Difference of Sleep Pattern between Ward and Outpatient Clinic Nurses
in Haji Adam Malik Hospital Medan
Zuraini, Aldy S. Rambe, dan Darulkutni Nasution
Department of Neurology, Medical Faculty University of Sumatera Utara Haji Adam Malik Hospital, Medan, Indonesia
Abstract: Background and Objective: Sleep and wake have a cycle known as circadian rhythm. Characteristic of human circadian system is activity in daytime and sleep in night time. Sixty to seventy percent of night shift workers had experienced sleep disturbance. The objective of this study is to determine the difference of sleep pattern between ward and outpatient nurses at Haji Adam Malik Hospital Medan.
Methods: A cross sectional study, conducted in Haji Adam Malik Hospital Medan between January–April 2005. Sample was taken randomly, consisted of 120 nurses of ward and 62 nurses of outpatient clinic at Haji Adam Malik Hospital Medan. Chi-Square test was used for statistical analysis.
Results: Sixty nurses (50.4%) of the ward had sleep time less than 6 hours. Sleep latent period over 30 minutes was found in 16 nurses (13.4%) and day time sleepiness was found in 90 nurses (75.0%). While in outpatients clinic, 26 nurses had sleep time less than 6 hours(41.3%), 3 nurses had sleep latent period more than 30 minutes (4.8%) and 43 nurses had daytime sleepiness (69.4).
Conclusions: There is no significant difference of sleep pattern between nurses in ward and outpatient clinics at Haji Adam Malik Hospital Medan.
Keywords: sleep pattern, circadian rhythm
INTRODUCTIONS
Sleep is an active and complex state comprising four stages of non rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. Wakefulness and sleep stage are characterized by physiologic measures that are assessed by polysomnography.1,2,3
Stage 1 sleep is characterized by a low-voltage, mixed frequency EEG and slow, rolling eye movements. Reactivity to outside stimuli is decreased, and mentation may occur but is no longer reality-oriented. Stage 2 consists of moderate low-voltage back ground EEG with sleep spindles (bursts of 12-to 14-Hz activity lasting 0.5 to 2 seconds) and K-complexes (brief high-voltage discharge with an initial negative deflection followed by a positive component) heart and respiratory rates are regular and slightly slower. Stage 3 sleep consist of high-amplitude theta (5 to 7
Hz) and delta (1 to 3 Hz) frequencies, as well as interspersed K-complexes and sleep spindles. Stage 4 sleep is similar to stage 3, except that high–voltage delta waves make up least 50% of the EEG and sleep spindles are few or absent. Stage 3 and 4 are often combined and referred as to delta sleep, slow-wave sleep, or deep sleep. During this deeper sleep, heart and respiratory rates are slowed and regular. During NREM sleep, the tonic chin EMG is of moderately high amplitude but less than of quite wakefulness.1,2,4
a secondary period of increased sleepiness occurs over the mid afternoon. The biological clock makes it difficult for people to sleep during the day and to remain awake during the night.5,6
It is uncertain how many hours a person needs to sleep, whereas total sleep time depends on age. Commonly, sleeping less than 6 hours a day can cause sleep deprivation.1,7
Approximately 20 to 25 percent of the working population is involved in some from of shift work.5
A wide range of important occupations is involved in shift work (e.g., doctors, nurses, police, fire-man, airline pilots, air-traffic controllers, diplomats, international business executive, radar operators, postal workers, long distance truck drivers, and others).1
No definitive studies have been done on the precise prevalence of problem sleepiness among shift workers, but in survey studies, about 60 to 70 percent of shift workers, complain of sleep difficulty or problem sleepiness. Physiological measures during stimulated late night shift hours indicate a degree of sleepiness that is considered severe and clinically pathological when present during the day. Clearly, excessive sleepiness is a major problem for shift workers, especially night shift 8 to 8.5 hours.5
The objective of this study is to determine the difference of sleep pattern between ward nurses who work with shift system and outpatient clinic nurses who work without shift system at H. Adam Malik Hospital Medan.
