HIV-AIDS Policy and Health System in Indonesia: A Document Review
By: M. Suharni; Ignatius Praptoraharjo; Iko Safika; Satiti Retno P; Eviana Hapsari Dewi; Ignatius Hersumpana;Eunice Priscilla S; Sisilya Bolilanga
Design & layout: Pustaka Sempu
National Library: Catalog under Issuance
HIV-AIDS Policy and Health System in Indonesia: A Document Review/ M. Suharni; Ignatius Praptoraharjo; Iko Safika; Satiti Retno P; Eviana Hapsari Dewi; Ignatius Hersumpana;Eunice Priscilla S; Sisilya Bolilanga / Yogyakarta: Center for Health Policy and Management (CHPM) Faculty of Medicine, Universitas Gadjah Mada (Publishing affiliation with INSISTPress). 17x25cm; 161pages
First edition, September 2016 ISBN: 978-602-0857-25-1
1. Desk Review 2. HIV and AIDS 3. Health System 4. Policy 5. Response I. HIV-AIDS Policy and Health System in Indonesia : A Document Review
Written with the support of the Australian government through a grant from the Department of Foreign Affairs and Trade (DFAT) to the Center for Policy and Health Management (CHPM), Faculty of Medicine, Universitas Gadjah Mada. This publication does not represent the views of either the Government of Australia or the Government of Indonesia.
All rights reserved.
Any part of the report may be used, reprinted, reproduced, quoted, or cited in any manner through proper citation and for the purpose of community education, not for commercial interests.
For more information please contact the Center for Policy and Health Management (CHPM), Faculty of Medicine, Universitas Gadjah Mada.
Suggested citation:
CHPM. 2016. HIV-AIDS Policy and Health System in Indonesia: A Document Review. Yogyakarta: CHPM UGM
Copyright © 2016 by
Foreword - DFAT
The Australia Government through its Australia Indonesia Partnership for HIV (AIPH) program supports Indonesia’s national goals of preventing and limiting the spread of HIV, improving the quality of life of people living with HIV, and alleviating the socio-economic impacts of the epidemic.
The present study was conducted by Universitas Gadjah Mada to examine the integration HIV and AIDS into the National Health System. It examined how HIV and AIDS program, which is mostly centrally driven, funded by donors funding and delivered in parallel to the existing health system, can be integrated into the system for its sustainability.
The study assessed the level of integration of HIV and AIDS program into the health system at the national, provincial and district/municipality levels in eight provinces in Indonesia i.e. North Sumatra, DKI Jakarta, East Java, Bali, South Sulawesi, West Papua, Papua, and West Nusa Tenggara.
The study echoes the notion that integration is an organisational framework that can strategically improve a program’s effectiveness, efficiency and sustainability. However, the effort to reach the expected integration level is highly dependent on various contexts within which AIDS control and the health system operate. Political commitment from local leaders, the local economy, laws and regulations that are not always in favour of HIV and AIDS control and the interaction among stakeholders in the health system and HIV and AIDS control determine the level of integration in study locations.
Evidence-based policy is strongly supported by the Australian Government in its partnership with the Government of Indonesia. It is highly expected that this study will assist the Government of Indonesia to further integrate HIV and AIDS programs into the health system and develop a sustainable strategy to support HIV and AIDS control.
James Gilling
Minister, Development Cooperation
Foreword - KPAN
The development of policies and programs for effective HIV and AIDS control has been ongoing for about 30 years. In order to provide solid evidence and basis for policy development of HIV and AIDS in Indonesia, these policies and programs need to be thoroughly examined. Changes in the epidemic situation, in government systems, the global situation and initiatives, the involvement of civil society organisations, and groups affected by HIV and AIDS are various factors that influence the evolution of policy and programs on HIV and AIDS over the years.
In the National Strategy and Action Plan for AIDS Response in Indonesia 2015-2019, the National AIDS Commission or Komisi Penanggulangan AIDS Nasional (KPAN) has emphasized the important contribution of scientific research to the development of evidence-based policies and programs of HIV and AIDS in the future. The KPAN strongly supports the document review on HIV and AIDS policies and programs conducted by the Center for Health Policy and Management, Faculty of Medicine, University of Gadjah Mada (Pusat Kebijakan dan Manajemen Kesehatan, Fakultas Kedokteran, Universitas Gadjah Mada – PKMK UGM). The study was supported by the Australia-Indonesia Partnership for HIV (AIPH) Program and Australian Department of Foreign Affairs and Trade (DFAT). Our study is a policy study aims to provide an understanding of the context, process, and substance of the existing policies and at the same time to map the gaps in the implementation of the policies. Therefore, KPAN looks forward to receiving the recommendations from this study for further analytical review and subsequent use by the governments, civil society organisations, program beneficiaries, and donor agencies or international development partner organisations in the development of HIV and AIDS programs within an underpinning and resilient health system. Furthermore, the results of this study may be used to promote improvement of the existing policies and programs while at the same time address various challenges and opportunities in the implementation of HIV and AIDS policies in Indonesia. Jakarta, October 2015
Table of Content
Foreword - DFAT ... 3
Foreword - KPAN ... 4
Table of Content ... 5
List of Tables and Figures ... 8
List of Acronyms ... 9
Executive Summary ... 14
INTRODUCTION ... 17
1.1. Rationale ... 1 7 1.2. Methods ... 20
1.2.1. Document Review ... 20
1.2.2. Field Visit: Interviews and Group Discussions ... 20
1.3. Study Period ... 21
1.4. Study Limitations ... 21
1.5. Outline of the Report ... 22
DYNAMICS OF HIV AND AIDS EPIDEMIOLOGY AND RESPONSE ... 23
2.1. HIV and AIDS epidemiology in Indonesia ... 23
2.2. Epidemic Response ... 26
2.2.1. Period of 1987 to 1996 ... 27
2.2.2. Period of 1997–2007 ... 29
2.2.3. Period of 2007–2013 ... 33
2.3. HIV and AIDS epidemy in Five Selected Provinces ... 37
2.3.1. North Sumatra ... 37
2.3.2. East Java ... 37
2.3.3. Bali ... 38
2.3.4. South Sulawesi ... 39
2.3.5. Papua ... 40
EVOLUTION OF HIV AND AIDS RESPONSE POLICIES IN INDONESIA ... 45
49
3.3. Lessons Learned from the HIV and AIDS Program Implementation ... 53
POLICIES AND PROGRAMS ... 60
ON HIV AND AIDS RESPONSE ... 60
4.1. Policies on Promotion and Prevention ... 60
4.2. Policy on Care, Support, and Treatment (CST) ... 70
4.3. Policy on Management of Strategic Information ... 75
4.4. Policy on Human Resources, Access and Logistic Management ... 77
4.5. Rights-based Policy ... 82
4.6. Policy on Multi-sectoral Governance ... 84
4.7. Policy on Funding ... 86
4.8. Policy on Impact Mitigation ... 88
HIV AND AIDS POLICY STAKEHOLDERS IN INDONESIA ... 89
5.1. International Development Partners ... 89
5.2. Ministry of Health ... 92
5.3. The National AIDS Commission ... 96
5.4. Provincial AIDS Commission ... 97
5.5. District/Municipality AIDS Commission ... 99
5.6. Civil Society Organisation ... 101
5.6.1 Non-Governmental Organisation (NGO) ... 101
5.6.2 Key Population Communities ... 103
5.7. Private Sector ... 105
INTEGRATION OF HIV AND AIDS RESPONSE INTO THE HEALTH SYSTEM ... 108
6.1. Institutional Integration: Contestation of Central and Local Governments ... 108
6.2. Integration into the Health Sector ... 114
6.3. Integration into the Non-Health Sector ... 117
6.4. Challenges of Integration ... 118
Conclusions and Recommendations ... 119
