16/02/18 17.53 STM Publishing House | Impacting the World of Science
Books & Journals, Online & Print
Home News Books & Journals Service About IOS Press Contact
Home Catalogue Journals Journal of Neonatal-Perinatal Medicine
Journal of Neonatal-Perinatal Medicine
ISSN print
Recommend this title to your librarian
1934-5798 1878-4429 11; 4 issues
Last issue (10:4) online on 29 December 2017 11:1 scheduled for March 2018
1-10
Biochemistry, Medicine & Health, Pediatrics
INSTITUTIONAL SUBSCRIPTION FOR 2018
€
350 / US$445
Excluding VAT
Subscribe to Print
Aims & Scope Editorial board Manuscript submission & Author instructions Abstracted/Indexed in Please visit the journal's websites: www.jnpm.org / www.jnpm.net.
Editor-in-Chief
Hany Z. Aly, MD, FAAP
Chairman, Department of Neonatology Cleveland Clinic Children's Hospital Cleveland, OH
H. Abdel-Hady, Mansoura, Egypt N. Badawi, Westmead, Australia S. Baumgart, Washington, DC, USA T. Berger, Lucerne, Switzerland N.-Y. Boo, Seremban, Malaysia H.U. Bucher, Zurich, Switzerland H. Caksen, Konya, Turkey A. Campana, Geneva, Switzerland R. Cooke, Liverpool, United Kingdom M. Cuttini, Rome, Italy
P. Dennery, Philadelphia, PA, USA S.M. Donn, Ann Arbor, MI, USA N. Evans, Sydney, Australia T.F. Fok, Hong Kong, China T. Hammad, Rockville, MD, USA R.H. Hentschel, Freiburg, Germany M. Khashaba, Mansoura, Egypt S. Kusuda, Tokyo, Japan A. Kwee, Utrecht, The Netherlands L. Liu, Xi’an, China
J.M. Lorenz, New York, NY, USA P. Manzoni, Torino, Italy R. Martin, Cleveland, OH, USA D.M. Null, Jr., Salt Lake City, UT, USA E. Papiernik, Paris, France
R. Polin, New York, NY, USA H. Rabe, Brighton, United Kingdom G. Samy, Cairo, Egypt
G.M. Sant'Anna, Montreal, QC, Canada K.-T.M. Schneider, Munich, Germany A. Sola, Irvine, CA, USA
B.D. Solomon, Bethesda, MD, USA G.E. Stahl, Camden, NJ, USA
IOS Press Copyright 2018
Disclaimer Sitemap FAQ
FOLLOW US ON FACEBOOK FOLLOW US ON TWITTER FOLLOW US ON GOOGLE+
Expand nextprevious Close Previous
0/0
Next
J.J. Steichen, Cincinnati, OH, USA P.-N. Tsao, Taipei, Taiwan
J.N. Van Den Anker, Washington, DC, USA M. Vento, Valencia, Spain
P. Wintermark, Montreal, QC, Canada M.R. Wolfson, Philadelphia, PA, USA
North America Europe Asia
16/02/18 17.53 IOS Press
The aim of the
Journal of Neonatal-Perinatal Medicine
is to strengthen research and
education of the neonatal community on the optimal physical, mental and social
health and well-being of infants through high quality publications on
neonatal-perinatal medicine and to provide examples of best practices in order to improve
the quality, safety and effectiveness of infants’ healthcare worldwide.
The vision for the journal is to be ‘The Reference Journal’ in the field of neonatology.
Show:
results per page
Journal of Neonatal-Perinatal Medicine - Volume 9, issue 4
Purchase individual online access for 1 year to this journal.
Price: EUR 90.00
Authors:
Karakash, S.D. (https://content.iospress.com:443/search?
q=author%3A%28%22Karakash%2C+S.D.%22%29) | Tschankoshvili, N.
(https://content.iospress.com:443/search?q=author%3A%28%22Tschankoshvili%2C+N.%22%29) | Weedon,
J. (https://content.iospress.com:443/search?q=author%3A%28%22Weedon%2C+J.%22%29) | Schwartz, R.M.
(https://content.iospress.com:443/search?q=author%3A%28%22Schwartz%2C+R.M.%22%29) | Kirschbaum,
C. (https://content.iospress.com:443/search?q=author%3A%28%22Kirschbaum%2C+C.%22%29) | Minkoff,
H. (https://content.iospress.com:443/search?q=author%3A%28%22Minkoff%2C+H.%22%29)
Article Type:
Review Article
Abstract:
OBJECTIVE: We sought to determine whether hypocortisolism is associated with preterm
birth, using hair cortisol as a marker of long term hypothalamic-pituitary-adrenal axis activity.
STUDY DESIGN: In a prospective, matched, case-control study, 29 women who had a preterm birth at
24–36w5d gestation were compared to 29 women who delivered at term, matched for maternal
age, gestational age, and ethnicity. Cases’ samples were collected within 72
h of preterm birth and
controls at the same gestational age as the corresponding case. Participants completed validated
questionnaires regarding general stress and childhood trauma. The Wilcoxon signed-rank test was
used to compare … Show more
Keywords:
Hair cortisol, preterm birth, stress in pregnancy, stress response
Mark all
!
Hypocortisolism and preterm birth
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm1640)
!
16/02/18 17.53 Journal of Neonatal-Perinatal Medicine - Volume 9, issue 4 - Journals - IOS Press
Page 2 of 7 https://content.iospress.com/journals/journal-of-neonatal-perinatal-medicine/9/4?start=0
DOI:
10.3233/NPM-161640
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 333-339, 2016
Price: EUR 27.50
Authors:
Ibrahim, Z.H. (https://content.iospress.com:443/search?
q=author%3A%28%22Ibrahim%2C+Z.H.%22%29) | Chari, G. (https://content.iospress.com:443/search?
q=author%3A%28%22Chari%2C+G.%22%29) | Abdel Baki, S. (https://content.iospress.com:443/search?
q=author%3A%28%22Abdel+Baki%2C+S.%22%29) | Bronshtein, V.
(https://content.iospress.com:443/search?q=author%3A%28%22Bronshtein%2C+V.%22%29) | Kim, M.R.
(https://content.iospress.com:443/search?q=author%3A%28%22Kim%2C+M.R.%22%29) | Weedon, J.
(https://content.iospress.com:443/search?q=author%3A%28%22Weedon%2C+J.%22%29) | Cracco, J.
(https://content.iospress.com:443/search?q=author%3A%28%22Cracco%2C+J.%22%29) | Aranda, J.V.
(https://content.iospress.com:443/search?q=author%3A%28%22Aranda%2C+J.V.%22%29)
Article Type:
Research Article
Abstract:
OBJECTIVES: First, to determine the feasibility of an ultra-compact wireless device (micro
EEG) to obtain multichannel electroencephalographic (EEG) recording in the Neonatal Intensive
Care Unit (NICU). Second, to identify problem areas in order to improve wireless EEG performance.
STUDY DESIGN: 28 subjects (gestational age 24–30 weeks, postnatal age <30 days) were recruited
at 2 sites as part of an ongoing study of neonatal apnea and wireless EEG. Infants underwent 8-9
hour EEG recordings every 2–4 weeks using an electrode cap (ANT-Neuro) connected to the
wireless EEG device (Bio-Signal Group). A 23 electrode configuration was used incorporating the …
Show more
Keywords:
Apnea, electroencephalography, premature infants, seizure
DOI:
10.3233/NPM-161643
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 341-348, 2016
Authors:
Korkmaz, Levent (https://content.iospress.com:443/search?
q=author%3A%28%22Korkmaz%2C+Levent%22%29) | Baştuğ, Osman
(https://content.iospress.com:443/search?
q=author%3A%28%22Ba%C5%9Ftu%C4%9F%2C+Osman%22%29) | Daar, Ghaniya
Wireless multichannel electroencephalography in the newborn
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm1643)
!
The effects of thyroid function on retinopathy of prematurity
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm915150)
(https://content.iospress.com:443/search?q=author%3A%28%22Daar%2C+Ghaniya%22%29) | Korkut,
Sabriye (https://content.iospress.com:443/search?q=author%3A%28%22Korkut%2C+Sabriye%22%29) |
Özdemir, Ahmet (https://content.iospress.com:443/search?
q=author%3A%28%22%C3%96zdemir%2C+Ahmet%22%29) | Adnan Öztürk, Mehmet
(https://content.iospress.com:443/search?
q=author%3A%28%22Adnan+%C3%96zt%C3%BCrk%2C+Mehmet%22%29) | Güneş, Tamer
(https://content.iospress.com:443/search?q=author%3A%28%22G%C3%BCne%C5%9F%2C+Tamer%22%29)
| Kurtoğlu, Selim (https://content.iospress.com:443/search?
q=author%3A%28%22Kurto%C4%9Flu%2C+Selim%22%29)
Article Type:
Research Article
Abstract:
OBJECTIVES: To assess whether TSH and fT4 have a role in the angiogenesis of
vaso-obliteration and neovascularization which are the basic pathophysiology of ROP. METHODS: In this
retrospective case-control study, the control group (n
=
56) included preterm newborns with risk for
ROP while the laser group (n
=
63) was recruited from cases who developed severe
neovascularization and needed laser photocoagulation therapy. Considering the first
(vaso-obliteration) and second (neovascularization) phases of the disease, in this study we researched the
distribution of thyroid function tests between groups. RESULTS: With regard to the first phase of the
disease, … Show more
Keywords:
Retinopathy of prematurity, thyroxine, thyroid stimulating hormone, vascular endothelial
growth factor
DOI:
10.3233/NPM-915150
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 349-356, 2016
Price: EUR 27.50
Authors:
McClure, C. (https://content.iospress.com:443/search?