MATERIAL AND METHODS
This is a cross sectional study, conducted in Haji Adam Malik Hospital Medan between January–April 2005. Ward nurses who did not work on shift and outpatient clinic nurses on shift work outside Haji Adam Malik Hospital Medan were excluded. One hundred and eighty two sample were eligible in this study, consist of 120 nurses of ward and 62 nurses of out patient clinic in Haji Adam Malik Hospital Medan. After getting information from us, questionnaire was given to them.
The questionnaire was adapted from a study that conducted by Bruni O, et al. (1997) in Rome. The questionnaire was in two sections, The first was to obtain demographic data about age, sex, and marital status. The second section was made up to 45 items. The items were grouped into eight
components (duration of night-time sleep, sleep latency, bedtime difficulties, sleep quality, night awakenings, nocturnal symptoms, morning symptoms, and daytime sleepiness). Evaluation was about sleep disorder experienced in the last 6 months.8
Statistical analysis was done using cross tabulation with chi-square test. Computerized using SPSS software, version 11.5.
RESULTS
Of the eligible ward nurses, 114 (95%) were female, while in outpatient clinic nurses, 60 (96.8%) were female.
Of the 120 ward nurses, 106 (88.3%) participants were married, of 63 outpatient clinic nurses, 57 (91.9%) participants were married.
1. Duration of Night-Time Sleep
There was no significant difference between nurses who have duration of night-time sleep < 6 hours and > 6 hours in both ward and outpatient clinic nurses (p = 0.278) (Table 3).
2. Sleep Latency
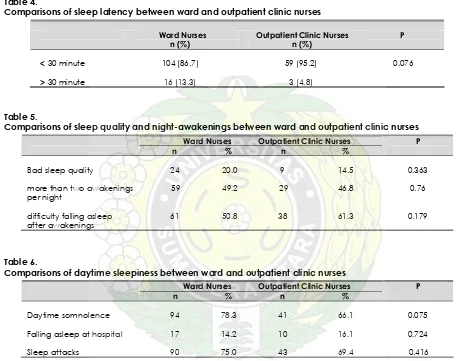
There was no significant difference between nurses who have sleep latency < 30 minutes and > 30 minutes in both ward and outpatient clinic nurses (p = 0,076) (Table 4).
3. Sleep Quality
There was no significant difference in bad sleep quality between ward and outpatient clinic nurses (p = 0.363) (Table 5).
4. Night-awakenings
There was no significant difference in more than two awakenings per night (p = 0.76) and difficulty falling asleep after awakenings (p = 0.179) between ward and outpatient clinic nurses (Table 5).
5. Daytime Sleepiness
There was no significant difference of daytime somnolence (p = 0,075), falling asleep in hospital (p = 0.724), and sleep attacks (p = 0.416) between ward and outpatient clinic nurses (Table 6).
Table 1.
Demographic characteristic of samples
Ward Nurses Outpatient Clinic Nurses
n % n %
Sex
Male 6 5 2 3.2
Female 114 95 60 96.8
Status
Married 106 88.3 57 91.9
Unmarried 14 11.7 5 8.1
Age
< 30 years old 42 35 5 8.1
31–40 years old 71 59.2 40 64.5
41–50 years old 6 5 15 24.5
> 50 years old 1 0.8 2 3.2
Table 2.