7.1. Conclusions ... 119
7.2. Recommendations ... 120
REFERENCES ... 122
Official Documents of the Government of Republic of Indonesia ... 124
Donors ... ... 125
Websites ... ... 125
Annex 1 ... 126
Annex 2 ... 128
Annex 3 ... 137
Annex 4 ... 154
Annex 5 ... 155
Annex 6 ... 156
Annex 7 ... 157
Annex 8 ... 158
Annex 9 ... 160
List of Tables and Figures
List of Tables
Table 1 – Cumulative Number of HIV and AIDS Cases based on the mode of transmission as
per December 1996 ... 27
Table 2 – Annual number of people with HIV and AIDS PLWHAin Indonesia from 1987 to 1996 ... ... 28
Table 3 – Cumulative Number of HIV and AIDS Cases for the Provinces of Papua and West Papua ... ... 42
Table 4 – HIV and AIDS Response Programs in Bali Province ... 57
Table 5 –Achievement of 2008 Target ... 65
Table 6 – Actively Reporting HIV and AIDS Service Facilities, 2011–2013 ... 73
Table 7 – Total of ARV Service Providers in Indonesia ... 80
Table 8 – International Development Partners working on HIV and AIDS Response in Indonesia, 1996 - 2015 ... 91
Table 9 – The Role of Local Government in HIV and AIDS Response ... 109
Table 10 – Vertical Policy Approach in HIV and AIDS Response ... 113
List of Figures Figure 1 –Prevalence of HIV among Injecting Drug Users and Sex Workers, 1997-2003 ... 25
Figure 2 – Sequence of HIV Transmission (Riono, 2004) ... 26
Figure 3 – Prevalence of HIV and AIDS in Key Populations in Jakarta, Indonesia, 2002 and 2004 ... ... 30
Figure 4 – Ten Provinces with the Highest Number of HIV and AIDS Cases (December 2006) ... 30
Figure 5 – Prevalence of HIV and AIDS Cases per 100.000 People by Province in Indonesia by 2006 ... ... 31
Figure 6 – Cumulative percentage of HIV and AIDS in Indonesia based on the mode of transmission by 31 December 2006 ... 32
Figure 7 – Total number of reported HIV and AIDS cases up to September 2013 ... 35
Figure 8 – Total of HIV and AIDS, and Deaths by HIV AND AIDS in East Java (xxxx – xxxx) ... 38
Figure 9 – Trend of Cumulative Total of HIV and AIDS Reported to Bali Provincial Health Office based on Transmission Risk Factors Year 1987–2012 ... 38
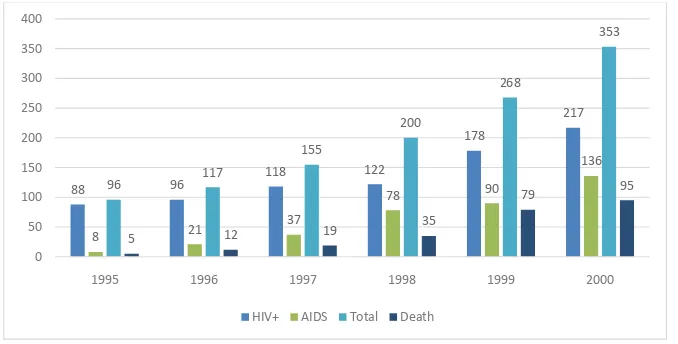
Figure 10 – Cumulative Number of HIV and AIDS Cases in Irian Jaya (Papua), 1995–2000 .... 40
Figure 13 – Frequency of Clinical Visit and Risk Behavioural Change ... 52
Figure 15 – Use of Condoms by Injection Drug User by Type of Partner ... 66
Figure 16 – Proportion of People Who Shared Used Needlesin the Previous Week by Municipality in 2004, 2007, 2011 ... 67
Figure 17 – Use of Condoms by FSW, MSM and PWID, 2004-2011 ... 69
Figure 17 – Use of Condoms by Female Sex Workers, 2002-2011 ... 69
Figure 18 – Case Fatality Rate of Reported AIDS by Year, 2000– September 2013 ... 74
Figure 19 – Sterile Syringe Service Program in 19 Provinces, 72 Districts/Municipalities ... 81
List of Acronyms
ANC Antenatal Care
AFAO Australian Federation of AIDS Organisations Inc AIDS Acquired Immunodeficiency Syndrome AIPH Australia–Indonesia Partnership for HIV AJI Independent Journalist Alliance
APBN State Budget
APBD Local Budget
Apindo Indonesian Employers’ Association ART Antiretroviral Therapy ARV Antiretroviral
ASA Stop AIDS Action
AusAID Australia Agency for International Development Bapas Correctional Centers
Bappeda Local Development Planning Agency Bappenas National Development Planning Agency BCC Behaviour Change Communication
BKKBN National Family Planning Coordination Board BLK Medical Laboratory Center
BLU General Services Board
BNN/P/K National/ Provincial/ Municipality/District Bureau of Narcotics BPJS Social Security Executing Agency (government program for health and
for employment)
BPOM National Drug and Food Control Agency
BPPT Agency for the Assessment and Application of Technology BPS Central Bureau of Statistics
BSS Behavioural Survey Surveillance
CATS Community Access to Treatment Services Study CBO Community Based Organisation
CCM Country Coordinating Mechanism
CFR Case Fatality Rate
CST Care, Support, and Treatment
Dephukham Ministry of Law and Human Rights Depkes Ministry of Health
Depkeu Ministry of Finance
Depkominfo Ministry of Communication and Information Deplu Ministry of Foreign Affairs Dikcapil/KKB Civil Registry Department/Demography
Dikbud Provincial/District/Municipality Office of Education and Culture Dinkes Provincial/District/Municipality Local Office of Health
Dinpar Provincial/District/Municipality Local Office of Tourism Dinsos Provincial/District/Municipality Local Office of Social Affairs Dishub Provincial/District/Municipality Local Office of Transportation Disnaker Provincial/District/Municipality Local Office of Manpower Dispenda Provincial/District/Municipality Local Office of Local Revenue Dispora Provincial/District/Municipality Local Office of Youth and Sports Ditjen PP&PL Directorate General of Disease Control and Environmental Sanitation DIY Special Region of Yogyakarta
GRA Group Risk Assessment
GWL-Ina Indonesian Gay, Transgender and Lesbian
IBBS Integrated Biological and Behavioural Surveillance IBRD International Bank for Reconstruction and Development IDHS Indonesia Demographic and Health Survey
IHPCP Indonesia HIV Prevention and Care Project IKON Addictive Drugs Victims Association ILOM Indigenous Leader Outreach Model IO Opportunistic Infection
IPF Indonesia Partnership Fund
IPPI Indonesia Positive Women Association Iptek Science and Technology
IRA Individual Risk Assessment
Jangkar Network of Agencies in Harm Reduction Keppres Presidential Decree
KIA Mother and Child Health
KIE Communication, Information, and Education KLB Outbreaks/ Epidemics
KPA AIDS Commission
KPAN/P/K National/ Provincial/ Municipality/District AIDS Commission KSPI Congress of Indonesian Workers Union
Menakertrans Minister of Manpower and Transmigration Mendiknas Minister of National Education
MTR-SRAN Mid-Term Report-National Action Plan Strategy Napza Addictive Drugs
NSP Needle Syringe Programme
Permenkokesra Regulation of Coordinating Minister of People’s Welfare PICT Provider Initiative Counseling and Testing
PKBI Indonesia Family Planning Association
PKMK-UGM Centre for Policy and Health Management of University of Gadjah Mada PPB Periodic Presumptive Treatment PPH HIV Research Center
Renstrakes Strategic Health Plan RKPD Local Government Work Plan RPJM Mid-Term Development Plan
RPJPD Local Government Long-Term Development Plan RS Hospital
RSCM Cipto Mangunkusumo Hosital RSKO Drug Addiction Hospital RSUP Central Level Public Hospital Rutan Prison
SBSI Indonesia Prosperous Workers Union SDM Human Resources
S&D Stigma and Discrimination Setkab Cabinet Secretary
SIK Health Information System SKN National Health System
SKPD Local Government Component Working Unit SOP Standard Operational Procedure
SPM Minimum Service Standards SRAN National Strategy and Action Plan SSP Behavioural Survey Surveillance
STBP Biologic and Behavioural Integrated Surveillance STD Sexually Transmitted Disease
STI Sexually Transmitted Infection Stranas National Strategy
SUM Scale Up at Most Population Group
TB-HIV Tuberculosis-Human Immunodeficiency Virus TNI Indonesia National Army
UN United Nations
Uncen University of Cendrawasih Unicef United Nations Children’s Fund
UNAIDS Joint United Nations Programme on HIV and AIDS UPT Technical Executing Unit
USAID United States Agency for International Development UU Law/ Regulation
VCT Voluntary Counseling and Testing WPS Women Sex Worker
Executive Summary
In response to the growing epidemic of HIV and AIDS in Indonesia, a wide range of responses and countermeasures has been introduced by the Indonesian health systems. The current study aims to examine changes in the health system responses to curb the HIV epidemic over the last 3 decades. The study revealed that the health system responses to HIV and AIDS epidemic in Indonesia reflect complex contestations between various approaches, principles, and actors operating within a constantly changing sociological context.
