World Health House Indraprastha Estate, Mahatma Gandhi Marg, New Delhi-110002, India www.searo.who.int
in the South-East Asia Region
foodborne diseases
Burden of
Globally, billions of people are at risk of foodborne diseases (FBDs) and millions fall ill from these every year. Many die as a result of consuming unsafe food. FBDs can also affect economic development through the tourism, agricultural and food export industries. The South-East Asia Region has the second highest burden of FBDs after the African Region, with more than 150 million cases and 175 000 deaths annually.
The World Health Organization has launched a comprehensive and first of its kind report to estimate the global and regional burden of FBDs. This report will support policy-makers in implementing the right strategies to prevent, detect and manage foodborne risks to improve food safety. It highlights the work of WHO's Regional Office for South-East Asia with national governments on improving surveillance of foodborne diseases and meeting unique local challenges.
Burden of foodborne diseases
© World Health Organization 2016
All rights reserved.
Requests for publications, or for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – can be obtained from SEARO Library, World Health Organization, Regional Office for South-East Asia, Indraprastha Estate, Mahatma Gandhi Marg, New Delhi 110 002, India (fax: +91 11 23370197; e-mail: searolibrary@who.int).
The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO Library Cataloguing-in-Publication data
World Health Organization, Regional Office for South-East Asia.
Burden of foodborne diseases in the South-East Asia Region.
1. Foodborne Diseases 2. Epidemiology 3. Food contamination
Acronyms ... v
Introduction: Foodborne diseases ...1
Foodborne infections ...2
Chemicals and toxins in food ...3
Food allergy ...4
Global burden of foodborne diseases ...5
Objectives ...5
Methodology ...6
Gaps and limitations ...9
Foodborne diseases in the WHO South-East Asia Region...11
Foodborne diseases in under-five children ...13
Conclusions and action points ...17
Annexes 1. Classification of foodborne diseases ...21
2 A guide to national burden of foodborne disease study ...42
3 Categorization of subgroups under WHO regions ...47
Acronyms
CA Codex Alimentarius
DALY disability-adjusted life-year
ETEC enterotoxigenic Escherichia coli
EPEC enteropathogenic Escherichia coli
FAO Food and Agriculture Organization of the United Nations
FBDs foodborne diseases
FERG Foodborne Disease Burden Epidemiology Reference Group
GEMS Global Environmental Monitoring System
HAV hepatitis A virus
IHR (2005) International Health Regulations (2005)
INFOSAN International Food Safety Authorities Network
NTS non-typhoidal Salmonella enterica
POPs persistent organic pollutants
sp., spp. species (sing. and plural)
Introduction: Foodborne diseases
Food is an essential requirement for humans but it can also be a vehicle of disease transmission if contaminated with harmful microbes (bacteria, viruses or parasites) or chemicals/toxins. Globally, billions of people are at risk of foodborne diseases (FBDs) and millions fall ill every year. Many also die as a result of consuming unsafe food.
Foodborne illnesses are mainly caused due to food contamination with harmful bacteria, viruses, parasites, toxins or chemicals. Microbial and chemical risks could be introduced at the farm level (e.g. using water contaminated by industrial waste or poultry farm waste for irrigation of crops). Similarly, such risks may emerge during processing, transportation or storage of food and food products.
While many FBDs may be self-limiting, some can be very serious and even result in death. These diseases may be more serious in children, pregnant women and those who are older or have a weakened immune system. Children who survive some of the more serious FBDs may suffer from delayed physical and mental development, impacting their quality of life permanently. Food allergy is another emerging problem. A brief description of major FBDs of public health importance is presented in Annex 1.
FBDs are more critical in developing countries due to various reasons, such as use of unsafe water for cleaning and processing of food, poor food production processes and food handling, absence of adequate food storage infrastructure, and inadequate or poorly enforced regulatory standards. The tropical climate in many countries in the Region also favours the proliferation of pests and naturally occurring toxins and increase the risk of contracting parasitic diseases including worm infestations.
Foodborne infections
When certain disease-causing microbes (bacteria, viruses or parasites) contaminate food, they can cause foodborne illness, often called “food poisoning”. Foods that are contaminated may not look, taste or smell any different from foods that are safe to eat. Salmonella, Campylobacter, Shigella and Escherichia coli (also called E. coli) are the common bacteria that cause foodborne illnesses. Salmonella is the most common cause of foodborne illnesses and meat, egg and seafood are common food sources for much illnesses. Some foodborne bacteria like Listeria monocytogenes can even grow inside the refrigerator in ready-to-eat food. Staphylococcus aureus bacteria grow in food and produce toxins that cause staphylococcal food poisoning. Viruses that commonly cause foodborne illnesses are norovirus and hepatitis A virus (HAV), which can be transmitted through contaminated water as well as contaminated surfaces.
Foodborne bacteria are often naturally present in food and under the right conditions, a single bacterium can grow into millions of bacteria in a few hours. These bacteria multiply rapidly on foods with lots of protein or carbohydrates when food temperature is between 5 °C and 60 °C, which is often known as the “food danger zone”. Therefore, most foodborne illnesses and outbreaks are reported during the summer months.
Bacteria grow and multiply on some types of food more easily than on others. The types of foods that bacteria prefer include meat, poultry, dairy products, eggs, seafood, cooked rice, prepared fruit and salads. These foods are more likely to be infected by foodborne bacteria but other foods could also be infected or cross-contaminated by them if appropriate food safety measures are not taken during preparation, storage, transportation and handling .
Chemicals and toxins in food
Food adulteration and falsification are still a problem in countries of the WHO South-East Asia Region where informal food production and distribution systems are deeply entrenched at the community level. Adulteration of food is normally observed in its most crude form where prohibited substances are either added or used to partly or wholly substitute healthy ingredients or to artificially create the impression of freshness in stale food. Adulterants may be in solid form, of chemicals, or liquid and made up of colouring substances. Poisonous colouring agents like auramine, rhodomine b, malachite green and Sudan red are applied on food items for colouring, brightness and freshness. This can damage the liver and kidneys sometimes. These agents also cause stomach cancer, asthma and bladder cancer. Colouring agents such as chrome, tartazine and erythrosine are used in spices, sauces, juices, lentils and oils, causing cancer, allergy and respiratory problems. The calcium carbide of industrial grade used for fruit ripening by unscrupulous traders may contain toxic impurities such as traces of arsenic and phosphorous, which can be quite harmful for the health and can lead to various ailments..
Dioxins are byproducts of industrial processes but could also result from natural phenomena such as volcanic eruptions and forest fires. Human exposure is primarily through food – mainly meat and dairy products, fish and shellfish. These toxins accumulate in humans, especially in body fat. Dioxins are toxic to the thyroid gland and inhibit sperm production, and prolonged exposure leads to accumulation in the body. The dioxin concentration in breast milk fat directly reflects its concentration in body fat.
Mycotoxins are a group of naturally occurring chemicals produced by certain moulds or fungi. They can grow on a variety of different crops and foodstuffs including cereals, nuts, spices and dried fruits. Mycotoxins are produced by several fungi in foodstuffs and these feed during production, storage and transportation, often under warm and humid conditions. Mycotoxins of most concern from a food safety perspective include the aflatoxins, ochratoxin A, fumonisins, trichothecenes and zearalenone. Aflatoxins are most commonly found in maize and peanuts, and feed as contaminants, and these can also be found in the milk of animals that are fed aflatoxin-contaminated feed in the form of aflatoxin M1.
these toxins are not destroyed by normal cooking or processing. Naturally occurring cyanogenic glycosides are found in raw or unprocessed cassava (Manihot esculenta), which can cause nerve damage or death if consumed in quantity.
