Medical Director, La Jolla Spa MD, La Jolla, CA Clinical Professor of Dermatology/Medicine, University of California, San Diego, CA, USA. Associate Dermatology Associates of San Diego County, CA Clinical Assistant Professor of Dermatology, Mount Sinai School of Medicine, New York, NY, USA.
INTRODUCTION
Always burns easily, never tans Burns always burns easily, tans minimally Burns moderately, tans gradually Burns minimally, always tans well Burns rarely, tans proJus Never burns; deeply pigmented (Data from Goldman MP, Fitzpatrick RE 1999 Cutaneous laser surgery, 2nd edn. Less dramatic improvement The risk may outweigh the benefit: the. treatment may be too aggressive to treat a relatively minor problem.
EXPECTED BENEFITS
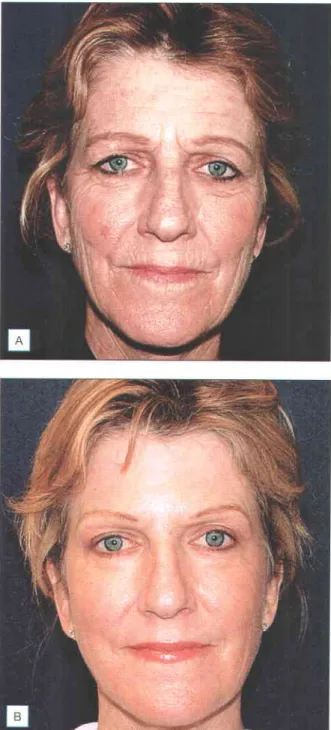
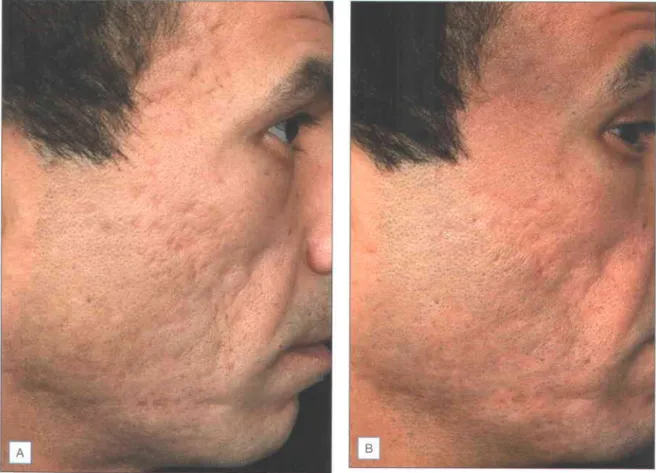
Patients with Fitzpatrick skin types IV-VI can certainly be treated, but with the understanding that these patients have a 1000/o risk of hyperpigmentation, which usually occurs one month after treatment and may take months to resolve unless properly treated. Many consider the ideal patients for facial laser resurfacing to be Fitzpatrick skin types I-III, with moderate to severe photodamage and rhythms (Fig. r.z) and/or soft atrophic acne scars with bevelled edges (Fig.

OVERVIEW OF TREATMENT STRATEGY
The photoaging scale (see Box 1.1) is a 9-point clinical classification system used to evaluate the degree of wrinkling and photodamage (see Table I 2) Patients are classified into one of three groups corresponding to mild, moderate and severe wrinkling, which will represent the depth and number of wrinkles, and the degree of elastosis and dyschromia. To assess the response of the scars to the CO2 laser, you can assess the level of improvement by gently stretching the area of skin with the scars.
TREATMENT TECHNIQUE o Equipment
Atrophic scars will flatten as the skin is stretched. However, deep acne scars will not stretch, and this is a predictor that they are unlikely to respond to laser resurfacing.
TREATMENT ALGORITHM . Preoperative evaluation
Before the treatment, it must be assessed how many passes with the laser are necessary and, if applicable, in which areas. Further passes with the laser should be oriented perpendicular to the first pass, as this will reduce the risk of striations on the skin postoperatively.
