Diabetic and non-diabetic subjects with
ischemic stroke: Differences, subtype
distribution and outcome
Antonino Tuttolomondo
a,*
, Antonio Pinto
a, Giuseppe Salemi
b,
Domenico Di Raimondo
a, Riccardo Di Sciacca
a,
Paola Fernandez
a, Paolo Ragonese
b, Giovanni Savettieri
b,
Giuseppe Licata
aa
Biomedical Department of Internal and Specialistic Medicine, University of Palermo, P.zza delle Cliniche n.2, 90127 Palermo, Italy
b
Neurology Department, University of Palermo, Palermo, Italy
Received 28 July 2006; received in revised form 17 January 2007
KEYWORDS
Ischemic stroke; Diabetes mellitus; TOAST classification; Scandinavian Stroke Scale
Abstract Background and aim:Diabetes mellitus increases the risk of stroke, and pathophysiological changes of diabetic cerebral vessels may differ in comparison with non-diabetic ones; nonetheless, the clinical and prognostic profile of stroke in diabetic patients is not yet fully understood. On this basis, the aim of our study was to evaluate cerebrovascular risk factor prevalence in diabetic stroke patients in comparison with non-diabetics, to analyze whether diabetics have a different prevalence of stroke subtypes as classified by the TOAST classification, and deter-mine whether diabetics and non-diabetics have a different prognosis.
Methods and results:We enrolled 102 diabetics and 204 non-diabetic subjects with acute ischemic stroke, matched by sex and age (3 years). We used as outcome indicators the Scandinavian Stroke Scale (SSS) score at admission and the modified Rankin disability scale at discharge and at a 6-month follow-up. We classified ische-mic stroke according to the TOAST classification.
Diabetes was associated with lacunar ischemic stroke subtype, with a record of hypertension, and with a better SSS score at admission. The association of diabetes
* Corresponding author. Tel.:þ39 091 655 2128; fax:þ39 091 655 2285. E-mail address:pinto@neomedia.it(A. Tuttolomondo).
0939-4753/$ - see front matterª2007 Elsevier B.V. All rights reserved. doi:10.1016/j.numecd.2007.02.003
with lacunar stroke remained significant even after adjustment for hypertension or for large artery atherosclerotic and cardioembolic stroke subtypes.
Conclusion:Our study shows some significant differences in acute ischemic stroke among diabetics in comparison with non-diabetics (higher frequency of hyperten-sion, higher prevalence of lacunar stroke subtype, lower neurological deficit at admission in diabetics).
ª2007 Elsevier B.V. All rights reserved.
Introduction
Diabetes mellitus (DM) is a well-established independent risk factor for ischemic stroke (IS) [1e3]. The Framingham Study[4]found a 2.5-fold
incidence of ischemic stroke in diabetic men and a 3.6-fold one in diabetic women. In the largest case control study with adjustment for multiple known risk factors [5], the risk of stroke for dia-betic individuals increased by 2.3. Two other large studies [6,7] reported similar findings with odds ratios (OR) of 2.12 and 2.47. However, it is dif-ficult to determine the level of association be-tween DM and IS, as DM is also associated with a twofold higher incidence of hypertension and cardiac disease and with an increased incidence of asymptomatic carotid artery disease and hyper-lipidemia [8], all strong independent risk factors for IS.
Other studies [8e11] have established that the
association between DM and stroke is related to the pathologic changes observed in brain vessels. As diabetic angiopathy is presumed to differ from atherosclerotic angiopathy, strokes experi-enced by diabetic vs. non-diabetic individuals may also differ. However, data on stroke type, topography, and outcome in diabetic persons con-flict[10,11]. Moreover, most studies did not assess the interaction between DM and hypertension and the distinct clinical impact of cerebral diabetic angiopathy.
We therefore addressed the hypothesis that ischemic stroke of diabetic patients could differ from stroke in non-diabetic ones and on this basis the aim of this study was:
1. to evaluate cerebrovascular risk factor preva-lence in diabetic stroke patients in comparison with non-diabetics;
2. to analyze if diabetics have a different preva-lence of stroke subtypes as classified by the TOAST group classification[12]; and
3. to determine if diabetics and non-diabetics have different severity at onset of the stroke, and functional outcome at discharge, and on a 6-month follow-up.