Food poisoning from the consumption of poisonous wild mushrooms has been reported frequently during the monsoon season in countries of the South-East Asia Region. In some episodes, whole families have lost their lives due to consumption of poisonous wild mushrooms. The majority of fatal mushroom poisoning occurs due to ingestion of Amanita phalloides – the death cap – due to its high content of Amatoxin, a potent cytotoxin. Fatal poisoning is usually associated with delayed onset of symptoms, which are very severe and have a toxic effect on the liver, kidney and nervous system. Unfortunately, cases remain undiagnosed, under-reported and unpublished as these happen in rural communities.
Food allergy
Food allergy is an abnormal response to a food triggered by the body’s immune system. Individuals with food allergies develop symptoms by eating foods that for the vast majority of the population are part of a healthy diet. Food allergy is a growing problem. The prevalence of food allergies in the general population has been roughly estimated to be around 1–3% in adults and 4–6% in children.
Peanut or groundnut allergy occurs early in life (<five years of age) and is believed to be lifelong. Egg and milk allergies are most common food allergies among infants but are often outgrown. More than 70 foods have been described as causing food allergies. Several studies indicate that 75% of allergic reactions among children are due to a limited number of foods, namely egg, peanuts, milk, fish and nuts. Fruits, vegetables, nuts and peanuts are responsible for most allergic reactions among adults.
Global burden of foodborne
diseases
Foodborne diseases (FBDs) are an important cause of illness and death around the world. However, the extent and cost of unsafe food, and especially the burden due to chemical and parasitic contaminants in food, is still not fully known. Epidemiological data on FBDs and laboratory capacity to detect the cause of FBDs are not available widely, particularly in the developing world. As a result, many foodborne outbreaks often go unrecognized, unreported or uninvestigated.
A major problem in addressing food safety concerns is the lack of accurate data/ information regarding the extent and cost of FBDs. Lack of comprehensive data and information on the burden of FBDs makes it challenging for policy-makers to set public health priorities and allocate resources. Therefore, the World Health Organization (WHO) has taken an initiative to carry out an estimation of the global burden of FBDs and generation of evidence-based data and information that will enable policy-makers to prioritize and allocate resources for food safety.
Objectives
WHO Department of Food Safety, Zoonoses and Foodborne Diseases together with its partners launched the initiative to estimate the global burden of FBDs in 2006. The primary goal of the initiative is to enable policy-makers and other stakeholders to set appropriate, evidence-based priorities in the area of food safety. After an initial consultation, WHO established a Foodborne Disease Burden Epidemiology Reference Group (FERG) in 2007 to lead the initiative. These objectives were to:
• provide estimates on the global burden of FBDs according to age, sex and regions for a defined list of causative agents of microbial, parasitic and chemical origin;
• increase awareness and commitment among Member States for the
implementation of food safety standards; and
• encourage Member States to use burden of foodborne disease estimates for cost-effective analyses of prevention, intervention and control measures.
Methodology
These objectives were addressed through the establishment of six task forces, each pursuing on groups of hazards or select aspects of the methodology. Together with the WHO Secretariat, these task forces commissioned systematic reviews and other studies to provide the data from which burden estimates could be calculated.
According to WHO, it was important to provide estimates of foodborne disease at as localized a level as possible because not all foodborne hazards affect every country equally. On account of gaps in the information available from certain countries (especially developing countries), subregional estimates are considered more robust as they build on the data from several countries in each Region.
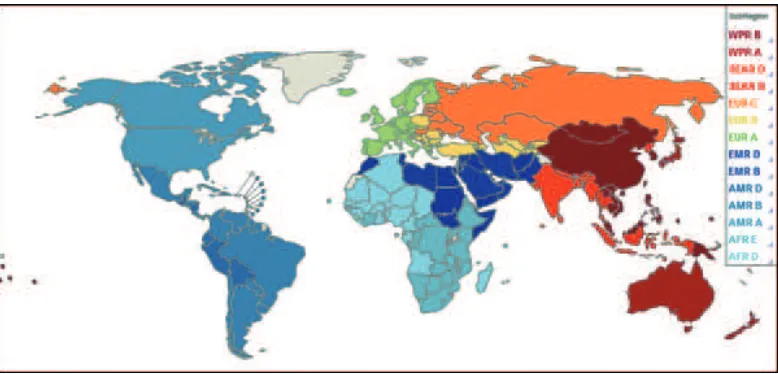
The six WHO regions were divided into 14 subregions as shown in Figure 1, based on five categories considering child and adult mortality rates, as follows:
• Category A: very low child and adult mortality
• Category B: low child mortality and very low adult mortality • Category C: low child mortality and high adult mortality • Category D: high child and adult mortality
Figure 1: Categorization of subgroups under WHO regions for estimation of global burden of foodborne diseases
Source: FERG Report (2015)
The list of countries that were divided into 14 subregions is available in Annex 3. A country can obtain national estimates by referring to estimates for the subregion to which it belong.
In addition to providing global and regional estimates, the initiative also sought to promote actions at a national level. This involved capacity-building through national foodborne disease burden studies, and encouraging the use of information on the burden of disease in setting evidence-informed policies. A suite of tools and resources were created to facilitate national studies on the burden of foodborne diseases and pilot studies were conducted in four countries (Albania, Japan, Thailand and Uganda).
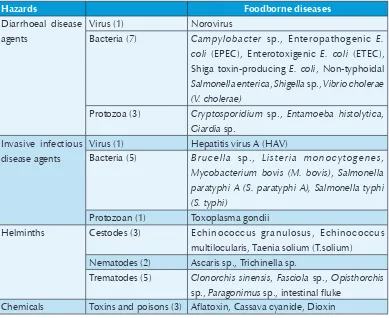
Table 1: Hazards and foodborne diseases considered in studies
Hazards Foodborne diseases
Diarrhoeal disease agents
Virus (1) Norovirus
Bacteria (7) Campylobacter sp., Enteropathogenic E. coli (EPEC), Enterotoxigenic E. coli (ETEC), Shiga toxin-producing E. coli, Non-typhoidal
Salmonella enterica, Shigella sp., Vibrio cholerae (V. cholerae)
Protozoa (3) Cryptosporidium sp., Entamoeba histolytica,
Giardia sp. Invasive infectious
disease agents
Virus (1) Hepatitis virus A (HAV)
Bacteria (5) Brucella sp., Listeria monocytogenes,
Mycobacterium bovis (M. bovis), Salmonella paratyphi A (S. paratyphi A), Salmonella typhi (S. typhi)
Protozoan (1) Toxoplasma gondii
Helminths Cestodes (3) Echinococcus granulosus, Echinococcus
multilocularis, Taenia solium (T.solium) Nematodes (2) Ascaris sp., Trichinella sp.
Trematodes (5) Clonorchis sinensis, Fasciola sp., Opisthorchis
sp., Paragonimus sp., intestinal fluke Chemicals Toxins and poisons (3) Aflatoxin, Cassava cyanide, Dioxin
Together, the 31 hazards caused an estimated 600 million foodborne illnesses, 420 000 deaths and 33 million disability-adjusted life-years (DALY) in 2010. DALY is a measure of the overall disease burden expressed as the number of years lost due to ill-health, disability or early death.