TROUBLE SHOOTING AND IMPORTANT TIPS
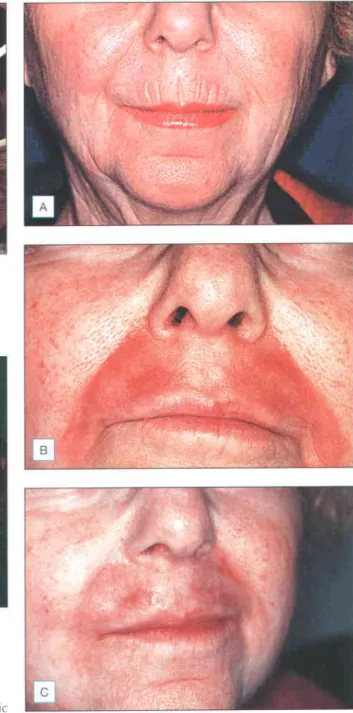
One of the problems with laser resurfacing is recognizing when to stop treating an area. The epidermal dabs of the single-pass areas can be left intact to promote wound healing in these areas and create a transition area with the untreated skin (Fig. r.r4).

SIDE EFFECTS, COMPLICATIONS, AND ALTERNATIVE APPROACH E5
Pseudohypopigmentation refers to the relative hypopigmentation of the repaired skin compared to the actinically bronzed and photodamaged non-renewed skin. Ectropion is a rare complication that can occur due to excessive tissue tightening of the lower eyelids.

ADVANCED TOPICS
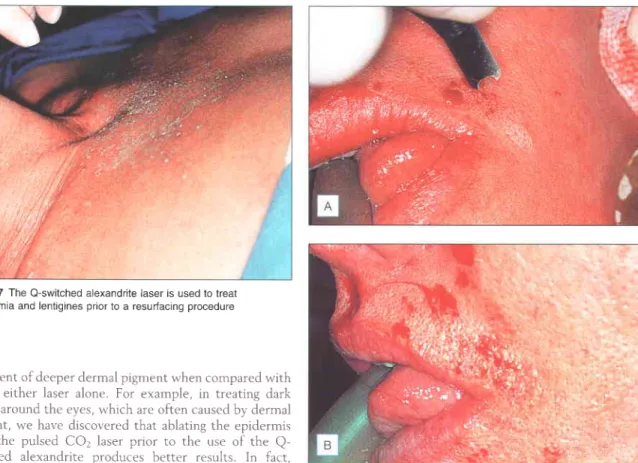
For the treatment of the above-mentioned irregularities, the use of the Er:YAG laser allows deeper penetration and finer imaging necessary to enhance such lesions (Fig. r.z8). Manuskiatti W, Fitzpatrick RE, Goldman MP, et al. 1999 Prophylactic antibiotics in patients undergoing laser skin resurfacing.

TECHNIQUES
There is a trade-off between absolute hemostasis and reduced thermal iniurv when comparing CO2 lasers with the dual-mode Contour Er: YAG laser. Any Er:YAG laser can be used for these procedures, as the goal is to provide only surface vaporization.
OUTCOMES
Indeed, one of the real advantages of Er: YAG laser is the hands-off nature of this technique, with very little tissue manipulation. Er:YAG beam should be diverged over a distance of more than about 5 in. By retracting the handpiece, a very significant reduction in fluences for spring purposes can be achieved.
SUMMARY
Post-inflammatory hyperpigmentation is almost guaranteed in those with darker skin types, but is never permanent when properly treated, according to Polnikorn et al Hydroquinone cream 40lo begins at 3-4 weeks after surgery and continues for approximately 6-8 week. Contrary to popular belief, this is a problem for those with skin types I and II, and is rarely seen in those with darker skin types.
FURTHER READING
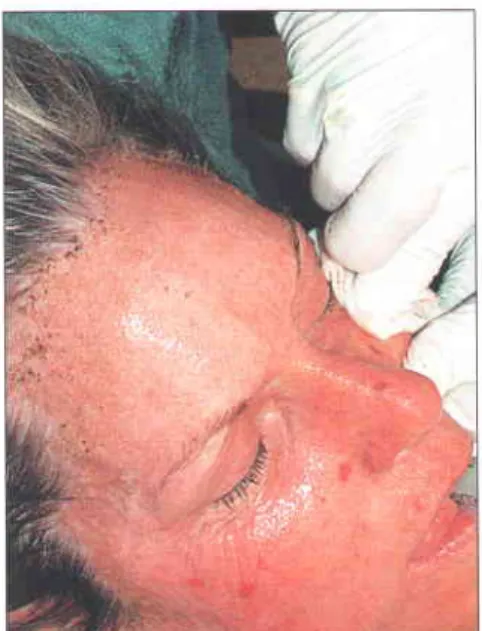
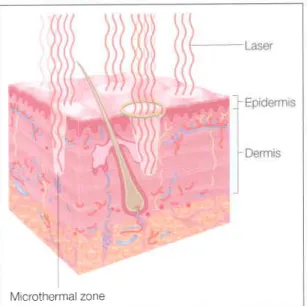
Patients can often apply make-up or sunscreen after treatment (Fig. z.r) Intervening normal tissue allows rapid re-epithelialization by keratinocyte migration and division of transient amplifying cells in the treatment column After 2-3 days, the tips of the injured areas are shed as microscopic epidermal necrotic debris (MENDs;. The depth and area of the thermal effect is determined by the energy placement and the size of the point of the hand part.