q=author%3A%28%22McClure%2C+C.%22%29) | Jang, S. Young (https://content.iospress.com:443/search?
q=author%3A%28%22Jang%2C+S.+Young%22%29) | Fairchild, K. (https://content.iospress.com:443/search?
q=author%3A%28%22Fairchild%2C+K.%22%29)
Article Type:
Research Article
Abstract:
BACKGROUND: Alarm overload is a significant concern in the Neonatal Intensive Care Unit
(NICU). Selecting a longer oxygen saturation (SpO2 ) averaging time will reduce the number of
alarms but may mask fluctuations in oxygenation. OBJECTIVE: Characterize bedside monitor alarms
in the NICU and estimate the impact of longer SpO2 averaging time and alarm delay. METHODS: All
bedside monitor alarms were analyzed over a 12-month period in the University of Virginia NICU,
using the default averaging time (8 seconds) and SpO2 alarm limits set at 88–95% for infants on
supplemental oxygen. In 10 … Show more
Keywords:
Alarm, pulse oximetry, oxygen saturation, preterm infant, averaging, hypoxemia, very low
birthweight
DOI:
10.3233/NPM-16162
Alarms, oxygen saturations, and SpO averaging time in the NICU
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm162)
16/02/18 17.53 Journal of Neonatal-Perinatal Medicine - Volume 9, issue 4 - Journals - IOS Press
Page 4 of 7 https://content.iospress.com/journals/journal-of-neonatal-perinatal-medicine/9/4?start=0
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 357-362, 2016
Price: EUR 27.50
Authors:
Elmekkawi, A. (https://content.iospress.com:443/search?
q=author%3A%28%22Elmekkawi%2C+A.%22%29) | Abdelgadir, D.
(https://content.iospress.com:443/search?q=author%3A%28%22Abdelgadir%2C+D.%22%29) | Van Dyk, J.
(https://content.iospress.com:443/search?q=author%3A%28%22Van+Dyk%2C+J.%22%29) | Choudhury, J.
(https://content.iospress.com:443/search?q=author%3A%28%22Choudhury%2C+J.%22%29) | Dunn, M.
(https://content.iospress.com:443/search?q=author%3A%28%22Dunn%2C+M.%22%29)
Article Type:
Research Article
Abstract:
OBJECTIVES: A new guideline for the early respiratory management of preterm infants that
included early nCPAP and INSURE was recently introduced in our NICU. This case series describes
the clinical courses of a group of preterm infants managed according to this guideline, and reports
the rates of successful extubation within 30 minutes of surfactant administration with and without
the use of naloxone and adverse events encountered. STUDY DESIGN: Descriptive case series of all
preterm babies admitted to our unit who were candidates for INSURE procedure with
premedication from August 2012 to August 2013. RESULTS: A … Show more
Keywords:
Endotracheal intubation, preterm, newborn, premedication, naloxone, INSURE
DOI:
10.3233/NPM-915141
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 363-370, 2016
Price: EUR 27.50
Authors:
Mehta, Y. (https://content.iospress.com:443/search?q=author%3A%28%22Mehta%2C+Y.%22%29)
| Shetye, J. (https://content.iospress.com:443/search?q=author%3A%28%22Shetye%2C+J.%22%29) |
Nanavati, R. (https://content.iospress.com:443/search?q=author%3A%28%22Nanavati%2C+R.%22%29) |
Mehta, A. (https://content.iospress.com:443/search?q=author%3A%28%22Mehta%2C+A.%22%29)
Article Type:
Research Article
Use of naloxone to minimize extubation failure after premedication for
INSURE procedure in preterm neonates
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm915141)
!
Physiological effects of a single chest physiotherapy session in
mechanically ventilated and extubated preterm neonates
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm915140)
Abstract:
OBJECTIVE: To assess the changes on various physiological cardio-respiratory parameters
with a single chest physiotherapy session in mechanically ventilated and extubated preterm
neonates with respiratory distress syndrome. STUDY DESIGN: This is a prospective observational
study in a neonatal intensive care unit setting. Sixty preterm neonates with respiratory distress
syndrome, thirty mechanically ventilated and thirty extubated preterm neonates requiring chest
physiotherapy were enrolled in the study. Parameters like heart rate (HR), respiratory rate (RR),
Silverman Anderson score (SA score in extubated), oxygen saturation (SpO2 ) and auscultation
findings were noted just before, immediately after chest physiotherapy but before suctioning,
immediately … Show more
Keywords:
Respiratory therapy, premature, suction, airway extubation, oxygen, NICU
DOI:
10.3233/NPM-16915140
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 371-376, 2016
Price: EUR 27.50
Authors:
El-Kafrawy, Ula
(https://content.iospress.com:443/search?q=author%3A%28%22El-Kafrawy%2C+Ula%22%29) | Taylor, R.J. (https://content.iospress.com:443/search?
q=author%3A%28%22Taylor%2C+R.J.%22%29)
Article Type:
Research Article
Abstract:
OBJECTIVES: To determine the accuracy of weighing ventilated infants on incubator scales
and whether the accuracy can be improved by the addition of a ventilator tube compensator (VTC)
device to counterbalance the force exerted by the ventilator tubing. STUDY DESIGN: Body weights
on integral incubator scales were compared in ventilated infants (with and without a VTC), with
body weights on standalone electronic scales (true weight). Individual and series of trend weights
were obtained on the infants. The method of Bland and Altman was used to assess the introduced
bias. RESULTS: The study included 60 ventilated … Show more
Keywords:
Neonatology, intensive care, ventilated infants, incubator scales, weight measurement
DOI:
10.3233/NPM-161623
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 377-383, 2016
Price: EUR 27.50
Optimizing care of ventilated infants by improving weighing accuracy
on incubator scales
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm1623)
!
Influence of maternal factors on the successful outcome of kangaroo
mother care in low birth-weight infants: A randomized controlled trial
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm1628)
16/02/18 17.53 Journal of Neonatal-Perinatal Medicine - Volume 9, issue 4 - Journals - IOS Press
Page 6 of 7 https://content.iospress.com/journals/journal-of-neonatal-perinatal-medicine/9/4?start=0
Authors:
Lumbanraja, S.N. (https://content.iospress.com:443/search?
q=author%3A%28%22Lumbanraja%2C+S.N.%22%29)
Article Type:
Research Article
Abstract:
BACKGROUND: Kangaroo mother care (KMC) is associated with positive neonatal
outcomes. Studies demonstrated significant influence of maternal factors on the success of applying
KMC. AIM: To determine maternal factors that influence on anthropometric parameters in low birth
weight babies that received kangaroo mother care. METHODS: This is a randomized controlled
study that involved low birth weight newborns. We randomly assigned newborns into two groups; a
group who received KMC and a group who received conventional care. Maternal factors were
recorded. We followed weight, length, and head circumferences of newborns for thirty days.
RESULTS: … Show more
Keywords:
Low birth weight, KMC method, growth parameters
DOI:
10.3233/NPM-161628
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 385-392, 2016
Price: EUR 27.50
Authors:
Studer, E.M. (https://content.iospress.com:443/search?
q=author%3A%28%22Studer%2C+E.M.%22%29) | Marc-Aurele, K.L.
(https://content.iospress.com:443/search?q=author%3A%28%22Marc-Aurele%2C+K.L.%22%29)
Article Type:
Research Article
Abstract:
OBJECTIVE: Determine content of antenatal prematurity consultations and identify factors
associated with satisfaction. DESIGN: This is an observational study of consultations for possible
preterm delivery. Consultations were audio-recorded and analyzed. Parents and physicians were
surveyed post-consultation. RESULTS: We analyzed 17 audio-recordings. Mean gestation was
28 weeks. Frequency of topics discussed were: antenatal steroids 82%, intubation 82%, breast milk
76%, time in NICU 65%, development 59%, and survival 53%. Parents frequently asked about length
of hospitalization stay, feeding, and separation concerns. Parents’ greatest fears were developmental
problems, survival, separation from baby, infant health, and length of hospitalization. … Show more
Keywords:
Preterm, neonatology, antenatal, prenatal, consultation, parental, and communication
DOI:
10.3233/NPM-16168
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 393-400, 2016
Price: EUR 27.50
Lost in explanation: Lessons learned from audio-recordings and surveys
of the antenatal consultation
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm168)
Authors:
Cordero, L. (https://content.iospress.com:443/search?
q=author%3A%28%22Cordero%2C+L.%22%29) | Oza-Frank, R. (https://content.iospress.com:443/search?
q=author%3A%28%22Oza-Frank%2C+R.%22%29) | Moore-Clingenpeel, M.