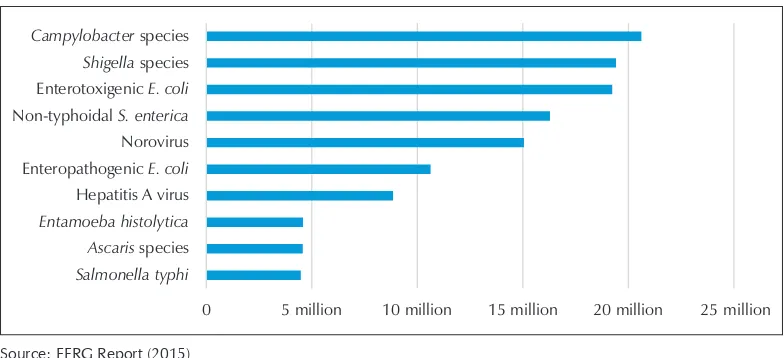
Diarrhoeal diseases are the leading cause of foodborne disease illnesses – particularly norovirus and Campylobacter spp.. It is estimated that one in 10 people in the world fall ill every year due to eating contaminated food, as shown in Figure 2. Foodborne diarrhoeal disease agents caused 230 000 deaths, particularly non-typhoidal
S. enterica (NTS), which causes diarrhoeal and invasive disease. Other major causes of
Figure 2: Burden of foodborne illness
1 in 10 people in the world fall ill every year due to eating contaminated food
Source: FERG Report (2015)
The global burden of FBDs is considerable with marked regional variations. The burden of FBDs is borne by individuals of all ages, but particularly children under five years of age and persons living in low-income regions of the world. Nearly 40% of the foodborne disease burden was among children under five years of age with 18 million DALY lost due to foodborne diarrhoeal disease agents, particularly NTS and EPEC. Other foodborne hazards with a substantial contribution to the global burden included S.typhi and T. solium.
Gaps and limitations
Estimates are based on the best available data at the time of reporting. Identified data gaps were filled using imputation, assumptions and other methods.
Data gaps were a major hurdle to making estimates of the foodborne disease burden in these national studies. The global and regional estimates provided by FERG offer an interim solution until improved surveillance and laboratory capacity is developed.
It is likely that the true number of illnesses and deaths resulting from FBDs worldwide is even higher because:
• many cases of food poisoning go unrecognized and untreated,
• there are gaps in the collection and reporting of data (especially in developing countries) on the burden of FBDs,
• there are other causes beyond the 31 hazards included in this report, especially in the chemical domain,
WHO is focusing its efforts on supporting national policy-makers and governments in improving surveillance of FBDs to obtain a clearer picture of the unique local challenges and implement the right strategies to prevent, detect and manage foodborne risks.
The report prepared by the WHO Foodborne Disease Burden Epidemiology Reference Group provides the first estimates of global foodborne disease in terms of incidence, mortality and disease burden in the form of DALY. This report is the outcome of 10 years of monumental work by WHO and its donors and partners as well as a number of individuals contributing to this initiative from around the world. The report is an essential part of WHO’s efforts to facilitate global prevention, detection and response to public health threats associated with unsafe food. It is a continuation of WHO activities dedicated to driving food safety as highlighted during World Health Day 2015.
Foodborne diseases in the WHO
South-East Asia Region
Home to a quarter of the world’s population, the WHO South-East Asia Region has the second highest burden of FBDs per population among WHO regions. It has more than half of the global infections and deaths due to typhoid fever or hepatitis A.
Based on data (2010) from the FERG report, the annual burden of FBDs in the South-East Asia Region includes more than:
• 150 million illnesses
• 175 000 deaths
• 12 million DALYs.
Figure 3: Top 10 causes of foodborne illnesses in the WHO South-East Asia Region
0 5 million 10 million 15 million 20 million 25 million
Salmonella typhi Ascaris species Entamoeba histolytica Hepatitis A virus Enteropathogenic E. coli Norovirus Non-typhoidal S. enterica Enterotoxigenic E. coli Shigella species Campylobacter species
As shown in Figure 3, Campylobacter sp. was the leading cause of foodborne illness with an estimated more than 20 million cases every year in the Region. This was followed
by Shigella sp. and enterotoxigenic Escherichia coli with more than 19 million cases
each. At the fourth spot, NTS was estimated to cause more than 16 million infections.
In aggregate terms, E. coli and S. spp. were the leading causes of foodborne illnesses. Norovirus and hepatitis A virus also caused significant diseases in the Region. Amoebiasis caused by Entamoeba histolytica and worm infestation by Ascaris sp. were the leading parasitic causes of illness due to contaminated food.
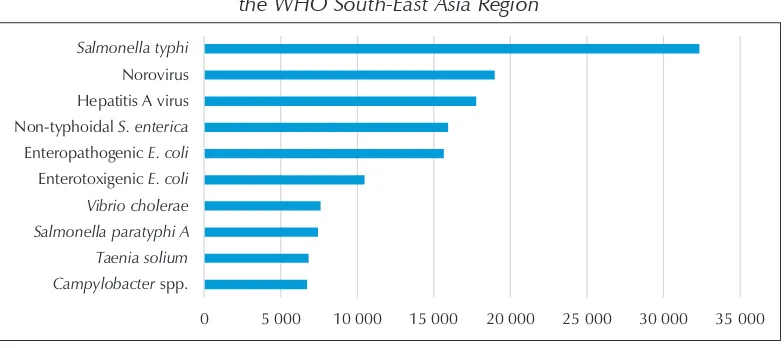
Figure 4: Top 10 causes of deaths due to foodborne illnesses in the WHO South-East Asia Region
0 5 000 10 000 15 000 20 000 25 000 30 000 35 000
Campylobacter spp. Taenia solium Salmonella paratyphi A Vibrio cholerae Enterotoxigenic E. coli Enteropathogenic E. coli Non-typhoidal S. enterica Hepatitis A virus Norovirus Salmonella typhi
Source: FERG Report (2015)
As shown in Figure 4, the leading cause of death due to foodborne diseases in the Region was S. typhi (more than 32 000 deaths), followed by norovirus (nearly 19 000 deaths) and hepatitis A virus (nearly 18 000 deaths) respectively. NTS at fourth position was responsible for nearly 16 000 deaths in the Region. EPEC and ETEC caused more than 15 000 and 10 000 deaths respectively. Cholera (caused by V.cholerae) and paratyphoid fever (caused by S.paratyphi A) were estimated to have caused more than 7600 and nearly 7500 deaths respectively.
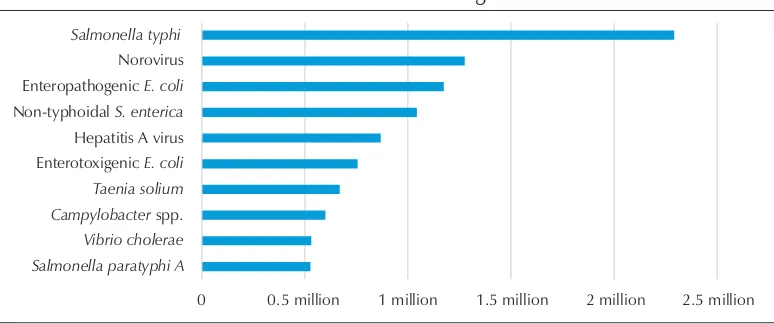
Going by the estimated burden of FBDs in terms of DALYs in the Region as shown in Figure 5, S. typhi is the leading cause of ill-health, disability or early death and leads to the highest number of DALYs (nearly 2.3 million). S. paratyphi A that causes a similar illness was also estimated to be responsible for more than half a million DALYs every year.
