesis is not plagiarized or made by others. Anything related to other's works are written in quotation added with the name of the authors where the resources are listed on the bibliography.
If then this pronouncement is proven to be wrong, the writer is prepared to accept any academic punishment, including the withdrawal of his academic degree.
Surakarta April , 2015
ACKNOWLEDGMENT
Thanks to Allah the almighty, for his blessing and his mercies from which the writer has got the power to complete this thesis writing.
The Thesis is written to fulfill the requirement for Master's degree from graduate program of sport since education department of Sebelas Maret University Surakarta.
I am able to finish my thesis writing entitled "physical activity and osteoporosis fracture among older women in Malaysia"
The writer wishes to express his greatest appreciation on the supervisors: prof. Dr. Sugiyanto , as the first Supervisor and prof, Dr Agus Kristiyanto . as the second supervisor for their invaluable. And the writer also would like to express the deepest gratitude to:
1. The director of graduate program of the university of Sebelas Maret Surakarta. 2. The Head of sport since Education Department of Graduate program of the
University of Sebelas Maret Surakarta, prof, Dr . Agus Kristiyanto.
ABSTRACT
Rabiah Abdurruhman Omar, A 121302038 (Physical Activity And Osteoporosis Fracture Among Older Women in Malaysia) THESİS Sport Science Program Study, Post Graduate Program, Sebelas Maret University Surakarta, April 2014. Advisor (1) Prof. Dr. Sugiyanto. (2) Prof. Dr. Agus Kristiyanto.
Osteoporosis is a major age related disease affecting millions of women throughout the world. In premenopausal women, high-impact exercise has been suggested to be the most effective regimen. In women the loss of bone mass accelerates as they go through menopause due to a reduction in estrogen level. To study the relationship of physical activity in three levels of mild, moderate, and vigorous on bone strength which presents osteoporosis risk, factors such as age, race, weight, social class, educational level, menopause age, past medical history, smoking, and drinking alcohol were selected and the correlation among them were analyzed.
The results showed that Menopause age was positively correlated with medical history, BMD levels, drinking habit, smoking habit, and negatively correlated with mild exercise “physical activities 1”. Medical history is positively associated with BMD levels. Smoking habit was positively associated with drinking habit and negatively correlated with moderate exercise “physical activities 2” and level of BMD. Drinking habit was negatively correlated with BMD levels and positively correlated with mild exercise “physical activities 1” and moderate exercise “physical activities 2”. Drug usage history was positively with early menopause age, medical history, social class and negatively correlated with mild exercise “physical activity 1” and moderate exercise “physical activities 2”. Mild exercise “physical activities 1” was positively associated with moderate exercise “physical exercise 2” and vigorous exercise “physical exercise 3” and negatively correlated with BMD levels. Moderate exercise “physical activity 2” was positively correlated with vigorous exercise “physical activities 3” and negatively associated with BMD levels. This study indicated that there is significant relationship between physical activity and osteoporosis risk among Malaysian women of 50 years and older.
Keywords: Osteoporosis, Physical activity, and Fracture.
TABLE OF CONTENTS
TITLE ... i
PRONOUNCEMENT ... ii
ACKNOWLEDGMENT ... iii
ABSTRACT ... iv
TABLE OF CONTENT ... v
TABLE OF APPENDIXES ... vii
TABLE ... viii
TABLE OF FIGURE ... ix
CHAPTER I INTRODUCTION A.Background of the Study ... 1
B.Research Problems ... 8
C.Objectives the Study ... 9
D.Significance of Study ... 10
CHAPTER II UNDERLYING THEORY A.Theory ... 11
B.Conceptual Framework ... 47
C.Research Variables ... 48
D.Research Hypothesis ... 51
CHAPTER III RESEARCH METHODOLOGY A.Place and Time ... 53
B.Method of the Research ... 53
C.Population and Sample ... 54
D.Data Collection ... 55
E.Data Analysis ... 55
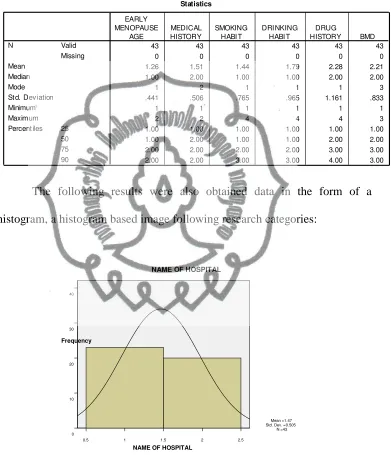
CHAPTER IV RESULTS AND DISCUSSION A.Description Data ... 57
B.Result of the Research ... 66
C.Discussion of Result Data Analysis ... 73
CHAPTER V CONCLUSION, IMPLICATION AND RECOMMENDATION A.Conclusion ... 67
B.Implication of Study ... 69
C.Suggestion ... 70
REFERENCES……… 81
xiii
TABLE OF APPENDIXES
Appendix 1 Questionnaire ... 83
Appendix 2 Data Analysis……….. 88
Appendix 3 Description ... 91
Appendix 4 Analysis of Correlations ... 98
Appendix 5 List of Acronym ... 100
TABLE
Table II.1 Common causes of secondary osteoporosis ... 16
Table IV.1 Description Data ... 57
Table IV.2 Description Data (Continue) ... 58
Table IV.3 Characteristics o f the Sample ... 67
Table IV.4 BMI (kg/m2) ... 68
Table IV.5 Menopause Stage ... 68
Table IV.6 Medical History of the Sample ... 69
Table IV.7 Osteoporosis Minor Risk Factors of the Sample (Smoking & Drinking) ... 71
Table IV.8 Level of Osteoporosis of the Sample ... 72
Table IV.9 Reliabilities, Means, and Standard Deviations of Scales ... 73
TABLE OF FIGURE
Figure II.1 Normal Bone Tissuean ... 11
Figure II.2 Osteoporotic Bone Tissue ... 11
Figure II.3 Bone repair process after an osteoporosis fracture ... 14
Figure II.4 A Hip Fracture ... 18
Figure II.5 Vertebral fracture ... 20
Figure II.6 Certain exercises recommended for osteoporotic patients .... 40
Figure IV.1 Name of Hospital ... 58
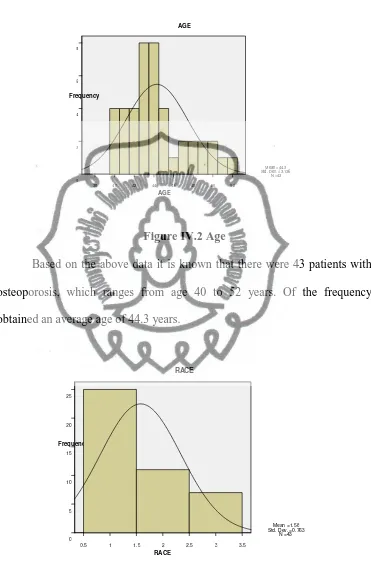
Figure IV.2 Age ... 59
Figure IV.3 Race ... 59
Figure IV.4 BMI ... 60
Figure IV.5 Social Class ... 61
Figure IV.6 Level of Education ... 61
Figure IV.7 Early Menopause Age ... 62
Figure IV.8 Medical History ... 63
Figure IV.9 Smoking Habit ... 63
Figure IV.10 Drinking Habit ... 64
Figure IV.11 Drug History ... 65
Figure IV.12 BMD ... 66
1 CHAPTER I INTRODUCTION
A. Background of the Study
The word osteoporosis means porous bones in Latin. Osteoporosis is a common bone disease in older adults and a major public health problem worldwide, that causes bones to become weak, fracture brittle and prone. That's an appropriate description of what happens to the skeleton when someone has the disease. Due to a loss of bone tissue, bones that were once dense and strong may be unable to withstand the stress of even normal activity, such as bending over or twisting torso to look behind. The inside of a normal bone has small spaces, like a honeycomb. In osteoporosis, the size of these spaces increases so that the bones lose strength and density. At the same time, the outside of the bone also grows weaker and thinner. Therefore, as bones become more porous and fragile, the density and quality of bone are reduced and the risk of fracture is greatly increased.