Methods
Case findings
Our cases were consecutive diabetic patients di-agnosed with acute ischemic stroke admitted to the Department of Internal Medicine of Policlinico Universitario ‘‘P. Giaccone’’, Palermo, Italy, in the period 1998e2004.
Patients were defined as type 2 diabetics if they had known diabetes treated by diet, oral hypogly-cemic drugs or insulin before stroke (see Risk factors assessment). We excluded patients with stress hyperglycemia and new-onset diabetes be-cause we intended to analyze only chronic hyper-glycemia effects on stroke subtype prevalence and clinical outcome. Stroke was defined as a clinical syndrome of rapidly developing symptoms or signs of focal loss of cerebral function with symptoms which had lasted more than 24 h and had no appar-ent cause other than vascular origin[13]. Brain CT findings excluded primary intracerebral hemor-rhage, intraventricular hemorhemor-rhage, and subarach-noid hemorrhage. Diabetic stroke patients were matched with non-diabetic patients with acute ischemic stroke admitted to the Department of In-ternal Medicine of the University of Palermo with a diagnosis of acute ischemic stroke; two controls were matched to each case by sex and age (3 years).
The study was approved by the local ethics committee; the patients, or, when not possible, a family member, gave informed consent. All the procedures followed were in accordance with Italian guidelines.
Clinical protocol and TOAST classification
of ischemic stroke
cases and controls. The SSS was used to assess neurological deficit of the acute phase of stroke, through an evaluation of consciousness level, eye movement, strength in arms, hand, and legs, orientation, language, facial weakness, and gait, giving rise to a score ranging from 58 (absence of deficit) to 0 (severely impaired). According to the modified Rankin disability score the functional ability and functional outcome after stroke were graded by a score ranging from 1 (no significant disability, able to perform all usual activities of everyday life) to 6 (death). SSS and Rankin score were assessed by an experienced neurologist and by four internists that received specific training. Intrahospital mortality was ascertained. At follow-up the modified Rankin score was ascertained by the same staff in a outpatient modality.
Both diabetic and non-diabetic patients with ischemic stroke underwent the following diagnostic instrumental evaluations at admission: electrocar-diography, 24-h electrocardiography monitoring, transthoracic echocardiography, carotid ultra-sound, and brain computed tomography in baseline conditions and after 48e72 h. The type of acute
ischemic stroke was classified according to the TOAST classification in one of the following five sub-groups: (1) large artery atherosclerosis (LAAS); (2) cardio-embolic infarct (CEI); (3) Lacunar in-farct (LAC); (4) stroke of other determined etiol-ogy (ODE); (5) stroke of undetermined etioletiol-ogy (UDE)[12].
Risk factors assessment
Type 2 diabetes was determined on the basis of clinical records and by using a clinically based algorithm that considered age at onset, presenting weight and symptoms, family history, onset of insulin treatment, and history of ketoacidosis. Hypertension was defined according to older World Health Organization criteria (systolic 160 and/or diastolic 95 mmHg or on antihypertensive treat-ment on admission)[14].
Statistical methods
Both univariate and multivariate analysis were performed using conditional logistic regression analysis by the SAS package to analyze the associ-ation between diabetes and TOAST subtypes of ischemic stroke, and to evaluate the association between diabetes and lacunar stroke after correc-tion for other TOAST subtypes and hypertension. To compare acute neurological deficit between diabetic and non-diabetic subjects with ischemic
stroke, SSS was dichotomized according to the median value of the pooled distribution in both groups (diabetic and non-diabetic, median value 33). The modified Rankin disability scale was dichoto-mized as 0 (raw score from 0 to 2) and 1 (raw score from 3 to 6).
Results
We enrolled 102 type 2 diabetes subjects with acute ischemic stroke and 204 non-diabetic pa-tients with acute ischemic stroke. Diabetics and non-diabetics were matched by age (3 years) and sex. Among diabetic subjects, 44 (43%) were women and 58 (57%) were men; the median age at inclusion was 66 years (range 49e88 years).