Figure 5: Top 10 causes of DALYs due to foodborne illnesses in the WHO South-East Asia Region
0 0.5 million 1 million 1.5 million 2 million 2.5 million Salmonella paratyphi A
Vibrio cholerae Campylobacter spp. Taenia solium Enterotoxigenic E. coli Hepatitis A virus Non-typhoidal S. enterica Enteropathogenic E. coli Norovirus Salmonella typhi
Source: FERG Report (2015)
Viral causes of foodborne diseases – norovirus and hepatitis A virus were estimated to be responsible for nearly 1.3 million and 870 000 DALYs every year.
Interestingly, non-typhoidal S. enterica continued to occupy the fourth position among the top 10 causes of DALYs and was estimated to be responsible for more than a million DALYs. EPEC and ETEC were responsible for nearly 1.2 million and 760 000 DALYs respectively.
The pork tapeworm was responsible for nearly 670 000 DALY and Campylobacter sp. and cholera led to 600 000 and 530 000 DALY respectively.
Foodborne diseases in under-five children
Figure 6: Under-five children suffering from diarrhoea in the WHO South-East Asia Region
3 in 10 children under five years of age suffer from diarrhoea
Source: FERG Report (2015)
The Region contributes to one third of the global deaths due to diarrhoea in children under five years of age that could be prevented.
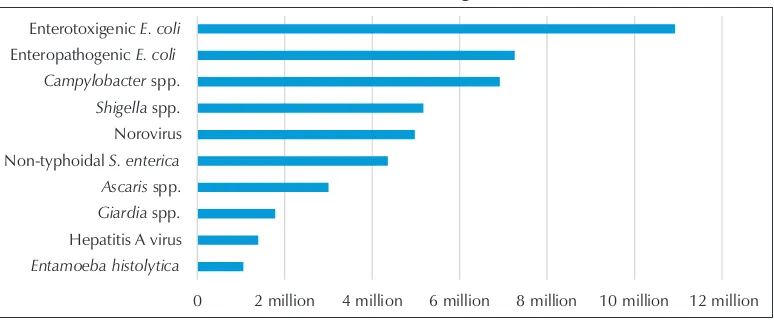
Figure 7: Top 10 causes of foodborne illnesses in children under five years of age in the South-East Asia Region
0 2 million 4 million 6 million 8 million 10 million 12 million Entamoeba histolytica
Hepatitis A virus Giardia spp. Ascaris spp. Non-typhoidal S. enterica Norovirus Shigella spp. Campylobacter spp. Enteropathogenic E. coli
Enterotoxigenic E. coli
Source: FERG Report (2015)
In children under five years of age (as shown in Figure 7), the top three causes of foodborne illnesses were ETEC (nearly 11 million cases), EPEC (nearly 7.3 million cases)
and Campylobacter sp. (nearly 7 million cases).
Shigella sp., norovirus and NTS caused 5.2, 5 and 4.4 million illnesses respectively and hepatitis A virus caused nearly 1.4 million cases in children under five years of age.
Figure 8: Top 10 causes of deaths due to foodborne illnesses in children under five years of age in the South-East Asia Region
0 1 000 2 000 3 000 4 000 5 000 6 000 7 000 8 000 Taenia solium
Salmonella paratyphi A Shigella spp. Hepatitis A virus Campylobacter spp. Enterotoxigenic E. coli Non-typhoidal S. enterica Norovirus Salmonella typhi Enteropathogenic E. coli
Source: FERG report (2015)
As shown in Figure 8, the top three causes of death due to FBDs in children under five years of age in the Region were EPEC (nearly 7400), S.typhi (6600) and norovirus (4000).
Other major causes of death in children under five years of age were estimated to be NTS (3663 deaths), ETEC (3532 deaths), Campylobacter spp. (3322 deaths) and hepatitis A virus (2805 deaths).
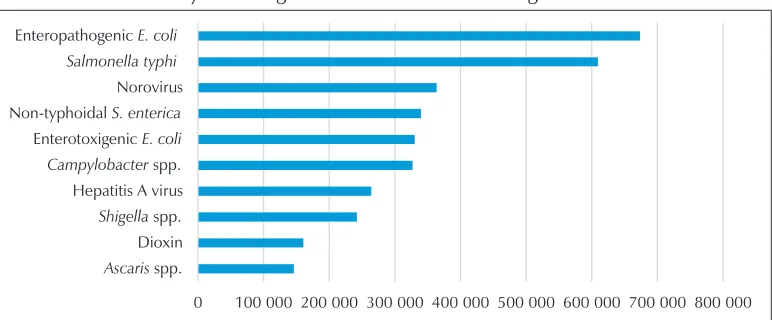
Figure 9: Top 10 causes of DALYs due to foodborne illnesses in children under five years of age in the South-East Asia Region
0 100 000 200 000 300 000 400 000 500 000 600 000 700 000 800 000 Ascaris spp.
Dioxin Shigella spp. Hepatitis A virus Campylobacter spp. Enterotoxigenic E. coli Non-typhoidal S. enterica Norovirus Salmonella typhi Enteropathogenic E. coli
In terms of DALY due to FBDs in children under five years of age (as shown in Figure 9), the leading cause was EPEC (nearly 674 000 DALY), followed by S. typhi (610 000 DALY) and norovirus (nearly 364 000 DALY).
Other causes of DALYs include NTS, ETEC, Campylobacter sp. hepatitis A virus,
Shigella sp. and dioxin. Interestingly, dioxin was estimated to have a significant impact
Conclusions and action points
The most comprehensive report to date on the impact of contaminated food on health and well-being is titled ‘Estimates of the Global Burden of Foodborne Diseases’. These estimates are the result of a decade of work, including inputs from more than 100 experts from around the world. Based on what we know now, it is apparent that the global burden of FBDs is considerable. The FERG report highlights the global threat posed by FBDs in the context of globalization of the food trade. Unsafe food endangers everyone and billions of people are at risk.
The global burden of FBDs is considerable with marked regional variations. The burden of FBDs is borne by individuals of all ages, and particularly children under five years of age and persons living in low-income regions of the world. These estimates are conservative; further studies are needed to address the data gaps and limitations of this study. The considerable difference in the burden of foodborne disease between low- and high-income regions suggests that a major proportion of the current burden is avoidable and that control methods do exist.
The report highlights that action to reduce illnesses and deaths from FBDs must be tailored according to regional and national needs as the types of contaminants and reasons for their prevalence differ across the world. The report will support policy-makers in implementing the right strategies to prevent, detect and manage foodborne risks to improve food safety.
economic growth, full and productive employment and decent work for all) will also be cited through promoting the safety of food supply domestically and internationally.
The report also reinforces the need for governments, the food industry and individuals to do more to make food safe and prevent foodborne illnesses and intoxications. Safe drinking water, good hygienic practices and improved sanitation are keys for preventing foodborne illnesses and intoxications.
The majority of FBDs and deaths are preventable. Food safety is a public health priority and governments should develop policies and regulatory frameworks to establish and implement effective food safety systems. Food safety systems should ensure that food producers and suppliers along the whole food chain operate responsibly and supply safe food to consumers.
Food safety is a shared responsibility. All food operators and consumers should understand the roles they must play to protect their health and that of the wider community. All stakeholders can contribute to improvements in food safety throughout the food chain by incorporating these estimates into policy development at the national and international levels.
Think globally, act locally: while there is no single, global solution to the problem of FBDs, a strengthened food safety system in one country will positively impact the safety of food in other countries. There is need for coordinated, cross-border action across the entire food supply chain.
Coordinated action at the global, regional and national levels is needed to address risks of FBDs and ensure food safety. Education and training are needed on prevention of FBDs among food producers, suppliers, handlers and the general public, including women and school children.