Osteoporosis is often called the "silent disease," because most of the time, bone loss occurs without any symptoms at all. When osteoporosis becomes severe, it can lead to fractures and a condition called kyphosis, which is a spinal compression and sometimes described as the dowager's hump. Both fractures and kyphosis can be very painful. This pain is usually more severe than the typical aches and pains that many people feel, as they get older. Osteoporosis, or thinning bones, can result in painful fractures.
The Consensus Development Conference statement in 1993 defined osteoporosis as a disease characterized by low bone mass and micro architectural deterioration of bone tissue, leading to an enhanced bone fragility and a consequent increase in fracture risk (Meyer et al., 2000). In 1994, the World Health Organization (WHO) established Bone Mineral or Mass Density (BMD) measurement criteria allowing the diagnosis of osteoporosis before incident fractures (Willig et al., 2001).
In 2000, the National Institute of Health (NIH) of the United States defined osteoporosis as a disease of deteriorating bone strength that leads to increasing risks for bone fracture. The bone strength by NIH‟s definition is
composed of two major indexes, which are bone density and bone quality. The largest part of the bone growth happens during puberty when over sixty percent of the bone mass is synthesized. After this period, it is a balance between production and break down, which determines the total bone mass.
For instance, when the skeleton undergoes more resorption than generation of tissue over time, a person may develop osteoporosis. Bone loss starts at the trabecular tissue, which has a bigger surface and therefore lower bone density compared to compact cortical tissue. Both local and systemic regulatory systems are important to maintain this homeostasis while skeleton is undergoing continuous modeling and remodeling (Vuori, 2004). Modeling results in creation of bone mass in response to mechanical loading and changes the shape of bones without previous resorption while remodeling denotes continuous bone formation and resorption, but the bone shape
remains. Among young people this process is balanced and the amount of bone resorption is completely replaced during bone formation. As age increases, however, less bone tissue is formed compared to the mass and therefore resorption causes an accumulated bone loss.
1. Osteoporosis in Women
Osteoporosis is a major age related disease affecting millions of women throughout the world. It is characterized by a decreased amount of bone and increased susceptibility to fracture. In women, the loss of bone mass increases as they go through menopause. A decrease in estrogen hormone level results an increase of bone loss (Wolff et al., 1999). The loss of bone occurs silently and progressively. Often there are no symptoms until the first fracture occurs. Postmenopausal osteoporosis happens during and after menopause as level of the bone-building hormone, estrogen, declines, which is also called type 1 primary osteoporosis.
In most women, menopause occurs around age 50. Estrogen level begins to fall 2 to 3 years before last menstrual cycle. The decline continues until 3 to 4 years after last menstrual cycle. Bone loss accelerates because estrogen, which provides valuable assistance in maintaining bone health, is no longer sufficiently available. A woman may lose 1 to 3 percent of bone mass a year during the first 5 to 7 years after menopause. Around age 70, bone loss slows but doesn't stop. By old age, many women have lost 35 percent to 50 percent of their bone mass.
2. Osteoporosis Treatment
Although osteoporosis is more common in women than in men, the incidence in men is also increasing. The disability, mortality, and cost of hip and vertebral fractures are substantial in the rapidly growing, aging population so that prevention and treatment of osteoporosis is a major public health concern (Meyer et al., 2000)
No certain treatment is yet available for osteoporosis once it is established. Fluoride, which stimulates bone formation, may decrease bone resorption but do not necessarily increase bone mass and therefore prevent further fractures. Recent evidences have, however, suggested that estrogen treatment in osteoporotic women significantly increases spinal bone mass and reduces the rate of vertebral fracture (Albertsson et al., 2007).
3. Osteoporosis Fractures
Osteoporosis is based on the major risk factor such as reduced bone strength or density, which includes those individuals at a high risk but without fractures. Despite the use of a „„bone mass‟‟ definition, it is
important to realize that bone density is a single risk factor, measured at a single point of time. Other risk factors include aging, being female, life expectancy, bone loss, bone turnover, low body weight, low sex hormones or menopause, smoking, and some medications also have important considerations.
As bones become more brittle with age due to bone mass loss, there is a greater risk of incurring an osteoporosis fracture. Approximately
40% of women and about 10- 15% of men suffer from fracture, especially of vertebral bodies, the femur and the forearm. The estimated incidence of femoral neck fractures is about 1.66 million per year worldwide. As life expectancy goes up, the incidence of osteoporosis increases four fold (Roche Diagnostics, 2009).
Fractures due to skeletal fragility in elderly people are an increasing public health issue worldwide, and the devastating medical and social costs can be expected to increase unless effective prevention and treatment regimens are developed. Hip fracture is the most severe complication of osteoporosis, placing the greatest demand on resources and having the great impact on patients because of increased mortality, long-term disability and loss of independence (Willig et al., 2001).
Exercise has been shown to be essential for maximizing peak bone mass and reducing subsequent bone loss (Beck et al., 2003). In premenopausal women, high-impact exercise has been suggested to be the most effective regimen.
4. Epidemiology of Osteoporosis
The incidence of osteoporosis and resulting osteoporotic fractures is increasing.
Worldwide Epidemiology
Data demonstrate that Caucasian or Asian women are more susceptible to the osteoporosis. Both genetic and behavioral risk factors contribute to the development of osteoporosis (Piaseu and Belza, 2001).