(https://content.iospress.com:443/search?q=author%3A%28%22Moore-Clingenpeel%2C+M.%22%29) |
Landon, M.B. (https://content.iospress.com:443/search?q=author%3A%28%22Landon%2C+M.B.%22%29) |
Nankervis, C.A. (https://content.iospress.com:443/search?
q=author%3A%28%22Nankervis%2C+C.A.%22%29)
Article Type:
Research Article
Abstract:
BACKGROUND: In the US, at the time of discharge from the hospital, 79% of women had
initiated breastfeeding. Intention to breastfeed is a strong predictor of breastfeeding initiation;
however, we reported initiation failure in 45% of women with pregestational diabetes who intended
to breastfeed. Information regarding intention and initiation among women with other high risk
obstetrical conditions (HROB) remains scarce. OBJECTIVE: To ascertain demographic and clinical
factors associated with breastfeeding initiation failure among women with HROB conditions who
intended to breastfeed. METHODS: The study population is comprised of 89 women with diabetes
(DM), 57 who … Show more
Keywords:
Breastfeeding initiation, high risk pregnancies
DOI:
10.3233/NPM-161610
Citation:
Journal of Neonatal-Perinatal Medicine
(https://content.iospress.com:443/journals/journal-of-neonatal-perinatal-medicine), vol. 9, no. 4, pp. 401-409, 2016
Price: EUR 27.50
1
2
Next »
Failure to initiate breastfeeding among high risk obstetrical patients
who intended to breastfeed
(https://content.iospress.com:443/articles/journal-of-neonatal-perinatal-medicine/npm1610)
Journal of Neonatal-Perinatal Medicine 9 (2016) 385–392 DOI:10.3233/NPM-161628
IOS Press
385
Original Research
Influence of maternal factors
on the successful outcome of kangaroo
mother care in low birth-weight infants:
A randomized controlled trial
S.N. Lumbanraja
∗Department of Obstetrics and Gynecology, University of Sumatera Utara, Medan, Indonesia
Received 16 March 2016
Revised 29 May 2016
Accepted 24 August 2016
Abstract.
BACKGROUND: Kangaroo mother care (KMC) is associated with positive neonatal outcomes. Studies demonstrated significant influence of maternal factors on the success of applying KMC.
AIM:To determine maternal factors that influence on anthropometric parameters in low birth weight babies that received kangaroo mother care.
METHODS:This is a randomized controlled study that involved low birth weight newborns. We randomly assigned newborns into two groups; a group who received KMC and a group who received conventional care. Maternal factors were recorded. We followed weight, length, and head circumferences of newborns for thirty days.
RESULTS:A total of 40 newborns were included. Weight parameters were significantly higher in the KMC group than the conventional group. From maternal characteristics, only gestational age was found to influence increased head circumference in KMC group (p= 0.035); however, it did not affect the increase in weight or length. Maternal age, parity, education, mode of delivery, fetal sex, and initial Apgar score did not influence growth parameters in either groups.
CONCLUSION:KMC was associated with increased weight gain in LBW infants. Gestational age influences head growth in infants who received KMC.
Keywords: Low birth weight, KMC method, growth parameters
1. Introduction
Low Birth Weight (LBW) remains a major cause of neonatal morbidity and mortality. Around 16% of newborns experience LBW with an incidence of 18
∗Address for correspondence: S.N. Lumbanraja, MD,
Depart-ment of Obstetrics and Gynecology, University of Sumatera Utara, Medan, Indonesia. Tel.: +62 8126536472; E-mail: [email protected].
million annually worldwide. In developing countries, incidence of LBW is two times higher than in devel-oped countries [1]. LBW is associated with many complications such as growth disorders, cognitive disorders, and development of chronic diseases in the elderly [2].
Factors such as maternal age, multigravida, short interpergnancy-intervals, socioeconomic factors, maternal education, and pregnancy weight gain
increase the incidence of LBW [3–5]. Another study showed a 1.2 times increased risk of LBW in women with low socioeconomic status and 1.7 times in women with low education [6]. LBW is also closely linked with maternal height [7]. Mumbare et al. [8] showed that maternal weight <55 kg, maternal height <145 cm, and inadequate antenatal care, were the most influential factors that induce LBW [8]. Taha et al. [9] showed that maternal age and parity had significant effects on birth weight [9]. However, Negi et al. [10] on the other hand showed that primigravid had higher risk of having LBW baby and there was no relationship between maternal age, height and weight with LBW [10]. In Indonesia, Trihardani et al. (2011) showed that the risk factors associated with LBW were maternal body mass index, pregnancy weight gain, and parity, while there was no signifi-cant relationship found between LBW and maternal age, maternal height, frequency of antenatal care, or interpregnancy-interval [11]. Pregnancy before age 20 or over age 35 has tendency to an unmet need of adequate nutrition for fetal growth [12]. In short interpregnancy-intervals, mother does not have enough time between pregnancies to revover nutrient store, either micro- or macronutrient [13].
Keeping LBW infants warm is a crucial point because of the vulnerability to hypothermia which could led to life-threatening infection, apnea or mas-sive bleeding [14]. Incubator is one way to cope with LBW babies, but it impedes early contact and breast feeding [15]. Some invasive procedures in incubator also induce stress in babies, proved by some studies that showed increasing of heart rate and respiratory rate in infants treated in an incubator [16]. As an alter-native, KMC was developed by Martinez and Rey in Bogota (1978), inspired from how marsupials to keep their childern warm [17].
KMC is known to be quite effective in the treat-ment of LBW, in addition of the ease and inexpensive application. It was very important in many remote areas in Indonesia due to the lack of resuscitation facilities [18]. Majority of studies showed KMC had better effects than conventional method, although these were still controversial [19–21]. Pratiwi et al. [22] showed that the birth weight≥1500 gr and age
>10 days related to the success of KMC. Gestational age≥34 weeks, KMC duration≥65 minutes, high
maternal education level (p= 0.408) did not influence the incidence of LBW [22].
As many factors contributed to the successful application of KMC, clinicians should have predicted
neonatal is the most vulnerable period in human life. This study aimed to study the influence of maternal factors on the successful of KMC in LBW.
2. Methods
2.1. Study design
This was an analytical, cohort prospective study that was conducted at Adam Malik General Hospi-tal and Pirngadi HospiHospi-tal, Medan, Indonesia from June to November 2015. Written informed consents were obtained from all parents. This study has been approved by the Ethical Committee of University of Sumatera Utara, Medan, Indonesia.
2.2. Study population
This study enrolled newborn with LBW in this institution. LBW is defined as weight below 2500 g. We randomly assigned the newborns into two groups. In the first group, the newborn was given KMC and in the second group they were cared for in an incubator as the conventional method. We only included babies with birth weight 1000–2500 g, stable hemodynamic status, needed neither oxygen nor continuous intra-venous fluids, and mothers were healthy enough and willing to practice KMC. We also restriced the samples to mothers who did exclusive breast-feeding since breastbreast-feeding is known to influence KMC outcomes. Exclusion criteria were babies with congenital anomalies, severe perinatal complications that required NICU care, experienced a malignancy, metabolic disorders, and cardiovascular disorders.
2.3. Study protocols
The baseline information of maternal and fetal demographics were recorded. Maternal factors included age, gestational age, number of parity, edu-cation, and mode of delivery. We also included fetal demographics such as sex and initial Apgar scores.
S.N. Lumbanraja / Kangaroo care in LBW infants 387
not in KMC, babies were placed in the craddle with bodies covered. This method was conducted for 4–6 hours each day. Babies in both the groups were pro-vided vitamin and mineral supplementation as per the protocol.
The subjects were followed up for 30 days. Every day, anthropometrics were measured. Babies were weighed naked on an electronic weighing scale (GEA). The weighing machine was calibrated daily. The lengths were measured with infantometer (GEA) at birth, day 10, day 20, and day 30. The head cir-cumferences were measured with a standard tape at birth, day 10, day 20, and day 30. All measurements were carried out independently by two investigators who were masked to group assignment of the infants. We take the mean of both measurements. Within the follow up, if there were sucking disorder, breathing disorders, or loss of consciousness, babies were given further interventions, and were excluded from the study.
Infants’ weight was plotted using Fenton’s growth charts. We calculated accurate weight gain velocity with the following formula GV = [1000×(Wn-W1)]: [(Dn-D1)×(Wn+W1)/2] and estimated weight gain
velocity with formula GV [1000×ln (Wn/W1)]:
(Dn-D1). The magnitude of errors were reflected by the percentage of absolute difference with formula 100×(Estimated GV – Accurate GV): Accurate
GV. We also calculated a z-score for weight in www.peditools.org/fenton/2013 at birth and at day 30.
3. Data analysis
Data were analyzed by SPSS (Statistical Product and Service Solutions, Chicago, IL, USA) 22.0 for Windows. Categorical data were expressed as number and continuous data as mean±SD. Chi-square test (Fisher’s exact test) was used to examine the relation between qualitative variables. independent, T-dependent, Pearson correlation were used to evaluate quantitative variables. Significance was determined whenpvalue was <0.05.
4. Results
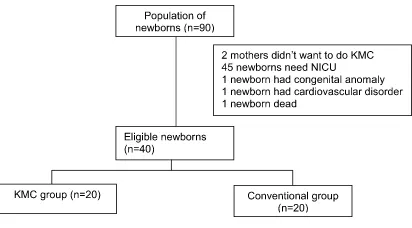
During the period of June 2015-October 2015, ninety infants were born with LBW. Two mothers were not willing to participate in KMC. Some new-borns were excluded from the study, as 45 newnew-borns
Fig. 1. Samples of this study.
needed NICU care, 1 had congenital anomalies, 1 had cardiovascular disorders, and 1 newborn died. Finally, about 40 newborns were eligible in this study. No loss to follow up or withdrawal from the study (Fig. 1).