Key action points towards ensuring food safety in the Region include the conduct of national studies on the burden of FBDs, strengthening of laboratory capacity to be able to detect FBDs, and strengthening the surveillance of FBDs, including the collation of local data to validate regional estimates and translation of estimates of FBDs into food safety policy.
2015 clearly illustrates that most Member States have limited capacity for surveillance, assessment and management of priority food safety events. Therefore, the WHO Regional Office for South-East Asia is providing technical support to Member States to evaluate existing national foodborne disease surveillance systems, including risk assessment and the management of food safety events, and to identify action plans to improve surveillance, assessment and management of priority FBDs and food safety events.
WHO is working with governments and partners to reduce the level of food contamination throughout different stages of the food-chain. These stages include the point of final consumption to the levels at which the exposure to pathogens and contaminants does not pose significant risks for human health.
WHO promotes the use of international platforms such as the joint WHO-FAO (Food and Agriculture Organization of the United Nations) International Food Safety Authorities Network (INFOSAN) to ensure effective and rapid communication during food safety emergencies. WHO also works closely with other international organizations to ensure food safety along the entire food-chain, from production to consumption, in line with the Codex Alimentarius (CA). CA is a collection of international food standards, guidelines and codes of practice covering all main foods and steps in the food supply chain.
FBDs are preventable. WHO is promoting the important role that everyone can play to promote food safety through systematic disease prevention and awareness programmes. WHO’s Five Keys to Safer Food explains the basic principles that each individual should know all over the world to prevent FBDs:
(1) Keep clean
– thoroughly wash raw fruits and vegetables with tap water. – keep clean hands, kitchen and chopping board all the time.
(2) Separate raw and cooked food
– do not mix raw food and ready-to-eat food. – do not mix raw meat, fish and raw vegetables.
(3) Cook thoroughly
(4) Keep food at safe temperatures
– refrigerate cooked food within two hours of preparation.
– never defrost food at room temperature; defrost frozen food in the refrigerator, cold water or the microwave.
(5) Use safe water and raw materials
– use safe drinking water for food preparation.
B
Classification of foodborne diseases
1Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
1. Initial or major signs and symptoms of the upper digestive tracts (nausea, vomiting) 1.1 Incubation period tends to be less than 1 hour
Fungal agents
Poisoning by mushrooms of the group that causes gastrointestinal irritation
Possibly resin-type substances found in some types of mushrooms
From 30 minutes to 2 hours
Nausea, vomiting, retching, diarrhoea, abdominal pains
Many varieties of wild mushrooms
Vomit Ingestion of unknown toxic varieties of mushrooms, through confusion with other edible varieties Chemical agents
Antimony poisoning Antimony in enamelled iron utensils
From a few minutes to 1 hour
Vomiting, abdominal pains, diarrhoea
Very acid food and beverages
Vomit, stool and urine
Use of utensils that contain antimony, storage of very acid food in enamelled iron utensils
Cadmium poisoning Cadmium in plated utensils
From 15 to 30 minutes
Nausea, vomiting, abdominal pains, diarrhoea, shock
Very acid foods and drinks, candies and other cake decorations
Vomit, stool, urine and blood
Use of utensils that contain cadmium, storage of very acid food in containers that contain cadmium, ingestion of foods that contain cadmium
2
2
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Copper poisoning Copper in pipes and utensils
From a few minutes to a few hours
Metallic taste, nausea, vomiting (green vomit), abdominal pains, diarrhoea
Very acid food and beverages
Vomit, gastric lavage, urine and blood
Storage of very acid food in copper utensils or use of copper tubing in serving very acid beverages, defective valves on devices to prevent reflux (in dispensers) Fluoride poisoning
(fluorosis)
Sodium fluoride in insecticides
From a few minutes to 2 hours
Salty or soapy taste, numbness in the mouth, vomiting, diarrhoea, abdominal pains, pallour, cyanosis, dilated pupils, spasms, collapse, shock
Any accidentally contaminated food, particularly dry food such as powdered milk, flour, baking powder and cake mixes
Vomit and gastric lavages
Storage of insecticides in the same place as food, confusion of pesticides with powdered foods
Lead poisoning Lead contained in earthenware pots, pesticides, paints, plaster and putty
30 minutes or more
Metallic taste, burning in the mouth, abdominal pains, milky vomit, black stool or presence of blood, bad breath, shock, blue line at the edge of gums ("lead line")
Very acid food and beverages stored in vessels containing lead, any accidentally contaminated food
Vomit, gastric lavages, stool, blood and urine
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
1.2 Incubation period of 1 to 6 hours Bacterial agents
Bacillus cereus gastroenteritis (type emetic)
Exoenterotoxin of B. cereus
From ½ to 5 hours Nausea, vomiting, occasionally diarrhoea
Cooked or fried rice and plates of rice with meat
Vomit and stool Storage of cooked food at warm temperatures, food cooked in large containers, food prepared several hours before serving
Staphylococcal food poisoning
Exoenterotoxins A, B, C, D and E of Staphylococcus aureus.
Staphylococci from the nose, skin, and lesions of infected people and animals, and infected udders of cows
From 1 to 8 hours, average of 2 to 4 hours
Nausea, vomiting, retching, abdominal pains, diarrhoea, prostration
Ham, beef or poultry products, cream-filled pastries, food mixes and leftover food
Patient: vomit, stool, rectal swab. Carrier: nasal swabs, swabs from lesion, and rectal swabs
Inadequate refrigeration, handler touched cooked food, preparation of food several hours before serving, handlers with purulent infections, food kept at warm temperatures (bacterial incubation), fermentation of foods abnormally low in acids
Chemical agents 3
Nitrite poisoning Nitrites or nitrates used as compounds to cure meat, or water from shallow wells
From 1 to 2 hours Nausea, vomiting, cyanosis, headache, dizziness,
weakness, loss of consciousness, chocolate-coloured blood
Cured meats, any accidentally contaminated food and exposure to excessive nitrification
Blood Use of excessive quantities of nitrites or nitrates to cure food or conceal spoilage, confusion of nitrites with common salt, and other condiments, inadequate refrigeration, excessive nitrification in fertilized food
2
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Diarrheal shellfish poisoning (DSP)
Okadaico acid and other toxins produced by dinoflagellates of the Dinophysis spp.
From 1/2 to 12 hours, usually 4 hours
Diarrhoea, nausea, abdominal pains
Mussels, clams, oysters
Gastric rinse Shellfish caught in water with high concentration of Dynophysis spp.