First, there is discordance between the vertical and horizontal strategies to address the increasing number of HIV and AIDS cases. The vertical strategy relies on a rigid and highly centralized technical intervention. In contrast, the horizontal strategy emphasizes multi-sectoral and decentralized approaches. Secondly, in policy making processes, political and economical considerations often outweigh epidemiological evidence as the basis for decision making. For instance, evidence has shown that the use of condom in high risk population should be promoted; however political considerations have prevented widespread campaign on condom use. Furthermore, there is often a conflicting role between the central and local governments. With strong access over epidemiological data, there is a predominance of central government actors particularly in technical intervention. However, local government have stronger role given their politically strategic position and autonomy in program implementation. Finally, disagreement is often found between school of thoughts represented by different institutions working in HIV and AIDS, for example USAID and AusAID (now DFAT), GFATM, local and international NGOs, and government agencies.
Two main challenges in the formulation of HIV and AIDS policy emerged from these circumstances. First, from the political and economic standpoint, it is important to align the HIV and AIDS policy and strategies with the government administration which has been undergone decentralization including the health sector. Second, it is crucial to find strategies for HIV and AIDS services integration into the existing health programs to ensure sustainable response given the limited resources and different capacitycity of local governments.
the organisational capability for implementation." Furthermore, Prichett’s study showed a unique pattern in the response of developing countries in managing development programs. This pattern refers to a phenomenon called "Isomorphic Mimicry" technique – a technique used by a non-poisonous snake to deceive their predators by mimicking the appearance of other snake species that are poisonous (i.e. adopting mottled skin). By establishing new entities and institutions, enforcing policies, signing mutual commitments and so forth, policy makers will appear to have delivered a good response. The mottled skin of non-poisonous snake represented the institutions and policies issued by the government described above. Such an attempt is in fact ineffective because it was not followed by adequate implementation capacity within the municipality.
The other important issue was funding sources. At present, the majority of funding for HIV/AIDS is contributed by foreign donors. Government policies to encourage the local government to procure funding for HIV and AIDS response have been issued. A number of local governments have allocated funding from local budget (Anggaran Pendapatan dan Belanja Daerah/APBD), however, the allocated budget may only finance the administrative costs. Therefore, funding to sustain HIV and AIDS programs and services are still considered insufficient.
Lastly, the role of civil society represented by the key population has not been optimal. Although the identities of existing communities such as people living with HIV and AIDS (PLWHA) and Intravenous Drug Users (IDUs) are quite well accepted by the society, however, this is not the case for Female Sex Workers (FSWs), transgenders, Men who have Sex with Men (MSM), and homosexuals.
Recommendations
INTRODUCTION
1.1. Rationale
The health system responses to HIV and AIDS epidemic in Indonesia have been ongoing for more than two decades. After the first AIDS case in Bali was officially reported in April 1987,1 the Minister of Health (MoH) issued Ministerial Regulation No. 339/IV/1988 on the Establishment of HIV and AIDS Committee in Indonesia. However, the present study argued that the Presidential Decree No. 36/1994 on the establishment of National AIDS Commission (Komisi Penanggulangan AIDS/KPA) in 1994 laid the foundation of government's formal response to HIV and AIDS epidemic. This policy was succeeded by various international collaboration programs through bilateral (e.g. USAID, AusAID, and DfID) and multilateral collaborations (GFATM, UNAIDS, Indonesia Partnership Funds), and other non-governmental agencies. The total funds that have been disbursed by both international and government agencies since 1996 were at least USD 445 million, most of which came from foreign aid.2 Between 1988 and 2013, a wide range of policies in response to the HIV and AIDS epidemic have been imposed by the government at both central and local levels. Several regulations provide the foundations – such as the Presidential Decree No. 36/1994 on AIDS commission as well as several local regulations (Perda) on HIV and AIDS at the district level. A few regulations introduced cutting edge approaches – such as the Presidential Decree No. 75/2006 which aimed to revitalize the authority of National AIDS Commission (KPAN), Regulation of the Minister of Health No. 567/2006 and the Regulation of Minister of the People’s Welfare No. 2/2007, both on the Distribution of Syringes.
However, responses from various parties to these policies seemed to be inadequate to support the Government of Indonesia (GoI) in achieving the national HIV and AIDS target. In 2014, as outlined in the 2010-2014 National Strategy and Action Plan (Strategi dan Rencana Aksi Nasional/ SRAN) for HIV and AIDS, the GoI aimed to achieve the goals of preventing 294,000 new infections, extending outreach services to 80% of key populations through
1 The first incidence of AIDS in Indonesia resulted to an intense debate in the mid to late 1980s. In October 1983, Tempo magazine released a report titled "AIDS, Welcome to Indonesia", which exposes a research of Dr. Zubairi Djoerban among transgender in Jakarta with indicative findings of AIDS – there was no HIV test at that time. In September 1985, the Minister had stated the discovery of 5 cases of AIDS in Bali, but two months after that the Minister said there was no AIDS in Indonesia. In April 1986, Tempo reported deaths of a 25 year old female AIDS patient through the article of "The Last Days of an AIDS Victim" – this case was also not recognized and reported officially by the government. On 10 April 1986, Kompas carried a report that "the existence of AIDS in Indonesia is still in debate". Only in 1987, the death of a 44 year old Dutch tourist in Bali was officially reported by the government as the first AIDS case in Indonesia – reported by Kompas, "A Dutch Tourist with AIDS Died in Bali", 11 April1987. See also Zubairi Djoerban (1999). Aiming AIDS: Endeavor in Understanding HIV and PLWHA. Yogyakarta: Galang Press and Foundation of Advancement of Internal Medicine.
2
comprehensive program, and achieving 60% of condom use during unsafe sexual intercourse. The 2011 Integrated Biological and Behavioural Surveillance (IBBS)3 by the Directorate General of Disease Control and Environmental Sanitation, Ministry of Health of Republic of Indonesia (MoH) showed that HIV prevalence in key populations was as high as 42% in Injecting Drug Users (IDUs), 22% in transgender sex workers, 10% in direct Female Sex Workers (FSWs), and 3% in indirect FSWs and 3% in Men having Sex with Men (MSM). Despite years of HIV and AIDS prevention programs, the potential for HIV transmission in Indonesia remains very high. The Ministry of Health reported that in 2012, a total of 8.7 million people were at risk of HIV. The 2011 IBBS data also revealed an alarming level of high risk behaviors. For example, only 32% of commercial sex workers use condom consistently. Amongst IDUs, around 13% shared used needles. In addition, the level of knowledge of HIV and AIDS has not been so encouraging. On average, only 22.7% of high-risk groups had a comprehensive knowledge of HIV and AIDS. The lowest percentage was found amongst the group of inmates (12%). In addition to the increasing rate of high risk population, the spread of HIV and AIDS transmission rate was evenly distributed across areas. During the period of 2007 to 2013, HIV and AIDS cases were widely spread in almost 80% of districts and municipalities across Indonesia. At least 7 of 10 districts and municipalities in Indonesia have now reported the cases of HIV and AIDS in their regions.
Previous studies indicated that this worrying situation was partly a result of the lack of integration of HIV and AIDS response into the existing health system – in other words, the HIV and AIDS response and the delivery of programs and services is still fragmented. There are several reasons that might explain this situation e.g. conflict of interests, different priorities in each program, and the lack of understanding on how the Indonesian health system is operationalized.4 As the governance of health system is the platform within which HIV and AIDS programs is delivered, strengthening of the health system is required as a necessary and sufficient condition for the effectiveness of HIV and AIDS response in Indonesia. Therefore, an understanding on the health system becomes a basic requirement to improve the effectiveness and efficiency of HIV and AIDS interventions.
