2011 International Conference on Electrical Engineering and Informatics
17-19 July 2011, Bandung, Indonesia
Doppler Blood Flow Detector for Haemorrhoidal
Artery Ligation
Daniel Santoso
1, Sugandi Hardjanto
21
Department of Electronics and Computer Engineering, Satya Wacana Christian University 52 th – 60th Diponegoro Rd., Salatiga, Indonesia 50711
1
2
Kasih Ibu General Hospital
404th Slamet Riyadi Rd., Surakarta, Indonesia 57142
2
Abstract— Haemorrhoidal artery ligation (HAL) is a novel non-invasive surgical treatment for haemorrhoids. The procedure entails precise identification of the superior rectal arteries supplying haemorrhoids using a Doppler transducer mounted on a proctoscope and a Doppler signal processor. To perform HAL the surgeon at Kasih Ibu General Hospital used medical device called Ultrasonic Blood Flow Detector KM-25 series from HADECO Co., Ltd. The problem is that the performance of the device has significantly degraded due to wear. The arterial sound produced by the device is also inherently indistinct when operated in operating room. The offered solution was to develop own receiver and proctoscope according the partner’s requirement. A prototype of the detector has been successfully developed and fully functional in the hospital. It consists of two major parts, i.e. proctoscope and the main unit. The proctoscope is a product of AMI GmbH, Austria. The prototype of the main unit consists of a receiver, a power amplifier, and a loudspeaker. Using specially designed 75 W RMS power amplifier, the average sound pressure level produced is 60 dBA in a spot within 1.5 meter from the loudspeaker. Within 6 month of evaluation period, it has been used to perform surgery on 27 patients mostly with grade III-IV haemorrhoids.
Keywords— haemorrhoids, HAL, Doppler
I. INTRODUCTION
Haemorrhoids, also known as piles, are symptomatic dilated anal cushions, which have a normal physiological role in maintaining continence. A combination of ageing, resulting in degeneration of the connective tissue framework supporting the anal cushions, together with repeated passage of hard stools, leads to their descent and prolapse [1]. This in turn results in venous engorgement that can be exacerbated by further straining or conditions in which there is raised intra-abdominal pressure, such as pregnancy. Localized trauma to the prolapsing tissue causes bleeding [2]. Haemorrhoids are generally classified as external or internal with relation to the dentate line, whilst internal haemorrhoids are further subdivided according to the degree of prolapse. First degree piles remain internal but bleed. Second degree piles prolapse on defaecation, but reduce spontaneously, whilst third degree requires manual reduction. Fourth degree haemorrhoids are permanently prolapsed and cannot be reduced [3].
Conservative treatment has traditionally been recommended for the treatment of grade I and II haemorrhoids including; changing bowel habit through dietary and life-style changes, increased oral hydration and the use of stool softeners and laxatives. Increased dietary fibre has been demonstrated to be consistently beneficial in relieving over-all symptoms and bleeding [4]. Non-surgical interventions including rubber band ligation, injection sclerotherapy, cryotherapy, laser therapy, diathermy coagulation and infrared coagulation [5]. These can be performed in outpatient setting and are considered to be primary options in the treatment of grade I-III haemorrhoids [6]. Meta analysis of outcomes from these interventions has demonstrated rubber band ligation to be most effective in terms of response to treatment and reduced requirement for further intervention [6].
Surgical intervention is usually the treatment of choice for grade III-IV haemorrhoids, prolapsed grade II haemorrhoids that have failed to respond to non-surgical treatments, and circumferential grade II haemorrhoids [7].
Surgical haemorrhoidectomy involving excision of the haemorrhoidal cushions is the traditional surgical approach used for treating haemorrhoids [8]. It is a technique that has been demonstrated to have successful long-term results and has been previously stated as the only effective treatment for large external haemorrhoids [9]. Unfortunately there is significant morbidity associated with surgical haemorrhoidectomy. In particular it has a reputation for being extremely painful procedure for a fairly benign condition [10]. Other significant short term complication include; urination retention (20.1%), bleeding (secondary or reactionary) (2.4%-6%), and subcutaneous abscesses (0.5%) whilst documented long term complications include anal fissure (1%-2.6%), anal stenosis (1%), incontinence (0.4%), fistula (0.5%) and recurrent haemorrhoidal symptoms (20%) [5].