Prevalence of sleep disorders (presence more than 1/week)
Variable
Outpatient Ward Nurses Clinic Nurses P n (%) n (%)
BEDTIME PROBLEM
3 Reluctant to go bed 23(19.2) 6 (9.2) 0.97
4 Bedtime variations 48(40.0) 15(24.2) 0.34
5 Difficulty getting to sleep at night 31(25.8) 19(30.6) 0.491
6 Anxiety/fear when falling asleep 26(21.7) 5(8.1) 0.21
7 Drink stimulant beverages in the evening 16(13.3) 8(12.9) 0.95
8 Need for light or TV in the bedroom 66(55.0) 40(64.5) 0.17
9 Need for a transitional object 46(38.3) 21(33.9) 0.554
10 Fluids or drugs to facilitate sleep 7(5.8) 7(11.3) 0.19
11 Hypnic jerks 31(25.8) 19(30.6) 0.491
12 Rhythmic movement while falling asleep 18(15.0) 9(14.5) 0.931
13 Hypnagogic hallucinations 14(11.7) 8(12.9) 0.808
14 Falling asleep sweating 43(35.8) 19(30.6) 0.484
SLEEP QUALITY
15 Bad sleep quality 24(20.0) 9(14.5) 0.363
NIGHT AWAKENINGS
16 More than two awakenings per night 59(49.2) 29(46.8) 0.76
17 Waking up screaming in the night 21(17.5) 7(11.3) 0.271
18 Waking up to drink or eat in the night 39(32.5) 15(24.2) 0.245
19 Getting up to use the bathroom 88(73.3) 44(71.2) 0.735
20 Waking up complaining of headache 31(25.8) 19(30.6) 0.491
21 Waking up with leg cramps 44(36.7) 19(30.6) 0.418
22 Difficulty falling asleep after awakenings 61(50.8) 38(61.3) 0.179
NOCTURNAL SYMPTOMS
23 Nocturnal hyperkinesia 26(21.7) 7(11.3) 0.085
24 Unusual movement during sleep 16(13.3) 8(12.9) 0.95
25 Pains of unknown origin during sleep 31(25.8) 19(30.6) 0.491
26 Sleep breathing difficulties 14(11.7) 5(8.1) 0.451
27 Sleep apnea 13(10.8) 3(4.8) 0.176
28 Snoring 44(36.7) 19(30.6) 0.418
29 Night sweating 39(32.5) 17(24.4) 0.482
30 Sleepwalking 1(0.8) 2(3.2) 0.230
31 Sleep talking 19(15.5) 6(9.7) 0.253
32 Bed-wetting 5(4.2) 4(6.4) 0.50
33 Bruxism 20(16.7) 4(6.4) 0.054
34 Sleep terrors 15(12.5) 5(8.1) 0.365
35 Nightmares 44(36.7) 19(30.6) 0.418
36 Report of frightening dream 31(25.8) 19(30.6) 0.491
37 Convulsions during sleep 11(9.2) 5(8.1) 0.803
MORNING SYMPTOMS
38 Difficulty in waking up in the morning 31(25.8) 19(30.6) 0.491
39 Variation of waking time 59(49.2) 35(56.5) 0.351
40 Restless sleep 33(27.5) 13(21.0) 0.337
41 Sleep paralysis 13(10.8) 3(4.8) 0.176
42 Hallucinations on waking up in the morning 9(7.5) 4(6.5) 0.795
DAYTIME SLEEPINESS
43 Daytime somnolence 94(78.3) 41(66.1) 0.075
44 Falling asleep at school 17(14.2) 10(16.1) 0.724
Table 3.
Comparisons of duration of night-time sleep between ward and outpatient clinic nurses
Ward Nurses n (%)
Outpatient Clinic Nurses n (%)
P
< 6 hours 60 (50.4) 26 (41.9) 0.278
> 6 hours 59 (49.6) 36 (58.1)
Table 4.
Comparisons of sleep latency between ward and outpatient clinic nurses
Ward Nurses n (%)
Outpatient Clinic Nurses n (%)
P
< 30 minute 104 (86.7) 59 (95.2) 0.076
> 30 minute 16 (13.3) 3 (4.8)
Table 5.
Comparisons of sleep quality and night-awakenings between ward and outpatient clinic nurses
Ward Nurses Outpatient Clinic Nurses
n % n %
P
Bad sleep quality 24 20.0 9 14.5 0.363
more than two awakenings 59 49.2 29 46.8 0.76
per night
difficulty falling asleep 61 50.8 38 61.3 0.179
after awakenings
Table 6.