A report from WHO Consensus Development Conference in 2000 (Consensus Development Conference 1991) described that in the United States there are approximately 1.3 million patients suffering from osteoporotic fractures per year. Among these, about 50% had vertebral fractures, another 25% had hip fractures and the last 25% had wrist fractures or others. Additionally, there were reports stating that about 30% of European women who were 50 years old or more had osteoporosis. According to the United States National Health and Nutrition Survey (NHANES III) in 1997, there was an estimate that 13-18% of female American Caucasian having osteoporosis while 27-50% of all American Caucasian women had osteopenia, which enhanced the rate of onset for osteoporosis in these women when they become older. On the other hand, looking only at the American Caucasian female population aged 80 or more, about 70% of them will have osteoporosis.
In general, bone fractures are much more prevalent in men than in women since from adolescence to middle age men‟s lifestyle and
activities are generally more physically intense, including some activities that are more risky and/or more dangerous than those that are common to women. It was found that men experienced bone fracture as the consequences of high-energy trauma. However, after the age of 40-50 bone fracture incidence seems to be totally opposite to what occurs with females. Bone fractures from various parts of the body such as
wrists, vertebra, pelvis and hip in women are substantially increased (Melton et al., 1992).
In these cases fractures are the results of low-energy trauma; in other words, they are osteoporotic fractures. In the United States, there are about 500,000 cases of spinal fractures per year (Melton et al., 1992) and there are ten times more prevalent in women than in men. It can be said that half of American Caucasian females age of 70 or more have fractures at one or more vertebrae. For hip fractures, the incidence rate in the Caucasian female population ranged from the highest, 737 fractures per 100,000 population per year for Norwegian females, to the lowest, of 280 fractures per 100,000 population for Finnish women (Maggi et al., 1991).
Epidemiology in Asia
The incidence rates in Asian countries are increasing every year. For example, with Hong Kong Chinese females, the incidences for hip fracture almost doubled from 179 fractures per 100,000 population in 1965 to 389 fractures per 100,000 population in 1985 (Lau, 1997). Recently in Japan, a study shows that the incidence of hip fractures rose from a total of 92,400 cases from 1997 to 2001 to 117,900 yearly (Orimo Nakamura and Fukunaga, 2006). There is also an estimation of more than 6 million cases of hip fracture occurring worldwide in 2050 and half of these, or 3 million cases, will happen in Asia (Lau, 1997).
5. Physical Activity
In premenopausal women, high-impact exercise has been suggested to be the most effective regimen. In women the loss of bone mass accelerates as they go through menopause due to a reduction in estrogen level.
B. Research Problems
Osteoporosis impacts both morbidity e.g. pain, fractures and immobility in life. As people are getting older, osteoporosis will affect a constant bigger part of the population. Although nowadays there are more educated people, but as the structure of the society has changed, people for instance use more cars and have more passive professions, the total physical activity in a population is markedly reduced. It‟s estimated that 30-50 % of the women and 15-30 % of men suffer from osteoporotic associated fracture during lifetime.
Therefore, it is necessary to determine whether higher levels of physical activity reduce the incidence of distal forearm and proximal humerus, hip and vertebral osteoporotic fractures among Malaysian women 50 years of age and older. This study addresses the following questions: 1. Why exercise is important to reduce osteoporosis fracture?
2. How physical activity is effective to treat osteoporosis fracture? 3. What are preventive methods to reduce osteoporosis fractures?
The current study investigates the pattern of past physical activity in 3 levels of mild, moderate and vigorous at various stages throughout life, and evaluates the impact of physical activity on future osteoporosis.
C. Objectives of the Study
This study aims to explore the impact of physical activity on bone strength to reduce the incidence of osteoporosis, morbidity and mortality related osteoporosis among older Malaysian women of 50 years and older from the perspective of physical activity. The objectives of this study are as follows:
1. To determine incidence of osteoporosis and osteoporosis fractures among Malaysian women of 50 years and older
2. To define the relationship between osteoporosis fractures and physical activity
3. To examine the impact of exercise frequency on osteoporosis fracture among Malaysian women of 50 years and older
4. To study the risk factors associated with osteoporosis among Malaysian women of 50 years and older
5. To increase health awareness among older Malaysian women in order to deal with the disease in a better efficient way.
D. Significance of Study
The present study is expected to imply possible preventive actions that can be taken in adulthood to decrease the likelihood of developing osteoporosis throughout the normal lifetime aging process.
11 CHAPTER II UNDERLYING THEORY
A. Theory
1. Osteoporosis
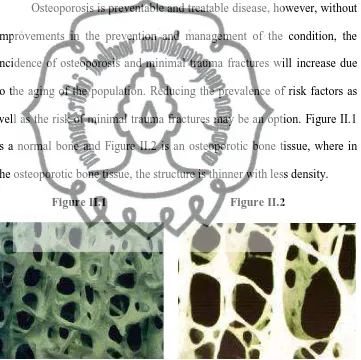
Osteoporosis is preventable and treatable disease, however, without improvements in the prevention and management of the condition, the incidence of osteoporosis and minimal trauma fractures will increase due to the aging of the population. Reducing the prevalence of risk factors as well as the risk of minimal trauma fractures may be an option. Figure II.1 is a normal bone and Figure II.2 is an osteoporotic bone tissue, where in the osteoporotic bone tissue, the structure is thinner with less density.
Figure II.1 Figure II.2
Normal Bone Tissuean Osteoporotic Bone Tissue
2. Pathogenesis
formation while bone resorption is less which results in deposition of bone tissue until the point when the bone stops growing. This point with the highest density of bone mass is called Peak Bone Mass, which is at 30-34 years of age (Limpaphayom et al., 2001). After that, there is a balance between bone formation and bone resorption and results in constant bone mass. At the age of 40-45 years, the rate of bone formation starts to decline and that equals to a balance shift towards bone resorption, which results in decreasing of bone mass. After a woman enters menopause, the rate of bone resorption will increase tremendously, whereby the continuous loss of bone mass occurs. Bone mass will eventually decline and thus enhances the risk of bone fracture, which is called the state of having osteoporosis. Therefore, any treatment or prevention that decelerates the rate of bone resorption decreases the risk of osteoporosis. 3. Bone Mass
The most important factor for bone mass is ethnicity. It was found that the highest bone mass is Africans, followed by Caucasians and Asians. In terms of genetics, the peak bone mass of a person is closely related to his/her mother‟s bone mass density. On the other hand, strength training in children and adolescents increases their peak bone mass. In contrast, smoking cigarette and consuming alcohol beverages reduce the peak bone mass (Lau et al., 2001).
The rate for bone resorption in women is high and rapid during the first 10 years after menopause and this is called postmenopausal bone loss.
The rate of bone mass decline can be about 3-5% per year due to reduction of estrogen levels which induces osteoclast activity, thus increasing bone resorption. This process takes place in cancellous or trabecular bone rather than cortical bone, hence bone fracture in postmenopausal women often happens in more porous bone such as spine. After this period, the rate of bone deterioration declines, being almost the same as what occurs in males (Chien et al., 2005). However, some women may lose bone at a higher rate during the rest of their lives.