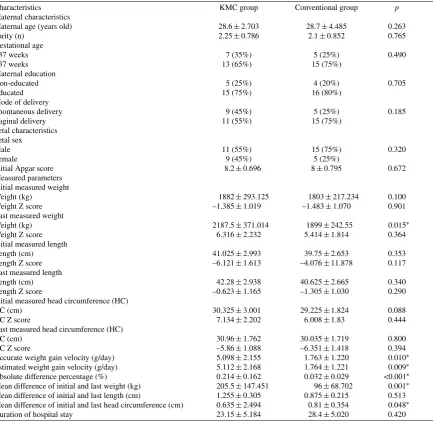
Maternal and fetal demographic characteristics were shown in Table 1. No differences were found between groups in maternal age, parity, gestational age, maternal education, mode of delivery, fetal sex, and Apgar score. The initial measured weight, length, and head circumferences were similar in both groups (p= 0.100; p= 0.353; and p= 0.088, respectively). Last measured weight was signifi-cantly higher in KMC group than conventional group (2187.5±371.04 vs 1899±242.55;p= 0.015). The difference of initial and last weight was also higher in KMC group than conventional group (205.5±147.451 vs 96±68.702; p= 0.001). To ensure this weight parameter, we calculated the weight gain velocity. The accurate weight gain velocity was 5.098±2.155 g/day and the estimated weight gain velocity was 5.112±2.168 g/day. As a result, accurate and estimated weight gain veloc-ityand absolute difference percentage were found higher significantly in KMC group than conventional group (p= 0.01;p= 0.009;p< 0.001), but there were no differences of last measured weight Z score found between both groups (p= 0.364). We also found no differences of last measured length and head cir-cumference Z score between both groups (Fig. 2). Although mean difference of initial and last head circumference (cm) showed a significant difference (p= 0.004), other parameters regarding head circum-ferences show no significant difcircum-ferences. Duration of hospital stay did not differ between conventional and KMC groups (28.4±5.020 vs 23.15±5.184;
p= 0.42).
Table 1
Demographic characteristics of maternal, fetal, and measured parameters
Characteristics KMC group Conventional group p
Maternal characteristics
Maternal age (years old) 28.6±2.703 28.7±4.485 0.263
Parity (n) 2.25±0.786 2.1±0.852 0.765
Gestational age
<37 weeks 7 (35%) 5 (25%) 0.490
>37 weeks 13 (65%) 15 (75%)
Maternal education
Non-educated 5 (25%) 4 (20%) 0.705
Educated 15 (75%) 16 (80%)
Mode of delivery
Spontaneous delivery 9 (45%) 5 (25%) 0.185
Vaginal delivery 11 (55%) 15 (75%)
Fetal characteristics Fetal sex
Male 11 (55%) 15 (75%) 0.320
Female 9 (45%) 5 (25%)
Initial Apgar score 8.2±0.696 8±0.795 0.672
Measured parameters Initial measured weight
Weight (kg) 1882±293.125 1803±217.234 0.100
Weight Z score –1.385±1.019 –1.483±1.070 0.901
Last measured weight
Weight (kg) 2187.5±371.014 1899±242.55 0.015∗
Weight Z score 6.316±2.232 5.414±1.814 0.364
Initial measured length
Length (cm) 41.025±2.993 39.75±2.653 0.353
Length Z score –6.121±1.613 –4.076±11.878 0.117
Last measured length
Length (cm) 42.28±2.938 40.625±2.665 0.340
Length Z score –0.623±1.165 –1.305±1.030 0.290
Initial measured head circumference (HC)
HC (cm) 30.325±3.001 29.225±1.824 0.088
HC Z score 7.134±2.202 6.008±1.83 0.444
Last measured head circumference (HC)
HC (cm) 30.96±1.762 30.035±1.719 0.800
HC Z score –5.86±1.088 –6.351±1.418 0.394
Accurate weight gain velocity (g/day) 5.098±2.155 1.763±1.220 0.010∗
Estimated weight gain velocity (g/day) 5.112±2.168 1.764±1.221 0.009∗
Absolute difference percentage (%) 0.214±0.162 0.032±0.029 <0.001∗
Mean difference of initial and last weight (kg) 205.5±147.451 96±68.702 0.001∗
Mean difference of initial and last length (cm) 1.255±0.305 0.875±0.215 0.513 Mean difference of initial and last head circumference (cm) 0.635±2.494 0.81±0.354 0.048∗
Duration of hospital stay 23.15±5.184 28.4±5.020 0.420
∗Significant difference.
and last head circumference (–0.314±3.746 vs 1.415±1.064;p= 0.035). However, gestational age was not associated with other parameters. There were no differences among maternal age, parity, maternal education, mode of delivery, fetal sex, and initial Apgar scores with accurate weight gain velocity, estimated weight gain velocity, absolute difference percentage, mean differences of initial and last weight, length, and head circumferences (Table 2).
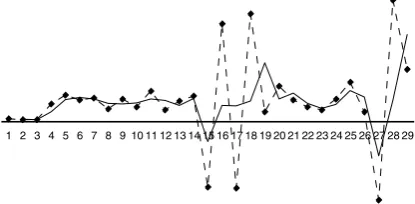
We plotted a mean weight gain graph. Peak weight
the graph showed irregular weight gains, at last day, weight was increased higher than the initial weight assessment (Fig. 3).
5. Discussion
S.N.
Lumbanr
aja
/
Kangar
oo
car
e
in
LBW
infants
389
Table 2
Difference accurate weight gain velocity, estimated weight gain velocity, mean differences of initial and last weight, length, and had circumference between subgroups of maternal and fetal characteristics
Characteristics Accurate weight Estimated weight Absolute difference Mean differences of Mean differences of Mean differences of initial
gain velocity gain velocity percentage initial and last weight initial and last length and last head circumference
Maternal characteristics
Maternal age (years old) r0.309p0.186 r0.309p0.185 r–0.325p0.163 r0.155p0.515 r–0.325p0.163 r0.155p0.515
Parity (n) r0.134p0.574 r0.134p0.572 r–0.417p0.068 r0.350p0.130 r–0.417p0.068 r0.350p0.130
Gestational age
<37 weeks 5.793±1.898 5.810±1.913 0.258±0.156 338.57±137.165 1.286±0.474 –0.314±3.746
>37 weeks 4.680±2.289 4.691±2.304 0.189±0.168 283.85±158.248 1.192±0.236 1.415±1.064
pvalue 0.810 0.812 0.980 0.815 0.271 0.035*
Maternal education
Non educated 3.819±1.223 3.824±1.229 0.111±0.078 208.33±79.352 1.050±0.197 1.600±1.580
Educated 5.604±2.309 5.622±2.324 0.257±0.173 343.57±156.579 1.300±0.351 0.471±2.683
pvalue 0.061 0.08 0.015 0.074 0.487 0.774
Mode of delivery
Vaginal delivery 4.773±1.541 4.782±1.552 0.175±0.1257 281.25±114.697 1.300±0.417 –0.025±3.471
Caesarean section 5.267±2.565 5.283±2.581 0.238±0.186 317.50±172.844 1.175±0.263 1.517±1.048
pvalue 0.059 0.059 0.85 0.346 0.723 0.073
Fetal characteristics Fetal sex
Male 5.408±2.535 5.426±2.549 0.248±0.170 315.27±169.534 1.063±0.1912 1.482±1.155
Female 4.654±1.699 4.664±1.713 0.171±0.153 285.56±129.722 1.422±0.3632 –0.011±3.298
Pvalue 0.069 0.07 0.271 0.142 0.266 0.142
Intial Apgar score r–0.041p0.864 r–0.041p0.865 r0.064p0.788 r–0.141p0.554 r0.292p0.211 r0.018p0.938
Fig. 2. Distribution of Z score for babies’ weight, length, and head circumference (HC) at initial (int) and last day (last) 30 measurement.
Fig. 3. Mean weight gain in KMC group (red line showed the real weight gain and black line showed smoothed curved).
[22] and Rodriguez et al. [23] showed no difference in weight gain with the application of KMC in LBW born either with spontaneous delivery or cesarean section [23].
KMC is a method of maternal-fetal skin to skin contact as a loving incubator that is applied as soon as possible after birth [24]. This method makes mothers and families as providers of biological and psycho-emotional needs for their children [25]. According to WHO guidelines, continuous KMC is indicated in infants with birth weight below 2000 g. Intermittent KMC can also be useful in infants hospitalized in NICU, but still needs further research [26].
The main point of KMC is emphasized at attach-ment between parents and childern. Feldman et al. [27] had successfully demonstrated the positive impact in the relationship between mother and child [27]. Athanasopolou et al. [28] showed that KMC resolved negative moods such as anxiety and depres-sion in mothers [28]. KMC procedure also increased the mothers’ confidence and competence in caring for
effects contribute to the improvement to the growth and development [29].