Haemorrhoidal artery ligation (HAL) is a novel non-invasive surgical treatment for haemorrhoids that was developed by the Japanese surgeon Morinaga in 1995 [11]. It is a technique that is based upon an understanding of the pathogenesis and arterial inflow to haemorrhoids and can potentially be performed under sedation and/or local anaesthesia. The procedure entails precise identification of the A1 - 3
superior rectal arteries supplying haemorrhoids using a Doppler transducer located in the side wall of a special proctoscope, as shown in Fig. 1.
Fig. 1 Proctoscope usage in HAL surgery
Using an applied frequency of 8.2 MHz and an introduction
angle of approximately 60o a screening depth of
approximately 7 mm is provided [12]. This enables identification of the haemorrhoidal arteries which are then selectively suture ligated 2-3 cm above the dentate line through a lateral ligation window within the proctoscope (situated proximally to the transducer). Ligation of these arteries prevents inflowing blood to the haemorrhoidal venous plexi internal pressures and subsequently results in both a cessation of haemorrhoidal bleeding and shrinkage of haemorrhoidal tissues [11]. Morinaga et al’s initial study reported promising results using the HAL on 116 patients. One month post the procedure symptoms of bleeding have stopped in 96% of the patients, 95% had pain relief and 78% had improvement in prolapse symptoms [11]. These results have been replicated by several other single centre studies of larger sample sizes [12]–[14]. These studies also demonstrated that the technique is well tolerated, is a relatively painless procedure and is able to be performed with reduced anaesthetic intervention using sedation and/or local anaesthesia. This also results in reduced length of hospital admission. The majority of patients treated by the HAL technique in studies to date have suffered with grade II or III haemorrhoids with only small numbers of grade IV patients.
The research team collaborated with a surgeon from local hospital in conducting this interdisciplinary research. He has a great interest in minimally invasive surgery techniques, including HAL. To date, to perform HAL he used medical device called Ultrasonic Blood Flow Detector KM-25 series from HADECO Co., Ltd. The problem is that the performance of the device has significantly degraded due to wear. Furthermore, the device has been discontinued and the company has been closed. Thus it would be impossible to get the part or product replacement. The major drawback is that arterial sound produced by the device is not sufficiently distinct when operated in operating room. Solution offered by the research team was to develop own receiver and proctoscope according our partner’s requirement.
The research regarding the device was conducted in two consecutive phase. The result of the first phase was published in a proceeding and disseminated in a national seminar [15]. The prototype of the research had not been used yet in real
surgery because of the inadequate performance. Nevertheless, the prototype was able to detect blood flowing inside the radial artery at the wrist. This preliminary achievement paved the way for development of fully functional Doppler blood flow detector for haemorrhoidal artery ligation.
II. PRINCIPLES,DESIGNANDIMPLEMENTATION
In this chapter, the fundamental principles of blood flow detection using Doppler ultrasound are reviewed first to establish better understanding upon design and implementation section that discussed subsequently.
A. Principles of Doppler Blood Flow Detection
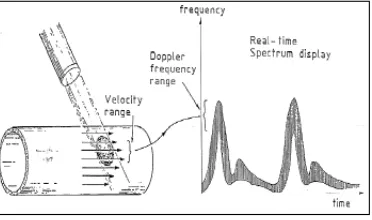
Doppler principle has been widely accepted as aural means for fluid flow measurement in various kind of medium, including blood flow in the blood vessel [16]. The Doppler Effect is the frequency phase shift of the signal or wave when it is reflected from a moving object, in this case the flow of red cells. If the blood flow is toward the transducer, the perceived frequency will be higher. If the blood flow is moving away from the transducer, the perceived frequency decreases. Doppler systems are totally dependent on the changes in the frequency of the transmitted ultrasound that results from the encounter of the wavefront with moving fluid. Direction of the flow is determined from the frequency phase shift of the returning wave. A visual understanding of this principle can be gained by observing Fig. 2.
