Treatment of Blount Disease Using Illizarov ;
Simple and Effective Technique
A Case Series
dr. Iman Dwi Winanto, SpOT
NIP. 198302092008011008
DEPARTEMEN ILMU BEDAH ORTHOPAEDI DAN TRAUMATOLOGI
FAKULTAS KEDOKTERAN
UNIVERSITAS SUMATERA UTARA
MEDAN
INTRODUCTION
Blou t’s disease is consider to be a developmental condition, which affects the proximal medial tibial physis, characterized by disordered ossification of the medial aspect of the proximal
tibial physis, epiphysis, and metaphysis, resulting in progressive varus deformity. This progressive
deformity is manifested by varus angulation and internal rotation of the tibia in the proximal
metaphyseal region immediately below the knee.1 The natural history of this disease leads to irreversible pathologic changes, especially at the medial portion of the proximal tibial epiphysis . The
precise etiology is not known, although disorder of enchondral ossification and growth disturbances
of the subjacent physis. has been identified.1,2,3
Blount disease can occur in growing children of any age and is classified into 2 groups: early
onset and late onset. Early onset (in children < 3 y) is termed the infantile type. The late-onset group
includes the juvenile form (in children aged 4-10 y) and adolescent form (in those aged 11 years and
older) of the disease. Juvenile tibia vara usually is discussed with the infantile type, and the
remainder of this article addresses infantile and juvenile types as part of the broader grouping of the
infantile type.1,2
Indications for operative treatment include increasing severity of symptoms or progression
of deformity, children older than 3 years with Blount disease, who are either noncompliant or not
good candidates for brace treatment because of obesity or bilateral involvement, should be treated
with a varus-correcting osteotomy. The proximal tibial varus should decrease within 12 months in
those children who are compliant with bracing. The radiographic appearance of the medial epiphysis
and metaphysis should normalize by 5 years of age. If such improvement does not occur,
varus-correcting osteotomy should be recommended. 1,2,6
Early surgery to realign the leg (that is, osteotomy performed by 4 years of age) is necessary
to prevent progression to stage IV disease, which is the formation of a physeal bar. The osteotomy
unloads the medial compartment of the knee and facilitates growth of the proximal medial physis.
Restoration of normal growth in the medial tibial physis is less likely to occur if surgery is delayed.
Simple osteotomy after 5 years of age does not assure permanent correction and carries a higher
risk of recurrent deformity because of the greater pathologic change and potential for physeal bar
The proximal tibia osteotomy is performed with attention to the risks related to osteotomy
in the upper tibia and the need for obtaining adequate correction of the deformity. The fibula is
osteotomized through a separate lateral incision, taking care to avoid injury to the deep motor
branches of the peroneal nerve. The tibial osteotomy can be accomplished in a variety of ways. A
straight transverse osteotomy optimally allows for necessary adjustment in correction of frontal,
sagittal, and rotational deformity. Many surgery technique are available i treati g lou t’s disease. Treatment using illizarov with acute or gradual correction allow accurate alignment of the lower
Case History
First case
An eight years old girl presented with a progressively increasing varus deformity of both
proximal tibia since two years [Figure 1]. She had no history of trauma or fever and swelling of left knee previously. Functionally, she had pain during exercises and had difficulty in running and
participating in sports activities, besides cosmetic concerns. She was of average build with no
obvious signs of rickets. There was no muscle atrophy and the knee range of motion was 0-130°. The
knee was stable in full extension. The tibial varus was about 30o. There were no patellofemoral signs
or symptoms.
Standard antero-posterior and lateral radiographs of the left knee demonstrated tibia vara
with medial beaking and a significant depression of the medial tibial epiphysis and metaphysis
[Figure 2]. The mechanical axis deviation was assessed on a standing full-length radiograph of both lower limbs with the patellae facing forward, which showed: Tibiofemoral angle 570 MD angle 410
figure 2
She was treated withmultiple osteotomy on left proximal shaft tibia at the apex of the
center of rotation of angulation (CORA) (which was calculated on the radiographs) and distal shaft
fibula. All these osteotomies were done with small incision and multiple drilling technique with
c-arm guided. All the deformities were corrected gradually and fixed with Illizarov device, she regained
a knee range of motion from 0-130°. 3 days after the surgery she can stand with walker frame and
can achieve early mobilization.
She was then followed up clinically and radiologically at one-monthly intervals to look for
recurrence of varus or overcorrection due to resumption of growth on the medial side and the
gradual correction [Figure 3a&b]. On follow-up, the status of the medial tibial physis was studied closely and it was found that the deformity is corrected gradually with no significant complication,
on 3 months follow up the tibiofemoral angle is corrected to 290 and the MD angle is corrected to 1800 and after 6 months follow-up she had a correction of the tibiofemoral angle 18 0 and the MD
Figure 3a
Figure 4a
Second case
A seven years old boy presented with a progressively increasing varus deformity of both
proximal tibia[Figure 5]. He had no history of trauma or fever and swelling of left knee previously. Functionally, he had difficulty during exercises, in running and participating in sports activities,
besides cosmetic concerns. He was of average build with no obvious signs of rickets. There was no
muscle atrophy and the knee range of motion for both knee was 0-120°. The knee was stable in full
extension, but there was knee recurvatum found on both knee joint. The tibial varus was about 30o. There were no patellofemoral signs or symptoms. The biochemical parameters were within normal
limits.