PATIENT SELECTION
In 2006, Weiss et al published the use of the AffirmrM device to treat photodamage and scarring. There are also reports of treatment of hypopigmentation using fractional technology (Friedman et al 2006).
OVERVIEW OF TREATMENT STRATEGY o Treatment approach
Neither current fractional technologies nor PSR can truly compare to traditional CO2 recovery for the treatment of difficult rhythms and excessive solar elastosis, but both can offer significant improvements with a superior safety profile and more comfortable healing time for the patient. During the initial consultation, a complete medical and surgical history must be obtained from the patient.

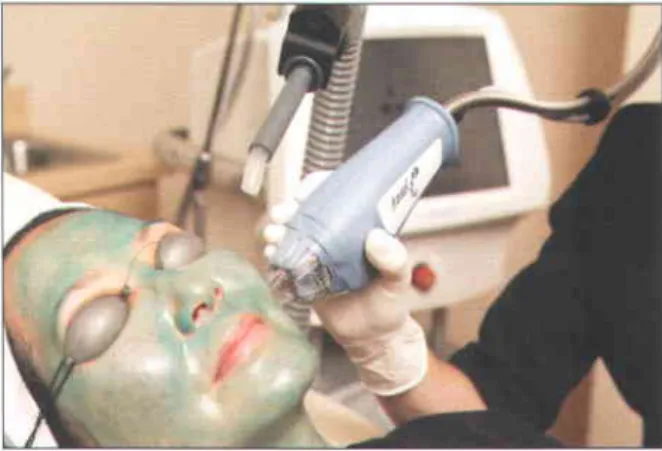
TREATMENT TECHNIQUES o Patients
The benefits, risks, and limitations of the different types of ablative and microablative resurfacing should be discussed in detail with the patient, including mention of alternative therapies, so that the patient can make an informed decision.
TREATMENT ALGORITHM o Fractional photothermolysis
Again, when the end of the cosmetic unit is reached, the handpiece should be moved back over the same line. A 7 mm tio is available for use in treating small areas such as To avoid demarcation lines with high energy protocols, the boundaries of the treatment area should be feathered by increasing the distance of the nose from the skin surface to approximately 1 cm.
TROUBLESHOOTING
There are three recommended treatment guidelines, called PSRI, PSR2 and PSR3 (Table n.l). The PSRI protocol uses a series of low-energy treatments, 3 weeks apart. The first treatment is performed at 7.0-7.2 J and energies are increased as tolerated on subsequent visits. Recovery time is 3-4 days. The PSRI protocol is a good choice for people with mild to moderate light damage or for people who cannot tolerate more than a few days of healing time. The PSR2 protocol uses one high-energy pass (3.0-4.0 J) with recovery time of 5-7 days, and the PSR3 protocol uses two high-energy passes (3.0-4.0J) with a recovery time of 6-10 days.
SIDE EFFECTS, COMPLICATIONS, AND ALTE RNATIVE APPROACH ES
We hold the towel approximately 5 mm from the surface of the skin. After the procedure, no charring occurs and the epidermis remains intact. application. Patients should be instructed to avoid sun exposure and apply a gentle ointment to the face at frequent intervals while the skin heals.
ADVANCED TOPICS: TREATMENT TIPS FOR EXPERI ENCED PRACTITION ERS
Alster T, Tanzi E 2006 Plasma skin resurfacing for neck, chest and hand rejuvenation: Investigation of a new device Lasers in Surgery and Medicine 38:20. Rahman Z, Tanner H, Chan KF, Jiang K 2006b Histological and Clinical Evaluation of the Use of Forced Cold Air with Fractional Laser Resurfacing in Surgery and Medicine 3 8 : 6 2.