Fig. 2 Doppler principle in blood flow detection
Doppler frequency is proportional to blood velocity in the sampled volume and as the arterial blood flow is pulsed the Doppler signal has a spectrum that constantly varies in the time domain. In ideal conditions the Doppler power spectrum has a similar form to a blood flow histogram in the sampled volume. This is depicted in Fig. 3.
Doppler ultrasound systems either continuous or pulsed are used as non-invasive method for detection and evaluation of blood flow [17]. Continuous wave (CW) Doppler is the older and electronically simpler of the two kinds. As the name implies, CW Doppler involves continuous generation of ultrasound waves coupled with continuous ultrasound reception. A two crystal transducer accomplishes this dual function with one crystal devoted to each function. The main advantage of CW Doppler is its ability to measure high blood velocities accurately. The main disadvantage of CW Doppler is its lack of selectivity or depth discrimination. Since CW Doppler is constantly transmitting and receiving from two different transducer heads (crystals) there is no provision for range gating to allow selective placing of a given Doppler sample volume in space. As a consequence, the output from a CW examination contains Doppler shift data from every red cell reflecting ultrasound back to the transducer along the course of the ultrasound beam.
Pulsed wave (PW) Doppler systems use a transducer that alternates transmission and reception of ultrasound. One main advantage of pulsed Doppler is its ability to provide Doppler shift data selectively from a small segment along the ultrasound beam, referred to as the sample volume. An ultrasound pulse is transmitted into the tissues travels for a given time (time X) until it is reflected back by a moving red cell. It then returns to the transducer over the same time interval but at a shifted frequency. The total transit time to and from the area is 2X. Since the speed of ultrasound in the tissues is constant, there is a simple relationship between roundtrip travel time and the location of the sample volume relative to the transducer face (i.e., distance to sample volume equals ultrasound speed divided by round trip travel time).
The blood flow velocity profile in humans is within 20 – 750 mm/s range and the ultrasound velocity in tissue is around 1540 – 1600 m/s [18], [19]. Using an applied frequency of 8.2
MHz, the Doppler signal bandwidth (fd) can be calculated
using the following expression:
o
where v is the blood velocity (m/s), c is the ultrasound
velocity in the medium, and fo is the transducer frequency.
Using this expression and the values given above it is possible to see that the Doppler signal is within 200 – 7500 Hz. Utilizing the Doppler Effect it is possible to receive that frequency which will be amplified and mixed into an acoustic wave.
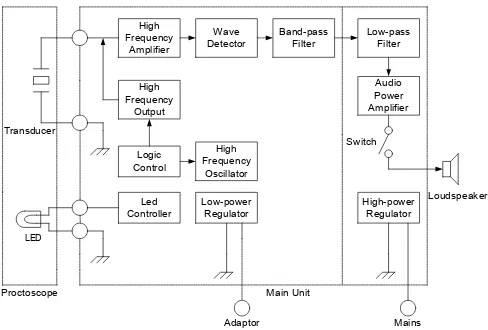
B. Design and Implementation of Doppler Blood Flow Detector
The developed medical device consists of two major parts, the proctoscope and the main unit. Proctoscope is a medical instrument that facilitates haemorrhoid arteries detection and ligation inside the anus. Main unit serves as ultrasound signal processor that produces audible arterial sound when blood flow is detected. A block diagram for the complete system is shown in Fig. 4.
Fig. 4 The block diagram of the Doppler blood flow detector
Since proctoscope will always comes into direct contact with living tissue, the safety, sterility, and comfort during use become major considerations. Therefore commercial product
from AMI GmbH, Austria (www.ami.at) is utilized. The
proctoscope involves a hollow insertion plastic cylinder which is enclosed at the distal end and open at the near end, and can be inserted through the anus. The cylinder has an ultrasound transducer in its interior wall for detecting blood flow in the affected artery, and a ligation hole next to the transducer. The transducer made from piezoelectric ceramic, which is excited in pulsed mode using 8.2 MHz carrier frequency. There are four high-bright LEDs attached at the near end of the proctoscope to provide decent illumination during ligation.