Standard antero-posterior and lateral radiographs of the left knee demonstrated tibia vara
with medial beaking and a significant depression of the medial tibial epiphysis and metaphysis
[Figure 6]. The mechanical axis deviation was assessed on a standing full-length radiograph of both lower limbs with the patella facing forward, which showed: tibiofemoral angle 530 MD angle 440
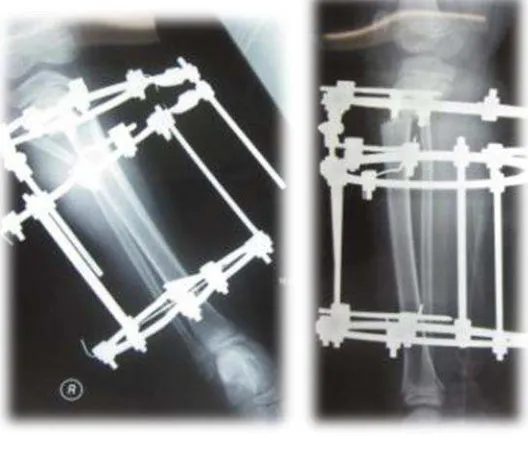
Figure 6
He was treated with osteotomy on left proximal shaft tibia at the apex of the center of
rotation of angulation (CORA) (which was calculated on the radiographs) and distal shaft fibula.
These osteotomies were done with small incision and multiple drilling technique with c-arm guided.
The deformities were corrected gradually and fixed with Illizarov device, he regained a knee range of
motion from 0-120°. First day post surgery the tibiofemoral angle was 30o and the MD angle was 21o , he can achieve early mobilization and one week after the surgery he can stand with walker frame.
He was then followed up clinically and radiologically 2 weeks intervals to look for recurrence
of varus or overcorrection due to resumption of growth on the medial side and the gradual
correction [Figure 7] and one monthly after 4 weeks followed up. On follow-up, the status of the medial tibial physis was studied closely and it was found that the deformity is corrected gradually
with no significant complication, on 3 months follow up the tibiofemoral angle is corrected to 22o
Figure 7a
Third case
Is the same patient from the second case, Standard antero-posterior and lateral radiographs
of the right knee demonstrated tibia vara with medial beaking and a significant depression of the
medial tibial epiphysis and metaphysis [Figure 8]. The mechanical axis deviation was assessed on a standing full-length radiograph of both lower limbs with the patellae facing forward, which showed:
tibiofemoral angle 44o MD angle 34o
Figure 8
He was treated with osteotomy on left proximal shaft tibia at the apex of the center of
rotation of angulation (CORA) (which was calculated on the radiographs) and distal shaft fibula.
These osteotomies were done with small incision and multiple drilling technique with c-arm guided.
The deformities were corrected acutely and fixed with Illizarov device, he regained a knee range of
motion from 0-120°. First day after surgery the tibiofemoral angle was 19o and the MD angle was 16o ,
he can achieve early mobilization and one week after the surgery he can stand with walker frame
He was then followed up clinically and radiologically 2 weeks intervals to look for recurrence of varus
or overcorrection due to resumption of growth on the medial side and the gradual correction [Figure 9] and one monthly after 4 weeks followed up. On follow-up, the status of the medial tibial physis was studied closely and it was found that the deformity is corrected gradually with no significant
complication, on 3 months follow up the tibiofemoral angle is corrected to 11o and the MD angle is corrected to 80 and he can achieve full weight bearing without any support bust still need a walker
Figure 9
Figure 11a,b
Outcome
Correction achieve by acute correction for rotational deformity followed by gradual
correction for angulation deformity. The result are both tibiofemoral angle and
metaphyseal-diaphyseal angle achieved, there were no complications of compartment syndrome and peroneal
Discussion
The objective of the osteotomy in surgical treatment for Blou t’s disease is to o tai a neutral mechanical axis with horizontal knee joint. Following the osteotomy, fixation may be
achieved with external or internal fixation. The use of cast immobilization alone has been associated
with a loss of correction.
I ter al fi atio after osteoto for Blou t’s disease has ee asso iated ith pro le s.
Loder et al reported poor result s in patients treated with internal fixation and noted many were
internally fixed in malposition. Crossed K-wires have been associated with a loss of fixation. The use
of plates has been associated with stress shielding, delayed and nonunion, and hardware breakage,
and requires a second surgical procedure to remove the implant.8,9
External fixation allows for acute or gradual correction and for later adjustment as clinically
and radiographycally indicated.in addition, external fixation allows for correction of the co existent
leg length discrepancy. Price et al reported the successful use of dynamic external fixation to
stabilize osteotomies for tibia vara without supplemental casting.
Summary
Corre tio of Blou t’s disease usi g illizaro e ter al fi atio is a si ple, safe, sta le a d
effective technique. Compared to internal fixation this technique showed minimal damaged to the
soft tissue, provide early mobilization and early weight bearing. Acute correction can be followed by
DAFTAR PUSTAKA
![Figure 2]. The mechanical axis deviation was assessed on a standing full-length radiograph of both](https://thumb-ap.123doks.com/thumbv2/123dok/583555.69426/5.595.213.360.183.448/figure-mechanical-axis-deviation-assessed-standing-length-radiograph.webp)


![Figure 6]. The mechanical axis deviation was assessed on a standing full-length radiograph of both](https://thumb-ap.123doks.com/thumbv2/123dok/583555.69426/9.595.113.423.175.440/figure-mechanical-axis-deviation-assessed-standing-length-radiograph.webp)