In this study, an assessment of growth was based on infant’s weight, length, and head circumference, which were the important markers of a child health [30, 31]. Bera et al. [32] showed that in infants receiving KMC, the growth parameters and men-tal development was better than infants who were treated conventionally [32]. Ali et al. [19] showed that infants treated by incubator has higher weight gain per day (19.3 vs.10.4 g,p< 0.001), shorter duration of stay (6.9% vs. 23.2%p= 0.014), lower infection rate (6.9% vs. 23.2% p= 0.014) than babies who applied KMC [19]. Palencia et al. [33] found that the growth in height for age was higher within percentiles weight for age (p= 0.0001). Male gender had a higher weight than females (p= 0.031) [33]. This study was simliar to the study in Indonesia previously. In this study, there we showed that compared to conventional group, last measured weight, difference of initial and last weight, as well as weight gain velocity were higher in KMC group. No differences were found regarding of length and head circumference. Hak-sari (2004) and Rahmayanti [21] in Indonesia also found no difference between weight/age, length/age, head circumference/age in LBW infant treated with KMC and conventional therapy [21]. In the other hand, Rao et al. (2007) conversely showed that infants treated by incubator has a higher weight gain, head circumference (0:49 vs 0.75 cm,p= 0:02), and body length (0.99 vs. 0.7 cm, p= 0.008) compared with infants who applied KMC [20]. It indicated the need to predict which method gives more benefit, KMC or incubator.
We should highlight some factors several authors argued that weight gain should approximate an intrauterine growth rate of 16.8 to 30.7 g/day [31]. In this study, the accurate weight gain velocity was 5.098±2.155 g/day and the estimated weight gain velocity was 5.112±2.168 g/day, which were still far below the recommended growth rate. The Z score of weight was still below expected average. Newborns were still categorized small for gestational age in the end of the study.
S.N. Lumbanraja / Kangaroo care in LBW infants 391
Korraa et al. [34] found that newborns who received KMC had shown lower cerebral blood flow resistive index (p< 0.05) which indicated improved in cerebral blood flow [34]. The influence of immature organ in preterm babies may be considered and this need further research [35]. This marked that KMC is use-ful in all condition regardless of maternal and fetal characteristics.
The strength of this study is the follow-up param-eters that are better than other studies. The better follow-up rate in the KMC group could be due to the active involvement of the mother in the care of her LBW baby. The limitations of this study is the small samples, only conducted in two institutions, and short follow up period. Further large research is needed to ensure these findings.
6. Conclusion
There were no differences of growth parameters between subgroups of maternal and fetal character-istics except the tendency delayed growth of head circumferences in preterm infants.
Acknowledgments
I am greatly appreciate to all observers and my students who directly or indirectly were involved in supporting me to finish this study.
Conflict of interest
The author declared no conflict of interest in this study.
References
[1] Beddek F, Demmouche A, Mai AH, Ghani A, Benali A. Low birth weight in Sidi Bel Abbes region (west of Algeria): Retrospective study of 10008 deliveries. J Blood Disorders Transf 2014;5:1-4.
[2] United Nations Children’s Fund and World Health Orga-nization, Low Birthweight: Country, regional and global estimates. UNICEF, New York, 2004, p. 1.
[3] Kumari R, Guduri GB, Venkateswarulu. A study on mater-nal factors affecting low birth weight in institutiomater-nal deliveries. IOSR J Dental Med Sci 2015;14(1):45-8. [4] Nagargoji MM, Chaudary SS, Deshmukh JS, Gupta SC,
Misra SK. A case control study of risk factors for LBW in
Nagapur city of Maharasthra. Indian J Community Health 2010;22(2):4-7.
[5] Azimul SK, Matin A, Shabnam JH, Shamianaz S, Bannerje M. Maternal factors affecting low birth weight in urban area of Bangladesh. J Dhaka Med Coll 2009;18(1):64-9. [6] Jackson HD, Wei Y, Chen F. Quantitative data analysis
of multiple factors associated with low birth weight in Bibb county, Georgia. J Ga Public Health Assoc 2008;1(1): 24-32.
[7] Agarwal K, Agarwal A, Agrawal VK, Agrawal P, Chaud-hary V. Prevalence and determinants of “low birth weight” among institutional deliveries. Ann Nigerian Med 2011;5:48-52.
[8] Mumbare SS, Maindarkar G, Darade R, Yenge S, Tolani MK, Patole K. Maternal risk factors associated with term low birth weight neonates: A matched-pair case control study. Indian Pediatr 2012;49(6):25-8.
[9] Taha E, A/Gadir MA, Nasralla K, Mukhtar Y, Yousif E, El-Sadig E. Investigation of the risk factors of low birth weight (LBW) in the national ribat university hospital, khartoum. Sudanese J Pub Health 2012;7(4):142-5.
[10] Negi KS, Kandpal SD, Kukreti M. Epidemiological factors affecting low birth weight. JK Science 2006;8(1):31-134. [11] Trihardiani I, Niken P. Risk factors of low birth weight in
the job area of Public Health Center in East Singkawang and North Singkawang. Available from: https://core.ac.uk/down load/files/379/11731574.pdf [Accessed 14th May 2015]. [12] Proverawati A, Maisaroh S. Nutrisi Janin dan Ibu Hamil.
Yogyakarta: Nuha Medika: 2010, pp. 88-148.
[13] Erica RE, Armstrong S. Pencegahan Kematian Ibu Hamil. Jakarta: Binarupa Aksara; 1994, pp. 40-41.
[14] WHO: Kangaroo mother care: A practical guide. World Health Organization: Geneva, Switzerland: 2003. [15] Alisjahbana A, Usman A, Irawati S, Triyati A. Prevention
of hypothermia of low birth infants using kangaroo method. Pediatr Indones 1998;38:205-14.
[16] Whitfield MF, Grunau RE. Behavior, pain perception, and the extremely low-birth weight survivor. Clin Perinatol 2000;27:363-79.
[17] Mart´ınez H, Rey E, Navarrete L, Marquette C. Programa Madre Canguro en el Instituto Materno Infantil de Bogot´a. Primer Encuentro Internacional del Programa Madre Can-guro. Bogot´a: UNICEF; 1990, pp. 21-43.
[18] Whitelaw A, Sleath K. Myth of the marsupial mother: Home care of very low birth weight babies in Bogota, Colombia. Lancet 1985;25(1):1206-8.
[19] Ali SM, Sharma J, Sharma R, Alam S. Kangaroo Mother Care as compared to conventional care for low birth weight babies. Dicle Med J 2009;36(3):155-60.
[20] Rao SP, Udani R, Nanavati R. Kangaroo mother care for low birth weight infants: A randomized controlled trial. Indian Pediatr 2008;45(17):17-23.
[21] Rahmayanti SD. The effect of kangaroo mother care on infants growth, knowledge and attitudes of mother in caring for low birth weight in Cibabat Hospital Cimahi. Avail-able from http://lib.ui.ac.id/file?file=digital/20285372-T %20Siti%20Dewi%20Rahmawati.pdf.
[22] Pratiwi R, Kosim MS, Wijayahadi N. Prognostic factor for success in the Kangaroo Mother Care method for low birth weight babies. Paeditr Indones 2015;15(3):142-6. [23] Rodriguez AN, Nel M, Dippenar H, Prinsloo EA. Good
[24] Charpak N, Ruiz-Pelaez JG, Figueroa CZ, Charpak Y. A randomised controlled trial of Kangaroo mother care: Results of follow up at 1 year of corrected age. Pediatrics 2001;108:1072-9.
[25] Kadam S, Binoy S, Kanbur WA, Mondkar JA, Fernandez A. Feasibility of kangaroo mother care in Mumbai. Indian J Pediatr 2005;72:35-8.
[26] Ludington-Hoe SM, Morgan K, Abouelfettoh A. A clinical guideline for implementation of kangaroo care with prema-ture infants of 30 or more weeks’ postmenstrual age. Adv Neonatal Care 2008;8:S3-S23.
[27] Feldman R, Eidelman AI, Sirota L, Weller A. Comparison of skin-to-skin (kangaroo) and traditional care: Parent-ing outcomes and preterm infant development. Pediatrics 2002;110(1):1-3.
[28] Athanasopolou E, Fox JRE. Effects of kangaroo mother care on maternal mood and interaction patterns between parents and their preterm, low birth weight infants: A systematic review. Infant Mental Health J 2014;35(3):245-62. [29] Tessier R, Cristo M, Velez S, Giron M, Figueroa de Calume
Z. Kangaroo mother care and the bonding hypothesis. Kan-garoo mother care and the bonding hypothesis. Pediatrics 1998;102:17-23.
[30] Kaushal SK, Misra SK, Gupta SC, Singh R. A study of maternal factors and birth weight in a border district of uttar pradesh: A hospital based study. Indian J Community Health 2012;24(2):86-9.
[31] Weller A, Rozin A, Goldstein A, et al. Longitudinal assess-ment of pituitarythyroid axis and andrenal function in preterm infants raised by “kangaroo mother care”. Horm Res 2002;57:22-6.
[32] Bera A, Ghosh J, Singh AK, Hazra A, Mukherjee S, Mukherjee R. Effect of kangaroo mother care on growth and development of low birthweight babies up to 12 months of age: A controlled clinical trial. Acta Paediatr 2014;103(6): 643-50.