In comparison to women, the rate of bone resorption in men is less with only 1-2% per year, starting from the age of 40-50. The major reason of bone loss in men and women is due to inefficient osteoblasts, called age-related bone loss. In both genders, there is an exponentially increased incidence for osteoporotic fracture as age increases. In women, the incidence increases from the age of 65 compared to 70-75 in men.
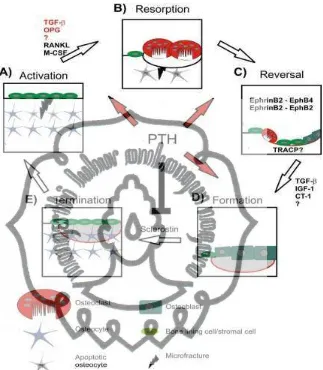
Glucocorticoids, vitamin D deficiency, some endocrine diseases such as thyroid and parathyroid diseases and rheumatoid arthritis are other factors that accelerate the bone resorption. The most important cause of osteoporotic fractures is an external compression, which usually occurs because of a fall. Factors involved in a fall are commonly (Limpaphayom et al., 2001) postural reflex control, muscle coordination, visualization and fat padding around the bone that absorb the compression and age is extremely relevant to all of these factors. Figure 2.2 shows the process of bone tissue repair after an osteoporosis fracture.
4. Types of Osteoporosis a. Primary Osteoporosis
Primary osteoporosis occurs in patients, in whom a secondary cause of osteoporosis cannot be identified, including juvenile and idiopathic osteoporosis. Juvenile osteoporosis usually occurs in children or young adults of both sexes. Idiopathic osteoporosis can be further subdivided into postmenopausal (type I) and age-associated or senile (type II) osteoporosis. Type I osteoporosis occurs in women aged 50-65
Figure II.3 Bone repair process after an osteoporosis fracture
years and is characterized by a phase of accelerated bone loss in trabecular bone. In this phase, fractures of the distal forearm and vertebral bodies are common. Postmenopausal bone loss is the results of increased bone desorption or in other term high turnover related to the reduction of estrogens production. The process of bone loss proceeds much more rapidly after menopause. Approximately 10-15 years after menopause, the initially accelerated bone metabolism normalizes and mainly age-associated processes affect bone mass evolution (Kosmin, 2011).
Type II osteoporosis occurs in women and men older than 70 years in their cortical and trabecular bone. In addition to wrist and vertebral fractures, hip fractures are often seen in patients with type II osteoporosis (Kosmin, 2011). Age-related osteoporosis is caused by a decrease in bone production resulting from the deterioration of osteoblast, occurred in both male and female.
b. Secondary Osteoporosis
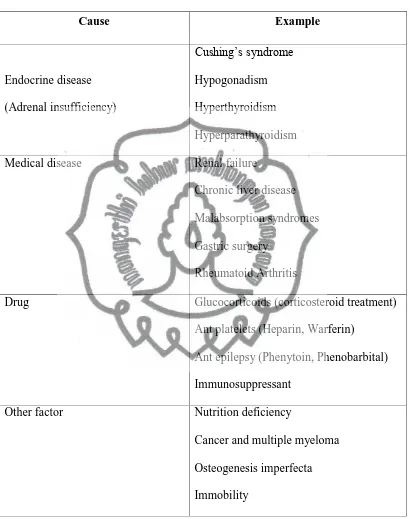
When osteoporosis occurs as a consequence of a disease or a drug, it is termed as secondary osteoporosis (Roche Diagnostics, 2009). Common causes of secondary osteoporosis are shown in Table II.1.
Table II.1 Common causes of secondary osteoporosis
Cause Example
Endocrine disease (Adrenal insufficiency)
Cushing‟s syndrome
Hypogonadism Hyperthyroidism Hyperparathyroidism
Medical disease Renal failure
Chronic liver disease Malabsorption syndromes Gastric surgery
Rheumatoid Arthritis
Drug Glucocorticoids (corticosteroid treatment)
Ant platelets (Heparin, Warferin) Ant epilepsy (Phenytoin, Phenobarbital) Immunosuppressant
Other factor Nutrition deficiency
Cancer and multiple myeloma Osteogenesis imperfecta Immobility
5. Osteoporosis Fracture
Normal bone is a living, strong and flexible tissue that adapts to mechanical load. However, in some people and situations, bone is more brittle and fractures may occur. The fracture happens in both sexes at any age, but is more common in women over 50 years old.
Women with osteoporosis may take several fractures with accumulative sequelae, which could shorten their vital and good period of their life. A 50% of Swedish women and about 80% of Swedish men never take a fracture in their lifetime, whereas some sooner or later are severely affected by osteoporosis and take several fractures.
Typical osteoporotic fractures are fractures of the vertebrae (spine), hip, proximal humerus and distal forearm (wrist). Almost all types of fractures are related to low BMD and, therefore, these age-related fractures could be osteoporotic in nature (Cummings and Melton, 2002). Regardless of the type of fracture, women with prior fractures had twice the risk of subsequent fracture compared with women without prior fracture (Klotzbuecher et al., 2000).
a. Distal Forearm and Proximal Humerus Fractures
In Sweden, distal forearm (aka. reverse Colles‟ or Smith‟s fractures) and proximal humerus fractures account for approximately 25,000 and 10,000 fractures annually (Sääf et al., 2003). The lifetime risk of forearm fracture in women of 50 year old in Sweden has been estimated to 21% (Johnell and Kanis, 2005). Besides, pelvis and ribs fractures also occur in women with osteoporosis. Except facial and
skull fractures, all fractures are related to low BMD or osteoporosis (Stone et al., 2003).
b. Hip Fractures
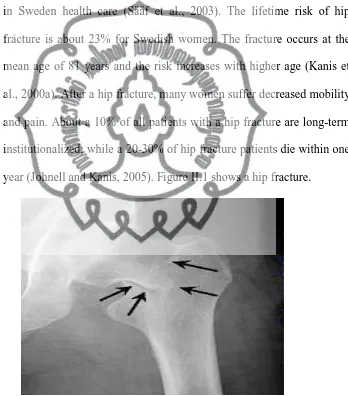
Hip fractures are either cervical or trochanteric and account for approximately 26% (18,000) of the 70,000 fractures recorded annually in Sweden health care (Sääf et al., 2003). The lifetime risk of hip fracture is about 23% for Swedish women. The fracture occurs at the mean age of 81 years and the risk increases with higher age (Kanis et al., 2000a). After a hip fracture, many women suffer decreased mobility and pain. About a 10% of all patients with a hip fracture are long-term institutionalized, while a 20-30% of hip fracture patients die within one year (Johnell and Kanis, 2005). Figure II.1 shows a hip fracture.