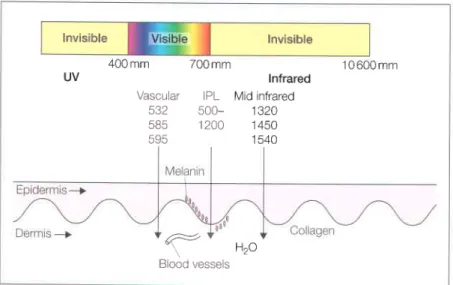
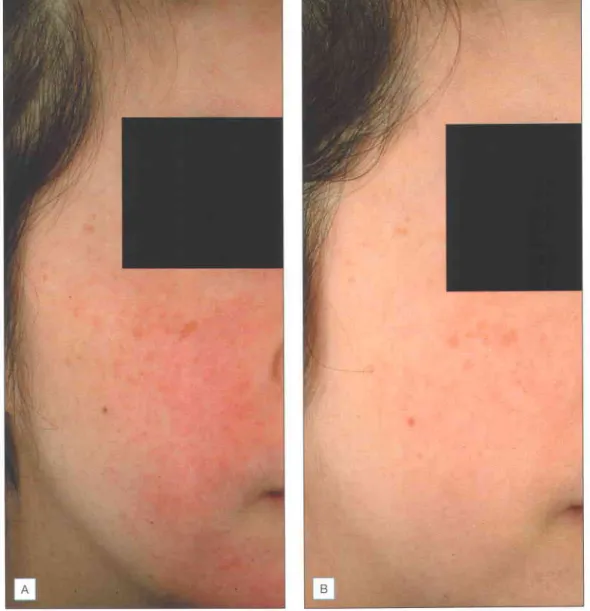
INTENSE PULSED LIGHT
IPL is used for almost all the same indications as laser systems. LEDs are now used to treat a wide range of dermatological conditions including acne, photodamage, non-melanoma skin cancers, skin rejuvenation, dyschromia, vitiligo and wound healing.
LIGHT.EMITTING DIODES
LED photomodulation can be used for skin rejuvenation alone, but has also been effective in increasing outcomes in patients receiving concurrent non-ablative thermal and vascular treatments such as IPL, pulsed dye laser, KTP and infrared lasers, radiofrequency energy/ and ablative lasers . Patient choice for LED therapy is extensive due to its excellent safety profile and extensive list of applications. Patients in whom LED treatment is contraindicated are those with photosensitivity due to drugs such as antibiotics or systemic diseases such as lupus erythematosus.
OVERVIEW OF TREATMENT STRATEGY . Treatment approach
The fluence is incrementally increased until the thermal sensor reads between 42 and 48"C. The 1450-nm and 1540-nm units do not offer this option. The IPL emits a strong flash of light that can be seen by the patient even with eye protection.
ADVANCED TOPICS: TREATMENT TIPS FOR EXPERI ENCED PRACTITION ERS
Appropriate eye protection in the form of dark lenses is required for the surgeon and staff present. Similarly, IPL treatments for small networks of vessels can be used in conjunction with KTP or FLPDL for larger, discrete vessels in the paranasal fold.
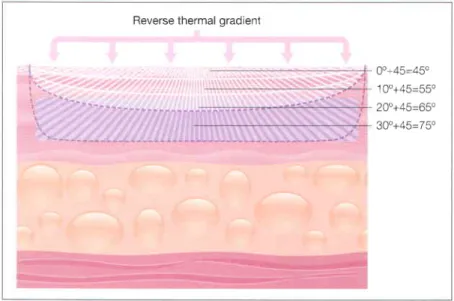
The depth of the RF field in the tissue varies with the surface area of the treatment tip electrode design The larger the surface area of the tip electrode, the deeper the heat produced. The depth of the protected tissue area on the surface is controlled by the time and intensity of cooling.