[33] Palencia D, Mendoza CJ, Torres J, Echandia CA. Kangaroo mother program: Physical growth and morbidity in a cohort of children, followed from 40 weeks of postconceptional age until first year. Colombia Medica 2009;40(3):292-9. [34] Korraa AA, El Nagger AA, Mohamed RA, Helmy NM.
Impact of kangaroo mother care on cerebral blood flow of preterm infants. Ital J Pediatr 2014;40:83.
Author Index Volume 9 (2016)
Abdallah, C., see Ismawan, J.M. (3) 321–323 Abdel Al, H., see El Shemi, M.S. (1) 73–82 Abdelgadir, D., see Elmekkawi, A. (4) 363–370 AbdelRahman, A.O., see El Shemi, M.S. (1) 73–82 Abo-Lila, R., see Elbahtiti, A. (2) 179–185 Abouda, H.S., see Kehila, M. (2) 127–131 Adam, S., see Browne, P.C. (2) 217–222 Adam, S., see Latif, E. (3) 325–331 Adcock, D., see Teruya, M. (2) 139–143 Adinnu, K.M., see Nnebue, C.C. (3) 303–312 Aditya, I., V. Tat, A. Sawana, A. Mohamed, R. Tuffner
and T. Mondal, Use of Doppler velocimetry in diagnosis and prognosis of intrauterine growth restriction (IUGR): A Review (2) 117–126 Ahmad, A., T. Mondal and B. Klein, Atrial arrhythmia
after newborn eye exam, to caffeine or not to caf-feine? (4) 427–432
Ahmadzia, H.K., S.M. Thomas, A.P. Murtha, R.P. He-ine and L.R. Brancazio, Obstetric hemorrhage survey: Attitudes and practices of maternal-fetal medicine fellows (2) 133–137
Al Hail, M., see Al Omar, S. (3) 251–259
Al Omar, S., H. Salama, M. Al Hail, H. Al Rifai, M. Bunahia, W. El kasem, F.J. Siddiqui, M. Dilawar, H. Yassin, F. Masud, A. Mohamed and A. Man-sour, Effect of early adjunctive use of oral silde-nafi l and inhaled nitric oxide on the outcome of pulmonary hypertension in newborn infants. A feasibility study (3) 251–259
Al Rifai, H., see Al Omar, S. (3) 251–259 Al-Hendy, A., see Latif, E. (3) 325–331 Allred, E.N., see Singh, R. (2) 159–170 Alpan, G., see Feldman, A. (3) 295–302 Al-Sawan, R., see Elbahtiti, A. (2) 179–185 Aly, N.Y., see Elbahtiti, A. (2) 179–185 Anyanwu, B.C., see Nnebue, C.C. (3) 303–312 Aranda, J.V., see Ibrahim, Z.H. (4) 341–348 Arnold, C., see Birenbaum, H.J. (2) 187–194 August, D. and Y. Kandasamy, Signifi cance of
ante-natal glucocorticoid exposure for pressure injury prevalence in neonates (1) 23–29
Ayala-Ramírez, P., T. Buitrago, A. Poveda, J.L. Ro-dríguez, M. Olaya-C and R. García-Robles, Increased tissue factor and thrombomodulin expression and histopathological changes in placentas of pregnancies with preeclampsia (1) 31–39
Bader, M.Y., see Kylat, R.I. (3) 313–316 Badr, M., see Browne, P.C. (2) 217–222 Baki, S.A., see Ibrahim, Z.H. (4) 341–348
Bapat, R., R. McClead, E. Shepherd, G. Ryshen and T. Bartman, Challenges, successes and opportuni-ties for reducing readmissions in a referral-based children’s hospital NICU (4) 433–440
Bartholomew, A., see Kylat, R.I. (3) 313–316 Bartman, T., see Bapat, R. (4) 433–440 Bas¸tug˘, O., see Korkmaz, L. (4) 349–356 Benítez, P.R., see Nicolás, C. (1) 41–48 Bernal, J.E., see Olaya-C, M. (1) 49–57 Berry, A., see Chawla, S. (3) 291–293 Berwal, A., see Nagaraj, N. (4) 417–421 Berwal, P.K., see Nagaraj, N. (4) 417–421 Bhambhani, K., see Chawla, S. (3) 291–293 Biberoglu, E., see Daglar, K. (3) 279–284
Birenbaum, H.J., E.R. Pfoh, S. Helou, M.A. Pane, G.A. Marinkovich, A. Dentry, H.-C. Yeh, L. Up-degraff, C. Arnold, S. Liverman and H. Cawman, Chronic lung disease in very low birth weight in-fants: Persistence and improvement of a quality improvement process in a tertiary level neonatal intensive care unit (2) 187–194
Brancazio, L.R., see Ahmadzia, H.K. (2) 133–137 Bronshtein, V., see Ibrahim, Z.H. (4) 341–348 Brooks, C.R., see Browne, P.C. (2) 217–222 Browne, P.C., S. Adam, M. Badr, C.R. Brooks, J.
Ed-wards, P. Walker, S. Mohamed and A.R. Gregg, Prenatal diagnosis of sub-microscopic partial tri-somy 10q using chromosomal microarray analy-sis in a phenotypically abnormal fetus with nor-mal karyotype (2) 217–222
Browne, P.C., see Latif, E. (3) 325–331
1934-5798/16/$35.00 © 2016 – IOS Press and the authors. All rights reserved
Journal of Neonatal-Perinatal Medicine 9 (2016) 441–446 441 IOS Press
Buitrago, T., see Ayala-Ramírez, P. (1) 31–39 Bunahia, M., see Al Omar, S. (3) 251–259
Campbell, W., see Stirling, K.M. (2) 201–209 Canencia, L.M., see Nicolás, C. (1) 41–48 Cannell, J., see Latif, E. (3) 325–331
Cawman, H., see Birenbaum, H.J. (2) 187–194 Chaiwiriyawong, P., see Nakwan, N. (3) 243–250 Chanoufi , M.B., see Kehila, M. (2) 127–131 Chari, G., see Ibrahim, Z.H. (4) 341–348
Chawla, S., F. Elbakoush, G. Natarajan, M. Dwaihy, A. Berry, Y. Ravindranath, K. Bhambhani and S.B. Narayan, Cord blood lead level in an urban inner-city hospital (3) 291–293
Cheong, S.M., S. Totsu, H. Nakanishi, A. Uchiyama and S. Kusuda, Outcomes of peripherally in-serted double lumen central catheter in very low birth weight infants (1) 99–105
Cheour, H., see Kehila, M. (2) 127–131 Choudhury, J., see Elmekkawi, A. (4) 363–370 Clive, B., G. Corsten, L.S. Penney, M. Van den Hof
and W. El-Naggar, Severe laryngeal stenosis in newly born twins with 22q11.2 deletion syn-drome: A case report (2) 223–226
Cordero, L., R. Oza-Frank, M. Moore-Clingenpeel, M.B. Landon and C.A. Nankervis, Failure to ini-tiate breastfeeding among high risk obstetrical patients who intended to breastfeed (4) 401–409 Corsten, G., see Clive, B. (2) 223–226
Cracco, J., see Ibrahim, Z.H. (4) 341–348 Cramer, N., see Kylat, R.I. (3) 313–316
Daar, G., see Korkmaz, L. (4) 349–356
Daglar, K., A. Tokmak, A. Kirbas, O. Kara, E. Bib-eroglu, D. Uygur and N. Danisman, Anterior placenta previa is associated with increased um-bilical cord blood hematocrit concentrations (3) 279–284
Daglar, K., see Türkmen, G.G. (4) 411–415 Danis¸man, N., see Türkmen, G.G. (4) 411–415 Danisman, N., see Daglar, K. (3) 279–284 Davis, N.L., see Pickering, A. (2) 171–178 de A. Lopes, J.M., see Rodrigues, M.A. (2) 195–200 De Benedictis, B., see Feldman, A. (3) 295–302 de Carvalho, P.N., see Rodrigues, M.A. (2) 195–200 Dentry, A., see Birenbaum, H.J. (2) 187–194 DeRoo, S.E.S., K.M. Lumpkins and D.E.