Figure II.4 A Hip Fracture c. Vertebral Fractures
Vertebral fractures can be classified into two major categories as subclinical and clinical. Overall, only about one third of all patients
with vertebral fractures identified on radiographs came to clinical attention and about 50% of patients were reported with back pain and 8% were hospitalized (Ross, 1997). Even when there is a vertebral fracture on the radiograph, it is often not mentioned by the radiologist, therefore it is rarely noted in the medical records and infrequently prompts preventive medical treatment (Gehlbach et al., 2000). The prevalence of radiographic vertebral deformity is increased in Europe, from 11.5% in women 50-54 years of age to 35% in women 75-79 (O'Neill et al., 1996).
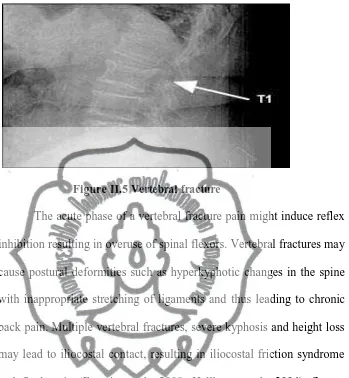
Vertebral fractures most commonly occur at the thoracolumbar junction and in the mid-thoracic area (Papaioannou et al., 2002). The lifetime risk of a clinically defined vertebral fracture at the age of 50 for a woman has been estimated at 15.1% (Johnell and Kanis 2005). It is generally believed that pain and disability after a vertebral fracture persist only for a few weeks or months (Silverman, 1992). Some studies, however, have described women who suffer from long-lasting pain and disability (Hasserius et al., 2005), as well as psychosocial consequences (Gold, 1996), for several years after the fracture. Further studies of Health-Related Quality of Life (HRQL) after vertebral fracture are needed, as methods for early identification of women at high fracture risk. Figure II.4 shows a vertebral fracture.
Figure II.5 Vertebral fracture
The acute phase of a vertebral fracture pain might induce reflex inhibition resulting in overuse of spinal flexors. Vertebral fractures may cause postural deformities such as hyperkyphotic changes in the spine with inappropriate stretching of ligaments and thus leading to chronic back pain. Multiple vertebral fractures, severe kyphosis and height loss may lead to iliocostal contact, resulting in iliocostal friction syndrome and flank pain (Francis et al., 2008; Hallberg et al., 2004). Severe vertebral fractures in the thoracic spine result in a decreased lung capacity, which may result in respiratory symptoms. Vertebral fractures in the lumbar spine result in a decreased abdominal volume and cause the abdomen to protrude. A spinal orthosis might decrease the kyphotic angle, reduce pain and improve quality of life (Pfeifer et al., 2004).
physiotherapists working in the clinic to get an eventual hint of possible osteporotic vertebral osteoporosis (Moayyeri et al., 2008).
Performing isometric contraction of par spinal muscles might decrease post vertebral fracture pain and oedema. Physiotherapists should supervise osteoporotic persons to perform back strengthening exercises for instance "back-ups" lying prone (with a pillow under the stomach) and raising the upper part of the body a bit from the surface without the support of the arms, in order to improve muscle strength, vertebral bone mass, and to relieve back pain. Such back strengthening exercises may help to reduce the risk of further vertebral fractures (Francis et al. 2008, Hongo et al. 2007, Malmros et al. 1998, Sinaki et al. 2002).
6. Risk Factors of Osteoporosis Fracture a. General Risk Factors
Without a bone fracture, there may be no obvious physical evidence of osteoporosis symptoms during a medical examination. As a consideration of public health economics, it‟s not reasonable to check every one using a bone densitometer; therefore using risk factors assessment for osteoporosis and osteoporotic fractures, which is easy, comfortable and safe seems to be a more appropriate method to identify the need for further evaluation. National Osteoporosis Foundation recommends for a BMD testing for cases as follows: current smoking, low body weight (<127lb), family history of osteoporosis, personal
history of low trauma fracture at age >45 year, postmenopausal women (age 50–65) with risk factors for osteoporosis (besides menopause), women age 65 years and older regardless of additional risk factors, postmenopausal women who present with fractures, women considering therapy for osteoporosis if BMD testing would facilitate such decision and finally women who have been on HRT for prolonged periods. b. Menopausal Women‟s Risk Factors
Risk factors in menopausal women can be categorized as modifiable and non- modifiable factors. Non-modifiable risk factors are as follow: age (65 years and older), female, Caucasian and Asian women, early menopause (before age 45), women whose ovaries were removed before menopause, small body build, family history of fractures, and experience of bone fragility fracture, while modifiable risk factors are as follows: inadequate calcium intake, sedentary lifestyle, regular smoking, regular drinking of alcohol, regular and excessive drinking of coffee, Body Mass Index (BMI) lower than 19kg, excess exercise, propensity for falling due to impaired vision and estrogen deficiency in pre-menopause due to taking gonadotropin releasing hormone (GnRH) analogue.
7. Osteoporosis Symptoms
A decrease in bone mass in osteoporosis does not cause pain or other symptoms. Osteoporosis disease often happens to be asymptomatic until there is a broken bone or a fracture, thus it is called a silent disease.
Osteoporotic fractures cause pain and disability. In most cases this will remain throughout life, but in other cases it will gradually disappear or improve (Hurricane, 2005). Osteoporosis symptoms can be a pain in the bones, reduced height and body hunchback.
c. Pain in Bones
The bone pain in osteoporosis can be acute or chronic. Acute pain comes from a bone or periosteum due to a recent fracture, while chronic pain comes from the soft tissue due to a ligament and muscle deformity.
d. Reduced Height
Height shrinkage occurs due to compression fractures in the vertebrae and it is usually accompanied either by symptoms or asymptomatic, which lasts for several days with a severe pain to several months, respectively. A reduced height occurs if there is fracture in several places of the rear vertebrae for several times and therefore the height will be shorter than the long span arms. In normal circumstances, the height and the long span arms both have the same size. Long stretches of both arms are measured from the tip of the right middle finger across the chest to the tip of the left middle finger.
e. Body Hunchback
Body hunchback aka kyphosis is the spinal deformities, which can occur as the result of compression fractures.
8. Osteoporosis Diagnosis
There are mainly two criteria to diagnose osteoporosis either by measurement of BMD or by biochemical markers of bone turnover.
BMD can be measured by Dual Energy X-ray Absorptiometry (DXA). WHO diagnostic criteria are used to diagnose osteoporosis in women by comparing the measured BMD with maximum BMD in young women and considering lower value or one equal to 2.5 times of standard deviation for diagnosis of osteoporosis. Risk of bone fracture is increased 1.4-2.6 times for one time of decreasing of standard deviation (Grade A, Level Ia).