This study was conducted to bridge the gap of knowledge between the health system and HIV and AIDS control (intervention) programs. The goal of this review was to provide policy recommendations on the integration of HIV and AIDS into the health service system. This review employed the following methodology:
3
Also called Integrated Biological and Behavioural Survey (IBBS), is a survey aimed at measuring the prevalence of HIV within the highest risk population, the level of their knowledge about HIV AND AIDS, their risk behaviors for HIV transmission, as well as determining the extent of coverage of the intervention programs in reaching out the highest-risk and most vulnerable populations. The survey is updated every 2-3 years. 4
• Documenting the genealogy and policies on HIV and AIDS response programs in Indonesia;
• Mapping of the existing policies, regulations, and programs regarding HIV and AIDS; • Identifying the gaps between policy and program implementation. Policies that act
as facilitators or barriers to effective HIV and AIDS control were identified.
• Formulating of policy recommendations on the integration HIV and AIDS response policies into the governance of health service system.
A number of key questions that guided this review include: • Genealogy and Policies
Which important events or facts that triggered the emergence of policies on HIV and AIDS in Indonesia for the past 25 years? How were these policies developed? Who were the actors involved? What was the focus of the policies at that time and has the focus been changed?
• Policy, epidemic situation, and policy implementation
Policy: What policies, both at national and local level, are currently implemented in HIV and AIDS programs? What have been stipulated in these policies? (e.g. relationship between government, private sector, and civil society organisations; prostitution; access to government funding and health services; supply-side policies by health service providers (e.g. community health centers or Pusat Kesehatan Masyarakat/ Puskesmas and hospitals) such as screening, STI treatment, HIV testing, provision of sterile syringe, methadone, condoms, etc.).
Epidemic situation: What is the latest situation of HIV and AIDS epidemic, both at national and selected districts i.e. Jakarta, Medan, Denpasar, Surabaya, Makassar, and Manokwari?
1.2. Methods
Based on the study rationale, the nature of data, and the key questions, the present study exercised the following methods:
1.2.1. Document Review
An extensive review was undertaken on all published and unpublished literatures produced between 1987 and 2013 related to HIV and AIDS response in Indonesia. These included regulations and laws, scientific articles, reviews, reports, etc., produced by the government, institutions working in the field of HIV and AIDS as well as research institutions. Document collections related to AIDS policy and programming were done by manual searching either offline or online.
Hand search of literature was also done by submitting request proposal to relevant agencies for their archived documents.
Analysis of literature was conducted based on the key questions and categorized using the following classification:
1. Local, national and international key events between 1987 and 2013, which set up the context of emergence and change of policies on HIV and AIDS in Indonesia. 2. Type of policies and programs related to promotion and prevention, care, support
and treatment, and mitigation of HIV and AIDS impact.
3. The role of health system in HIV and AIDS response, including governance, service delivery, financing, human resources (HR), strategic information, and provision of medical supplies for HIV and AIDS prevention and treatment.
4. Contextual factors: epidemiology, political commitment, social movement, global commitment, and program sustainability.
Epidemiological data of HIV and AIDS in Indonesia was obtained from HIV and AIDS behavioural and epidemiological surveys conducted by the Ministry of Health, KPA, or International Development Partners (Mitra Pembangunan Internasional/ MPI). Annex 1 contains the bibliography of documents reviewed in this study.
1.2.2. Field Visit: Interviews and Group Discussions
stakeholders as participants including representatives from health service providers, Provincial/District, Provincial and District/Municipality KPA Secretariats, and hospitals as well as those of program beneficiaries (i.e. transgender, FSW, MSM, drug users, and PLWHA). Interview and FGD guides are detailed in Annex 11. Triangulation was done by using interviewer notes, general data of the district/municipality, and results of the review to check the pattern, consistency, as well as variation in the data.
1.3. Study Period
The current study was conducted from September 2013 to January 2014. The study was conducted by a team of studiesrs from Center for Health Policy and Management, Faculty of Medicine, University of Gadjah Mada (Pusat Kebijakan dan Manajemen Kesehatan, Fakultas Kedokteran, Universitas Gadjah Mada/ PKMK UGM). Field visits were carried out in November 2013 along with research team members from the University of North Sumatra, University of Airlangga, State University of Papua, and University of Hasanuddin.
1.4. Study Limitations
The limitations of the present study are as follows:
1. The document review applied a historical perspective to describe the changes in policies and programs on HIV and AIDS in the past 25 years. There was a limited availability of literature related to policy and programs implemented in the early years of the HIV and AIDS epidemic in Indonesia. As a consequence, the description of the initial situation of the epidemic was limited. Although literature on the history of AIDS in Indonesia is widely available, the majority of these documents focused more on the description of the epidemic than on the important policy or events as the context of policy development.
2. HIV and AIDS is basically a multi-sector issue, consequently there is a myriad of policies and documents related to HIV and AIDS. This review was restricted to the context of Indonesian health system, and a description about HIV and AIDS response policy outside the health sectors is beyond the scope of this review. For example, literature related to political and economic aspects in the health sector which strongly influenced HIV and AIDS programs is not included in this study.
1.5. Outline of the Report
Findings of the present study are presented in the following chapters:
• The epidemiological context of HIV AND AIDS in Indonesia is described in Chapter 2. This chapter describes the history of HIV and AIDS in Indonesia followed by responses from the government, communities, and international agencies. This chapter is divided into three periods: 1987-1996, 1997-2006, and 2007-present based on the availability of epidemiological data, changes in the contextual factors surrounding health system governance and contestations within HIV and AIDS programs. Epidemiological profile of HIV and AIDS in the study areas (North Sumatra, East Java, Bali, South Sulawesi, and Papua) will be treated as examples of the epidemiological situation in Indonesia.
• Formulation and enforcement of regulations are the most common health system response to address the challenges of HIV and AIDS epidemic. Chapter 3 explores the context of HIV and AIDS regulations in Indonesia and how these regulations evolve over time until today. This chapter describes the policy context and references used as the basis to formulate policies on HIV and AIDS in Indonesia. Lessons learned from the implementation of the HIV and AIDS responses, which influenced the evolution of policies were presented
• Chapter 4 elaborates in more detail the existing policies related to HIV and AIDS by identifying important elements in those policies such as (1) promotion and prevention; and (2) care, support and treatment; or by analysing governance aspect in those policies such as (1) governance of strategic information; (2) human resources and logistics; (3) rights-based policies; (4) multi-stakeholders cooperation; (5) funding; and (6) impact mitigation.
• Chapter 5 details the institutions and key factors in HIV and AIDS programs and their specific contributions to policy development.
• Chapter 6 elaborates the integration of HIV and AIDS policies and programs into the Indonesia's health system as the core topic of this review.
DYNAMICS OF HIV AND AIDS EPIDEMIOLOGY AND RESPONSE
An accurate and thorough understanding of the epidemiological situation is an important prerequisite for an effective and context-specific policy formulation. HIV and AIDS epidemic has undergone through such dynamics in conjunction with the sociocultural, political, and economic changes in the society. The policy framework that shaped the HIV and AIDS response also underwent inevitable changes. This chapter describes the dynamics of HIV and AIDS epidemiology in Indonesia, the surrounding policy context, and approaches of previous HIV and AIDS control programs. This chapter also illustrated some case studies from the selected study sites.
Since it was first identified in 1987, the HIV and AIDS epidemic has been developing rapidly in line with the changes in the natural history of the epidemic, the health care system, as well as the political context and government system. The methods, prevalence estimation and key populations involved in the Integrated Biological and Behavioural Surveillance’ (IBBS) also influence the response of government and development partners towards HIV and AIDS epidemic. The availability of antiretroviral (ARV) treatment has substantially reduced HIV and AIDS-related mortality rateand increased longevity. Consequently, HIV and AIDS professionals are presented with more challenge to provide long-term care.
2.1. HIV and AIDS epidemiology in Indonesia
The first AIDS case in Indonesia was identified in Bali in 1987, during which was no HIV test available. Experts in this field immediately and repeatedly announced the potential spread of HIV and AIDS across the country. The potential of HIV and AiDS transmission in Indonesia was particularly high given the prevailing risk factors, such as the widespread availability of commercial sex industry, the high prevalence of Sexually Transmitted Infections (STIs), poverty, and the high rate of population mobility (Kaldor, 1999). Twelve years after the first case was identified, there was no significant increase in the number of cases despite the persistence of these risk factors. Interestingly, a number of risk factors that were perceived to accelerate increase in the number of cases have instead become prohibitive factors. For instance, poverty has in fact reduced the demand for commercial sex, although it might increase the number of commercial sex workers. However, increasing number of sex workers is not associated with increase in the turnover of customers.