Among non-diabetics 87 (43.1%) were women and 115 (56.9%) were men, and the median age was 67. In diabetic patients mean glycated hemoglobin (A1c) level was 7.3 mg/dl, mean diabetes dura-tion was 9.6 years; mean systolic blood pressure (SBP) was 147.5 mm/Hg; mean diastolic blood pressure (DBP) was: 92.3 mm/Hg; 43 (42.1%) had a previous diagnosis of retinopathy (background or proliferative), 29 (28.4%) had a CAD (coronary artery disease), 33 (32.3%) had a PAD (peripheral artery disease) and 29 (28.4%) had a diabetic nephropathy.
In non-diabetic patients mean systolic blood pressure (SBP) was 146.4 mm/Hg; mean diastolic blood pressure (DBP) was 94.5 mm/Hg; 51 (25%) had a CAD (coronary artery disease), 62 (30.3%) had a PAD (peripheral artery disease).
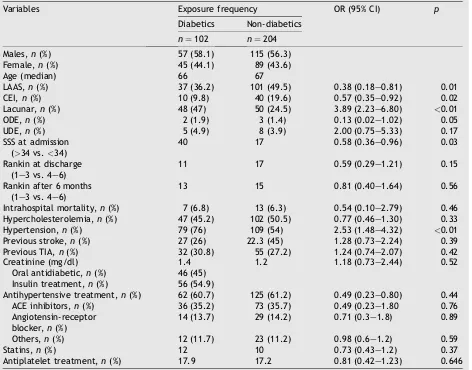
Age and sex distribution, by means of matching procedure, was similar for patients and controls and also similar was the distribution of each type of previous pharmacological treatment (antihyper-tensive treatment, statins, antiplatelet treatment) and in particular no difference was ascertained between diabetics and non-diabetics with regard to treatment with ACE inhibitors or angiotensin receptor blocker (seeTable 1).
We evaluated prevalence of risk factors for stroke (hypertension, hypercholesterolemia, pre-vious transient ischemic attack or stroke) and of each TOAST subtype of ischemic stroke (LAAS, CEI, LAC, ODE, UDE). We also analyzed the association between diabetes and some outcome indicators such as the SSS score and Rankin score at discharge and at a 6-month follow-up.
with a record of hypertension (OR 2.53, 95% CI 1.48e4.32), and with a higher SSS at admission
(OR 0.58, 95% CI 0.36e0.96) (seeTable 1). On a
mul-tivariate analysis the association of diabetes with lacunar (LAC) subtype of stroke is statistically significant (seeTable 2), and it remains significant also after adjustment for hypertension (adjusted OR 3.37, 95% CI 1.90e5.99) or for other TOAST
subtypes such as LAAS and CEI (adjusted OR 2.69, 95% CI 1.08e6.69) (seeTable 3).
No significant differences were observed be-tween diabetics and non-diabetics with regard to intrahospital mortality, Rankin score at discharge and after 6-month follow up.