As biochemical index of bone formation and resorption is changed by several factors, it is not suggested to use biochemical markers of bone turnover for diagnosis of osteoporosis and in addition, it may be unusual in several diseases. However, it can be used together with BMD to assess risk of bone fracture. The index is useful for treatment monitoring after three months and a year and to assess response to treatment with rapid detection. Biochemical index of bone resorption includes urinary deoxypyridinoline (DPD), urinary N-telopeptide (NTx) and serum C-telopeptide (CTx) while biochemical index of bone formation includes bone specific alkaline phosphatase (BSAP), osteocalcin and N-terminal propeptide of type 1 procollagen (P1NP).
9. Osteoporosis Investigations
Osteoporosis investigations are performed through laboratory investigation and bone strength assessments.
a. Laboratory Investigation
The objective of laboratory investigation is to assure diagnosis of osteoporosis, to assess the risk of osteoporosis and to determine causes of osteoporosis. In a primary laboratory investigation, a complete blood count is done to measure the serum calcium, phosphate, albumin and liver transaminases as well as serum alkaline phosphates‟. Renal function is also assessed through blood urea nitrogen and creatinine. A plain x-ray is also suggested to check lateral thoracolumbar spine or anteroposterior hip in case of indicated or suspected of bone fracture.
b. Bone Strength Assessment
Bone strength includes bone mass and bone quality. The latter one is not currently assessed accurately by any technologies for clinical uses; therefore bone density is mainly used for clinical assessment of bone strength. In osteoporosis, bone mass must be decreased more than 30-40% of normal value and diagnosis using a plain x-ray is not sensitive enough to indicate this reduction to be visible on radiogram. On the other hand, using a semi-quantitative method to assess radiogram from a plain x-ray film, such as Singh‟s index, cannot
control the assessment standard and therefore due to highly intra-observer and inter-intra-observer, it is not suggested to be used.
According to WHO standard, only DXA can be used for bone mass measurements in order to diagnose osteoporosis and other technologies such as quantitative ultrasonography (QUS) or peripheral DXA (pDXA) cannot replace DXA although they are useful in screening people with high risk of osteoporosis.
10. Osteoporosis Treatment
Changes in the lifestyle such as physical activity, dietary habits and
smoking can have a positive effect to treat osteoporosis. Taking calcium
and vitamin D supplements may also treat osteoporosis. The NIH has determined that physical activity along with calcium consumption are two major factors affecting maximum achievement of bone mass. Bones are living tissue, and calcium gets deposited and withdrawn daily from the skeleton. When the body does not consume enough calcium or does not absorb it adequately, the bones become depleted, making them brittle and weak. Calcium is the main building block of bone and is essential for bone health, but calcium intake alone does not ensure healthy bones. For adults 19 to 50 years, an estimated adequate daily calcium intake is 1,000 mg per day (NIH Consensus Development Conference Statement, 2000).
Antiresorptive treatment such as bisphosphonates and Selective
Estrogen Receptor Modulators (SERMs) and anabolic treatment such as
treatment. For vertebral compressions, an orthopaedic intervention such as
kyphoplasty or vertebroplasty can be a treatment option.
11. Strategies of Osteoporosis Reduction
The eight main strategies enhance the potential for sustainable behavior and system changes that reduce the burden of osteoporosis and improve the quality of life for patients. These strategies have to be designed and coordinated that efforts in one area (e.g. professional education) reinforce efforts in other areas (e.g. public education). The strategies are as follows: promote bone health and prevent osteoporosis as primary prevention, detect osteoporosis early and provide evidence-based treatment both as secondary prevention, integrate fracture care, rehabilitation and osteoporosis management and promote self-management and falls prevention both as tertiary prevention, promote evidence-based practice, develop and transfer new knowledge and provide leadership.
Osteoporosis and the resultant fractures cause severe suffering and
have a devastating impact on quality of life and healthcare costs. The osteoporosis action plan attempts to reduce the burden of osteoporosis at all stages in the continuum of care of health promotion (primary prevention), diagnosis and treatment (secondary prevention), and fracture care, rehabilitation and falls prevention (tertiary prevention). It requires the active involvement of health professionals, the public, patients, facilities and organizations. The action plan recommends a health promotion and public education campaign to promote bone health, early diagnosis and
management of osteoporosis. Health professional education promotes appropriate utilization of BMD tests and preventative drug therapies. Changes in ministry processes ensure that people have improved access to BMD testing and effective osteoporosis drug therapies. A self-management network helps people with or at high risk of osteoporosis to manage their condition and enjoy the best possible quality of life. A province-wide fracture clinic intervention improves prevention, diagnosis and treatment for patients with fragility fractures. Five multidisciplinary teams in Academic Health Science Centers across the province provide better-integrated care for complex osteoporosis cases. Rehabilitation pilot projects test evidence-based service delivery models to help improve care.
There are abundant researches supporting the fact that osteoporosis is preventable (Lengacher and Sellers, 2000). Yet several studies indicate that a significant number of women do not have adequate knowledge about osteoporosis, the associated risk factors and preventive behaviors (Terrio and Auld, 2002). Weiss and Sankaran (1998) conducted a study at Pennsylvania University with 144 college-age sorority women that examined knowledge, attitude and behavior toward osteoporosis prevention. The survey analysis revealed generally poor knowledge about osteoporosis and prevention strategies but strong desire for information about the disease and preventive behaviors. Only 46% of their respondents correctly identified physical inactivity as a risk factor for developing osteoporosis. Thus, more than half of the young and at-risk women
surveyed were unaware of one of the most critical risk factors for osteoporosis; therefore conducting an osteoporosis education program is beneficial for college-aged women.
12. Physical Activity
Sufficient physical activity includes at least 30 minutes of moderate-intensity physical activity and noticeably increases breathing depth and rate but still allows person to talk comfortably on most, if not all, days of the week. The amount of physical activity can be accumulated in shorter bouts, such as three 10-minute walks. Physical activity is beneficial for pain relief and an obvious effect was found in osteoporotic women suffering from backache.
a. Healthy Aging
Older people benefit from an active lifestyle, yet more than half of Australian men and women aged 60–75 years are not sufficiently active. It is important for all old people to understand that the body retains its ability to adapt to exercise training throughout life, even in those with a previously inactive lifestyle. Regular moderate physical activity in old patients should be part of an overall approach to tackle cardiovascular risk factor such as smoking, diet, depression and social isolation, dyslipidaemia, high blood pressure and diabetes.
An active lifestyle helps prevent the typical age-related decline in functional capacity, which is partly due to inactivity rather than an intrinsic effect of aging. Progressive resistance training i.e. performing
movements against a specific external force that is regularly increased during training markedly increases muscle strength in people 60 years and over, and improves ability to complete everyday tasks such as walking, standing up from a chair or climbing stairs. A daily walking program can improve walking endurance, even in nursing home residents. Physical activity in older people, particularly resistance training, may reduce the risk of disability and hospitalization, improve quality of life, and allow individuals to retain their independence.