The core of the circuitry in main unit is a skilful manipulation of ultrasonic wave as it propagates from the source to the flowing substance. The wave will then reflect back to the main unit for final manipulations so the desired output signal can fit within the limited human hearing reception.
A high frequency oscillator generates a square wave signal which is transformed into high voltage pulses by high frequency amplifier. The excitation of the signal is administered by logic controller. These pulses are guided with
the help of a transducer at approximately 60o with respect to
III.RESULTANDDISCUSSION
A prototype of the detector has been successfully developed and tested. Furthermore, the prototype had been fully functional as one of the medical devices in Kasih Ibu General Hospital starting from October 2010. The associated medical service also promoted as one of the ultimate services in that hospital.
As the design implies, the prototype consists of two major parts, i.e. proctoscope and the main unit. The proctoscope is a product of AMI GmbH, Austria consisting of two separated components, the handle and the probe. The probe can be removed from the handle for sterilization purpose. The probe is made of plastic, 80 mm long and 28 mm outer diameter. The proctoscope is depicted in Fig. 5.
Fig. 5 Proctoscope from AMI GmbH, Austria
The prototype of the main unit consists of three major parts, a receiver, a power amplifier, and a loudspeaker. The front panel of power amplifier houses main switch, power indicator, failure indicator, mute switch, and volume knob. The front panel of receiver houses main switch, light switch, and 5-pins DIN socket. Loudspeaker enclosure is bass reflex type housing a woofer speaker. The transducer and the LEDs in the probe are wired through the handle. The cables, using special adaptor then connected to the receiver through the socket. The main unit is shown in Fig. 6.
Fig. 6 Main unit
The specification can be listed as follows:
• power supply : AC 220 V 400 mA,
• power output : 75 W RMS,
• ultrasonic generator : 8.2 MHz pulsed wave,
• receiver dimension : 200 x 160 x 50 mm (w x h x d),
• amplifier dimension : 400 x 300 x 100 mm (w x h x d).
The haemorrhoid arterial sound that comes out from the speaker is clearly audible within a distance no more than 5 meters. In practical use, it is never distanced more than 1.5 meter from the doctor. Within the distance the average measured arterial sound pressure level is 60 dBA with the volume knob at the middle position.
To date, the prototype has been successfully used to treat more than 20 patients by HAL technique. Most of them suffer with grade III or IV haemorrhoids. The detail of the treated patients within certain period is summarized in Table 1.
TABLE I
SUMMARY OF TREATED PATIENTS
According to Table 1, within 6 months evaluation period there are 27 patients undergo surgery by HAL technique using the prototype. Thus far, there is no performance degradation or parts deterioration reported by the user.
IV.CONCLUSIONS
The Doppler blood flow detector for haemorrhoidal artery ligation has been successfully built and tested. The medical device consists of proctoscope and main unit. The proctoscope has transducer made from piezoelectric ceramic, pulsed mode with 8.2 MHz carrier frequency and illumination device made of LEDs. The main unit produces audible arterial sound in 80 – 2000 Hz frequency range when superior rectal artery supplying haemorrhoids is detected. Using specially designed 75 W RMS power amplifier, the average sound pressure level produced is 60 dBA in a spot within 1.5 meter from the loudspeaker.
The medical device has been demonstrated to have successful long-term utilization in the hospital. Within 6 month of evaluation period, it has been used to perform surgery on 27 patients mostly with grade III-IV haemorrhoids.
In design and implementation of the next generation of the device it is envisioned to incorporate visual indicator in addition to existing aural indicator. It is also envisioned to make muting more convenient by replacing the toggle switch with wired footswitch.