Among diabetic patients no significant differ-ences were observed in prevalence of autonomic Table 1 General characteristics of diabetic and non-diabetic stroke patients and univariate analysis
Variables Exposure frequency OR (95% CI) p
Diabetics Non-diabetics
n¼102 n¼204 Males,n(%) 57 (58.1) 115 (56.3) Female,n(%) 45 (44.1) 89 (43.6) Age (median) 66 67
LAAS,n(%) 37 (36.2) 101 (49.5) 0.38 (0.18e0.81) 0.01
CEI,n(%) 10 (9.8) 40 (19.6) 0.57 (0.35e0.92) 0.02
Lacunar,n(%) 48 (47) 50 (24.5) 3.89 (2.23e6.80) <0.01
ODE,n(%) 2 (1.9) 3 (1.4) 0.13 (0.02e1.02) 0.05
UDE,n(%) 5 (4.9) 8 (3.9) 2.00 (0.75e5.33) 0.17
SSS at admission (>34 vs.<34)
40 17 0.58 (0.36e0.96) 0.03
Rankin at discharge (1e3 vs. 4e6)
11 17 0.59 (0.29e1.21) 0.15
Rankin after 6 months (1e3 vs. 4e6)
13 15 0.81 (0.40e1.64) 0.56
Intrahospital mortality,n(%) 7 (6.8) 13 (6.3) 0.54 (0.10e2.79) 0.46
Hypercholesterolemia,n(%) 47 (45.2) 102 (50.5) 0.77 (0.46e1.30) 0.33
Hypertension,n(%) 79 (76) 109 (54) 2.53 (1.48e4.32) <0.01
Previous stroke,n(%) 27 (26) 22.3 (45) 1.28 (0.73e2.24) 0.39
Previous TIA,n(%) 32 (30.8) 55 (27.2) 1.24 (0.74e2.07) 0.42
Creatinine (mg/dl) 1.4 1.2 1.18 (0.73e2.44) 0.52
Oral antidiabetic,n(%) 46 (45) Insulin treatment,n(%) 56 (54.9)
Antihypertensive treatment,n(%) 62 (60.7) 125 (61.2) 0.49 (0.23e0.80) 0.44
ACE inhibitors,n(%) 36 (35.2) 73 (35.7) 0.49 (0.23e1.80 0.76
Angiotensin-receptor blocker,n(%)
14 (13.7) 29 (14.2) 0.71 (0.3e1.8) 0.89
Others,n(%) 12 (11.7) 23 (11.2) 0.98 (0.6e1.2) 0.59
Statins,n(%) 12 10 0.73 (0.43e1.2) 0.37
Antiplatelet treatment,n(%) 17.9 17.2 0.81 (0.42e1.23) 0.646 Values are expressed as number (%). LAAS, large artery atherosclerosis; LAC, lacunar; CEI, cardio-embolic infarcts; ODE, other determined etiology; UDE, undetermined etiology; SSS, Scandinavian Stroke Scale; TIA, transient ischemic attack; ACE, angioten-sin-converting enzyme; OR, odds ratio; CI, confidence interval.
Table 2 TOAST subtypes in diabetic stroke patients: multivariate analysis
Subtype OR 95% CI p
LAAS 0.71 0.28e1.79 0.47
CEI 0.38 0.12e1.22 0.10
Lacunar 2.69 1.08e6.69 0.03 OR, odds ratio; CI, confidence interval; LAAS, large artery atherosclerosis; CEI, cardio-embolic infarct.
Table 3 Relationship between diabetes status, lacunar TOAST subtype and hypertension in diabetic stroke patients: multivariate analysis
Ictus OR 95% CI p
Lacunar 3.37 1.90e5.99 0.0001
neuropathy, CAD and nephropathy in relation to stroke subtype, whereas a slight, but not signifi-cantly higher prevalence of proliferative or back-ground retinopathy was observed in diabetic patients with lacunar subtype.
Discussion
Our study shows a higher prevalence of lacunar stroke subtype and of hypertension among di-abetics, and how, after correction for other risk factors and TOAST subtype, the association be-tween diabetes and lacunar stroke remains statis-tically significant. The pathogenic plausibility of the relationship between diabetes and lacunar stroke is supported by pathological and autopsy reports[15,16]. More recently, Megherbi et al.[17] of the European BIOMED Study of Stroke Care Group showed that diabetic patients were more likely to have lacunar cerebral infarction than non-diabetic ones, whereas Karapanayotides et al. [18], reported that diabetes mellitus was associ-ated with a comparatively higher prevalence of subcortical infarct and higher frequency of small vessel disease, and that the outcome does not differ between diabetics and non-diabetics with ischemic stroke.
Also, our group [19] previously reported that diabetes, hypertension, and a history of transient ischemic attack were more frequent among pa-tients with lacunar stroke and that mean SSS score on admission was significantly lower in patients with lacunar stroke in comparison with patients with LAAS and CEI subtypes.
Nevertheless, in our present study we showed that on multivariate analysis the association of diabetes with lacunar (LAC) subtype of stroke remains significant even after adjustment for hypertension, which underlines how the relation-ship between diabetes and lacunar strokes could exist in our diabetic subjects with ischemic stroke, partially independent from hypertension.