Resistance training benefits not only the healthy elderly, but also those who are frail or have chronic diseases including diabetes, painful osteoarthritis or chronic heart failure. An active lifestyle in younger adulthood is not sufficient for current health benefits. Health benefits are more strongly correlated with recent activity than past activity.
b. Cardiovascular Benefits
Physical activity has cardiovascular benefits in older men and women. In men aged 71–93 years, increasing distance walked per day correlates with reduced risk for coronary heart disease, independently of other risk factors. Inactive people who become active in old age can still achieve substantial health benefits and show a marked reduction in overall mortality compared with sedentary peers. Even in those with existing cardiovascular disease, physical activity has shown to improve functional capacity and mental well being, and reduce mortality rates in
some groups. Unless contraindicated, physical activity should be encouraged in older people with well-compensated, clinically stable cardiovascular disease.
c. Chronic Disease Improvement
Progressive resistance training has demonstrated to improve glycogenic control and significantly increase strength in older patients with type 2 diabetes. Aerobic exercise has shown to increase glucose uptake during glucose tolerance testing and improve exercise tolerance in elderly patients. In patients with chronic obstructive pulmonary disease especially over 60 years old, exercise programs improve cardiovascular fitness, exercise endurance and health-related quality of life and mood.
d. Falls and Fracture Prevention
Falls are responsible for 90% of hip and 50% of vertebral fractures. Patients with a known history of falls can be targeted for tailored programs of progressive muscle strengthening, balance retraining exercises and walking. These programs reduce fall rates in elderly people, and lower the risk of moderate-to-severe injury by more than one third. Progressive resistance training is appropriate for patients at risk of fracture, because it improves muscle mass, strength and balance.
e. Bone Mass Maintenance
Progressive resistance training can contribute to maintenance of bone mass in older people.
f. Osteoarthritis Disease
Aerobic exercise, even with low-intensity, is effective in improving aerobic capacity in people with knee osteoarthritis. Both supervised exercise classes and one-to-one instruction are effective. Physical activity does not cause disease progression in osteoarthritis and in fact progressive resistance training may reduce pain in older people with osteoarthritis.
g. Sleep Quality
Exercise may improve sleep and quality of life in the over-60 age group.
h. Surgical Recovery
A 3-month exercise prehabilitation program before abdominal or cardiac surgery may improve functional capacity and quality of life, reduce postoperative complications, shorten hospital stays and maximize function compared with preoperative physical inactivity. i. Mental Health
Emerging evidence suggests that physical activity e.g. supervised exercise groups and light resistance training is effective in alleviating symptoms of depression in older adults and may be as effective as antidepressant medication in this age group. Conversely,
physical inactivity is a risk factor for depression in the elderly (Australian Institute of Health and Welfare-AIHW, 2004).
j. Osteoporosis Management
The primary goal of osteoporosis management is the prevention of fractures, thus, the key question is which physical activity is the best prescription for patients with osteoporosis. In other words, which exercise can reduce the risk of osteoporosis-related fractures. In an osteoporosis-specific perspective, the reduction of fractures is the appropriate primary outcome parameter for an exercise program, analo-gously to pharmacotherapy, but no Randomized Controlled Trials (RCT) with enough statistical power have been conducted to prove a significant reduction of fractures through exercise interventions, thus, in respect to RCT-based evidence, it sounds impossible to conclusively answer the key question by restricting the approach to osteoporotic fractures.
For many reasons, it may be adequate to broaden the goals of exercise to muscle function, falls and mobility-related disability. Osteoporotic fractures are the result of both decreased bone strength and fall risk is a consequence of age-associated neuromuscular decline. This geriatric perspective addresses fall risk, sarcopenia and onset of disability in addition to fractures and bone strength.
Osteoporotic fractures are seen as a part and a manifestation of the age-associated decline of the neuromuscular–skeletal system,
eventually resulting in disability. Referring to osteoporosis as a disorder of the muscle–bone unit, the term sarcopenia is important and it is defined as age-associated decline of muscle mass or in a broader sense as a decline of muscle function, therefore the key question can be completed as which exercise prescription is effective in preventing falls and postponing sarcopenia and disability.
Instead of fracture incidence, bone mass and bone strength have been chosen as the outcome parameter of exercise interventions, operationalized by diverse methods of densitometry. The results are inconclusive and controversial, a finding which can partly be explained by inherent methodological limitations of DXA measurement, different populations and different interventions. In the field of exercise, describing the details of an intervention is more difficult than in pharmaceutical prescriptions, so it is not really surprising that there is neither convincing evidence nor common consensus about the best prescription of exercise for osteoporotic patients yet (Kalapotharakos, 2005).
k. Rehabilitation Training
Osteoporotic patients need adequate and skilled supervision for their individual rehabilitation training. A knowledgeable physiotherapist can motivate a fragile person to begin exercising not only for the rehabilitation period of a fracture, but also to become physically active for all their life. Correct supervision, feedback and
follow-ups are extremely important to encourage further physical activity in osteoporotic patients. Strength training of moderate intensity and balance exercises are beneficial for most osteoporotic people (American College of Sports Medicine, 2004).
It is important to begin an exercise session with a gentle 10-minute warm-up (Karinkanta et al., 2007). Weight-bearing exercises, which are performed in stable positions, are adequate for fragile persons. The exercises should be safe to minimize the risk of arthritic complications, falls and fractures. It is important that the physiotherapist individualizes the loading when training equipment and weights are used (Englund et al., 2005; Hourigan et al., 2008).
The loading should be site-specific and be increased progressively to attain the best possible effect on bone mass (Marcus, 2001). In a study by Karinkanta in 2007 with osteopenic/osteoporotic women (mean age of 73 years), the intensity of the training stimulus was set at 50-60% of one repetition maximum (1RM) using 2 sets and 10-15 repetitions. Thereafter, the intensity progressed to 70-80% of 1RM with 3 sets and 8-10 repetitions. After one year of combined resistance and balance-jumping training physical function, dynamic balance and muscle strength of the lower limbs were improved (Karinkanta et al., 2007).
In osteoporotic people, trunk rotation and flexion exercises such as sit-ups should be largely avoided as they may be harmful and
increase the risk of vertebral compression (Francis et al., 2008). Middle-aged postmenopausal women, who performed 10 back extension exercises (back-ups) at each training session 5 days/week for a 2-year period and were free to continue in any self-selected physical activities for another 8 years had significant fewer vertebral compressions compared to a control group at a 10-year follow-up (Sinaki et al., 2002). Similar home-training back extension exercises for 4 months improved both back muscle strength and HRQL in postmenopausal osteoporotic women (Hongo et al., 2007).