ACKNOWLEDGMENT
REFERENCES
[1] O. C. Gass and J. Adams, “Haemorrhoids:Etiology and Patology,”
American Journal of Surgery, vol. 9, pp. 40–43, 1950.
[2] W. H. Thomson, “The nature of haemorrhoids,” British Journal of
Surgery, vol. 62, pp. 542–52, 1975.
[3] J. P. S. Thomson, R. J. Leicester, and L. E. Smith, Coloproctology and the Pelvic Floor, 2nd ed., Oxford, United Kingdom: Butterworth-Heinemann Ltd., 1992.
[4] P. Onso-Coello, G. Guyatt, and D. Hells-Ansdell et. al., “Laxatives for the treatment of haemorrhoids,” Cochrane Database System, CD004649 4, 2005.
[5] V. Shanmugam, M. A. Thaha, and K. S. Rabindranath et. al., “Rubber
band ligation versus excisional haemorrhoidectomy for haemorrhoids,” Cochrane Database System, CD005034 3, 2005.
[6] H. M. MacRae, R. S. MacLeod, “Comparison of haemorrhoidal
treatment modalities:A meta analysis,” Diseases of the Colon and
Rectum., vol. 38, pp. 687–694, 1995.
[7] H. Tucker, E. George, and R. Patel, “Stapled haemorrhoidopexy for the
treatment of haemorrhoids,” National Institute for Health and Clinical Excellence, High Holborn, London, NICE Tech. Rep. TA128, 2007. [8] A. L. Polglase, “Haemorrhoids:a clinical update,” The Medical Journal
of Australia, vol. 167, pp. 85–88, 1999.
[9] E. A. Carapeti, M. A. Kamm, and P. J. McDonald et.al., “Double-blind
randomized controlled trial of effect of metronidazole on pain after
day-case haemorrhoidectomy,” The Lancet, vol. 2, pp. 1119–1124,
1998.
[10] B. J. Mehigan, J. R. Monson, and J. E. Hartley, “Stapling procedure for
haemorrhoids versus Milligan-Morgan haemorrhoidectomy:randomized controlled trial,” The Lancet, vol. 355,
pp. 782–785, 2000.
[11] K. Morinaga, K. Hasuda, and T. Ikeda , “A novel therapy for internal
haemorrhoids:ligation of the haemorrhoidal artery with a newly
devised instrument (Moricorn) in conjunction with a Doppler flowmeter ,” American Journal of Gastroenterology, vol. 90, pp. 610– 613, 1995.
[12] M. Scheyer, E. Antonietti, and G. Rollinger et.al., “Doppler-guided
haemorrhoidal artery ligation,” American Journal of Surgery, vol. 191, pp. 89–93, 2006.
[13] P. P. Dal Monte, C. Tagariello, and T. Sarago et.al., “Transanal
haemorrhoidal dearterialization:non-excisional surgery for the treatment of haemorrhoidal disease,” Techniques in Coloproctology, vol. 11, pp. 333–338, 2007.
[14] M. Lienert, and B. Ulrich, “Doppler-guided ligation of the
haemorrhoidal arteries, ”Deutsche Journal of Medical , vol. 129, pp. 947–950, 2004.
[15] D. Santoso, D. Utomo, and I. Setyawan, “Rekayasa alat pendeteksi
aliran darah dengan prinsip Doppler untuk operasi wasir dengan teknik DG-HAL,” in Proc. SNTI, 2010, paper 7, p. TE7-1.
[16] P. Atkinson and J. P. Woodcock, Doppler ultrasound and its clinical
measurement, London, United Kingdom: Academic Press, 1982.
[17] S. M. Lawrence, “Computing the discrete time “analytic” signal via
FFT,” IEEE Transactions on Signal Processing, vol. 47, pp. 2600–
2603, 1999.
[18] P. J. Fish, “Non-stationary broadening in pulsed Doppler spectrum
measurements,” Ultrasound in Medicine and Biology, vol. 17, pp. 147– 155, 1991.
[19] P. Atkinson, “A fundamental interpretation of ultrasonic Doppler