This is an interesting finding in the light of several studies that have underlined the role of hypertension as the first risk factor for lacunar subtype [20,21], but this is actually true in non-diabetic patients, whereas in non-diabetic ones hy-pertension could represent only a cofactor of lacunar stroke determinism [22]. Indeed lacunar stroke, as microalbuminuria, could represent a ‘‘microvascular endpoint’’ candidate, so the role of diabetes in comparison with hypertension in patients with diabetes could play a major role in the pathogenesis of microvascular stroke such as the lacunar subtype.
Although several reports underline the role of diabetes in small vessel disease pathogenesis, the clinical and prognostic profile of ischemic stroke in diabetic patients in comparison with non-diabetic ones still appears unclear. More recently two studies analyzed the differences regarding clinical features of stroke in diabetic and non-diabetic subjects. Megherbi et al. [17] reported that dia-betic patients compared with those without diabe-tes were more likely to have limb weakness, dysarthria with a handicap (Rankin Scale) and sig-nificantly higher disability (Barthel Index) grade, while Karapanayotides et al. [18] reported that diabetic stroke patients are not associated with a poor functional outcome.
We have found that SSS score at admission was higher among diabetics. This result could be related to the higher frequency of lacunar stroke subtype among diabetics, because lacunar stroke could lead to a lower neurological deficit level at admission owing to smaller brain infarct size and in particular in diabetic subjects in whom arterioles involved in lacunae could be smaller. Furthermore, if the link between inflammation and stroke is well established[23]and with lacunar subtype[24], owing to the relationship between inflammation and pathologic changes in cerebral small vessels that cause lacunar infarction (migration of foamy macrophages in the vessel walls of cerebral arteri-oles together with hyaline thickening and ectasia of parenchymal arteries), it is likely that a minor grade of chronic inflammatory response in cerebral small vessels could be involved in the pathology of diabetic brain microangiopathy owing to the minor diameter of the brain arterioles (40e200 mm vs.
200e800 mm). All these issues could represent
a pathogenic basis of our findings regarding a better outcome of lacunar stroke in diabetic subjects in terms of acute neurological deficit evaluated through SSS score. Furthermore, our finding con-cerning a non-significant difference in terms of in-hospital mortality may depend on the fact that we observed a relatively lower mortality in compar-ison with Italian epidemiological data [25]. This finding, in our opinion, although no study has yet explored and/or confirmed our hypothesis, could be due to treatment in an Internal Medicine Depart-ment with better practice toward possible life-threatening complications of ischemic stroke such as arrhythmias, acute heart failure, thromboembo-lism, renal failure and infections. Furthermore it would be desirable that future studies compare medical management of stroke patients between neurological and internal medicine settings.
matching design and the selection of two controls for each case should have limited the impact of possible bias. On the other hand, our study was specifically designed to compare diabetics with non-diabetics whereas most previous population-based studies were aimed at different primary outcomes.
In conclusion, our study shows some significant differences in the acute ischemic stroke between diabetics and non-diabetics (higher frequency of hypertension, higher prevalence of lacunar stroke subtype, lower neurological deficit grade at admission in diabetic patients) offering a chance to characterize a clinical and prognostic profile of stroke in diabetic patients that is not yet univocal in the literature.
References
[1] Warlow CP. Epidemiology of stroke. Lancet 1998;352(Suppl. 1): 1e4.
[2] Sacco RL, Wolf PA, Gorelick PB. Risk factors and their man-agement for stroke prevention: outlook for 1999 and beyond. Neurology 1999;53(Suppl. 4):S15e24.
[3] Mantovsky B, Metzger B, Molitch M, Biller J. Cerebrovascu-lar disorders in patients with diabetes mellitus. J Diabetes Complications 1996;10:228e42.
[4] Kannel WB, McGee DL. Diabetes and cardiovascular disease: the Framingham Study. JAMA 1979;241:2035e8. [5] Jamrozik K, Boradhurst RJ, Anderson CS,
Stewart-Wynne EG. The role of lifestyle factors in the etiology of stroke. A population-based case-control study in Perth, Western Australia. Stroke 1994;25:51e9.