The Ministry of Health reported that over the period of 1991 to 1995, approximately 40,000 females sex workers (FSWs) were annually tested for HIV. This number was nearly one-fifth of the total FSWs throughout the country. It was found that the annual HIV prevalence was always below 0.03%. It might be inferred that despite the the high rates of population mobility and STI prevalence, the spread of the virus would not take place if the HIV virus was not present in the population.
Injecting Drug Users (IDUs) rapidly increased especially in large cities. In 1997, there was no HIV case found among participants of rehabilitation program at the Drug Dependence Hospital (Rumah Sakit Ketergantungan Obat/ RSKO) in Jakarta. However, within four years, it was found that one in two IDUs in Jakarta was infected with HIV.5 Within the next five years, IDUs became the major hub of HIV and AIDS spread in Indonesia. Thus, the main factor driving the spread of HIV and AIDS epidemic was not the size of sex industry or the high prevalence of STIs, but the influx of IDUs into the epidemic network (Family Health International/ FHI, 2002).
Nonetheless, the close relationship between IDUs and the commercial sex industry need to be considered because these two factors might work synergically and result in the rapid expansion of HIV and AIDS epidemic in Indonesia. The 2002 Behavioural Survey Surveillance (BSS) among IDUs in three major cities in Java showed a high number of IDUs practicing unprotected sex with non-IDUs. Approximately 20%-75% of IDUs reported unprotected sex with sex workers. Nearly one in ten IDUs also reported that they provided sex for money. This "synergy" has in fact accelerated the increase of HIV and AIDS prevalence among commercial sex workers. The 2004 BSS in Surabaya showed that the prevalence of HIV and AIDS among commercial sex workers brothel complex had tripled to 3.8% between 2001 and 2004. Among street-based sex workers, the prevalence of HIV and AIDS increased from 4.4% to 12.2% within a period of two years. In Jakarta, the HIV prevalence rose from 1.1% in 2000 to 6.4% within three years. Without the influx of IDUs into the sex industry, the prevalence rate would have been increasing at a slower pace.
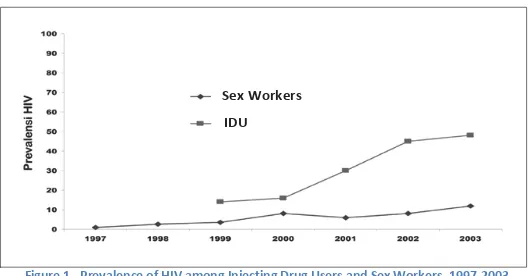
Figure 1 shows that the the rate of HIV and AIDS prevalence among IDUs increases in parallel with the prevalence among sex workers. It is also apparent that the prevalence among sex workers increases as the IDUs population entered the sexual networks (i.e. IDUs as commercial sex consumers or workers). Previous studies (MoH, 2005; Riono and Jazan, 2004) identified factors that associated with the increase of HIV prevalence as follows:
1. Proportion of people who had been infected in a population; 2. Size of the population;
3. Level of high risk behaviour in a population (e.g., the use of condoms among sex workers, frequency of commercial sex transaction etc.);
4. Interaction between high risk populations (e.g., sexual contacts between IDUs and sex workers).
5
(Source: The Central Bureau of Statisticts & the Ministry of Health of Republic of Indonesia, 2004)
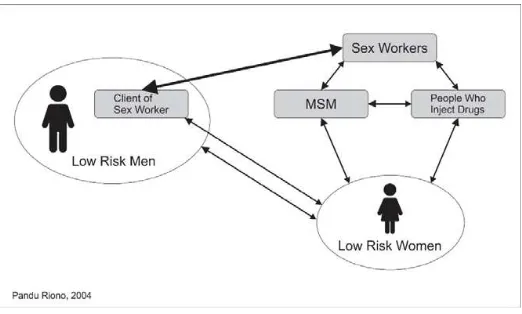
Despite the high prevalence of HIV and AIDS among IDUs, in 2006 KPAN estimated that the growth rate of new infections among IDUs seemed relatively stagnant. Although the HIV and AIDS prevalence in FSWs, transgender, and FSW clients are lower than in IDUs, these groups have a larger size of population which results in higher number of cases. KPAN estimated that within the following decade, new transmissions will be predominated by heterosexual contacts as it accounted for nearly 70% of new infections (KPAN 2007). Given such trend in HIV and AIDS epidemic, studies on high risk sexual behaviour have become increasingly important in order to gain a comprehensive understanding of the epidemic situation. It is particularly important to ensure effective response and control the impact on other sectors. More attention was also addressed to interaction between transgender sex workers and their clients. The majority of clients of transgender sex workers identified themselves as heterosexuals. Many of them also had sex with female sex workers. With the high prevalence of HIV and AIDS in transgender sex workers – nearly 25% of transgender sex workers in most Indonesian municipalities are infected with HIV – their clients become the "bridge" of HIV transmission from transgender sex workers to FSWs and vice versa, and even to the general population (i.e. to their wives). In addition, the growing sex industries among men who have sex with men in several municipalities also need to be considered. Half of the male sex workers identified themselves as heterosexuals and also have sex with female sex partners (FHI, 2002). Sexual networks are closely interlinked and function as a highway for HIV to spread into the general population, as in Figure 2.
HIV and AIDS epidemic has been developing in Papua in a slightly different way. The number of IDUs in Papua is relatively lower than in other major municipalities in Indonesia. The main factor of the rapid spread of HIV and AIDS in Papua is sexual contacts especially heterosexual contacts. An anthropological study on Papuans sexuality described that the characteristics of sexual networks in Papua are very different compared to those in other areas. Premarital and intergenerational sex practices are very common (Butt et. al., 2002), which result in different patterns of HIV and AIDS transmissions and become the main
Figure 1 –Prevalence of HIV among Injecting Drug Users and Sex Workers, 1997-2003 Sex Workers
pathway of HIV and AIDS spread into the general population. The 2006 IBBS showed that the epidemic in Papua has reached the general population and developed into generalized epidemic), in which at least 2.4% of the adult population (15-49 years) are infected with HIV and AIDS.
Patterns of HIV transmission in Indonesia is mainly concentrated in the at risk populations such as injecting drug users, sex workers and men who have sex with men. However, since the populations are not isolated and they have social interaction with the broader population, the threat of transmitting the virus to the broader population is likely to happen.
The course of HIV and AIDS epidemic in Indonesia and its link to changes within the society reflect an epidemic situation which is concentrated on certain groups (e.g. IDUs and sex workers) and yet to find structural expanding transmission network condition to threaten the broader populations.
A structural interaction between at risk population and broader population has thus evolved, resulting in an emergent pattern of HIV transmission which different from the previous pattern. For example, the majority of infected IDUs are sexually active groups. They become powerful bridge to spread the virus to other groups, i.e. their sexual partners such as sex workers or housewives through risky sexual behaviour.
In addition to individual characteristics, there are also other factors influencing the extent of HIV and AIDS transmission, such as supports of health services providers, poverty, and mobilization of people.
2.2. Epidemic Response
government and non-governmental organisations in Indonesia from early 1990s to 2007. The development of HIV and AIDS epidemic in Indonesia was divided into three periods based on the predominant mode of transmission: 1) 1987-1996: HIV and AIDS was predominantly transmitted via sexual contacts; 2) 1997-2006: share of used needles became predominant as the mode of transmission; and 3) 2007-present: sexual contacts reemerged as the main mode of transmission.
2.2.1. Period of 1987 to 1996
Literature related to HIV and AIDS epidemic in the early years were reports on HIV and AIDS cases from the early years of this period until the end of 1996. The number of HIV-positive and AIDS were 381 and 154, respectively. These figures did not adequately reflect the magnitude of HIV and AIDS epidemic in Indonesia as there were no accurate data on the prevalence of high risk behaviours and estimates of key population estimates. Data used as reference were the profiles of people with HIV which 82.9% were in their productive age i.e. 15-49 years). Most of the key population were infected from unprotected sexual intercourse (95.7%), of which 62.6% were heterosexuals and 33.1% were male homosexuals/bisexuals contacts (National AIDS Strategy, 1994).