Comparisons of daytime sleepiness between ward and outpatient clinic nurses
Ward Nurses Outpatient Clinic Nurses
n % n %
P
Daytime somnolence 94 78.3 41 66.1 0.075
Falling asleep at hospital 17 14.2 10 16.1 0.724
Sleep attacks 90 75.0 43 69.4 0.416
Table 7.
Comparisons of daytime sleepiness between ward who have shift work < 2 years and > 2 years
< 2 years > 2 years
n % n %
P
Daytime somnolence 12 80 82 87.1 0.867
Falling asleep at hospital 3 20 14 13.3 0.489
DISCUSSIONS
Shift work sleep disorder consists of symptoms of insomnia or excessive sleepiness that occur as transient phenomena in relation to work schedules.9
Insomnia is defined as a sleep latency of greater than 30 minutes and less than 6 hours of sleep per night.10
The prevalence depends on the prevalence of shift work in the population. It appears that most individuals experience sleep difficulties after a night shift. Depending on which country is considered between 5% and 8% of the population is exposed to night work on regular or irregular basis. Thus, the prevalence of shift work sleep disturbance of 2% to 5% may be a reasonable estimate. These figures however, do not involve individual with early morning work, which may compressed another group at risk.9
The work is usually scheduled during the habitual hours of sleep (i.e., shift work-rotating or permanent shifts), roster work, on irregular work hours. The sleep complaint typically consists of an inability to maintain a normal sleep duration when the major sleep episode is begun in the morning (6 a.m. to 8 a.m.) after a night shift. The reduction in sleep length usually amounts to one to four hours (mainly affecting REM and stage 2 sleep). Subjectively, the sleep period is perceived as unsatisfactory and unrefreshing. The insomnia appeared despite the patient’s attempts to optimize environmental conditions for sleep. The condition usually persists for the duration of the work-shift period. Early morning work shift (starting between 4 a.m. and 7 a.m.) may also be associated with complaints of difficulty in sleep initiation as well as difficulty in awakening. Work on permanent evening shift can be associated with difficulties initiating the major sleep episode. Excessive sleepiness usually occurred during shift (mainly night) and was associated with the need to nap and impaired mental ability because of the reduced alertness.9
Problem sleepiness in shift workers is due to both sleep reductions and night time working. These come about by the failure of the unadjusted circadian system to prepare shift workers for a restful, uninterrupted bout of refreshing sleep, and the problem is amplified by the demands and distractions of a
day-oriented society. Even in those whose sleep is adequate, however, sleepiness will still occur during the night shift and on the drive home from evening shift because of the natural cycles of sleepiness driven by the circadian system or daily biological clock. Whatever countermeasures are used to improve sleep, sleepiness from this latter cause will be present until the usually slow process of resetting the timing of the clock occurs.5
No know anatomic or biochemical pathology has been described. The condition is directly related to circadian interference with sleep during the morning and evening, which conflicts with the shift workers need to sleep at these times. The excessive sleepiness during night work appears to be partly related to the lack of sleep and partly related to the conflict between requirement of working at night and the circadian sleepiness propensity during the night hours.9
Survey studies of shift workers indicate that they report an average of about 1 hours less sleep per 24 hours (i.e., about 7 hours less sleep per week) than their day-working counterparts. Physiological measures during stimulated late night shift hours indicate a degree of sleepiness that is considered severe and clinically pathological when present during the day.5
In this study there was no significant difference of sleep pattern including duration of night-time sleep (p=0.278), sleep latency (p=0.076), sleep quality (p = 0.363), more than two awakening per night (p=0.76), difficulty falling asleep after awakenings (p=0.179), daytime somnolence (p=0.075), falling asleep at hospital (p=0.724) and sleep attacks (p=0.416) sleep between nurses in ward and outpatient clinic. These findings were not in accordance with the result of previous study. This was probably due to lack of samples and the regular rotating shift system (i.e., alternate week of night and day shift) so that circadian rhythm was not constantly impaired.