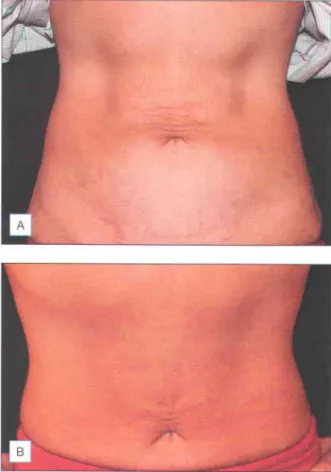
CLINICAL APPLICATION o Patient selection
The Accent bipolar and unipolar RF device was recently approved by the FDA for the treatment of rhytides on both the face and body. A pilot study of 26 patients with cellulite on the thighs and buttocks were treated with two sessions of unipolar RF with the Accent device. Recently, Alexiades-Armenakas completed two randomized, blinded, split-design, controlled trials with the Accent for the treatment of facial rhytides and laxity and for the treatment of facial cellulite.

TREATMENT PROTOCOLS . Patients
Multiple passes are performed only over the central two-thirds of the forehead where there is frontalis muscle deep to the treatment point. It is recommended that treatment pulses be placed laterally and below the bony orbital rim. The initial pass of the lower face should be set to .

SIDE EFFECTS, COMPLICATIONS, AND ALTERNATIVE APPROACH ES
The machine also stops any treatment pulse if all four corners of the treatment tip are not in contact with the skin (when using the fast treatment tip). If using the Accent system, it is imperative that the physician maintain mobility of the handpiece throughout the procedure.
ADVANCED TOPICS: TREATMENT TIPS FOR EXPERI ENCED PRACTITION ER5
There are only limited data on the optimal cooling parameters and efficacy of other cooling devices for the treatment of vascular lesions when used in dark-skinned patients. Furthermore, studies looking at the use of these devices for the treatment of port wine stains in patients with dark skin have shown an increased risk of complications.
OVERVIEW OF TREATMENT STRATEGY . Maior determinants
Many devices can be used for hair removal, including long pulsed ruby, alexandrite, diode and Nd:YAG lasers, as well as IPL Optimal cooling, longer wavelengths and long pulse widths are essential to improve efficacy and reduce side effects. These results were further confirmed by Alster et al (2001), who studied 20 dark-skinned patients who were safely and effectively treated with long-pulsed Nd:YAG lasers.
TREATMENT TECHNIQUES . Treatment algorithm
In all cases, a moderate-strength steroid mixture with antibiotics is administered once immediately after treatment to reduce the risk of PIH. The application of moderate-strength topical steroid immediately after laser and IPL surgery may also reduce the risk of PIH.
FUTURE STUDY
Lasers in Surgery and Medicine Sl3:245 Lee MW 2002 Combination of visible and infrared lasers for skin. Sadick NS, Makino Y 2004 Selective electrothermolysis in aesthetic medicine: a review Lasers in Surgery and Medicine.
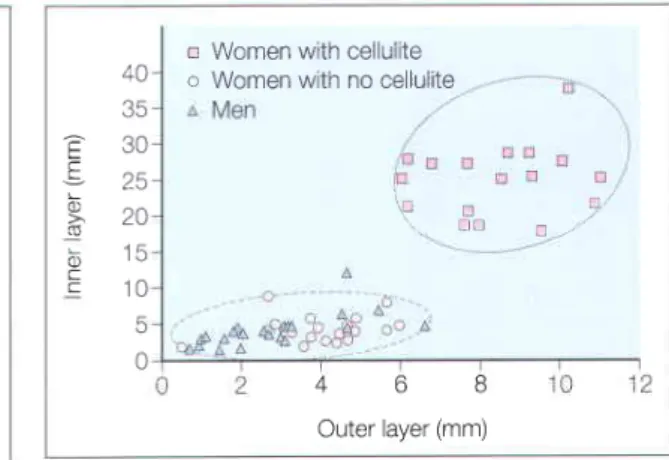
Many newer cellulite therapies attempt to increase lymphatic drainage and microvascular circulation. Recent in vivo magnetic resonance imaging (MRI) has confirmed gender differences in fibrous septal structures. In women with cellulite, there is a greater proportion of fibrous septa that are perpendicular to the skin and a smaller proportion of septa that are parallel to the skin (Figure 5.5), findings that to some extent confirm the initial work of Nurnberger and Muller.