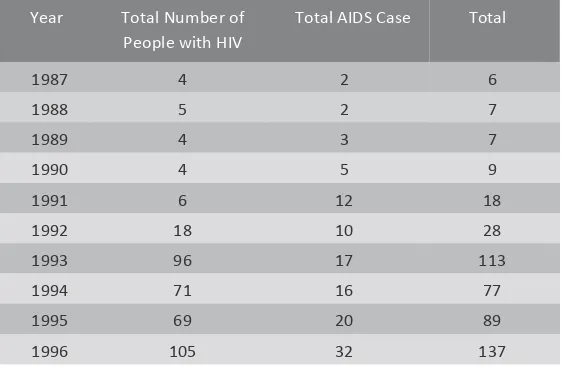
By December 1996 as reported by, Ministry of Health the cumulative number of HIV and AIDS cases was 232 and 107, respectively. The highest rate of HIV and AIDS cases was found in the age group of 20-29 years, especially amongst homo/bisexual populations. The mode of transmission and the number of HIV and AIDS cases as per December 1996 are shown in Tables 1 and 2.
Table 1 – Cumulative Number of HIV and AIDS Cases based on the mode of transmission as per December 1996 Risk Factors/Mode of Transmission HIV AIDS Total
Homo-Bisexual 278 48 326
Heterosexual 34 51 85
IDUs 2 3 5
Blood Transfusion 0 2 2
Hemophiliac 1 1 2
Perinatal Trans 1 0 1
Unknown 66 14 80
(Source: Directorate General of Disease Control and Environmental Sanitation, Ministry of Health of Republic of Indonesia)
Table 2 – Annual number of people with HIV and AIDS PLWHAin Indonesia from 1987 to 1996 Year Total Number of
People with HIV
Total AIDS Case Total
1987 4 2 6
1988 5 2 7
1989 4 3 7
1990 4 5 9
1991 6 12 18
1992 18 10 28
1993 96 17 113
1994 71 16 77
1995 69 20 89
1996 105 32 137
(Source: Directorate General of Disease Control and Environmental sanitation, Ministry of Health of Republic of Indonesia)
As mentioned before, AIDS cases had been found – although this was also a matter of debate – since the early 1980s. However, HIV and AIDS issue received a scant attention in Indonesia that only in 1986 had the Ministry of Health of the Republic of Indonesia established an AIDS Working Group chaired by the Ministry’s Head of Research and Development Agency. After the first discovery of AIDS case was published in 1987, the government established the National AIDS Committee chaired by the Director General of Communicable Disease Control and Environmental Sanitation. This response indicated that AIDS was perceived only as a health issue.
When the epidemic started to spread it was evident that HIV and AIDS did not only affect the health sector but also non-health sector. As a result, KPA was established by Presidential Decree No. 36/1994 as a coordinating institution for AIDS multi-sector responses. . The establishment of KPA was an initial institutional response and an acknowledgement that HIV and AIDS is a health and social problem which requires greater attention to mainstreaming HIV and AIDS issues in all government sectors.
Most of HIV and AIDS programs during this period focused on awareness raising of the existence of HIV and AIDS in Indonesia. These were delivered through educational programs with key messages that HIV and AIDS is a real threat and that HIV and AIDS is primarily transmitted through unprotected sex. As a result, civil society organisations working for the key populations started to flourish. These organisations commonly offered dissemination of information and STI clinics that provided services to key populations.
2.2.2. Period of 1997–2007
This period was signified by the establishment of HIV and AIDS behavioural surveillance systems (BSS) in Indonesia that was conducted in 1996 and later became the principal reference in assessing the HIV and AIDS epidemic situation in Indonesia. When the data on HIV and AIDS prevalence among IDUs from Yakita Foundation, Bogor, Jakarta RSKO, and Stop AIDS Action Program of FHI were published, the public began to realize the significance of injection drug use as a mode of transmission, especially with the high rate of the sharing of used needles among IDUs (90%). Data from the Indonesia HIV Prevention and Care Project (IHPCP) /AusAID Program in 2004 (Suresh Narayanan, 2004) revealed that the illegal drug industry in Indonesia was growing rapidly, both in terms of supply and demand. IHPCP also reported an increase in illegal drug production globally. Illegal drug business has become the world's second largest business after gun trade (i.e. USD 500 billion/year). The types of drugs sold in the market also increased, in parallel with the increasing number of users.
Surveillance among inmates was started as a basis to improve the services in prison. In 2002, it was found that HIV prevalence among inmates in Jakarta was 5.2% (Ministry of Health, 2004). The availability of service providers in prison is limited, therefore implementing voluntary, counseling and testing services in prison is urgent.
MSM group was also established as one of the key affected populations during this period, following the findings of HIV and AIDS prevalence among this group. Since the early 2000s, the prevalence of HIV and AIDS among key populations had increased to more than 5%. With these figures, Indonesia was classified as a concentrated epidemic region.
In 2006, experts estimated that more than 110,000 people had been infected with HIV and AIDS (Ministry of Health of Republic of Indonesia, 2006). The National Surveillance Data on HIV and AIDS reported that transmissions continuously increased. Until the end of 2006, the highest prevalence among commercial sex workers was found in Sorong, which reached 22.8%. Meanwhile, transmission through unsterile needles was more than 50% in Jakarta RSKO and 68% among inmates in Bekasi Penitentiary Facility.
Figure 3 – Prevalence of HIV and AIDS in Key Populations in Jakarta, Indonesia, 2002 and 2004 (Source: Ministry of Health of Republic of Indonesia, 2004)
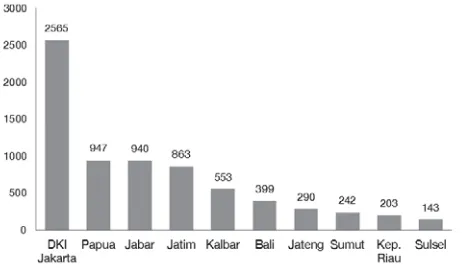
The spread of HIV and AIDS epidemic to all regions of Indonesia occurred during this period. At the end of 2000, only 16 provinces reported AIDS cases, however, this number increased to 25 provinces by the end of 2003, and to 32 provinces and 186 municipalities/districts in 2006 (MoH and Central Bureau of Statistics/BPS, 2007). Provinces with the highest number of AIDS cases in descending order were DKI Jakarta, Papua, West Java, East Java, Bali, West Kalimantan, North Sumatra, Central Java, Riau Islands, and Riau. Figure 4 illustrates the 10 provinces with the highest number of HIV and AIDS cases.
Figure 4 – Ten Provinces with the Highest Number of HIV and AIDS Cases (December 2006) (Source: Ministry of Health of Republic of Indonesia, 2004)
22
48
25
6
0 10 20 30 40 50 60
Female Sex Workers, 2002
IDU, 2002 Inmates, 2002 Male Sex Workers, 2004
Percent HIV
Positi
Center for Data and Information of the Ministry of Health in 2006 showed that the highest prevalence of HIV and AIDS cases per 100,000 population was found in Papua, followed by Jakarta (Figure 5).
Figure 5 – Prevalence of HIV and AIDS Cases per 100.000 People by Province in Indonesia by 2006 (Source: Ministry of Health of Republic of Indonesia, 2006)
During the period of ten years (1996 and 2006), the cumulative number of PLWHA increased by nearly a hundred-fold. By December 2006, a total of 13,424 PLWHA had been reported, of which 3,492
In terms of the distribution of HIV and AIDS prevalence by age groups, those affected by HIV and AIDS were mostly between 20-29 years (54.76%), followed by the 30-39 years (27.17%); and 40-49 years (7.90%). Thus, almost 90% of HIV and AIDS cases occurred in the productive age group of 20-49 years (89.93%). In addition, HIV and AIDS also affected infants and children younger than 15 years through mother-child transmissions or a transfusion of bloods/blood components (e.g. on patients with hemophilia). A comprehensive health services for women with HIV and AIDS were not fully in place.
Figure 6 – Cumulative percentage of HIV and AIDS in Indonesia based on the mode of transmission by 31 December 2006 (Source: Ministry of Health of Republic of Indonesia, 2006)
Until the early 1990s, the HIV and AIDS transmission among IDUs was never a concern, although the data in other countries showed that the use of used needles and exchange of needles between users had increased the spread of HIV and AIDS. Three HIV and three AIDS cases among IDUs in Indonesia were first reported in 1997 (MoH, 1997). Since then, the prevalence of HIV and AIDS showed an increasing trend – the prevalence rose sharply during the period of 2003 to 2006.