1.3 Incubation period usually from 7 to 12 hours
Fungal agents Poisoning caused by mushrooms of the cyclopeptide and Giromitra groups
Cyclopeptides and gyromitrine found in certain mushrooms
From 6 to 24 hours
Abdominal pains, feeling of fullness, vomiting, prolonged diarrhoea, loss of strength, thirst, muscle cramps, rapid and weak pulse, collapse, jaundice, somnolence, dilated pupils, coma, death
Amanita phalloides, A. verna, Galerina autumnalis. Esculenta giromitra (false colmenilla) and similar spp. of mushrooms
Urine, blood, vomit
Ingestion of certain spp. of Amanita, Galerina and Giromitra mushrooms, ingestion of unknown varieties of mushrooms, confusion of toxic mushrooms with edible varieties
Viral agent
Norovirus (Norwalk-like viruses)
Norovirus viruses are relatively stable in the environment and can survive freezing and heating to 60°C
12 to 48 hours Vomiting, watery, non-bloody diarrhoea with abdominal cramps, low-grade fever, myalgia, malaise,
Contaminated food or water
Stool specimens taken within 48 to 72 hours after onset of symptoms
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Small round viruses, productive of gastroenteritis
Includes adenovirus, coronavirus, rotavirus, parvovirus, and astrovirus
½ to 3 days, usually 36 hours
Nausea, vomiting, diarrhoea, abdominal pain, myalgia, headache, light fever. Duration: 36 hours
Shellfish from contaminated water
Stool, blood in acute and convalescent phases
Infected people who touch food ready for consumption, harvest of shellfish from contaminated waters, improper disposal of wastes, use of contaminated water
2. Manifestation of pharyngitis and respiratory signs and symptoms
2.1 Incubation period less than 1 hour Chemical agents
Calcium chloride poisoning
Freezing mixtures of calcium chloride for freezing desserts
A few minutes Burning in the tongue, mouth, and throat, vomiting
Frozen desserts Vomit Contamination of popsicles during freezing, permitting the introduction of calcium chloride in the syrup
Sodium hydroxide poisoning
Sodium hydroxide (caustic soda) in compounds used to wash bottles, detergent, drain cleaners, hair-relaxants
A few minutes Burning of the lips, mouth and throat; vomiting, abdominal pains, diarrhoea
Bottled beverages Vomit Improper rinsing of bottles washed with caustic substances
2.2 Incubation period from 18 to 72 hours Bacterial agents
Infections by beta-haemolytic streptococci
Streptococcus pyogenes of the throat and lesions of infected people
From 1 to 3 days Pharyngitis, fever, nausea, vomiting, rhinorrhoea, sometimes rash
Raw milk, foods containing egg
Pharyngeal swabs, vomit
2
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
2.3 Incubation period from 3 to 30 days
Rickettsial agent
Q Fever Coxiella burnetii 2-3 weeks (3-30 days)
Chills, headache, malaise, myalgia and sweets
Raw milk from infected cattle or goats, direct contact with contaminated materials
Serum Consumption of raw milk, direct contact with aborted materials, inadequate disinfection and disposal of aborted materials
3. Initial or major signs and symptoms of the lower digestive tract (abdominal pains, diarrhoea)
3.1 Incubation period usually from 7 to 12 hours
Bacterial agents
Gastroenteritis by Bacillus cereus (diarrheal type)
Exoenterotoxin of B. cereus, organisms in the soil
From 8 to 16 hours (average of 12 hours)
Nausea, abdominal pains, diarrhoea
Foods made from grains, rice, custard, sauces, meatballs, sausages, cooked vegetables, dehydrated or reconstituted products
Stool Inadequate refrigeration, storage of food at warm temperatures (bacterial incubation), preparation of food several hours before serving, improper reheating of leftovers
Gastroenteritis caused by Clostridium perfringens
Endoenterotoxin formed during the sporulation of C. perfringens in the intestines, the
From 8 to 22 hours (average of 10 hours)
Abdominal pains, diarrhoea
Cooked beef or poultry, broths, sauces and soups
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
3.2 Incubation period usually from 18 to 72 hours
Bacterial agents
Diarrheal diseases caused by Aeromonas
Aeromonas hydrophila
1 to 2 days Watery diarrhoea, abdominal pain, nausea, headache
Fish, shellfish, snails, water
Stool Contamination of food in sea or surface water
Campylobacter Infection
Campylobacter jejuni
2 to 7 days usually between 3 and 5
Abdominal pains, diarrhoea (frequently with mucus and blood), headache, myalgia, fever, anorexia, nausea, vomiting. Sequellae: Guillian-Barre syndrome
Raw milk, beef liver, raw clams
Stool or rectal swabs, blood
Drinking raw milk, handling raw products, eating raw or undercooked poultry, inadequate cooking or pasteurization, cross-contamination with raw meat
Cholera Endoenterotoxin of V. cholerae classical and El Tor biotypes, from faeces of infected persons
From 1 to 3 days Severe, watery diarrhoea (rice water stools), vomiting, abdominal pains, dehydration, thirst, collapse, loss of skin tone, shrivelled fingers, sunken eyes
Raw fish and shellfish, food washed or prepared with contaminated water, water
2
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Gastroenteritis caused by cholera like vibrio
Cholera like vibrio From 5 to 48 hours, average from 10 to 24 hours
Abdominal pains, diarrhoea, nausea, vomiting, fever, chills, headache, myalgia
Various foods, water
Stool, rectal swabs
Infected handlers who touch food, insufficient cooling, incomplete cooking, improper cleaning and disinfection of equipment
Diarrhoeal diseases caused by Enterohaemorrhagic usually 2 to 5 days
Watery diarrhoea followed by bloody diarrhoea, severe abdominal pain, blood in the urine. Sequelae: Haemolytic uremic syndrome (HUS)
Hamburger, raw milk, sausages, yogurt, lettuce, water
Stool, rectal swabs
Hamburger made from meat of infected animals, consumption of raw meat and milk, inadequate cooking, cross-contamination, infected people touching food ready for consumption, improper desiccation and fermentation of meats
Diarrhoea caused by Enteroinvasive Escherichia coli
Strains of Enteroinvasive E. coli
½ to 3 days Severe abdominal pain, fever, watery diarrhoea, (usually with mucus and blood present) tenesmus
Salads and other food that are not subsequently treated, water
Stool, rectal swabs
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Diarrhoea caused by ETEC
Strains of ETEC ½ to 3 days Profuse watery diarrhoea (without mucus or blood) abdominal pain, vomiting, prostration, dehydration, light fever
Salads and other food that are not subsequently thermally treated, fresh cheeses, water
Stool, rectal swabs
Inadequate cooking, infected people touching food ready for consumption, not washing hands after defecation, storage of food at room temperature, keeping food in the refrigerator in large containers, preparing food several hours before serving, improper reheating of food, use of raw milk in making cheese
Enteritis by Plesiomonas Pleisomonas shigeloides
1 to 2 days Diarrhoea with mucus and blood in the stool
Water Stool, rectal swabs
Inadequate cooking
Salmonellosis Various serotypes of Salmonella from faeces of infected people and animals
From 6 to 72 hours, average from 18 to 36 hours
Abdominal pains, diarrhoea, chills, fever, nausea, vomiting, malaise
Beef and poultry and their by-products, egg products, other foods contaminated with salmonellae
Stool, rectal swabs
3
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Shigellosis Shigella flexneri, S. dysenteriae, S. sonnei and S. boydii
From ½ to 7 days, usually from 1 to 3 days
Abdominal pains, diarrhoea, mucoid faeces with blood present, fever
Any food ready for consumption that becomes contaminated, frequently salads, water
Stool, rectal swabs
Infected handlers touching the food, inadequate refrigeration, improper cooking and reheating