Other adequate home-training programs are exercises which are performed in stable positions e.g. positioned on the knees and hands (all fours) and trying to lift one arm and the opposite leg simultaneously while holding in a diagonal, standing with the palms placed against the neck or at the hips and simultaneously forcing the elbows back and straightening the back, and rising from a stable chair without using the arms (Albertsson et al., 2007; Kalapotharakos et al., 2005; Khan et al., 2001). A home-training program improved muscle strength, mobility and quality of life in osteopenic/osteoporotic postmenopausal women who performed the exercises regularly 7 days/week for 12 weeks (Chien et al., 2005).
Decreased muscle strength and deteriorated vestibularis function are important causes to impaired balance ability and increased frequency of falls amongst the elderly (Kristinsdottir et al., 2000; Choy
et al., 2007). Age-related changes are found both in strength and somatosensation at the age of 50-60 years. Postural sway during quiet standing has been found to increase with each decade of life in healthy adults aged 40-80 years.
The vestibular system shows a reduction in function, with a loss of 40% of the vestibular hair and nerve cells at the age of 70 years. Falls generally result from an interaction of multiple and diverse risk factors and situations. Age, disease and the presence of environmental hazards influence the incidence of falls and the severity of fall injuries. A fall should be defined as an unexpected event in which a person comes to rest on the ground, floor or lower level (Lamb et al., 2005).
Balance performance can be considerably improved at high ages by strength training of the lower extremities and by specific training, which is directed towards stimulating of the sensory systems (visual, vestibular and somatosenory) and their central integration (Kronhed et al., 2001; Kammerlind et al., 2001). Balance exercises can be performed in a training group by walking around and changing direction eventually combined by turning head or moving eyes, whole-body 360° rotation, walking on tiptoes and on heels, walking forward (heel to toe) and walking backward (toe to heel) on a line, jogging around a chair and turning to the left or right on command, standing on a foam support with the open and closed eyes, rising from the sitting to standing position and bowing to the left or right, exercising on balance
boards, and by various ball exercises (Hansson 2007; Kronhed et al., 2001; Kammerlind et al., 2001; Madureira et al., 2007).
Home exercises can be performed standing in a corner (eventually with the back of a chair placed close to the person to prevent falls) with both feet together on a firm or a foam support and trying to close the eyes for one minute, standing on one leg with the open eyes for half a minute if possible, rising up on toes 5-20 times and carefully bending knee 5-20 times (eventually holding on the back of a chair) (Albertsson, 2007). Regularly participation in Tai Chi or in balance training groups have decreased risk for falls and falls injuries among the participants (American College of Sports Medicine 2004; Bean et al., 2004, Howe et al., 2007, Kannus et al., 2005, Madureira et al., 2007).
Line dance is proposed as an adequate training for postmenopausal women due to positive effects on balance performance (Shigematsu and Okura, 2006; Young et al., 2007).
According to a consensus statement to recommend for promoting health, in all ages, people should accumulate 30 minutes or more of moderate-intensity physical activity on most, preferably all, days of the week (US Department of Health and Human Services, 1996). However, people suffering from established osteoporosis are recommended to walk at a quiet pace. An increased risk of falls associated to brisk walks (progressively increased pace) was found in
women (mean age 66 years) with a previous humerus fracture in 2 years.
After a period of inactivity (for instance after a healed fracture), it is extremely important that physiotherapists encourage osteoporotic patients to regularly practice physical activity in order to reduce their risk for falling accidents, dependence and helplessness. In women (mean age of 68 years) with a recent fall-related distal forearm fracture, a decline was found concerning walking capacity and handgrip strength on the non-fractured side on the first year after fracture. Though the patients were apparently healthy, they exhibited risk factors for new falls and fractures. Thus, it is important to screen patients with a previous fracture for fall and fracture risk and targeted them for preventive measures besides fracture treatment (Nordell et al., 2005).
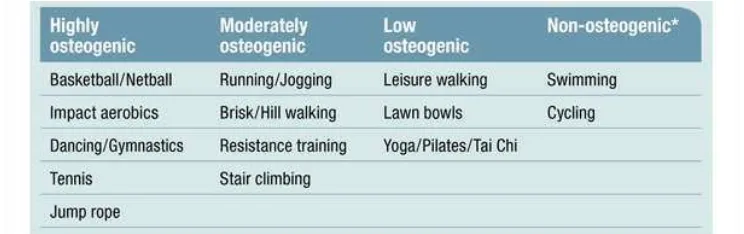
Physiotherapists should play a major role in maintaining and improving general physical functions in osteoporotic patients. Furthermore, the use of a physical activity referral scheme may improve physical activity level in patients visiting primary health care centers (Leijon et al., 2008). Figure 2.5 recommends certain exercises for low, moderate and highly osteoporotic patients in comparison with healthy people.
Figure II.6 Certain exercises recommended for osteoporotic patients 13. Exercise Intervention
a. Role of Physics and Physiology
Studies indicate that bone strength depends on the forces loaded on the bones (Frost, 2004). Given that bone deformation is the stimulus that regulates bone modeling and remodeling, force is the determining parameter. In physics, force changes movement and causes defor-mation. In common medical terminology, strength is used both for maximum voluntary muscle force and bone strength to describe the fracture load, i.e. the threshold of applied force, which is able to break a bone. Force loading of different parts of the body depends on leverage and stiffness. A helpful model to understand the mechanical concept of stiffness and force loading can easily be performed by a short self-examination. Jumping down from the height of a chair with a two legs landing on the forefeet as soft as possible generates ground reaction forces in the magnitude of 150–200% of body weight to one leg in individuals with a good neuromuscular coordination and applied in the region of distal metatarsal bones.
A stiff landing generates ground reaction forces up to 400% of body weight to one leg. The forces loaded on the legs can be calculated as quotient of kinetic energy in the moment of ground contact divided by the breaking distance (crumble zone), which is determined by muscle tension. In terms of physics, stiffness equals to force divided by distance. Thus, regulation of muscle tension determines the stiffness of the body. High stiffness means a short breaking distance equals to high force loading. To calculate the force loading of bones, the leverage has to be referred. The three fold accelerated gravitational forces of the body are applied on the distal metatarsal bones, generating a torque, which can be calculated as product of the applied force times length of the lever. The calf muscles counter this torque, acting on a 1:3 shorter lever. Thus, in one-leg jumping on the forefoot, the lower leg is loaded with forces of 12–14 fold of body weight. This example demonstrates the indispensable importance of physics in the discussion of exercise impact on bones (Kalapotharakos, 2005).
In medical articles, often quantified or even non-quantifiable terms are used to describe exercises, like high-intensity, mild, moderate, vigorous, non-strenuous, weight-bearing, brisk walking and etc., so the description of physical activity is often not sufficiently accurate to assess leverage, stiffness and force loading of the adminis-tered exercises. Referring to the impact of force loading, another parameter as rate of force development is indispensible. Referring to