evening and night shift were significantly longer.11
Harma et al., did a research about the effect of an irregular shift system on sleepiness at work in train drivers and railway traffic controllers. Severe sleepiness was reported in 49% (train drivers) and 50% (railway traffic controllers) of the night shift and in 20% (train drivers) and 15% (railway traffic controllers) of the morning shift. The risk for severe sleepiness was 6–14 times higher in the night shift an about twice as high in the morning shift compared with the day shift.12
Study conducted by Sallinen et al. toward train drivers and traffic controllers found that the risk for dozing off during the shift was associated only with the shift length, increasing by 17 and 35% for each working hour in the morning and the night shift. The result demonstrate advantageous and disadvantageous shift combinations in relation to sleep and make it possible to improve the ergonomic of irregular shift systems.13
In this study there is no significant difference between ward nurses who have shift work for < 2 years and > 2 years who have daytime somnolence (p = 0.867), falling asleep at hospital (p = 0.489), and sleep attacks (p = 0.633).
There was also no significant difference in other sleep disturbances (bedtime problems, nocturnal symptoms and morning symptoms) between ward nurses and outpatient clinics nurses.
CONCLUSIONS
In this study there was no significant difference of sleep pattern including duration of night-time sleep, sleep latency, sleep quality, more than two awakening per night, difficulty falling asleep after awakenings, daytime somnolence, falling asleep at hospital and sleep attacks sleep between nurses in ward and outpatient clinic.
To obtain a better result, a further study with large sample is needed.
REFERENCES
1. Fry JM. Sleep Disorder. In: Rowland LP, editors. Merritt’s Neurology. 10th
ed. Philadelphia: Lippincott Williams & Wilkins; 2000. p. 839-46.
2. Adam and Victor’s. Principles of Neurology. 7th
ed. New York: McGraw-Hill; 2001.
3. Mahowald MW. Disorder of Sleep and Arousal. In. Rizzo M, Eslinger PJ, editors. Principles and Practice of Behavioral Neurology and Neuropsychology. Philadelphia: W.B. Saunders Company; 2004. p. 701-14.
4. Dinner DS. Physiology of Sleep. In: Levin KH, Lüders HO, editors. Comprehensive Clinical Neurophysiology. Philadelphia: W.B. Saunders Company; 2000. p. 589– 96.
5. National Center on Sleep Disorders Research and Office of Prevention, Education and Control. Working Group Report on Problem Sleepiness. Philadelphia: National Institute of Health; 1997.
6. Winkelman JW, Fogel RB. Sleep Disorders. In: Samuaels MA, editors. Manual of Neurologic Therapeutics. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2004. p. 93–104.
7. Lumbantobing SM. Gangguan Tidur. Jakarta: FK-UI; 2004.
8. Bruni O, Fabrizi P, Ottaviano S, Cortesi F, Giannotti F, Guidetti V. Prevalence of sleep disorders in childhood and adolescence with headache: a case-control study. Cephalalgia 1997; 17: 492–8.
9. America Academy of Sleep Medicine. The International Classification of Sleep Disorders, Revised: Diagnostic and Coding Manual. Chicago: America Academy of Sleep Medicine; 2001.
10. Rye DB. Sleep Disorders. In: Johnson RT, Griffin JW, McArthur JC, editors. Current Therapy In Neurologic Disease. 6th ed. St. Louis: Mosby; 2002. p. 12–21.
12. Harma M, Sallinen M, Ranta R, Mutanen P, Muller K. The Effect of an Irregular Shift System on Sleepiness at Work in Train Drivers and Railway Traffic Controllers. Journal Sleep Research 2002; 11: 141–51.
13. Sallinen M, Harma M, Mutanen P, Ranta R, Virkkala J, Muller P. Sleep-wake rhythm in an irregular shift system. Journal Sleep Research 2003; 12: 103-12.
14. Marquie JC, Foret J. Sleep, age, and shift work experience. Journal Sleep Research 1999; 8: 297–304.