Gastroenteritis caused by V. parahaemolyticus
V. parahaemolyticus from sea water or marine products
From 2 to 48 hours, average 12 hours
Abdominal pains, diarrhoea, nausea, vomiting, fever, chills, headache
Raw or
contaminated sea food, shellfish
Stool, rectal swabs
Inadequate cooking, inadequate refrigeration, cross-contamination, improper cleaning of equipment, use of sea water in preparing food
Diarrhoea caused by yersiniosis
Yersinia enterocolitica
1 to 7 days Abdominal pains (can simulate appendicitis), light fever, headache, discomfort, anorexia, nausea, vomiting
Raw milk, water Stool, rectal swabs
Inadequate cooking or pasteurization, cross-contamination, contaminated ingredients or water
Viral agents
Viral gastroenteritis Enteric viruses (echovirus, coxsackievirus, reovirus, adenovirus)
From 3 to 5 days Diarrhoea, fever, vomiting, abdominal pains, sometimes respiratory symptoms
Food ready for consumption
Stool Poor personal hygiene, infected workers touching food, improper cooking and reheating
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Amoebic dysentery (amoebiasis)
Entamoeba histolytica
From a few days to several months usually between 2 and 4 weeks
Abdominal pains, constipation or diarrhoea with blood and mucus
Vegetables and raw fruits
Stool Poor personal hygiene, infected handlers touching the food, improper cooking and reheating
Giardiasis Giardia lamblia from faeces of infected people
From 1 to 6 weeks Abdominal pains, diarrhoea with mucus, fatty stools
Raw fruits and vegetables, water
Stool Poor personal hygiene, infected handlers touching food, improper cooking, improper waste water disposal
Cryptosporidiosis Cryptosporidium parvum
1 to 12 days, usually 7 days
Profuse watery diarrhoea, abdominal pain, anorexia, vomiting, light fever
Apple cider, water Stool, intestinal biopsy
Improper disposal of animal wastes, contamination from the animal environment, inadequate filtering of water
Hydatidosis (unilocular or multilocular)
Echinococcus granulosus, Echinococcus multilocularis
Months to years Abdominal pain, abnormal abdominal tenderness, hepatomegaly with an abdominal mass, jaundice, fever
Food or water contaminated with faeces of infected dog, fox
Biopsy or serum Consumption of raw vegetables or water contaminated with faeces of infected dog or fox
Liverfluke (Fascioliasis) Fasciola hepatica From 4 to 6 weeks Dyspepsia, fever, right upper quadrant pain, anorexia, hepatomegaly, splenomegaly, ascites, urticaria, respiratory symptoms, and jaundice
Aquatic plants or plants with high moisture content
Stool, tissue biopsy
3
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Opisthorchiasis O. viverrine, O. felineus
From 4 to 5 weeks Flatulence, fatigue, dyspepsia, right upper quadrant abdominal pain, anorexia, and mild hepatomegaly
raw or
undercooked fish
Stool Consuming raw or undercooked fish and improper sanitary disposal of faeces facilitate infestation of fish in ponds
Intestinal fluke (Fasciolopsis)
Fasciolopsis buksi, Echinostoma
6–8 weeks Diarrhoea, constipation, abdominal pain, dizziness, and headache, sometimes vomiting, fever, nausea, and allergic reactions such as oedema of the face
Raw or undercooked aquatic plants
Stool Consuming raw aquatic plants, faecal contamination (from humans or pigs) of water where aquatic plants are grown
Lung fluke (Paragonimiasis)
Paragonimus westermani
2–15 days Cough, fever, bloody sputum, loss of appetite, chest pain, and headache Chronic stage: productive cough with brownish sputum, chest pain, and night sweats
Raw or
undercooked crab or crayfish
Sputum, stool Crab or crayfish consumed raw or prepared only in vinegar, brine, or wine without cooking
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Taeniasis due to Taenia saginata (beef tapeworm)
T. saginata from meat from meat of infected cattle
From 8 to 14 weeks
General malaise, hunger, weight loss, abdominal pains
Raw or
undercooked meat
Stool Failure to inspect meat, improper cooking, improper wastewater disposal, pasture contaminated by waste water
Anisakiasis Anisakis pseudoterranova
From 4 to 6 weeks Stomach pain, nausea, vomiting, abdominal pain
Rock fish, herring, cod, salmon, squid, sushi
Stool Ingestion of raw or undercooked fish
Diphyllobotriasis (fish tapeworm infection)
Diphyllobothrium latum from flesh of infected fish
From 3 to 6 weeks Undefined gastrointestinal discomfort, anaemia may occur
Raw or
undercooked fresh water fish
Stool Inadequate cooking, improper wastewater disposal, lakes contaminated by waste water
Sparganosis Spirometra spp. painful oedema, seizures, hemiparesis, and headaches
Contaminated water, consuming raw flesh of frog or snake
Biopsy Drinking water contaminated with infected copepods or consuming raw or under-cooked flesh of frog or snake
4. Manifestation of neurological signs and symptoms (visual disorders, tingling, paralysis)
4.1 Incubation period tends to be less than 1 hour
Fungal agents Mushroom poisoning from the group that contains ibotenic acid
Ibotenic and muscimol found in certain mushrooms
From 30 to 60 minutes
Somnolence and state of intoxication, confusion, muscular spasms, delirium, visual disorders
Amanita muscaria, A. pantherina, and related spp. of mushrooms
3
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Poisoning caused by mushrooms of the group that contains muscarine (muscarinism)
Muscarine found in certain mushrooms
15 minutes to a few hours
Excessive saliva-tion, perspirasaliva-tion, lacrimation, drop in blood pressure, irregular pulse, contraction of the pupils, blurred vision, asthmatic breathing
Clitocybe deal-bata, C. rivulose, and many spp. of Inocybe and Bole-tus mushrooms
Vomit Ingestion of A. muscaria and related spp., consumption of unknown varieties of mushrooms, consumption of toxic mushrooms by mistake
Chemical agents Organophosphorus poisoning
Organophosphorus insecticides, such as parathion, TEPP, diazinon, malathion
From a few minutes to a few hours
Nausea, vomiting, abdominal pains, diarrhoea, headache,
nervousness, blurred vision, chest pains, cyanosis, confusion, spasmodic contraction, convulsions
Any accidentally contaminated food
Blood, urine, adipose tissue (for biopsy)
Spraying of crops immediately before harvest, storage of insecticides in the same place as food, confusion of pesticides with food in powdered form
Carbamate poisoning Carbaryl (sevin), Temik (aldicarb)
½ hour Epigastric pain, vomiting, abnormal salivation, contraction of the pupils, lack of muscular
Any accidentally contaminated food
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Dinoflagellates
Paralytic Shellfish Poisoning
Saxitoxin and other dinoflagellate toxins of the spp. Alexandrium and Gymnodinium
Several minutes to 30 minutes
Tingling, burning, and numbness around the lips and the tips of the fingers, dizzy spells, incoherent speech, respiratory paralysis
Mussels and clams Gastric lavage Harvesting shellfish from water with high concentrations of dinoflagellates of the spp. Alexandrium and Gymnodinium
Tetrodotoxism (tetraodon poisoning)
Tetrodoxin found in the intestines and gonads of puffer fish (blowfish, globefish)
From 10 minutes to 3 hours
Sensation of tingling in the fingers and toes, dizziness, pallor, numbness of the mouth and limbs, gastrointestinal symptoms, haemorrhage and flaking of the skin, fixation of the eyes, spasmodic contraction, paralysis, cyanosis
Fish of the puffer fish family
Stool Ingestion of fish of the puffer fish family, consumption of such fish without extracting intestines and gonads
Poisonous plants
Jimsonweed (thorn apple) poisoning
Tropane alkaloids found in Datura stramonium
Less than 1 hour Abnormal thirst, photophobia, distorted vision, difficulty speaking, delirium, facial flushing, delirium, coma, rapid pulse heart attack.