El-Metwal-ly, Scrotoschisis in a neonate with meconium peritonitis and periorchitis (1) 107–112
Diamond, M.P., see Latif, E. (3) 325–331
Dietze, T.R., F.F. Rose and T.A. Moore, Maternal variables associated with physiologic stress and perinatal complications in preterm infants (3) 271–277
Dilawar, M., see Al Omar, S. (3) 251–259 Donofrio, M.T., see Talemal, L. (3) 317–320 Dossett, E., see Stohl, H. (1) 1–5
Dunn, M., see Elmekkawi, A. (4) 363–370 Duru, C.B., see Nnebue, C.C. (3) 303–312 Dwaihy, M., see Chawla, S. (3) 291–293
Edwards, J., see Browne, P.C. (2) 217–222 El kasem, W., see Al Omar, S. (3) 251–259
El Shemi, M.S., M.H. Mohamed, A.O. AbdelRah-man, H. Abdel Al and N.M. Ramadan, Effect of intrauterine growth pattern on serum visfatin concentrations in full-term infants at birth and at 6 months of life (1) 73–82
Elbahtiti, A., N.Y. Aly, R. Abo-Lila and R. Al-Sawan, Therapeutic hypothermia for infants with hypox-ic ischemhypox-ic encephalopathy: A fi ve years’ single center experience in Kuwait (2) 179–185 Elbakoush, F., see Chawla, S. (3) 291–293 Eldin, K., see Teruya, M. (2) 139–143
El-Kafrawy, U. and R.J. Taylor, Optimizing care of ventilated infants by improving weighing accu-racy on incubator scales (4) 377–383
Elmekkawi, A., D. Abdelgadir, J. Van Dyk, J. Choud-hury and M. Dunn, Use of naloxone to minimize extubation failure after premedication for IN-SURE procedure in preterm neonates (4) 363– 370
El-Metwally, D.E., see DeRoo, S.E.S. (1) 107–112 El-Naggar, W., see Clive, B. (2) 223–226
Fairchild, K., see McClure, C. (4) 357–362
Feldman, A., B. De Benedictis, G. Alpan, E.F. La Gamma and J. Kase, Morbidity and mortality as-sociated with rewarming hypothermic very low birth weight infants (3) 295–302
Fernández, M.S., see Nicolás, C. (1) 41–48
Fernández-Fructuoso, J.R., S. Gil-Sánchez, E. Gómez-Santos, J.M. Lloreda-García, S. Sevilla-Denia and J.L. Leante-Castellanos, Neonatal Behc¸et’s disease with Raynaud phenomenon (4) 423–425 Finch, C., see Kiger, J.R. (3) 285–290
Frountzas, M., see Prodromidou, A. (1) 59–65
Galvis, S.H., see Olaya-C, M. (1) 49–57
Author Index Volume 9 (2016) 443
Gil-Sánchez, S., see Fernández-Fructuoso, J.R. (4) 423–425
Gomes Júnior, S., see Rodrigues, M.A. (2) 195–200 Gómez-Santos, E., see Fernández-Fructuoso, J.R. (4)
423–425
Gregg, A.R., see Browne, P.C. (2) 217–222 Grzybowski, M., see Singh, R. (2) 159–170 Gulati, A., see Stefanov, G. (2) 145–152 Günes¸, T., see Korkmaz, L. (4) 349–356 Gutierrez, S., see Olaya-C, M. (1) 49–57
Heine, R.P., see Ahmadzia, H.K. (2) 133–137 Helou, S., see Birenbaum, H.J. (2) 187–194 Hoyen, C., see Ruangkit, C. (1) 83–90 Hui, S.R., see Teruya, M. (2) 139–143 Hussain, N., see Stirling, K.M. (2) 201–209 Hussein, G., see Ramadan, M.K. (1) 15–22
Ibrahim, Z.H., G. Chari, S.A. Baki, V. Bronshtein, M.R. Kim, J. Weedon, J. Cracco and J.V. Aranda, Wireless multichannel electroencephalography in the newborn (4) 341–348
Ifeadike, C.O., see Nnebue, C.C. (3) 303–312 Ismawan, J.M. and C. Abdallah, Retained surfactant
catheter and pneumothorax in a premature neo-nate (3) 321–323
Jang, S.Y., see McClure, C. (4) 357–362 Johnson, S.L., see Morrison, A.K. (2) 227–231 Jorge, A.T., see Nicolás, C. (1) 41–48
Kandasamy, Y., see August, D. (1) 23–29 Kara, O., see Daglar, K. (3) 279–284
Karakash, S.D., N. Tschankoshvili, J. Weedon, R.M. Schwartz, C. Kirschbaum and H. Minkoff, Hy-pocortisolism and preterm birth (4) 333–339 Kase, J., see Feldman, A. (3) 295–302
Katikaneni, L., see Kiger, J.R. (3) 285–290 Kawato, H., see Miyata, M. (3) 261–269
Kehila, M., H.S. Abouda, K. Sahbi, H. Cheour and M.B. Chanoufi , Ultrasound cervical length mea-surement in prediction of labor induction out-come (2) 127–131
Kiger, J.R., S.N. Taylor, C.L. Wagner, C. Finch and L. Katikaneni, Preterm infant body composition cannot be accurately determined by weight and length (3) 285–290
Kim, M.R., see Ibrahim, Z.H. (4) 341–348 Kirbas, A., see Daglar, K. (3) 279–284 Kirbas, A., see Türkmen, G.G. (4) 411–415 Kirschbaum, C., see Karakash, S.D. (4) 333–339
Klein, B., see Ahmad, A. (4) 427–432 Kobayashi, M., see Miyata, M. (3) 261–269 Kohm, A.D., see Stohl, H. (1) 1–5
Korkmaz, L., O. Bas¸tug˘, G. Daar, S. Korkut, A. Öz-demir, M.A. Öztürk, T. Günes¸ and S. Kurtog˘lu, The effects of thyroid function on retinopathy of prematurity (4) 349–356
Korkut, S., see Korkmaz, L. (4) 349–356 Kotani, M., see Miyata, M. (3) 261–269 Kurtog˘lu, S., see Korkmaz, L. (4) 349–356
Kurtom, M.D.W., R.N.D. Quast, L. Worley and M.D.D.G. Oelberg, Incorrect umbilical vein catheterization is associated with severe periven-tricular hemorrhages and mortality in extremely premature newborns (1) 67–72
Kurtz, D., see Sherman, T.I. (1) 7–14 Kusuda, S., see Cheong, S.M. (1) 99–105
Kylat, R.I., A. Bartholomew, N. Cramer and M.Y. Bader, Neonatal listeriosis: Uncommon or mis-diagnosed? (3) 313–316
La Gamma, E.F., see Feldman, A. (3) 295–302 Lande, B.J., see Torres, E.B. (1) 113–115 Landon, M.B., see Cordero, L. (4) 401–409
Latif, E., S. Adam, B. Rungruang, A. Al-Hendy, M.P. Diamond, E. Rotem, J. Cannell and P.C. Browne, Use of uterine artery embolization to prevent pe-ripartum hemorrhage of placental abruption with fetal demise & severe DIC (3) 325–331 Leante-Castellanos, J.L., see Fernández-Fructuoso,
J.R. (4) 423–425
LeGallo, R., see Morrison, A.K. (2) 227–231 Leviton, A., see Singh, R. (2) 159–170 Liverman, S., see Birenbaum, H.J. (2) 187–194 Lloreda-García, J.M., see Fernández-Fructuoso, J.R.
(4) 423–425
Lumbanraja, S.N., Infl uence of maternal factors on the successful outcome of kangaroo mother care in low birth-weight infants: A randomized con-trolled trial (4) 385–392
Lumpkins, K.M., see DeRoo, S.E.S. (1) 107–112 Luna, M.S., see Nicolás, C. (1) 41–48
Mansour, A., see Al Omar, S. (3) 251–259 Manuel, V., see McConaghy, S. (1) 91–97 Marc-Aurele, K.L., see Studer, E.M. (4) 393–400 Marinkovich, G.A., see Birenbaum, H.J. (2) 187–194 Martin, C.R., see Singh, R. (2) 159–170
McClure, C., S.Y. Jang and K. Fairchild, Alarms, oxy-gen saturations, and SpO2 averaging time in the NICU (4) 357–362
McConaghy, S., V. Manuel, S. Nagji and R.K. Ohls, Epsilon globin gene expression in developing human fetal tissues (1) 91–97
McNelis, K. and S. Viswanathan, Effects of parenteral phosphorus dose restriction in preterm infants (2) 153–158
Mehta, A., see Mehta, Y. (4) 371–376
Mehta, Y., J. Shetye, R. Nanavati and A. Mehta, Phys-iological effects of a single chest physiotherapy session in mechanically ventilated and extubated preterm neonates (4) 371–376
Mercurio, C., see Nicolás, C. (1) 41–48 Minkoff, H., see Karakash, S.D. (4) 333–339 Mirza, F.G., see Ramadan, M.K. (1) 15–22
Miyata, M., K. Toyoshima, H. Yoda, M. Murase, H. Kawato, K. Yamamoto, K. Tanaka, M. Kotani and M. Kobayashi, Extensive use of vasodilator agents and functional echocardiography to moni-tor extremely-low-birth-weight infants in Japan (3) 261–269
Mohamed, A., see Aditya, I. (2) 117–126 Mohamed, A., see Al Omar, S. (3) 251–259 Mohamed, M.H., see El Shemi, M.S. (1) 73–82 Mohamed, S., see Browne, P.C. (2) 217–222 Mondal, T., see Aditya, I. (2) 117–126 Mondal, T., see Ahmad, A. (4) 427–432 Moore, T.A., see Dietze, T.R. (3) 271–277
Moore-Clingenpeel, M., see Cordero, L. (4) 401–409 Morrison, A.K., M. Patel, S.L. Johnson, R. LeGallo,
W.G. Teague and B. Vergales, Pulmonary inter-stitial glycogenosis in a patient with trisomy 21 (2) 227–231
Moya, F., see Sherman, T.I. (1) 7–14
Müller, M.J., T. Paul and S. Seeliger, Necrotizing en-terocolitis in premature infants and newborns (3) 233–242
Murase, M., see Miyata, M. (3) 261–269 Murtha, A.P., see Ahmadzia, H.K. (2) 133–137
Nagaraj, N., P.K. Berwal, A. Srinivas and A. Berwal, A study of acute kidney injury in hospitalized preterm neonates in NICU (4) 417–421
Nagji, S., see McConaghy, S. (1) 91–97 Nakanishi, H., see Cheong, S.M. (1) 99–105
Nakwan, N. and P. Chaiwiriyawong, An international survey on persistent pulmonary hypertension of the newborn: A need for an evidence-based man-agement (3) 243–250
Nanavati, R., see Mehta, Y. (4) 371–376
Nankervis, C.A., see Cordero, L. (4) 401–409 Narayan, S.B., see Chawla, S. (3) 291–293 Natarajan, G., see Chawla, S. (3) 291–293
Nicolás, C., P.R. Benítez, M.O.A. Riaño, L.M. Ca-nencia, C. Mercurio, M.S. Fernández, M.S. Luna and A.T. Jorge, Preeclampsia: Long-term effects on pediatric disability (1) 41–48
Nnebue, C.C., C.B. Duru, K.A. Uwakwe, C.O. Ifea-dike, B.C. Anyanwu, K.M. Adinnu, P.O. Nwane-ri and I.J. Ufoh, Neonatal care – what do mothers in a rural Nigerian community know and prac-tice? (3) 303–312
Nwaneri, P.O., see Nnebue, C.C. (3) 303–312
Oelberg, M.D.D.G., see Kurtom, M.D.W. (1) 67–72 Ohls, R.K., see McConaghy, S. (1) 91–97
Olaya-C, M., J. Salcedo-Betancourt, S.H. Galvis, A.M. Ortiz, S. Gutierrez and J.E. Bernal, Um-bilical cord and preeclampsia (1) 49–57 Olaya-C, M., see Ayala-Ramírez, P. (1) 31–39 Ortiz, A.M., see Olaya-C, M. (1) 49–57 Oza-Frank, R., see Cordero, L. (4) 401–409 Özdemir, A., see Korkmaz, L. (4) 349–356 Öztürk, M.A., see Korkmaz, L. (4) 349–356
Pais, G., see Stefanov, G. (2) 145–152 Pane, M.A., see Birenbaum, H.J. (2) 187–194 Patel, M., see Morrison, A.K. (2) 227–231 Paul, T., see Müller, M.J. (3) 233–242 Penney, L.S., see Clive, B. (2) 223–226 Perez, J.A., see Smith, D.P. (2) 211–215 Pergialiotis, V., see Prodromidou, A. (1) 59–65 Perrea, D., see Prodromidou, A. (1) 59–65 Pfoh, E.R., see Birenbaum, H.J. (2) 187–194 Pickering, A., R. White and N.L. Davis, Routine fecal
occult blood testing does not predict necrotizing enterocolitis in very low birth weight neonates (2) 171–178
Poveda, A., see Ayala-Ramírez, P. (1) 31–39 Prodromidou, A., M. Frountzas, D. Perrea, G.D.