During this period, the role of counseling and testing was increasingly considered important especially when the prevalence continued to increase. However, the provision of treatment was still low in coverage. From the institutional side, the coordination role of KPA was not fully functional. In 2004, the government and relevant stakeholders made a mutual political agreement through the Sentani Commitment which declared that efforts against HIV and AIDS response from national to local levels must be revitalised.
With the increasing importance of IDU transmission, three major HIV and AIDS programs for IDUs were observed during this period. The first program was pioneered by Yakita Bogor which used rehabilitation and education approaches. The second major program was IHPCP initiatives with twelve interventions6 in Harm Reduction7 focusing on the distribution of
6
Twelve types of interventions among others are NSP, syringes disposal, peer educator, primary health, care and treatment for PLWHA, oral substitution, drug treatment, VCT, infection prevention, outreach, and Information, Education, and Communication. The applied models are outreach by NGOs, Mobile Unit by NGOs and Puskesmas, Shop Front by NGOs and Puskesmas, and Pharmacies.
7
The main message of Harm Reduction is: "Stop using drugs. If you need to use, smoke, not inject. If you need 4.2
40.3
50.3
0.1 1.5
3.6
0 10 20 30 40 50 60
needles and syringes (Needle Syringe Program/ NSP) as well as methadone therapy. Third was the Indigenous Leader Outreach Model (ILOM) pioneered by FHI’s Stop AIDS Action with the following characteristics:
• Combination of epidemiologic and ethnographic approaches; • Outreach as a platform for services/ interventions;
• Involvement of target groups; and
• Focus on changes on behaviour and social norms related to at risk practices.
The purpose of this model was to identify and gain access to the IDUs groups, raise awareness of HIV and AIDS, promotion of risk reduction strategies, encourage the adoption of sustainable risk reduction, dissemination of information about the impact of HIV and AIDS, and advocacy. The followings are the illustration of the application of ILOM by Non-Governmental Organisations (NGOs):8
• Engage in the IDUs social environment.
• Provide information about HIV and AIDS and drugs, prevention and transmission (in discussions, or casually and entrust the media, if the group is in an "unconscious" state).
• Distribution of Information, Education and Communication (IEC) materials, alcohol swabs, sterilisation package, condoms (for sexually active).
• Perform Individual Risk Assessment (IRA) and Group Risk Assessment (GRA) for behavioural change and to provide alternatives.
• Continue support the behavioural change.
• Promote to take blood test (Voluntary Counseling and Testing/ VCT) for free at the kiosk, to determine the risk of assisted groups of HIV and AIDS.
• Promote activities organized by NGOs (medical examination and free medicines, peer support groups, and vocational training).
• Involve assisted groups and communities in HIV and AIDS prevention advocacy. 2.2.3. Period of 2007–2013
According to the Global Report of AIDS Epidemic by UNAIDS in 2008, the AIDS epidemic in Indonesia was one of the most rapid growing epidemic in Asia. In 2009, the estimated number of people living with HIV and AIDS increased to 333,200 people, of whom 25% were women. This figure shows the feminisation of HIV and AIDS epidemic in Indonesia. Of 11,856 cases reported in 2009, 6,962 were in productive age (less than 30 years). A total of 55 infants under 1 year old were also affected.
Without scaling up prevention, treatment, care and support in the affected provinces, the
8
number of PLWHA was projected to increase from 227,700 in 2008 to 501,400 in 2014.9 During this period, HIV and AIDS had spread across all 33 Indonesian provinces and 348 districts/municipalities, or nearly 80% of the total districts/municipalities in Indonesia. Between 2007 and 2013, the cumulative number of HIV and AIDS cases reached 118,787 and 45,650, respectively. Provinces with the highest number of HIV positives were DKI Jakarta (27,207), East Java (15,233), West Java (9,267), and Bali (7,922). The highest number of AIDS cases was reported in Papua (7,795), followed by East Java (7,714), DKI Jakarta (6,299) West Java (1,699), and South Sulawesi (1,660).
The 2010-2014 National Strategic Action Plan for HIV and AIDS Response reported that HIV and AIDS cases have been documented in more than 200 districts/municipalities across all provinces in Indonesia. By 2009, HIV and AIDS epidemic in most provinces were still concentrated on key populations with a prevalence of more than 5%. However, the HIV and AIDS epidemic in Papua had spread into the general population with prevalence rate ranging from 1.36% to 2.41%.10
The 2011 IBBS indicated that the highest prevalence of HIV and AIDS was found in the IDUs (36%) followed by transgender, direct FSWs, MSM, prisoners, indirect FSWs and high-risk men. This finding was similar to the results of 2007 IBBS. Compared to the 2007 survey, there was no change in the prevalence rate among direct FSWs, indirect FSWs, high-risk men, and transgender. Nevertheless, an increase in the prevalence by 2-3 folds was observed among MSM group.The prevalence among IDU group declined by 10% in Jakarta and 20% in Medan.11 The 2011 IBBS also measured the prevalence of STIs including syphilis, chlamydia, and gonorrhea. Syphilis was most commonly found in transgender group (25%). Compared to the 2007 survey, the prevalence of syphilis among direct and indirect FSW groups decreased by 4-8 folds, transgender by 20%, and high-risk men by 3%. These declines were mainly observed in brothel complex areas receiving Periodic Presumptive Treatment (Pengobatan Presumtif Berkala/ PPB) program. In contrast, the prevalence of syphilis in MSMs increased by 2-5 times compared to 2007.12
9
This has been revised in the 2012 Ministry of Health’s estimates to 590,000 (MoH, 2012). 10
BPS, Ministry of Health, KPAN (2006). "Risk behavior and prevalence of HIV-AIDS in Papua." Result of the 2006 Integrated Surveillance on HIV-AIDS and Behavior in Papua.
11
This decline is still in debate among experts in relation to the sampling method and estimation on the declining number of IDUs population. See Praptorahajo et al. (2013).
12
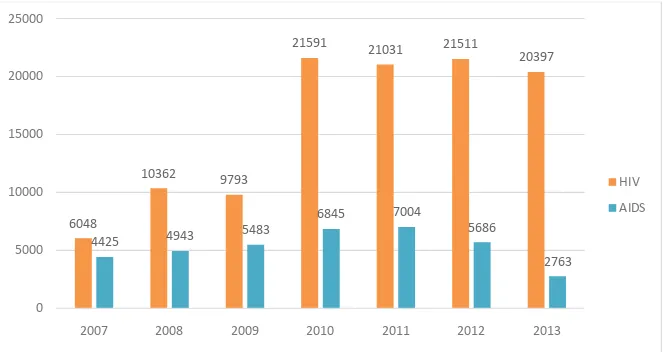
Figure 7 – Total number of reported HIV and AIDS cases up to September 2013 (Source: Ministry of Health of Republic of Indonesia, 2013)
During this period, the main mode of transmission was heterosexual (60.9%), injection drug use (14.4%), perinatal (17.4%) and homosexual (2.8%) transmissions. The case fatality rate due to AIDS at 2007 was 7,46 % then decreased to 0,30% as of June 2013, indicating an increase in the number of PLWHA receiving ARV treatment (Ministry of Health, 2013). There was no difference in the proportion of high risk groups in the same areas between 2007 and 2011 except in IDU population. Greater attention was paid to this increase in IDU population, as injection drug use can be an effective medium for HIV and AIDS transmission and double the risk of HIV and AIDS transmission to other high-risk groups. Unsafe behavior in injection drug use such as sharing of used needles was most frequently found in Jakarta (27%) and the least frequently in Medan (7%). Sharing of used needles behaviour is strongly influenced by the distribution system of needles and syringes as well as the level of integration with primary health services (Praptoraharjo et al., 2013). The proportion of IDUs who exchanged used needles showed a decline from 2004 to 2011.
HIV and AIDS response during this period focused on commercial sex workers and their clients due to the high number of population who are at risk of contracting HIV and AIDS via sexual transmission. Despite the higher prevalence rate of HIV and AIDS in IDUs, the number of population at risk due to unsafe sexual behavior was still higher. In addition, focus on commercial sex workers group also involved the awareness of close relationship between key populations. For example, the IDU transmissions are strongly associated with unprotected sex (e.g. practice of unprotected sex among IDUs, or commercial sex workers/clients who are also IDUs).