Any part of the herb, tomatoes grown with grafts
3
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Water hemlock poisoning
Resin or cicutoxin found in water hemlock
From 15 to 60 minutes
Excessive salivation, nausea, vomiting, stomach pains, frothing at the mouth, irregular breathing, convulsions, respiratory paralysis
Root of water hemlock (Cicuta virosaand C. masculata)
Urine Ingestion of water hemlock; confusion of the root of water hemlock with wild parsnip, sweet potato, or carrot
4.2 Incubation period usually between 1 and 6 hours
Chemical agents hydrocarbon, such as aldrin, chlordane, DDT, dieldrin, endrin, lindane, and toxaphene
From 30 minutes to 6 hours
Nausea, vomiting, paresthesia, dizziness, muscular weakness, anorexia, weight loss, confusion
Any accidentally contaminated food
Blood, urine, stool, gastric lavages
Storage of insecticides in the same place as food, confusion of pesticides with food in powdered form
Marine plankton
Ciguatera poisoning Ciguatoxin from the intestines, roe, gonads, and flesh of tropical marine fish
From 3 to 5 hours, sometimes more
Tingling and numbness around the mouth, metallic taste, dryness of the mouth, gastrointestinal
Numerous varieties of tropical fish
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
4.3 Incubation period usually from 12 to 72 hours
Bacterial agents
Botulism Exoneurotoxins A, B, E and F from Clostridium botulinum. The spores are found in soil and animal intestines
From 2 hours to 8 days, average from 18 to 36 hours
Vertigo, double or blurred vision, dryness of the mouth, difficulty in swallowing, speaking and breathing; descending flaccid paralysis, constipation, dilation or fixation of the pupils, respiratory paralysis. Gastrointestinal symptoms can precede neurological symptoms. Is frequently fatal
Home-canned foods with low acid content, vacuum-packed fish; fermented roe, fish and marine mammals, fish that have not been gutted
Blood, stool, gastric lavage
Improper preparation of canned food and smoked fish, uncontrolled fermentation
4.4 Incubation period higher than 72 hours Chemical agents
Mercury poisoning Ethyl and methyl compounds of mercury in industrial waste and organic mercury in fungicides
1 week or more Numbness, weakness of the legs, spastic paralysis, deterioration in the vision, blindness, coma
Grains treated with fungicides that contain mercury; pork, fish, and shellfish exposed to mercury compounds
3
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Triorthocresyl phosphate poisoning
Triorthocresyl phosphate used as an extract or as a substitute for kitchen oil
From 5 to 21 days, average 10 days
Gastrointestinal symptoms, pains in the legs, very accentuated equine gait, limpness of feet and wrist
Cooking oils, extracts and other foodstuffs contaminated with triorthocresyl phosphate
Biopsy of the gastronemius muscle
Use of the compound as an extract or as oil for cooking or for salads
5. Manifestation of signs and symptoms of generalized infection (fever, chills, discomfort, pains)
5.1 Incubation period between 12-72 hours Bacterial agents
Infection caused by Vibrio vulnificus
Vibrio vulnificus 16 hours Septicaemia, fever, malaise, prostration, typical of cases with previous liver problems
Oysters and raw clams
Blood People with liver problems
Anthrax Bacillus anthracis From 3 to 5 days Gastroenteritis, vomiting, haemorrhagic depositions
Meat from sick animals
Stool, vomiting Clinical manifestations after consumption of meat from sick animals
Streptococcus suis infection
Streptococcus suis 3 hours to 14 days Headache, fever, vomiting, meningitis, septicaemia, endocarditis, toxic shock syndrome, arthritis, acute
Infected pigs or contaminated pork
CSF or blood samples
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
5.2 Incubation period longer than 1 week
Bacterial agents
Brucellosis Brucella abortus, B. melitensis, and B. suis in tissues and milk of infected animals
From 7 to 21 days Fever, chills, sweats, weakness, malaise, headache, myalgia and arthralgia, weight loss
Raw milk, goat cheese made with raw milk
Blood Unpasteurized milk, livestock infected by brucellosis, contact with aborted materials
Tuberculosis Mycobacterium bovis
4–12 weeks Lung lesions basically but also in kidneys, liver, spleen and corresponding nodes
Raw milk and meat Culture from secretions or tissues
Consumption of raw milk, consumption of raw infected meat from domestic or wild animals
Listeria infection Listeria monocytogenes
3 to 70 days, usually 4 to 21 days
Fever, headache, nausea, vomiting, abortion, meningitis, encephalitis, and sepsis
Milk, fresh cheese, processed meats
Blood, urine Improper cooking, non-pasteurization of milk, prolonged cooling
Typhoid and paratyphoid fever
S. enterica Serotype typhi found in faeces of infected people, other serotypes (as paratyphi A, cholera suis) for cases of paratyphoid, faeces of humans and animals
From 7 to 28 days, average 14 days
Malaise, headache, fever, cough, nausea, vomiting, constipation, abdominal pains, chills, rose spots, bloody stool
Shellfish, food contaminated by handlers, raw milk, cheese, watercress, water
Stool, rectal swabs, blood in early part of the acute phase, urine in the acute phase
4
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Viral agents
Hepatitis A Hepatitis A virus found in the faeces, urine, or blood of infected people and other infected non-human primates
From 10 to 50 days, average 25 days
Fever, malaise, lassitude, anorexia, nausea, abdominal pains, jaundice
Shellfish, any food contaminated with hepatitis virus, water
Stool, urine, blood
Infected handlers touching food, poor personal hygiene, improper cooking, harvesting shellfish from waters contaminated with sewage, improper disposal of wastewater
Hepatitis E Hepatitis E virus From 15 to 65 days usually 35 to 40
Similar to above (high mortality for pregnant women)
Shellfish, any food contaminated with hepatitis virus, water
Stool, urine, blood
Infected handlers touching food, poor personal hygiene, improper cooking, harvesting shellfish from waters contaminated with sewage, improper disposal of waste water Parasitic agents
Angiostrongy-liasis (Eosinophilic meningoencephalitis)
Angiosgtrongylus cantonensis (lung-worm of rats) found in rodent droppings and the soil
From 14 to 16 days
Gastroenteritis, headache, stiffness of the neck and back, low-grade fever
Crabs, prawns, slugs, shrimp, raw snails
Blood Improper cooking
Toxoplasmosis Toxoplasma gondii found in tissues and
From 10 to 13 days
Fever, headache, myalgia, cutaneous
Raw or
undercooked meat
Lymph nodes (for biopsy), blood
B
Disease Etiologic agent or
cause
Incubation period (latency)
Signs and
symptoms Food implicated
Specimens to
be obtained Contributing factors
Trichinosis Trichinella spiralis found in pork and bear meat
From 4 to 28 days, average 9 days
Gastroenteritis, fever, oedema around the eyes, myalgia, chills, prostration, difficulty breathing
Pork, bear, walrus Muscle tissue (for biopsy)
Ingestion of undercooked pork or bear meat, improper cooking or temperatures, feeding pigs with garbage that has not been cooked or properly treated with heat 6. Allergic symptoms and signs (flushing and itching of the face)
Incubation period less than 1 hour
Bacterial agents (and animals)
Scombroid poisoning (Histamine Poisoning)
Histamine-like substances produced by Proteus spp. or other histidine bacteria found in the flesh of fish
From a few minutes to 1 hour
Headache, dizziness, nausea, vomiting, peppery taste, burning in the throat, facial swelling and flushing, colic, itching
Tuna fish, blue mackerel, Pacific dolphin, cheese
Vomit Inadequate refrigeration of scombroid fish, improper curing of cheese
Chemical agents Monosodium glutamate poisoning
Excessive quantity of monosodium glutamate
From a few minutes to 1 hour
Burning sensation in the back of the neck, forearms and chest; tightness, tingling, facial flushing, dizziness, headache, nausea
Food seasoned with monosodium glutamate
Use of excessive quantities of
monosodium glutamate to enhance flavour. Only some individuals are sensitive to the MSG
Nicotinic acid poisoning (niacin)
Sodium nicotinate used as colour preservative
From a few minutes to an hour
Reddening, hot flashes, itching, abdominal pains, swelling of the face and knees
Meat or other food to which sodium nicotinate has been added