[6] Giles WH, Kitter SJ, Hebel JR, Losonczy KG, Sherwin RW. Determinants of black-white differences in the risk of infarction cerebral. Arch Intern Med 1995;155:1319e24. [7] Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR.
Short-term predictors of incident stroke in older adults. Stroke 1996;27:1479e86.
[8] Abbott RD, Donahue RP, MacMahon SW, Reed DM, Yano K. Diabetes and the risk of stroke: the Honolulu Heart Program. JAMA 1987;257:949e52.
[9] Davis PH, Dambrosia JM, Schoenberg BS, Schoenberg DG, Pritchard DA, Lilienfeld AM, et al. Risk factors for ischemic stroke: a prospective study in Rochester. Minnesota. Ann Neurol 1987;22:319e27.
[10] Garcia MJ, McNamara PM, Gordon T, Kannell WB. Morbidity and mortality in diabetics in the Framingham population. Diabetes 1974;23:102e11.
[11] Alex M, Baron EK, Goldenberg S, Blumenthal HT. An autopsy study of cerebrovascular accident in diabetes mellitus. Circulation 1962;25:663e73.
[12] Adams HP, Bendixen BH, Kappelle J, Biller J, Love B, Gordon MD, et al. TOAST Investigators. Classification of subtype of acute ischemic stroke. Stroke 1993;24:35e41. [13] Hatano S. Experience from a multicenter Stroke register;
a preliminary report. Bull World Health Organ 1976;54: 541e53.
[14] Pogue VA, Ellis C, Michel J, Francis CK. New staging system of the fifth Joint National Committee report on the detection, evaluation, and treatment of high blood pressure (JNC-V) alters assessment of the severity and treatment of hypertension. Hypertension 1996;28(5): 713e8.
[15] Peress NS, Kane WC, Aronson SM. Central nervous system findings in a tenth decade autopsy population. Prog Brain Res 1973;40:473e83.
[16] Boiten J, Lodder J. Lacunar infarcts: Pathogenesis and validity of the clinical syndromes. Stroke 1991;22:1374e8. [17] Megherbi SE, Milan C, Minier D, Couvreur G, Osseby GV, Tilling K, et al., for the European BIOMED Study of Stroke Care Group. Association Between Diabetes and Stroke sub-type on survival and functional outcome 3 months after stroke. Stroke 2003;34:688e95.
[18] Karapanayiotides TH, Piechowski-Jozwiak B, Vam Melle G, Bogousslavsky J, Devuyst G. Stroke patterns, etiology and prognosis in patients with diabetes mellitus. Neurology 2004;62:1558e62.
[19] Pinto A, Tuttolomondo A, Di Raimondo D, Fernandez P, Licata G. Risk factors profile and clinical outcome of ische-mic stroke patients admitted in a Department of Internal Medicine and classified by TOAST classification. Int Angiol 2006;25(3):261e7.
[20] Fisher CM. Lacunes: small deep cerebral infarcts. Neurol-ogy 1965;15:774e84.
[21] Fisher CM. The arterial lesions underlying lacunes. Acta Neuropathol 1969;12:1e15.
[22] Mast H, Thompson JL, Lee SH, Mohr JP, Sacco RL. Hyper-tension and diabetes mellitus as determinants for multiple lacunar infarcts. Stroke 1995;26:30e3.
[23] Del Zoppo G, Ginis I, Hallenback JM, Iadecola C, Wang X, Feuerstein GZ. Inflammation and stroke: putative role for cytokines, adhesion molecules and i-NOS in brain Response to ischemia. Brain Pathol 2000;10:95e9.
[24] Castellanos M, Castillo J, Garcı´a MM, Leira R, Serena J, Chamorro A, et al. Inflammation-mediated damage in progressing lacunar infarctions: a potential therapeutic target. Stroke 2002;33:982e7.
[25] Francescutti C, Mariotti S, Simon G, D’Errigo P, Di Bidino R. The impact of stroke in Italy: first step for a Na-tional Burden of Disease Study. Disabil Rehabil 2005;27(5): 229e40.