6048
10362 9793
21591 21031 21511
20397
4425 4943 5483
6845 7004
5686
2763
0 5000 10000 15000 20000 25000
2007 2008 2009 2010 2011 2012 2013
*Number of reported AIDS case had been changed following the data validation with DOH in May 2012
HIV
The importance of continuum of care was also recognized in this period as several policies related to integrated services of STIs, HIV tests, Needle Syringe Program (NSP), methadone, Antiretroviral Therapy (ART), as well as collaboration between NGOs and Puskesmas were developed. However, the practice of continuum of care varied between areas especially on NSP service, methadone and ARV, due to different interpretation of the regulations between areas.13
The availability of services also improved during this period. Until September 2013, there were 889 Voluntary Counseling and Testing (VCT) services available. A total of 330 Care, Support and Treatment (CST) consisting of 266 hospital referrals and 114 satellite services were established. A total of 85 Methadone Maintenance Treatment (MMT), 886 STIs clinical services and 144 Prevention of Mother to Child Transmission (PMTCT) services were available in several provinces. In addition, 9 penitentiary facilities and prisons provided HIV and AIDS programs through MMT services, while HIV and AIDS referral activities were implemented by 127 penitentiary facilities and prisons.
Until September 2013, the total number of PLWHA receiving ARV treatment was 36,483. The most frequently used regiment was ARV line 1 (96.42%) and ARV line 2 (3.19%). By September 2013, the cumulative percentage of PLWHA was 55.7% male, 29.2% female, and 15.1% unknown. The number of female PLWHA showed an increase every year.14
From the institutional side, the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM) initiatives which was founded in 2002 raised the awareness of the need to revitalize the role of KPAN. The Presidential Decree No. 75/2006 on KPAN was issued to amend the Presidential Decree No. 36/1994 in order to strengthen the institutional role of KPAN’s. The policy reinforcement was followed by the preparation of the National Strategy for HIV and AIDS for 2007-2010, which clearly defined the comprehensive efforts on HIV and AIDS response based on the nature of the epidemics and adapted to the context of decentralisation.
13
Praptoraharjo et al. (2013). "Indonesia NSP Review". UNODC Indonesia. 14
Since the first AIDS case was reported in 1987 at Sangla Hospital Bali, many provinces started to report AIDS cases. The first AIDS case in North Sumatra was
found in Pirngadi Hospital Medan, in 1992.
In 1989, two cases of AIDS were found in Dr. Soetomo Hospital, Surabaya, EastJava. The first AIDS case in South Sulawesi was reported in 1996, while the one in Papua, i.e. in Merauke, was found
in 1992.
The highest prevalence of AIDS cases in the study locations by 2013 was 375.03% in Papua, 102.42% in Bali, 23.28% in East
Java, 21.20% in South Sulawesi, and 10.02% in North Sumatra. The national
AIDS prevalence was 22.03%.
(Directorate General of Disease Control and Environmental Health of Ministry of
Health, 2013)
2.3. HIV and AIDS epidemy in Five Selected Provinces
2.3.1. North Sumatra
The first HIV positive in North Sumatra was discovered in an FSW in Pirngadi Hospital Medan in 1992. The first AIDS case was found in a seafarer in 1994. In 1997, the HIV and AIDS Team was established at Dr. Adam Malik General Hospital in Medan. However, this team was not functional.
To ensure the continuation of AIDS Committee at the Adam Malik General Hospital Medan, the Decree on Establishment of Special Service Center (Pusat Pelayanan Khusus/ Posyansus) at RSUP Adam Malik General Hospital Medan was issued in April 2011. Based on the report from some NGOs, stigma and discrimination by health personnel were still prevalent at the time of the study. Between January 2006 to December 2013, the number of HIV and AIDS cases in Medan Municipality reached 3,410 consist of 2,198 cases in heterosexuals, and 958 cases in IDUs (Medan Municipality Health Office, 2013). Currently, the total number of HIV and AIDS cases in North Sumatra has reached 6,340 i.e. 2,198 HIV and 4,241 AIDS cases (Ministry of Health, 2013).
2.3.2. East Java
The first cases of AIDS in East Java were reported in two patients of RS Dr. Soetomo Hospital Surabaya in 1989. In 1990 there were no additional reports, yet 1 case was reported in 1991. The AIDS patient was diagnosed because of advanced Opportunistic Infections (OIs). Dr. Soetomo Hsopital was the first institution responded to this case. By 2013 the estimated number of PLWHA in East Java was 57,321 people, of which 19,017 were HIV positives and the rest were AIDS (33.2% of the estimated figure) (East Java Provincial AIDS Commission, 2013). East Java has been declared as a concentrated epidemic area, as it hosts the second highest number of AIDS cases after Papua as of June 2013.
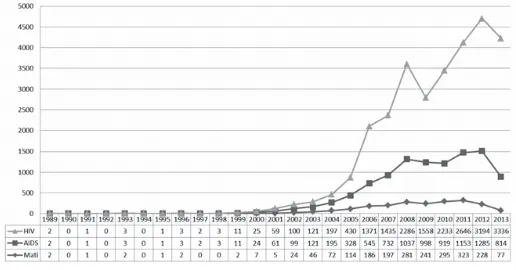
showed that as many as 1,268 AIDS cases occurred amongst housewives. This number is substantially higher than the number of cases in FSWs which totaled 568 cases (6.8%).15 Of the 627 pregnant women with HIV positive, 442 had access to ART. A total of 454 babies were born from HIV-positive mothers. Of the 65 babies born from HIV-positive mothers, 32 babies were declared positive of HIV (East Java Provincial AIDS Commission, 2013). Figure 8 shows the annual number of HIV, AIDS and mortality cases in East Java.
Figure 8 – Total of HIV and AIDS, and Deaths by HIV AND AIDS in East Java (xxxx – xxxx) (Source: East Java Provincial AIDS Commission, 2013)
2.3.3. Bali
The first AIDS case in Indonesia was discovered in Sanglah Hospital in Denpasar, Bali in 1987. The case was detected in a homosexual Dutch man who lived in Candi Dasa.
Figure 9 – Trend of Cumulative Total of HIV and AIDS Reported to Bali Provincial Health Office based on Transmission Risk Factors Year 1987–2012
(Source: Bali Provincial AIDS Commission, 2013) 15
The HIV and AIDS epidemic in Bali displayed a changing pattern over time. Although the first case was found amongst homosexual, but in 2000 the HIV and AIDS epidemic had expanded towards the group of IDUs. Currently, an increasing trend among heterosexuals group has been observed. HIV and AIDS cases had also been found in women and pregnant women. Until July 2013, the total number of HIV and AIDS cases in Bali was 8,003, i.e. 4,230 were HIV positives and 3,773 were AIDS cases. HIV and AIDS positives were also found in housewives, infants, and children. Data on HIV and AIDS epidemic in Bali was obtained from medical records and serological surveys conducted among high-risk groups. To describe the epidemiology among general population, a group of pregnant women was also sampled (KPA Bali Province, 2013).
The HIV and AIDS cases in Bali were not evenly distributed. Districts with the highest number of PLWHA were Denpasar, Buleleng, Badung, Gianyar, and Tabanan. The distance between districts within the province is not that far. For example, it will take approximately 45 minutes by car or motorcycle from Denpasar Municipality to Badung District or from Denpasar to Gianyar District. Such an easy access enables high mobility of people or clients from one area to another. Other factors that ease the transmission were concentration of population distribution, distribution of high-risk populations, and distribution of entertainment centers (Bali Provincial KPA, 2013).
2.3.4. South Sulawesi
The first HIV cases in South Sulawesi were documented in 1996. Three bride and groom were reported by the media to be HIV positives. All of the three brides had been former FSWs who were detained under the community/social problem operation by the Municipal Police in South Sulawesi. These three brides were sent to a social welfare rehabilitation of
Penyandang Masalah Kesejahteraan Sosial (PMKS) in South Sulawesi Province.
The South Sulawesi Provincial KPA had been established in 1994, however, there was no significant response towards HIV and AIDS after the first cases were reported. Around 1991 and 1992 there was a group of volunteers who started providing outreach services to FSWs and transgender population in South Sulawesi. The volunteer group was initiated from a discussion between students from several universities on the HIV and AIDS situation in South Sulawesi and became the forerunner of KRA-AIDS and Yayasan Gaya Celebes, the two prominent civil society organisations working in HIV and AIDS in South Sulawesi.