Vla-chos and V. Pergialiotis, The impact of obesity on cervical cerclage effi cacy: A systematic re-view of the literature (1) 59–65
Puppala, B.L., see Stefanov, G. (2) 145–152
Quast, R.N.D., see Kurtom, M.D.W. (1) 67–72
Rajab, M., see Ramadan, M.K. (1) 15–22
Author Index Volume 9 (2016) 445
Ramadan, N.M., see El Shemi, M.S. (1) 73–82 Ravindranath, Y., see Chawla, S. (3) 291–293 Riaño, M.O.A., see Nicolás, C. (1) 41–48
Rodrigues, M.A., P.N. de Carvalho, S. Gomes Júnior, F.F. Martins and J.M. de A. Lopes, Perinatal out-come comparing triplets and singleton births at a reference maternity hospital (2) 195–200 Rodríguez, J.L., see Ayala-Ramírez, P. (1) 31–39 Rose, F.F., see Dietze, T.R. (3) 271–277 Rotem, E., see Latif, E. (3) 325–331
Ruangkit, C., A. Satpute, B.A. Vogt, C. Hoyen and S. Viswanathan, Incidence and risk factors of uri-nary tract infection in very low birth weight in-fants (1) 83–90
Rungruang, B., see Latif, E. (3) 325–331 Ryshen, G., see Bapat, R. (4) 433–440
Sahbi, K., see Kehila, M. (2) 127–131 Saheb, W., see Ramadan, M.K. (1) 15–22 Salama, H., see Al Omar, S. (3) 251–259
Salcedo-Betancourt, J., see Olaya-C, M. (1) 49–57 Sanders, M.M., see Stirling, K.M. (2) 201–209 Santolaya-Forgas, J., see Torres, E.B. (1) 113–115 Satpute, A., see Ruangkit, C. (1) 83–90
Sawana, A., see Aditya, I. (2) 117–126
Schwartz, R.M., see Karakash, S.D. (4) 333–339 Seeliger, S., see Müller, M.J. (3) 233–242
Sevilla-Denia, S., see Fernández-Fructuoso, J.R. (4) 423–425
Shaffer, T.H., see Sherman, T.I. (1) 7–14 Shah, B., see Singh, R. (2) 159–170 Shepherd, E., see Bapat, R. (4) 433–440
Sherman, T.I., F. Moya, P.D. Simmons, D. Kurtz and T.H. Shaffer, Parental preferences regarding ad-ministration of an animal-derived versus a syn-thetic medication to newborn infants (1) 7–14 Shetye, J., see Mehta, Y. (4) 371–376
Siddiqui F.J., see Al Omar, S. (3) 251–259 Simmons, P.D., see Sherman, T.I. (1) 7–14
Singh, R., B. Shah, E.N. Allred, M. Grzybowski, C.R. Martin and A. Leviton for the ELGAN Study co-investigators, The antecedents and correlates of necrotizing enterocolitis and spontaneous intes-tinal perforation among infants born before the 28th week of gestation (2) 159–170
Smith, D.P. and J.A. Perez, Noninvasive inhaled ni-tric oxide for persistent pulmonary hypertension of the newborn: A single center experience (2) 211–215
Soundar, E., see Teruya, M. (2) 139–143 Srinivas, A., see Nagaraj, N. (4) 417–421
Stefanov, G., B.L. Puppala, G. Pais and A. Gulati, En-dothelin-1 levels and renal function in newborns of various gestational ages (2) 145–152
Stirling, K.M., N. Hussain, M.M. Sanders and W. Campbell, Association between maternal genital mycoplasma colonization and histologic chorio-amnionitis in preterm births (2) 201–209 Stohl, H., A.D. Kohm and E. Dossett, A rock and a
hard place: The selective serotonin reuptake in-hibitor dilemmas in addressing perinatal mood and anxiety disorders (1) 1–5
Studer, E.M. and K.L. Marc-Aurele, Lost in explana-tion: Lessons learned from audio-recordings and surveys of the antenatal consultation (4) 393–400
Talemal, L. and M.T. Donofrio, Hemodynamic con-sequences of a restrictive ductus arteriosus and foramen ovale in fetal transposition of the great arteries (3) 317–320
Tanaka, K., see Miyata, M. (3) 261–269 Tat, V., see Aditya, I. (2) 117–126
Taylor, R.J., see El-Kafrawy, U. (4) 377–383 Taylor, S.N., see Kiger, J.R. (3) 285–290 Teague, W.G., see Morrison, A.K. (2) 227–231 Teruya, J., see Teruya, M. (2) 139–143
Teruya, M., E. Soundar, S.R. Hui, K. Eldin, D. Adcock and J. Teruya, PIVKA-II correlates with INR but not protein C or protein S concentrations in cord blood among newborns (2) 139–143
Thomas, S.M., see Ahmadzia, H.K. (2) 133–137 Timur, H., see Türkmen, G.G. (4) 411–415 Tokmak, A., see Daglar, K. (3) 279–284 Tokmak, A., see Türkmen, G.G. (4) 411–415 Torres, E.B., B.J. Lande and J. Santolaya-Forgas,
A novel analytical approach to sensing fi tness bracelets for a personalized perinatal care: A case report (1) 113–115
Totsu, S., see Cheong, S.M. (1) 99–105 Toyoshima, K., see Miyata, M. (3) 261–269 Tschankoshvili, N., see Karakash, S.D. (4) 333–339 Tuffner, R., see Aditya, I. (2) 117–126
Türkmen, G.G., H. Timur, Z. Yilmaz, A. Kirbas, K. Daglar, A. Tokmak, D. Uygur and N. Danis¸man, Effect of intrahepatic cholestasis of pregnancy on maternal serum screening tests (4) 411–415
Uygur, D., see Daglar, K. (3) 279–284 Uygur, D., see Türkmen, G.G. (4) 411–415
Van den Hof, M., see Clive, B. (2) 223–226 Van Dyk, J., see Elmekkawi, A. (4) 363–370 Vergales, B., see Morrison, A.K. (2) 227–231 Viswanathan, S., see McNelis, K. (2) 153–158 Viswanathan, S., see Ruangkit, C. (1) 83–90 Vlachos, G.D., see Prodromidou, A. (1) 59–65 Vogt, B.A., see Ruangkit, C. (1) 83–90
Wagner, C.L., see Kiger, J.R. (3) 285–290 Walker, P., see Browne, P.C. (2) 217–222
Weedon, J., see Ibrahim, Z.H. (4) 341–348 Weedon, J., see Karakash, S.D. (4) 333–339 White, R., see Pickering, A. (2) 171–178 Worley, L., see Kurtom, M.D.W. (1) 67–72