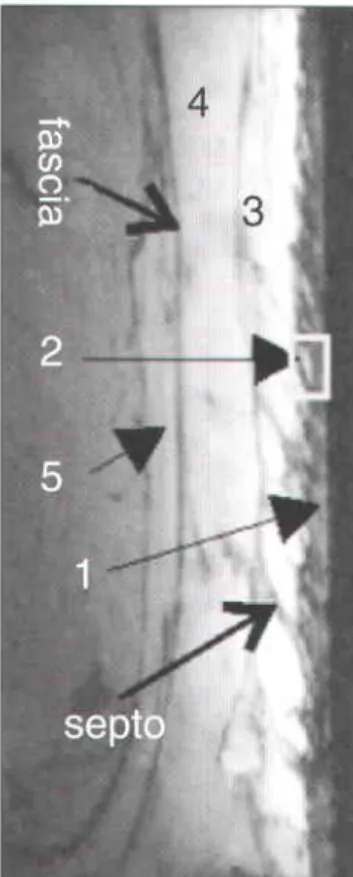
EVALUATION
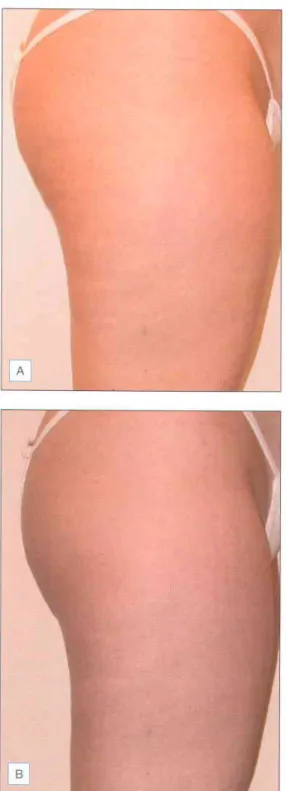
Note the extrusion of adipose tissue into the dermis of the affected individual (Reprinted with permission from Pierard-Franchiemont C, Pierand GE, Henry F, et al. 2000 A randomized, placebo-controlled trial of topical retinal in the treatment of cellulite Am J Clin Dermatol MR imaging shows that women with cellulite have a much greater increase in the thickness of the deep visceral fat layer compared to normal women or men (Reprinted with permission from Blackwell from Querleux B, Cornillon C, Jolivet O, Bittoun J Anatomy and physiology of subcutaneous adipose tissue by in vivo magnetic resonance imaging and spectroscopy: relationship to gender and presence of cellulite.
CLASSIFICATION
TREATMENT/MANAGEMENT
Another option is direct injection of pharmacological agents directly into the dermal-subcutaneous junction of the skin. The authors claimed that 900/o of patients reported favorable improvements in their areas affected by cellulite.
LASER/LIGHT/EN ERGY TREATM ENTS
Pierard-Franchiemont C, Pierand GE, Henry F, et al. 2000 A randomized, placebo-controlled trial of topical retinal for the treatment of cellulite. Rosenbaum M, Prieto V, Hellmer J, et al. 1998 An exploratory study of the morphology and biochemistry of cellulite Plastic Reconstructive Surgery.
ABLATIVE LASER SKIN RESURFACING
Due to the various side effects and complications that are possible after cutaneous laser surgery, it is important that each. Ectropion of the eyelids is another potentially serious complication after cutaneous laser resurfacing, which often requires surgical correction (Fig. Z.ro).

NONABLATIVE SKIN RESURFACING
FRACTIONAL PHOTOTH ERMOLYSIS
Furthermore, since the stratum corneum has a nominal water content, the cape remains intact immediately after treatment. Therefore, the wound created by fractional resurfacing is unique; it's not just an ablative laser used to make "holes". Erosions are occasional and can be controlled with generous application of medicated ointment based on vaseline and cold water compresses every 2-3 hours (Fig. 7.rz). Although the incidence of post-inflammatory hyperpigmentation is less than that seen after ablative laser skin resurfacing, topical bleaching agents and mild glycolic acid peels can accelerate its resolution.
VASCU LAR-SPECI FIC LASERS
Hair induction after laser hair removal and its treatment Journal of American Academy of Dermatology. Nanni CA, Alster TS 1999 Laser hair removal: side effects of Q-switched Nd:YAG, long-pulsed ruby, and alexandrite lasers Journal of the American Academy of Dermatology.

P parn
Polaris handpiece see Galaxy radio frequency unit polychromatic light sources, intense pulsed light, 49 port wine spots, 75.